Auvelity: A Rapid-Acting Antidepressant With Multimodal Activity
Information From Industry
Link to PDF
INDICATION
Auvelity is indicated for the treatment of major depressive disorder (MDD) in adults.
IMPORTANT SAFETY INFORMATION
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
- Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies.
- Closely monitor all antidepressant-treated patients for clinical worsening, and emergence of suicidal thoughts and behaviors.
- Auvelity is not approved for use in pediatric patients.
Please see Important Safety Information within this document and the full Prescribing Information
Early MDD Response May Improve Short and Long-Term Outcomes
Delayed treatment of major depressive disorder (MDD) and longer major depressive episode duration have been associated with poorer short- and long-term outcomes.1,2 People who experience shorter depressive episodes have better symptomatic outcomes, better functional outcomes, and lower relapse risk. Achieving a clinical response early in the disease trajectory with fewer treatment steps is associated with lower rates of relapse.3 A meta-analysis showed people with early improvement, defined as a ≥20%, ≥25%, or ≥30% symptom reduction on scales such as Hamilton Depression Rating Scale (HDRS17) and Montgomery–Åsberg Depression Rating Scale (MADRS), in the first 2 weeks, were 8 times more likely to achieve clinical response and 6 times more likely to achieve remission than those without early improvement.2 In a longitudinal, multicenter, observational study, people who responded to treatment within 6 weeks of initiating antidepressant treatment had approximately 4 times greater chance of achieving a positive outcome at 12 months, suggesting early clinical response (50% decrease from baseline in the 17-item Hamilton Depression Rating Scale [HDRS17] score by Week 6) is associated with improved quality of life and achieving long-term (12 months) remission.4
The Role of Glutamate in MDD
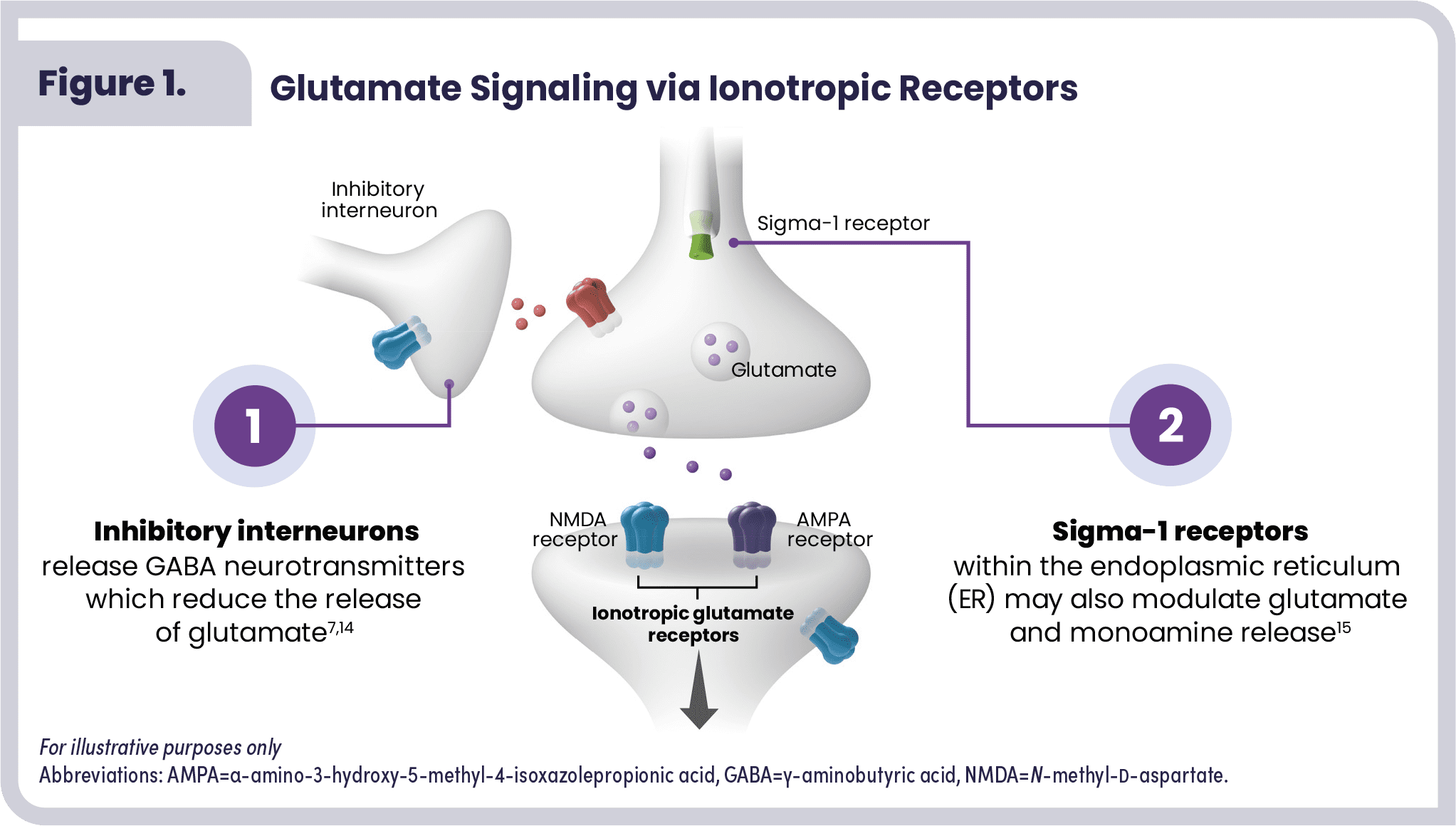
Glutamate dysfunction may play a key role in MDD. The pathophysiology of MDD is associated with disruptions of multiple neurotransmitters and receptors, including glutamatergic neurotransmission.5 Glutamate is the most abundant neurotransmitter in the CNS,6,7 being released by 40% of neurons in the brain (by contrast, fewer than 1% of neurons release each of the monoamines–dopamine, norepinephrine, and serotonin–which have also been implicated in the pathophysiology of MDD).6,8,9 Glutamate signals through metabotropic and ionotropic receptors, with N-methyl-d-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) being ionotropic receptors that are suspected targets in antidepressant effects.10,11
In vivo studies have found abnormal glutamate levels are common among patients with MDD.12,13 Modulating glutamate pathways in the brain is an emerging approach to treating MDD. The NMDA receptor in particular has emerged as a potential mediator of MDD pathophysiology.6,7
The sigma-1 receptor is thought to be a key modulator of neurobiological processes. Activation of the sigma-1 receptor, within the endoplasmic reticulum, may modulate glutamatergic and monoaminergic signaling, which may be dysregulated in MDD (Figure 1).16
AUVELITY® Mechanism of Action
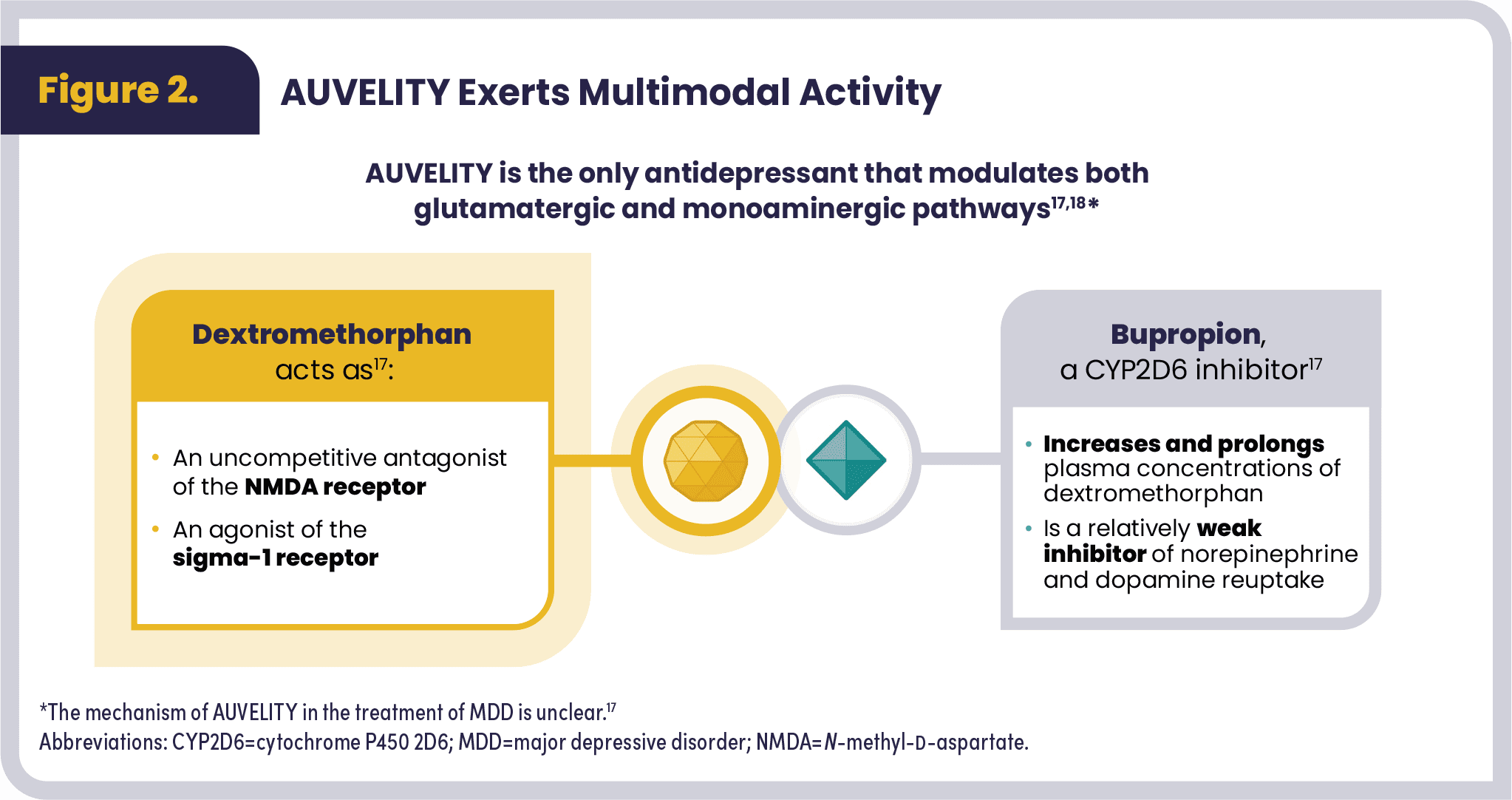
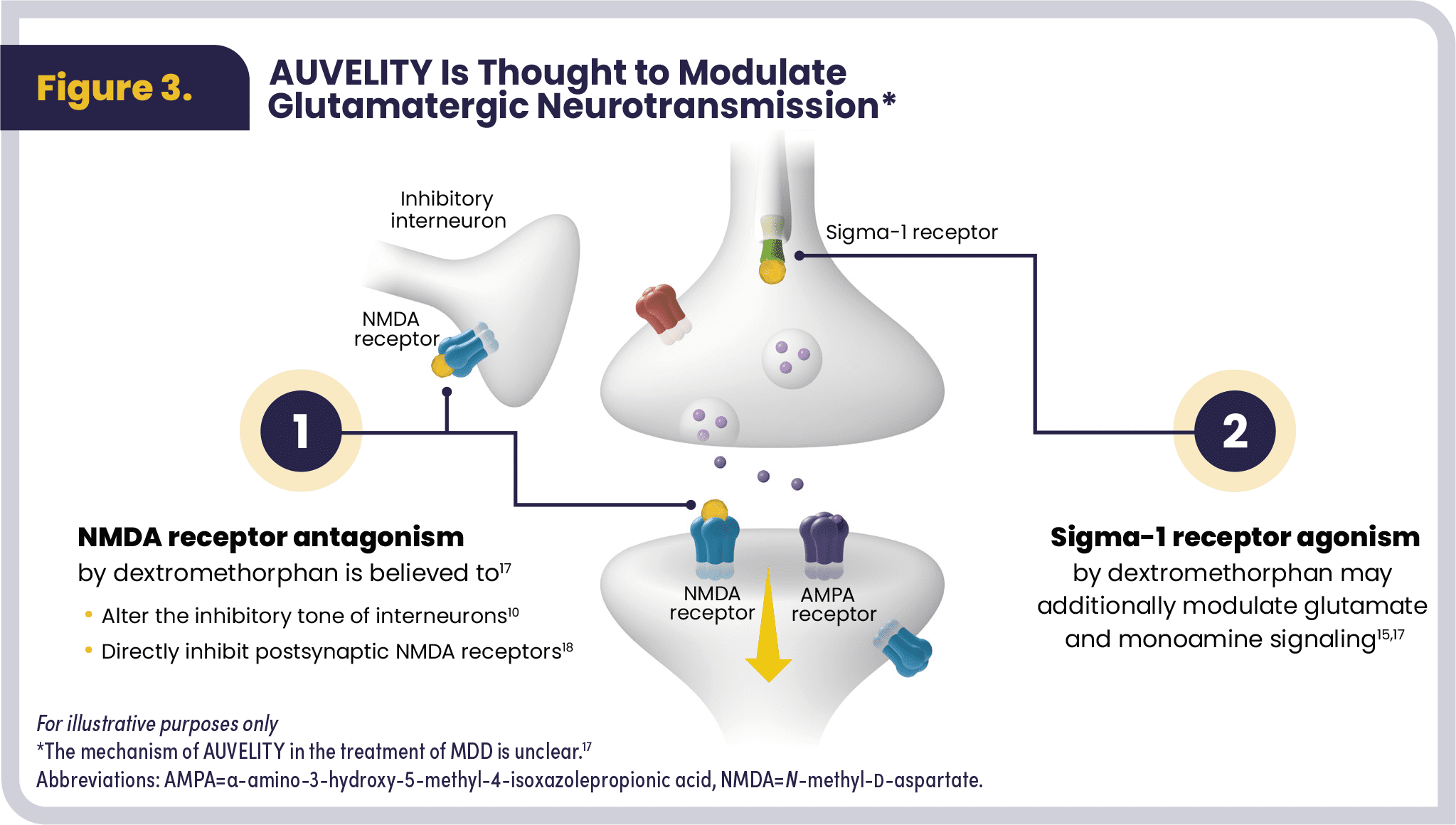
AUVELITY is an antidepressant with multimodal activity and is the only antidepressant that modulates both glutamatergic and monoaminergic pathways. AUVELITY is comprised of dextromethorphan and bupropion (see Figure 2).17,18 The exact mechanism of action of AUVELITY is unclear. Dextromethorphan is thought to act as an uncompetitive NMDA receptor antagonist that modulates glutamate signaling by altering the inhibitory tone of interneurons and by direct action on the postsynaptic NMDA receptor. Bupropion is a CYP2D6 inhibitor that increases and prolongs plasma concentrations of dextromethorphan. Bupropion is also a relatively weak inhibitor of norepinephrine and dopamine reuptake. Sigma-1 receptor agonism may additionally modulate glutamate and monoamine signaling (see Figure 3).16–19
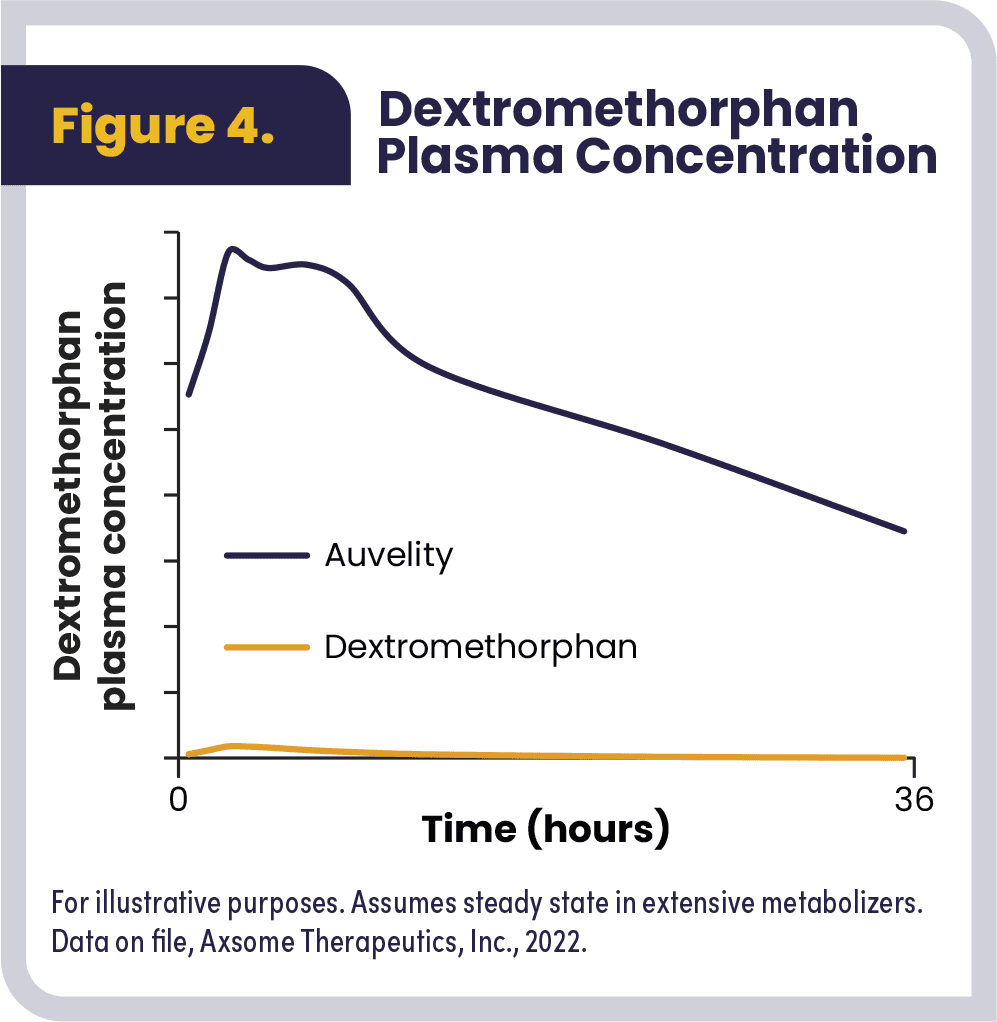
Dextromethorphan has low oral bioavailability due to its rapid and extensive metabolism by the cytochrome P450 (CYP) 2D6 liver enzyme. Dextromethorphan, when co-administered with bupropion, displays nonlinear pharmacokinetics, achieving steady-state plasma concentrations within 8 days. The accumulation ratios for dextromethorphan at steady state when given as AUVELITY are 20 and 32, respectively, based on Cmax and AUC0-12, compared to 1.3 and 1.4, respectively, for dextromethorphan alone (Figure 4).
Clinical Program Overview
The efficacy of AUVELITY was demonstrated in two clinical trials: the 6-week randomized, active-controlled, phase 2 ASCEND trial and the 6-week randomized, placebo-controlled, phase 3 GEMINI trial. The safety of AUVELITY was further evaluated in the phase 3, open-label, long-term COMET trial. AUVELITY was approved by the Food and Drug Administration (FDA) in August 2022.18,20–22
The ASCEND and GEMINI trials evaluated:20,21
- Patients aged 18 to 65 years who met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for current MDD without psychotic features
- Patients whose Montgomery-Åsberg Depression Rating Scale (MADRS) total score was ≥25 at baseline
- Patients whose Clinical Global Impressions-Severity (CGI-S) score was ≥4 at baseline
Patients were excluded from the ASCEND and GEMINI trials who:20,21
- Had a current or history of bipolar disorder, panic disorder, obsessive-compulsive disorder (OCD), psychotic disorder
- Had alcohol/substance abuse disorder within the past year
- Had a clinically significant risk of suicide
- Had a history of seizure disorder
- Were diagnosed with treatment-resistant depression
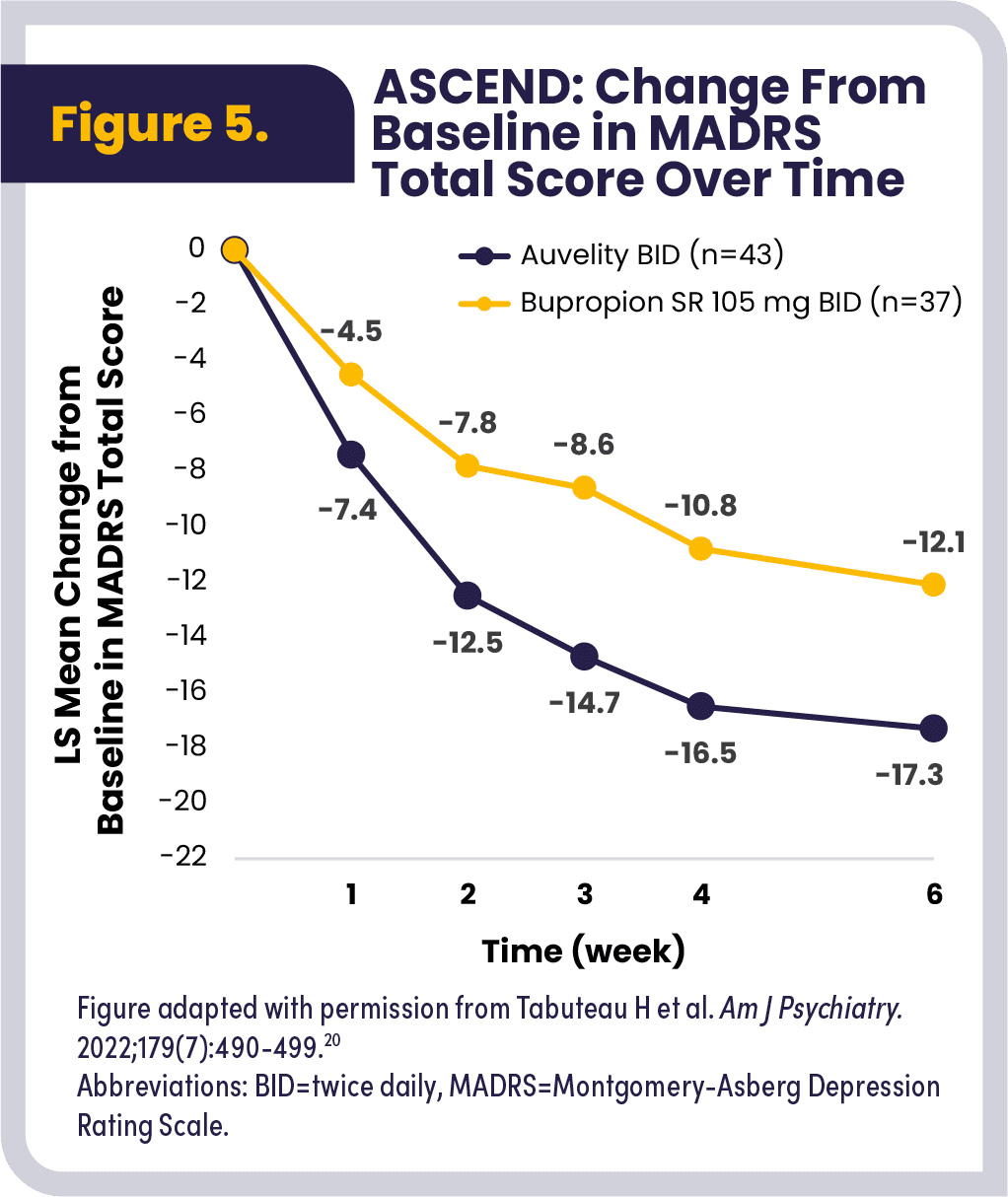
The phase 2 ASCEND trial evaluated the efficacy and safety of AUVELITY compared to 105 mg bupropion SR given BID as a control arm in 80 patients diagnosed with moderate to severe MDD.* Overall symptom improvement on the MADRS total score (primary endpoint) was assessed by averaging the change from baseline at each time point (Weeks 1–6). AUVELITY demonstrated statistically significant overall symptom improvement over 6 weeks. The overall LS mean change from baseline in the MADRS total score compared to bupropion SR 105 mg was -13.7 vs. -8.8 (P<.001).20
ASCEND also looked at the weekly mean change in MADRS total score from baseline over the 6-week treatment period (Figure 5). Approximately three times more patients achieved protocol-defined remission (MADRS total score ≤10) with AUVELITY compared with bupropion at Week 6 (47% vs 16%, respectively).20
Rapid and Sustained Efficacy
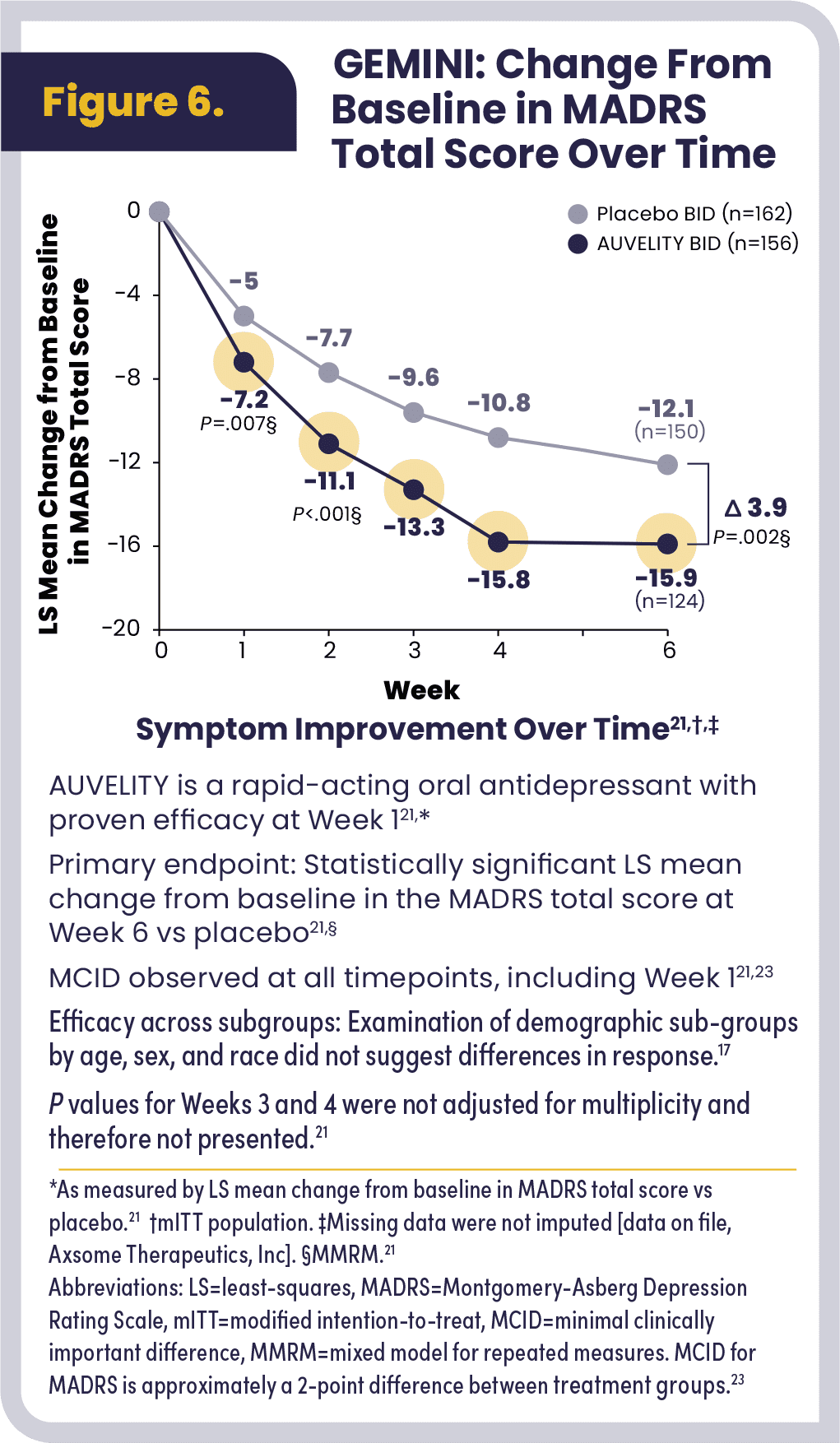
The GEMINI trial evaluated the efficacy and safety of AUVELITY compared to placebo in 327 patients diagnosed with moderate to severe MDD. The primary endpoint was LS mean change from baseline in MADRS total score at Week 6. AUVELITY demonstrated statistically significant symptom improvement as early as Week 1 and continued at Week 2 and Week 6 of therapy, compared to placebo (Figure 6). A change in MADRS of approximately 2 points is generally accepted as a minimal clinically important difference (MCID) for this endpoint.23 The MCID between active treatment and placebo was observed at all timepoints, with a 2.2 difference in MADRS at Week 1 and an increase to a 3.9 difference in MADRS by Week 6 between treatment groups (not an endpoint in the GEMINI trial).21
- Week 1: -7.2 in MADRS total score with AUVELITY compared to -5.0 with placebo (P=.007).
- Week 6: -15.9 with AUVELITY compared to -12.1 with placebo (P=.002).
- Week 1: twice as many patients taking AUVELITY achieved protocol-defined response of ≥50% improvement in MADRS total score from baseline compared to placebo (15% vs 7%, respectively).
- Week 6: 54% of patients taking AUVELITY achieved protocol-defined response, compared to 34% receiving placebo (P<.001).
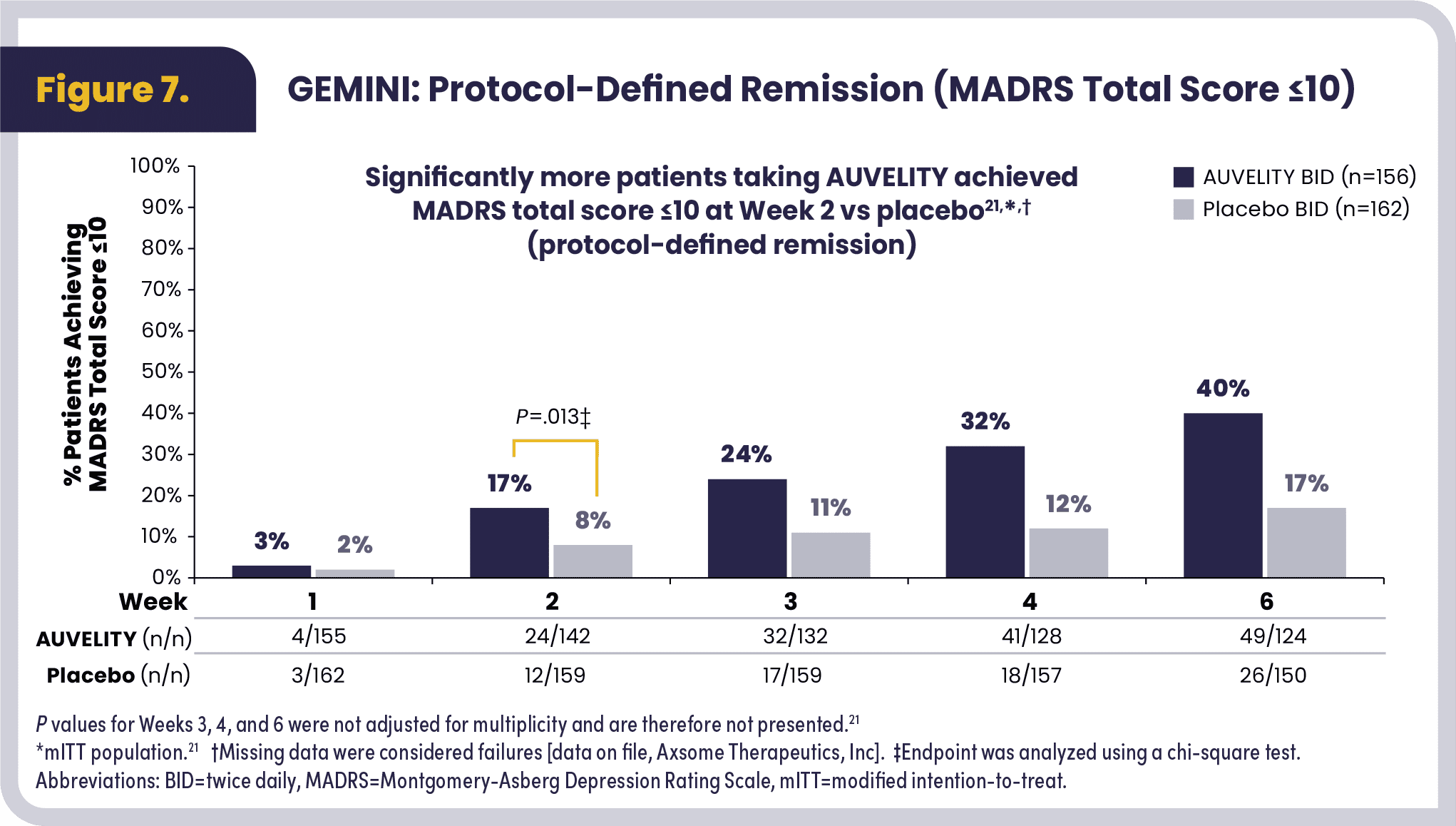
Moreover, 17% of patients taking AUVELITY achieved protocol-defined remission (MADRS total score ≤10) at Week 2 compared to 8% in the placebo cohort (P=.013), with the percentage increasing to 40% with AUVELITY and 17% with placebo at Week 6 (Figure 7).
Significantly more patients taking AUVELITY reported symptoms that were very much improved or much improved at Week 1 versus placebo using the Clinical Global Impression-Improvement (CGI-I) scale (22% vs 13%, respectively; P=.035). This increase was sustained at Week 6, with 58% of patients with AUVELITY having symptom improvement on the CGI-I scale compared to 43% with placebo (P=.016).21
A post hoc analysis of GEMINI assessed the anhedonic features in patients with moderate to severe MDD. The MADRS anhedonia scale includes 5 items: apparent sadness, reported sadness, concentration difficulties, lassitude, and inability to feel. In the GEMINI trial, baseline MADRS anhedonia scores were 19.8 in patients randomized to receive AUVELITY and 19.6 in patients randomized to receive placebo. At Week 1 and Week 6, 20.6% and 54.4% of patients on AUVELITY achieved response based on a ≥50% reduction in MADRS anhedonia subscale, compared to 7.4% and 36.0% of patients on placebo, respectively.24
Improvement in Scores Measuring Patient-Reported Functional and Quality of Life Outcomes
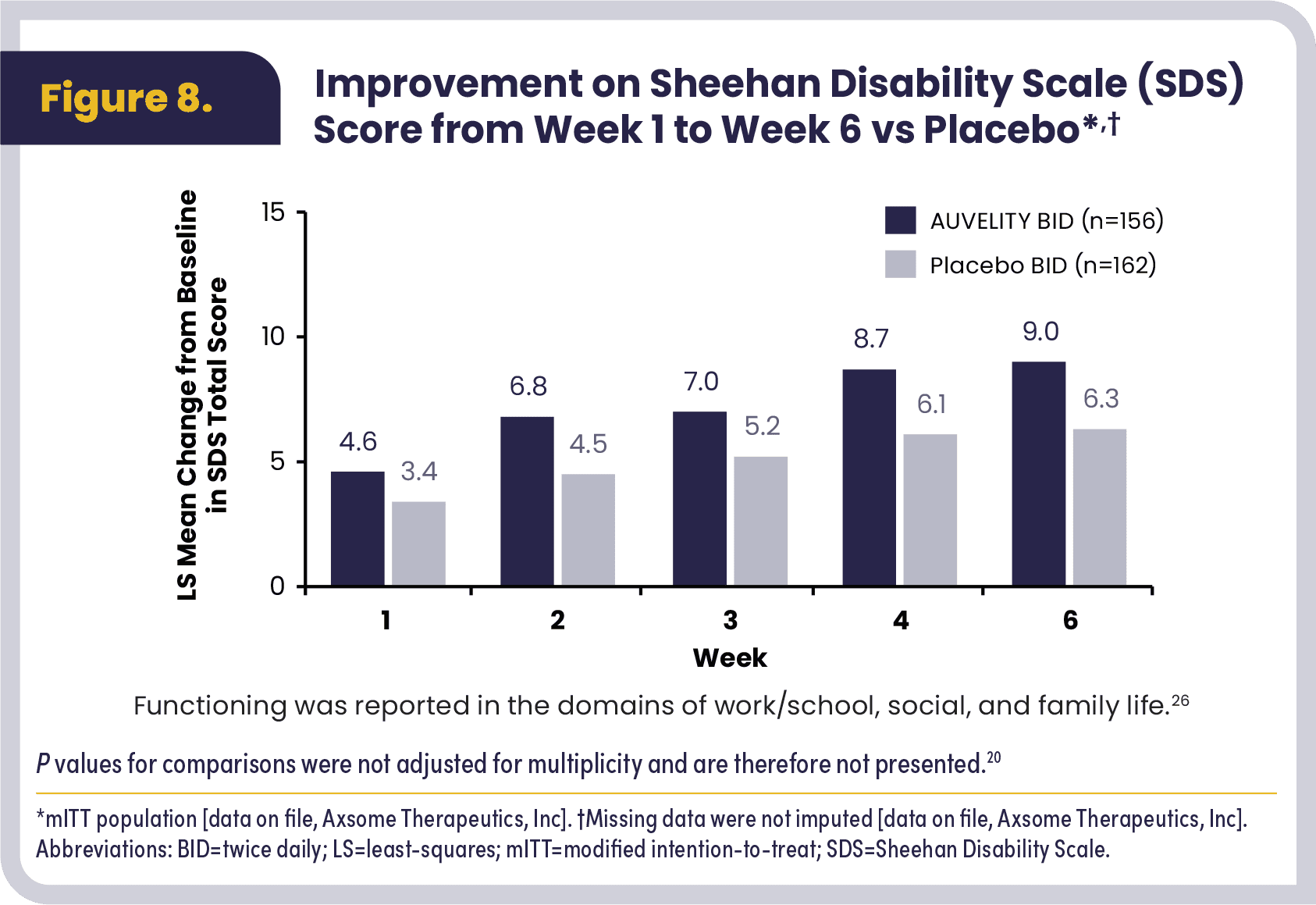
AUVELITY was associated with changes in scores that measure quality of life, depressive symptoms, and functionality, as assessed by patient-reported outcome measures. Patient-reported outcome measures were evaluated at Weeks 1, 2, 3, 4 and 6 of treatment with AUVELITY and placebo in the GEMINI study.21
Improvement in functional assessment scores using Sheehan Disability Scale (SDS), a well-validated, short, patient-reported scale assessing functional impairment in work or school, family life, and social life, with total scores ranging from 0 to 30, was seen at Week 1 to Week 6. At Week 6, LS mean change from baseline was 9.0 in patients receiving AUVELITY compared to a 6.3 in the placebo cohort. (Figure 8).21,25
Improved scores on the Quality of Life Enjoyment and Satisfaction Questionnaire Short Form (Q-LES-Q-SF), a self-report tool designed to measure the degree of enjoyment and satisfaction experienced in various areas of daily functioning, showed a 19.8 LS mean change from baseline with AUVELITY compared to 14.4 with placebo at Week 6.21,27 A decrease in depressive symptom severity scores was seen starting at Week 1 and continued through Week 6, showing a -7.7 LS mean change from baseline in Quick Inventory of Depressive Symptomatology-Self-Rated (QIDS-SR-16) compared with -5.7 with placebo at Week 6. Moreover, 47% of patients receiving AUVELITY reported being very much/much improved compared to 31% receiving placebo on the Patient Global Impression of Improvement (PGI-I) at Week 6.21
Safety and Tolerability
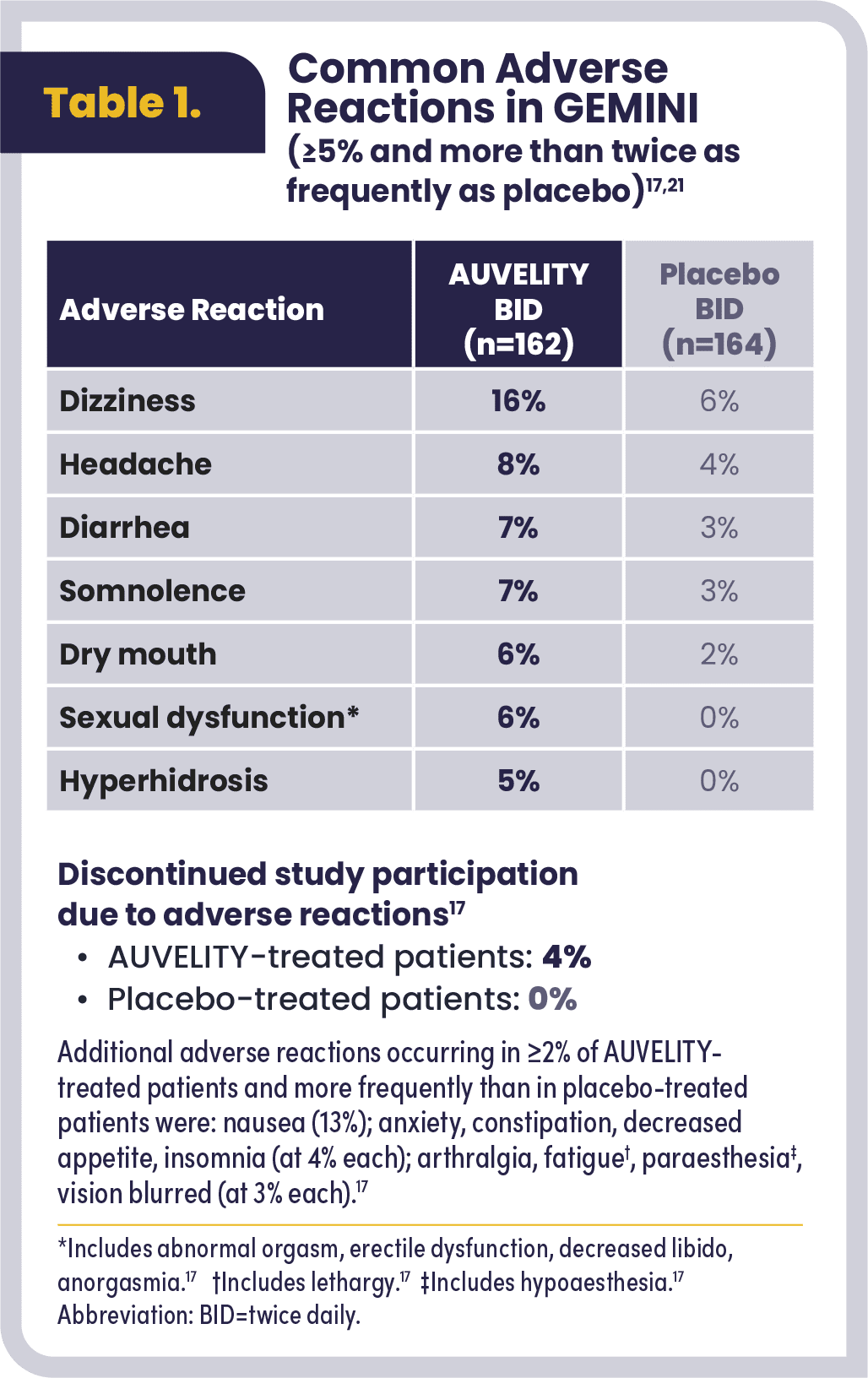
AUVELITY was evaluated for safety in over 1100 patients with MDD at the time of approval. A total of 1114 patients were evaluated from four clinical studies (two 6-week studies in MDD, one 6-week study in another indication, and one long-term study in MDD and another indication17). Overall, the GEMINI trial showed 62% of patients receiving AUVELITY experienced any adverse event compared to 45% receiving placebo. The most common adverse reactions (≥ 5% and more than twice as frequently as placebo) include dizziness, headache, diarrhea, somnolence, dry mouth, sexual dysfunction, and hyperhidrosis (Table 117).21
Four percent of AUVELITY-treated patients discontinued study participation due to an adverse event compared to 0% of placebo-treated patients.17 At Week 6, AUVELITY was associated with a 0.44 lb weight loss compared to a 0.88 lb weight gain in placebo-treated patients.21
Contraindications to taking AUVELITY include:
- Seizure disorder
- Current or prior diagnosis of bulimia or anorexia nervosa
- Undergoing abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs
- Use with an MAOI or within 14 days of stopping treatment with AUVELITY. Do not use AUVELITY within 14 days of discontinuing an MAOI
- Known hypersensitivity to bupropion, dextromethorphan, or any component of AUVELITY
Long-Term Safety and Efficacy
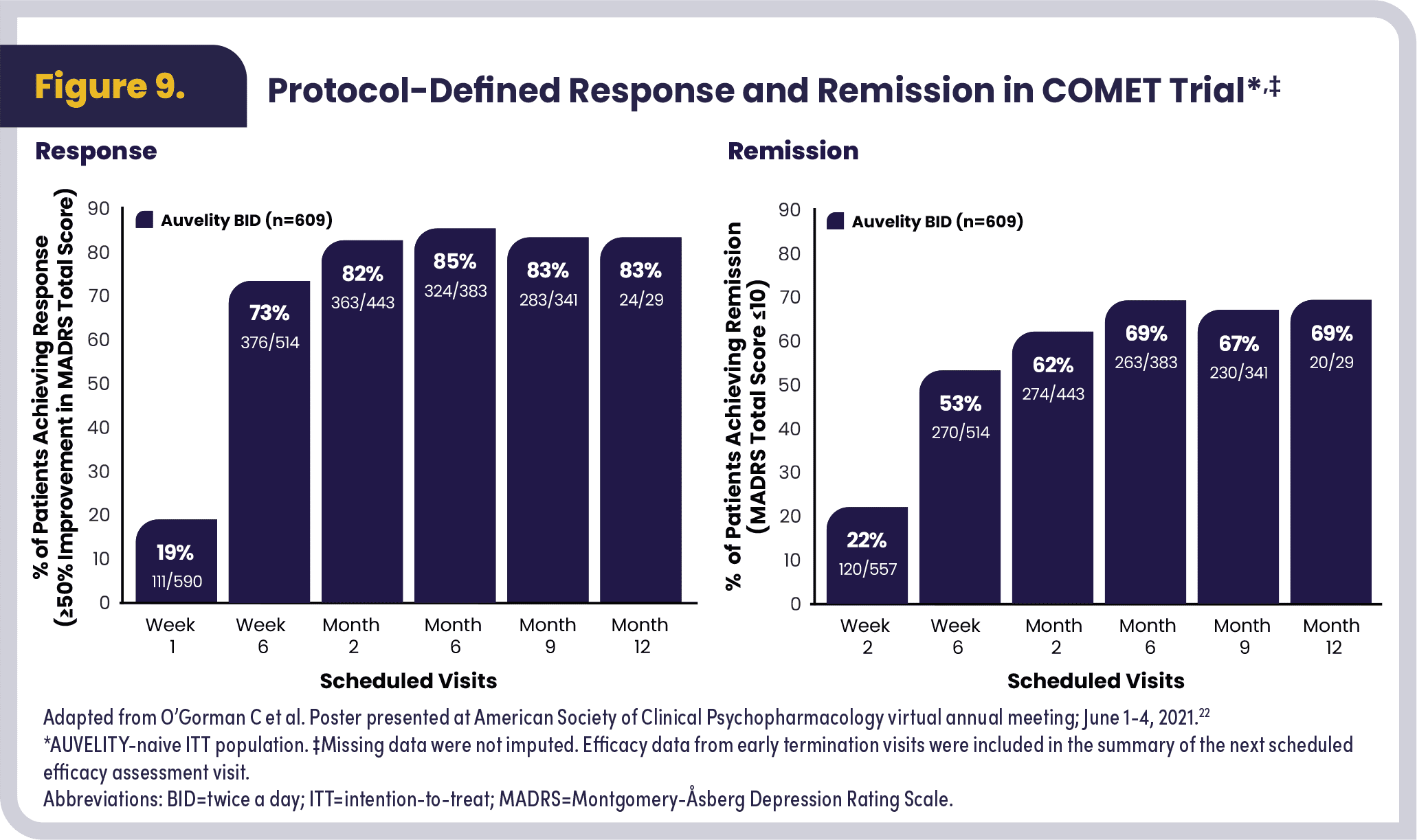
COMET was a phase 3, open-label, long-term trial evaluating the safety and efficacy of AUVELITY in 876 patients with moderate to severe MDD.22 COMET evaluated the efficacy results of 611 newly enrolled patients by MADRS total score change from baseline, MADRS response, remission up to 1 year, CGI-I, and SDS response in functioning. COMET also included 265 patients rolled over from prior controlled trials with AUVELITY. All newly enrolled patients were assessed for efficacy through Week 6, and only patients whose MADRS scores improved by ≥25% were eligible to continue in the study. Approximately 6% of patients met discontinuation criteria at Week 6. AUVELITY was generally well-tolerated in the long-term study; 8.4% of patients discontinued the study due to adverse events. The most common adverse events resulting in discontinuation were dizziness (1.3%), nausea (1.1%), and headache (1.0%). There was a mean decrease in MADRS total score of -9.1 at Week 1 and -21.1 at Week 6. The MADRS total score reductions were sustained from Week 6 through Month 12. COMET showed an increase in patients who achieved clinical response (≥50% improvement in MADRS) over time, with 19% (n=590) at Week 1, 73% (n=514) at Week 6, and 83% (n=29) at Month 12. There was an increase in patients who achieved remission (MADRS total score ≤10) over time, with 53% at Week 6 and 69% at Month 12 (Figure 9).22
Dosing and Administration
AUVELITY is an oral antidepressant treatment available in one dosage strength with a recommended therapeutic dose by day 4. Prior to starting therapy and during treatment with AUVELITY, it is important to assess blood pressure and monitor periodically during treatment; to screen patients for a personal or family history of bipolar disorder, mania, or hypomania; and to screen for current use of bupropion or dextromethorphan in other medications.17
The recommended starting dose of AUVELITY is 1 tablet (45 mg/105 mg dextromethorphan/bupropion) once daily in the morning. After 3 days, increase to 1 tablet twice daily, separated by at least 8 hours, which is the maximum recommended daily dose. Tablets should be swallowed whole and not crushed, divided, or chewed. AUVELITY can be taken with or without food.17
The recommended dosage of AUVELITY is reduced to 1 tablet by mouth daily in the morning17:
- In poor CYP2D6 metabolizers
- In moderate renal impairment
(eGFR 30 to 59 mL/minute/1.73 m2). - When co-administered with strong CYP2D6 inhibitors
AUVELITY has the following additional Warnings and Precautions17:
- Suicidal thoughts and behaviors in adolescents and young adults
- Seizure
- Increased blood pressure and hypertension
- Activation of mania or hypomania
- Psychosis and other neuropsychiatric reactions
- Angle-closure glaucoma
- Dizziness
- Serotonin syndrome
- Embryo-fetal toxicity
Summary
Glutamatergic dysfunction may play a key role in MDD, and glutamatergic modulation may offer an approach to treating MDD.7,19 AUVELITY exerts multimodal activity and is the only antidepressant for adults with MDD that modulates both glutamatergic and monoaminergic pathways.17,18 AUVELITY was evaluated for safety in 1114 patients from four clinical studies (two 6-week studies in MDD, one 6-week study in another indication, and one long-term study in MDD and another indication).17 In the 6-week randomized, placebo-controlled, phase 3 GEMINI trial, the most common adverse reactions were dizziness (16%), headache (8%), diarrhea (7%), somnolence (7%), dry mouth (6%), sexual dysfunction (6%), and hyperhidrosis (5%).17,21 Additional safety information for AUVELITY, including its contraindications, can be found in the Important Safety Information throughout this article and in the Prescribing Information. In the GEMINI trial, AUVELITY demonstrated efficacy at Week 1 and statistically significant LS mean change from baseline in the MADRS total score at Week 6 vs placebo (primary endpoint).21 In the COMET trial, a phase 3 open-label, long-term study evaluating safety and efficacy, there was a mean decrease in MADRS total score of -9.1 at Week 1 and -21.1 at Week 6. The MADRS total score reductions, on average, were sustained from Week 6 through Month 12. There was an increase in proportion of patients achieving protocol-defined remission, with 53% at Week 6 increasing to 69% at Month 6, and a comparable proportion maintaining remission at Month 12.22 AUVELITY is available in one dosage strength with a recommended therapeutic dose by day 4.17 The recommended starting dose of AUVELITY is one tablet (45 mg/105 mg dextromethorphan/bupropion) once daily in the morning. After 3 days, increase to one tablet twice daily, separated by at least 8 hours, which is the maximum recommended daily dose. Please refer to the Prescribing Information for more details on dosing and administration.17
*N=80 is the modified intention to treat (mITT) population. Patients without a confirmed diagnosis of moderate to severe MDD, as assessed by a blinded independent assessor, but who met all other entry criteria (n=17), were randomized for assessment of safety and were excluded from the efficacy population, as prespecified.
Go to https://www.axsome.com/auvelity-prescribing-information.pdf to view AUVELITY full Prescribing Information, including Boxed Warning for suicidal thoughts and behaviors.
References
- Habert J, Katzman MA, Oluboka OJ, et al. Functional Recovery in Major Depressive Disorder: Focus on Early Optimized Treatment. Prim Care Companion CNS Disord. 2016;18(5):10.4088/PCC.15r01926. Published 2016 Sep 1. https://doi.org/10.4088/PCC.15r01926
- Wagner S, Engel A, Engelmann J, et al. Early improvement as a resilience signal predicting later remission to antidepressant treatment in patients with major depressive disorder: Systematic review and meta-analysis. J Psychiatr Res. 2017;94:96–106. https://doi.org/10.1016/j.jpsychires.2017.07.003
- Arnaud A, Benner J, Suthoff E, et al. The impact of early remission on disease trajectory and patient outcomes in major depression disorder (MDD): A targeted literature review and microsimulation modeling approach based on the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. J Affect Disord. 2023;325:264–272. https://doi.org/10.1016/j.jad.2022.12.147
- Ciudad A, Álvarez E, Roca M, et al. Early response and remission as predictors of a good outcome of a major depressive episode at 12-month follow-up: A prospective, longitudinal, observational study. J Clin Psychiatry. 2012;73(2):185–191. https://doi.org/10.4088/JCP.10m06314
- Amidfar M, Woelfer M, Réus GZ, Quevedo J, Walter M, Kim YK. The role of NMDA receptor in neurobiology and treatment of major depressive disorder: Evidence from translational research. Prog Neuropsychopharmacol Biol Psychiatry. 2019;94:109668. https://doi.org/10.1016/j.pnpbp.2019.109668
- Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: An emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62(1):63–77. https://doi.org/10.1016/j.neuropharm.2011.07.036
- Murrough JW, Abdallah CG, Mathew SJ. Targeting glutamate signaling in depression: progress and prospects. Nat Rev Drug Discov. 2017;16(7):472–486. https://doi.org/10.1038/nrd.2017.16
- Gasiorowska A, Wydrych M, Drapich P, Zadrozny M, Steczkowska M, Niewiadomski W, Niewiadomska G. The Biology and Pathobiology of Glutamatergic, Cholinergic, and Dopaminergic Signaling in the Aging Brain. Front Aging Neurosci. 2021 Jul 13;13:654931 https://doi.org/10.3389/fnagi.2021.654931
- Chinta SJ, Andersen JK. Dopaminergic neurons. Int J Biochem Cell Biol. 2005 May;37(5):942-6. https://doi.org/10.1016/j.biocel.2004.09.009
- Duman RS, Aghajanian GK, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238–249. https://doi.org/10.1038/nm.4050
- Reiner A, Levitz J. Glutamatergic Signaling in the Central Nervous System: Ionotropic and Metabotropic Receptors in Concert. Neuron. 2018 Jun 27;98(6):1080-1098. https://doi.org/10.1016/j.neuron.2018.05.018
- Auer DP, Pütz B, Kraft E, et al. Reduced glutamate in the anterior cingulate cortex in depression: An in vivo proton magnetic resonance spectroscopy study. Biological Psychiatry. 2000;47(4):305-313. https://doi.org/10.1016/S0006-3223(99)00159-6
- Hasler G, van der Veen JW, Tumonis T, et al. Reduced prefrontal glutamate/glutamine and γ-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Archives of General Psychiatry. 2007;64(2):193-200. https://doi.org/10.1001/archpsyc.64.2.193
- Lener MS, Niciu MJ, Ballard ED, et al. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry. 2017 May 15;81(10):886-897.15. https://doi.org/10.1016/j.biopsych.2016.05.005
- Yang K, Wang C, Sun T. The roles of intracellular chaperone proteins, sigma receptors, in Parkinson’s disease (PD) and major depressive disorder (MDD). Front Pharmacol. 2019;10:528. Published 2019 May 21. https://doi.org/10.3389/fphar.2019.00528
- Ren P, Wang J, Li N, et al. Sigma-1 receptors in depression: Mechanism and therapeutic development. Front Pharmacol. 2022;13:925879. https://doi.org/10.3389/fphar.2022.925879
- AUVELITY®. Full prescribing information. Axsome Therapeutics, Inc; 2024.
- Stahl SM. Dextromethorphan/bupropion: A novel oral NMDA (N-methyl-D-aspartate) receptor antagonist with multimodal activity. CNS Spectr. 2019;24(5):461–466. https://doi.org/10.1017/S1092852919001470
- Duman RS, Sanacora G, Krystal JH. Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron. 2019;102(1):75–90. https://doi.org/10.1016/j.neuron.2019.03.013
- Tabuteau H, Jones A, Anderson A, et al. Effect of AXS-05 (dextromethorphan-bupropion) in major depressive disorder: A randomized double-blind controlled trial. Am J Psychiatry. 2022;179(7):490–499. https://doi.org/10.1176/appi.ajp.21080800
- Iosifescu DV, Jones A, O’Gorman C, et al. Efficacy and safety of AXS-05 (dextromethorphan-bupropion) in patients with major depressive disorder: A phase 3 randomized clinical trial (GEMINI). J Clin Psychiatry. 2022;83(4). https://doi.org/10.4088/JCP.21m14345
- O’Gorman C, Jones A, Tabuteau H. Sustained efficacy with long-term treatment with AXS-05: Results from the COMET phase 3 trial, a long-term, open-label study evaluating the efficacy and safety of AXS-05 for the treatment of MDD. Poster presented at: American Society of Clinical Psychopharmacology: virtual annual meeting; June 1-4, 2021.
- Duru G, Fantino B. The clinical relevance of changes in the Montgomery-Asberg Depression Rating Scale using the minimum clinically important difference approach. Curr Med Res Opin. 2008;24(5):1329–1335. https://doi.org/10.1185/030079908×291958
- Jones A, McIntyre RS, Jacobsen M, et al. Impact of AXS-05 (dextromethorphan-bupropion), an oral NMDA receptor antagonist, on anhedonic symptoms in major depressive disorder. CNS Spectr. 2023;28(2):264. https://doi.org/10.1017/S1092852923002171
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol. 1996;11(Suppl 3):89–95.
- Sheehan DV, Nakagome K, Asami Y, et al. Restoring function in major depressive disorder: A systematic review. J Affect Disord. 2017;215:299-313. https://doi.org/10.1016/j.jad.2017.02.029
- Endicott J, Nee J, Harrison W, et al. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull. 1993;29(2):321–326.
The Savings Card provides instant access for your patients with no registration or activation needed.*
To download a PDF of the Savings Card, visit AUVELITY.com/Card
For questions about eligibility criteria, call: 800-641-4654
*Subject to eligibility.