Abstract
Objective: To further characterize the safety and tolerability of oral xanomeline and trospium chloride in the treatment of people with schizophrenia experiencing acute psychosis.
Methods: Pooled analyses were performed on safety data from the 5-week, randomized, double-blind, placebo-controlled, inpatient EMERGENT-1, EMERGENT-2, and EMERGENT-3 trials of xanomeline/ trospium in adults with schizophrenia with a recent worsening of psychosis requiring hospitalization. Adverse events (AEs) including extrapyramidal motor symptoms (EPS), vital signs, and clinical laboratory values were monitored. Additional analyses of AEs were conducted on subgroups based on age (<45 years or ≥45 years), sex, race (Black or White), ethnicity (Hispanic/Latino or not Hispanic/ Latino), country (United States or Ukraine), and baseline body mass index (<30 kg/m2 or ≥30 kg/m2).
Results: The pooled safety population comprised 683 participants from the acute trials. Discontinuation rates were similar between groups (xanomeline/ trospium, 27.6%; placebo, 22.7%). Treatment-emergent AEs were reported by 67.9% (xanomeline/trospium) and 51.3% (placebo) of participants, and 51.8% (xanomeline/trospium) and 29.4% (placebo) experienced AEs deemed related to treatment. The most common AEs with xanomeline/trospium were mild or moderate in intensity, transient, and generally gastrointestinal in nature. Subgroups demonstrated clinically nonsignificant differences in incidences of the most common AEs. Rates of EPS, somnolence, and weight gain were low in both groups.
Conclusions: In pooled analyses, xanomeline/trospium was generally well tolerated in people with schizophrenia. The most common AEs were mild or moderate in intensity, transient, and consistent with the activity of xanomeline and trospium at muscarinic receptors. Rates of EPS, somnolence, and weight gain were low.
Trial Registration: ClinicalTrials.gov identifiers: NCT03697252, NCT04659161, NCT04738123.
J Clin Psychiatry 2025;86(1):24m15497
Author affiliations are listed at the end of this article.
See commentary by Citrome
Treatments for schizophrenia have relied on dopamine receptor blockade since the introduction of antipsychotics 70 years ago, and all available antipsychotics are either direct or functional antagonists of D2 dopamine receptors.1 However, these therapies exhibit tolerability deficits that, in conjunction with efficacy limitations, result in insufficiently managed symptoms and continued disability for many people treated with antipsychotics.1,2 Side effects also contribute to a nonadherence rate of nearly 50% in patients with schizophrenia and a resulting increased risk of relapse.3–5 Extrapyramidal motor symptoms such as akathisia, dystonia, and parkinsonism are among the most common side effects of antipsychotics.6 These often serious, involuntary movement disorders typically manifest shortly after treatment commences and may persist beyond discontinuation.7 Approximately 50% and 22% of people treated with first- and second-generation antipsychotics, respectively, develop extrapyramidal motor symptoms, which are a source of stigma, reduced quality of life, and poor adherence.7–10 Anticholinergic agents can alleviate treatment-related motor disorders but are associated with their own problematic adverse effects, such as blurred vision and urinary retention.11 Weight gain is another troubling side effect that impacts up to 72% of people using antipsychotics and is typically observed within weeks after initiating treatment.12,13 Weight gain increases the risk of cardiovascular morbidity and reduces quality of life for people on treatment.9,12,14 Additional side effects such as metabolic disturbances, tardive dyskinesia, and somnolence/sedation further contribute to disease burden.6,11,15 Effective therapies with better safety and tolerability profiles are a major unmet need for people living with schizophrenia.
Increasing evidence supports the role of muscarinic acetylcholine receptors as potential therapeutic targets in psychosis. Xanomeline is a preferential M1 and M4 muscarinic receptor agonist that has demonstrated antipsychotic properties in placebo-controlled clinical trials of Alzheimer’s disease and schizophrenia.16–18 Notably, xanomeline improved symptoms of psychosis without eliciting the side effects associated with current antipsychotics16,17; however, treatment resulted in gastrointestinal and cardiovascular side effects, including orthostasis and syncope, and development of xanomeline monotherapy was halted.1
Xanomeline is combined with the peripherally restricted muscarinic receptor antagonist trospium chloride with the goal of reducing side effects resulting from xanomeline activation of peripheral muscarinic receptors while leaving the centrally mediated effects of xanomeline intact, and was recently approved for the treatment of schizophrenia in adults by the U.S. Food and Drug Administration. Xanomeline/trospium efficacy and safety have been demonstrated in acutely symptomatic adults with schizophrenia in the acute EMERGENT-1 (NCT03697252),19 EMERGENT-2 (NCT04659161),20 and EMERGENT-3 (NCT04738123)21 trials. All 3 trials met the prespecified primary endpoint of change from baseline to week 5 in Positive and Negative Syndrome Scale (PANSS) total score. Xanomeline/trospium was also favored in most secondary outcome measures and generally well tolerated.19–22 The most common side effects were primarily gastrointestinal disorders related to the activity of xanomeline and trospium at peripheral muscarinic receptors, including nausea, vomiting, constipation, dyspepsia, and dry mouth, were mild or moderate in intensity, and were typically transient.
The nearly identical designs of the EMERGENT trials provide an opportunity to pool data and assess xanomeline/trospium safety and tolerability with the increased statistical power afforded by a larger population and to potentially identify rare events that did not meet clinically meaningful thresholds in the individual trials.23 Here, we further characterize the side effect profile of xanomeline/trospium in data pooled from the acute trials and assess the impact of treatment on adverse events (AEs) associated with available antipsychotics, including extrapyramidal motor symptoms, somnolence, and weight increase. In addition, the pooled analysis provides sufficient statistical power to examine safety in demographic and baseline characteristic subgroups.
METHODS
Trial Design
The acute EMERGENT-1, EMERGENT-2, and EMERGENT-3 trials were 5-week, randomized, double blind, placebo-controlled inpatient trials of xanomeline/ trospium in adults with schizophrenia.19–21 Study design details have been published previously. In brief, eligible participants were adults aged 18–60 (EMERGENT-1) or 18–65 (EMERGENT-2 and EMERGENT-3) years experiencing acute exacerbation of psychotic symptoms. Participants were randomized 1:1 to receive xanomeline/trospium or placebo twice daily for 5 weeks following a 7- to 14-day screening period to provide time for washout of prior antipsychotics; continued administration of as-needed anxiolytics was permitted. The flexible dosing schedule for xanomeline/trospium started at a dose of twice-daily 50-mg xanomeline/20- mg trospium and increased to a maximum of twice-daily 125-mg xanomeline/30-mg trospium by the end of the first week based on tolerability at the investigator’s discretion. Trials ran from September 2018 to December 2022 and enrolled participants at 30 sites in the United States (EMERGENT-1, EMERGENT-2, and EMERGENT-3) and 12 in Ukraine (EMERGENT-3 only).24–26
Centralized institutional review boards approved all protocols for the acute trials, which were conducted in accordance with the principles of the Declaration of Helsinki, the International Council of Harmonization guidelines for Good Clinical Practice, and the relevant regulations in the countries in which the research was conducted. Participants submitted written informed consent prior to enrollment. Trials adhered to Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Trial Population
Enrolled adults were required to have a primary diagnosis of schizophrenia, exacerbation of psychotic symptoms requiring hospitalization within 2 months of screening, baseline PANSS total score between 80 and 120 (inclusive), a score of ≥4 on at least 2 out of 4 PANSS positive scale items, and a Clinical Global Impression Severity score of ≥4. Exclusion criteria included a primary diagnosis other than schizophrenia in the year prior to screening, cases of first-episode psychosis, and a history of resistance to antipsychotic treatment.
Safety Assessments
Treatment-emergent AEs (TEAEs) were defined as events that began after the administration of the trial medication. Treatment-related AEs were defined as events the investigator considered possibly, probably, or definitely related to trial medication and were assessed at each visit. Weight, vital signs, and clinical laboratory values were measured at baseline and on the first day of treatment to the time of trial discharge on day 35. Vital signs were recorded 2 hours after the morning dose at each postbaseline visit to correspond with maximum concentration (Cmax) and included both seated and standing (after 2 minutes) measurements to assess orthostatic change. Participants were assessed for treatment-induced movement disorders using the Simpson-Angus Scale (SAS) to measure extrapyramidal symptoms (range, 0–40; higher scores reflect more severe drug-induced parkinsonian symptoms)27; the Barnes Akathisia Rating Scale (BARS) to assess akathisia (range, 0–14; higher scores reflect more severe symptoms)28; and the Abnormal Involuntary Movement Scale (AIMS) to assess tardive dyskinesia (TD) risk (range, 0–28; rating of ≥2 indicates evidence of TD).29 Movement scale assessments occurred on the first and last days of treatment in the EMERGENT-1 trial and at baseline and weekly during the treatment period in the EMERGENT-2 and EMERGENT-3 trials. In addition, the incidence of extrapyramidal motor symptoms was evaluated as any TEAE with a preferred term of dystonia, dyskinesia, akathisia, or extrapyramidal disorder. Data on suicide risk as measured with the Columbia Suicide Severity Rating Scale were generally unremarkable and will be addressed in future publications. Safety data were summarized descriptively by treatment group; no formal hypothesis testing was performed on safety data.
Statistical Analyses
Post hoc safety analyses were performed in the safety population, defined as all participants who received ≥1 dose of trial medication. Demographic and baseline characteristics were summarized for the safety population using descriptive statistics. For change from baseline measurements, baseline was defined as the most recent measurement prior to the first administration of trial medication. Data listings, summaries, and statistical analyses were generated using SAS® software version 9.4 or higher (Cary, NC).
Pooling data from the acute trials yielded a population large enough to accommodate analysis of safety in participant subgroups. For these analyses, incidence of TEAEs was analyzed based on the following baseline and demographic criteria: age based on the trial population median (<45 years or ≥45 years), sex, race (black or white), ethnicity (Hispanic/Latino or not Hispanic/Latino), country (United States or Ukraine), and baseline body mass index (BMI; <30 kg/m2 or ≥30 kg/m2).
RESULTS
Participants
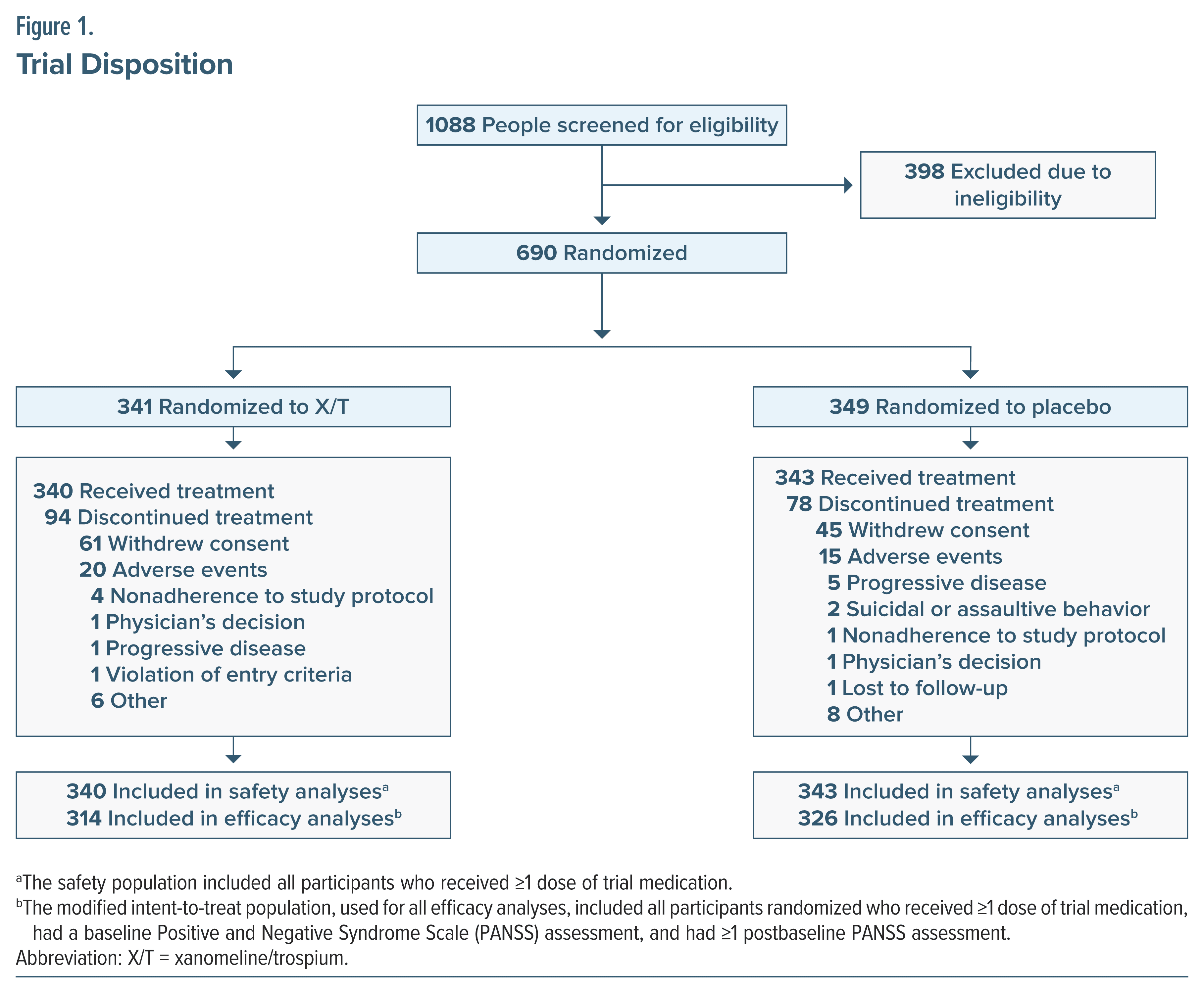
Across the EMERGENT trials, a total of 1,088 people were screened, and 690 individuals were randomized to receive xanomeline/trospium (n = 341) or placebo (n = 349) (Figure 1). The safety population included 340 participants in the xanomeline/trospium arm and 343 people in the placebo arm. Across treatment groups, 88.9% of participants had been treated with at least 1 prior antipsychotic. Overall, 25.2% of participants discontinued the trial early, including 27.6% in the xanomeline/trospium group and 22.7% in the placebo group. The most common reasons for discontinuation were withdrawal of consent (xanomeline/trospium, 17.9%; placebo, 13.1%) followed by AEs (xanomeline/ trospium, 5.9%; placebo, 4.4%). Among participants who received xanomeline/trospium, TEAEs leading to discontinuation in ≥2 participants were gastrointestinal (nausea, 1.5%; vomiting, 0.9%; and gastroesophageal reflux disease, 0.6%) whereas TEAEs leading to discontinuation in ≥2 participants in the placebo arm were psychiatric (schizophrenia, 2.3%; psychosis, 1.2%; and agitation, 0.6%).
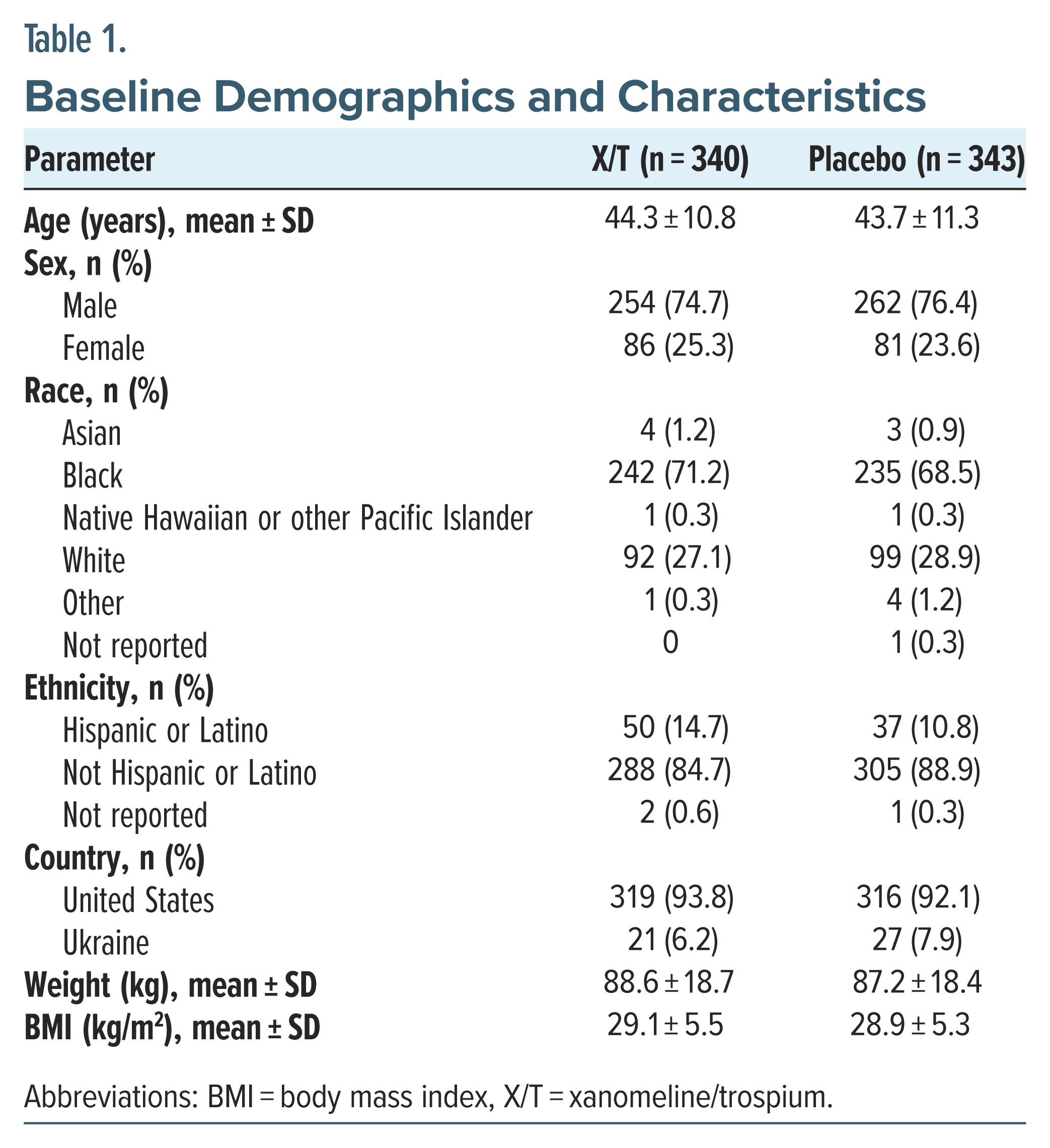
Baseline demographics and characteristics were largely consistent across the treatment groups (Table 1). Mean participant ages were 44.3 years (xanomeline/ trospium) and 43.7 years (placebo). Most participants were male (xanomeline/trospium, 74.7%; placebo, 76.4%) and Black (xanomeline/trospium, 71.2%; placebo, 68.5%) or White (xanomeline/trospium, 27.1%; placebo, 28.9%). A minority of each treatment arm comprised individuals from Ukraine (xanomeline/trospium, 6.2%; placebo, 7.9%). Mean weight and BMI were similar between treatment groups.
Treatment-Emergent Adverse Events
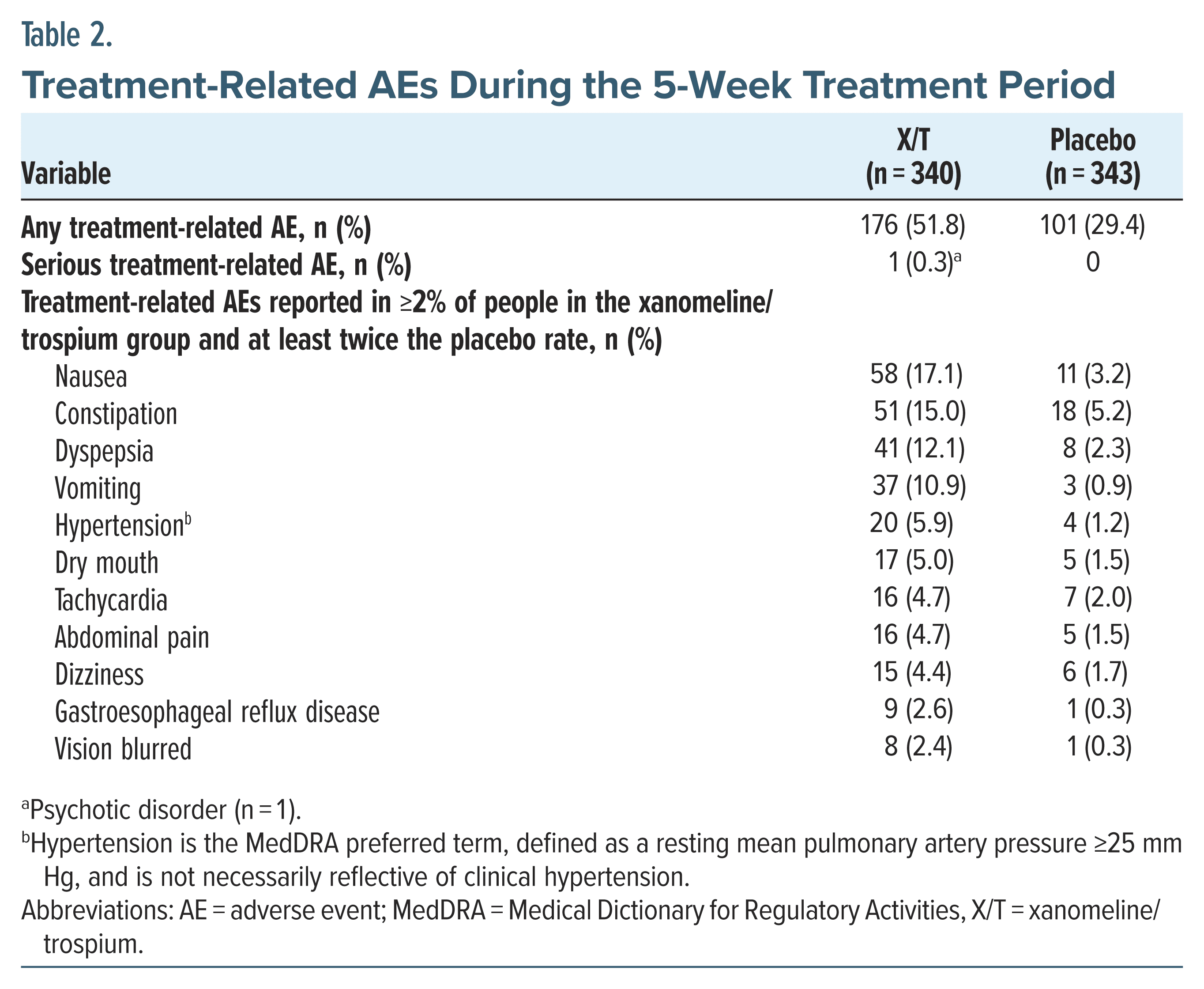
A total of 67.9% and 51.3% of people in the xanomeline/trospium and placebo arms, respectively, experienced ≥1 TEAE. TEAE rates in the xanomeline/ trospium group peaked early in the trial with a high of 28.8% of participants experiencing a cholinergic TEAE on day 7, declining to 16.8% by the last day of treatment (Supplementary Figure 1). The most common TEAEs (occurring in ≥5% of participants in the xanomeline/ trospium arm) were nausea (xanomeline/trospium vs placebo: 18.5% vs 3.8%; risk difference, 14.7%; 95% confidence interval [CI], 10.2 to 19.5), constipation (17.1% vs 6.1%; risk difference, 10.9%; 95% CI, 6.2 to 15.8), dyspepsia (15.9% vs 4.7%; risk difference, 11.2%; 95% CI, 6.8 to 15.8), vomiting (13.5% vs 1.7%; risk difference, 11.8; 95% CI, 7.8 to 15.9), headache (10.9% vs 10.5%; risk difference, 0.4; 95% CI, −4.3 to 5.1), hypertension (8.5% vs 1.7%; risk difference, 6.8%; 95% CI, 3.6 to 10.4), abdominal pain (5.9% vs 2.9%; risk difference, 3.0%; 95% CI, −0.2 to 6.3), somnolence (5.3% vs 4.4%; risk difference, 0.9%; 95% CI, −2.4 to 4.3), dry mouth (5.0% vs 1.5%; risk difference, 3.5%; 95% CI, 0.9 to 6.5), and tachycardia (5.0% vs 2.3%; risk difference, 2.7%; 95% CI, −0.2 to 5.8); all were mild or moderate in intensity (Supplementary Table 1). Most of the commonly reported TEAEs occurring within the first week of xanomeline/trospium administration resolved by the end of treatment, and cholinergic TEAEs generally began within the first 2 weeks of the treatment period and resolved by the end of the trial (Supplementary Figure 2). In contrast, when considering treatment related AEs, defined as those rated by the investigator as possibly, probably, or definitely related to trial medication, incidences were observed in 51.8% and 29.4% of people in the xanomeline/trospium and placebo groups, respectively (Table 2).
Body Weight
Xanomeline/trospium and placebo groups showed similarly minor increases in weight: a smaller mean change from baseline to week 5 in body weight was observed in the xanomeline/trospium group (1.41 ± 3.18 kg) compared with the placebo group (1.94 ± 5.00 kg). Approximately half as many people in the xanomeline/trospium group (5.3%) experienced clinically meaningful weight gain (defined as an increase of ≥7%) compared with placebo (11.4%). Comparable results were observed for BMI, with changes from baseline to week 5 of 0.46 ± 1.1 kg/m2 and 0.64 ± 1.6 kg/m2 observed in the xanomeline/trospium and placebo groups, respectively.
Extrapyramidal Motor Symptoms
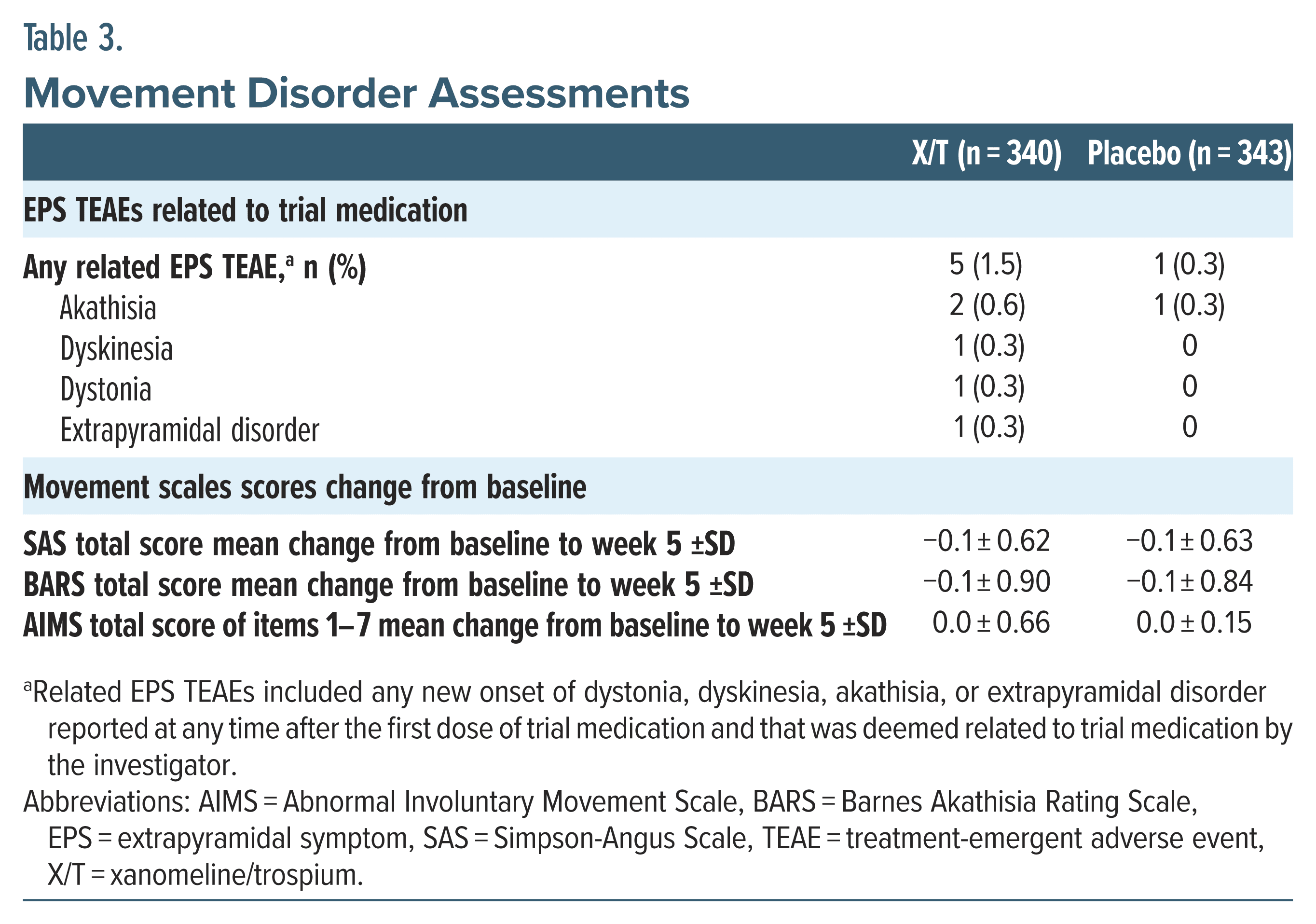
A low proportion of people treated with xanomeline/trospium (3.2%) or placebo (0.9%) experienced extrapyramidal motor symptom TEAEs. All extrapyramidal motor symptom TEAEs were mild or moderate and most resolved during the treatment period without dosage changes to trial medication. The most common extrapyramidal motor symptom TEAE was akathisia, reported by 8 (2.4%) and 3 (0.9%) participants in the xanomeline/trospium and placebo groups, respectively. Dystonia, dyskinesia, and extrapyramidal disorder TEAEs were each reported once. Although rates of extrapyramidal motor symptom TEAEs were higher in the xanomeline/trospium arm, most instances were deemed unrelated to treatment; among the participants who experienced extrapyramidal motor symptom TEAEs, 5 (1.5%) people in the xanomeline/trospium group and 1 (0.3%) person in the placebo group experienced symptoms considered treatment related (Table 3). There were no TEAE reports of TD. Changes from baseline to week 5 with xanomeline/trospium were close to 0 for SARS, BARS, and AIMS scores (Table 3).
Vital Signs
Heart rate and blood pressure, when measured at Cmax, increased with xanomeline/trospium compared with placebo. Mean supine heart rate increased over the first week of xanomeline/trospium treatment and partially attenuated with repeat dosing. By week 5, change from baseline in mean heart rate with xanomeline/ trospium and placebo was 10.4 ± 14.4 beats per minute (bpm) and 4.5 ± 13.4 bpm, respectively. Small increases in blood pressure followed a similar pattern, with peak elevations in the xanomeline/trospium group occurring in the first week and decreasing with continued treatment (Supplementary Figure 3). From baseline to week 5, mean systolic blood pressure changed by +0.7 mm Hg (xanomeline/trospium) and 0.0 mm Hg (placebo), and mean diastolic blood pressure increased by 1.9 mm Hg (xanomeline/trospium) and 0.4 mm Hg (placebo).
Subgroup Analyses
Rates of several of the most common TEAEs in the xanomeline/trospium group varied across demographic and baseline differentiators, although differences were not deemed clinically meaningful (Supplementary Table 2). Regarding the most common TEAEs reported with a difference in incidence of >5% between subgroups, females experienced constipation, nausea, and abdominal discomfort more often than males. Variations in the most common TEAEs occurred across racial and ethnic categories also, with White participants experiencing nausea and vomiting more frequently and constipation less frequently than Black participants; constipation and headache occurred more often in the Hispanic/Latino arm compared with the non-Hispanic/ Latino subgroup. Lastly, vomiting and dyspepsia were more common in the xanomeline/trospium group among those with a BMI of <30 kg/m2 vs ≥30 kg/m2, and dyspepsia was more common in the higher BMI group. Subgroup categories were generally balanced; for example, each race category contained approximately equal proportions of males and females, and the mean BMI was similar for males and females and across race categories.
DISCUSSION
Antipsychotics are the cornerstone of schizophrenia treatment but exhibit significant tolerability limitations. Side effects including extrapyramidal motor symptoms, weight gain, and somnolence/sedation reduce treatment tolerability and increase the risk of nonadherence and subsequent relapse.3,5,11 For people experiencing side effects of antipsychotic treatment, the solution may be less straightforward than switching to a different medication. Available antipsychotics exhibit overlapping safety and tolerability limitations, and health care providers may struggle to find medications for individuals in their care that improve symptoms without causing intolerable side effects. Achieving a balance between tolerability and clinical response is sufficiently difficult that up to 80% of insured people treated for schizophrenia are prescribed medications associated with risk factors for side effects they have experienced or are at risk for experiencing.30 Overlap in antipsychotic side effect profiles is not surprising given they all share the mechanism of D2 dopamine receptor blockade. New medications with alternative mechanisms to address symptoms of schizophrenia with improved safety and tolerability are an area of significant need. Xanomeline/ trospium acts preferentially via M1 and M4 muscarinic receptor agonism without direct action at D2 dopamine receptors, which may enable circumvention of some traditional adverse effects of antipsychotics related to dopamine blockade, including, for example, extrapyramidal motor symptoms and hyperprolactinemia.1,11,18,31 However, early studies evincing a therapeutic benefit of xanomeline in psychosis also revealed substantial side effects driven by xanomeline activation of peripheral muscarinic cholinergic receptors.16,17 The primarily gastrointestinal and cardiovascular side effects, including nausea, vomiting, diarrhea, syncope, and orthostasis, led to high rates of treatment discontinuation, underscoring the need for improved tolerability. The addition of trospium to block the activity of xanomeline at peripheral muscarinic receptors functions to reduce these side effects without substantially affecting xanomeline activity in the brain.
In pooled analyses of safety data from 3 short-term trials of xanomeline/trospium in adults with schizophrenia experiencing worsening psychosis, xanomeline/trospium was generally well tolerated. Most participants completed the trials, and overall discontinuation rates were similar in the xanomeline/ trospium (27.6%) and placebo (22.7%) groups. The side effect profile of xanomeline/trospium was consistent with the activity of xanomeline and trospium at muscarinic receptors: the most common TEAEs were primarily cholinergically mediated gastrointestinal events, including nausea, constipation, dyspepsia, and vomiting, all of which were mild or moderate in intensity. The most common cholinergic side effects generally began within 2 weeks of treatment initiation and lasted on average between 4 days (vomiting) and 20 days (dry mouth). Cholinergic side effects observed with placebo had similar onset, duration, and intensity. Nonetheless, gastrointestinal side effects are a significant concern for individuals taking medications and a major contributor to nonadherence in other clinical areas.32 Forthright discussion regarding the risk of side effects, their likely resolution within approximately 2 weeks of onset, and concomitant prescription of antiemetic medication may temper reluctance to initiate or continue treatment. Treatment with xanomeline/trospium was also associated with higher rates of TEAEs of hypertension and tachycardia; the latter is a known side effect of trospium chloride use.33 In addition, tachycardia is observed in approximately 5% of people treated with antipsychotics.34 These TEAEs were generally mild and transient and may not be reflective of clinically meaningful hypertension or tachycardia (ie, sustained increase in blood pressure or heart rate that may require treatment or confer cardiovascular risk). When measured early in the course of treatment and at or near Cmax, heart rate was increased in patients receiving xanomeline/trospium by approximately 10 beats per minute (bpm). While this increase could be clinically meaningful if sustained over days or weeks, the increases in heart rate observed with xanomeline/trospium attenuate after Cmax as exposure decreases and with repeated dosing, as shown here and with long-term treatment.35,36 Overall, treatment discontinuations due to TEAEs were low (xanomeline/trospium, 5.6%; placebo, 4.7%) relative to many short-term trials for antipsychotics.37–40
The xanomeline/trospium group exhibited few of the side effects often observed with antipsychotic use. Available antipsychotics increase the risk of extrapyramidal motor symptoms related to antagonism of D2 dopamine receptors, which can be bothersome, stigmatizing, and detrimental to quality of life.8,9,41,42 A small number of participants treated with xanomeline/ trospium experienced treatment-related extrapyramidal motor symptom TEAEs (xanomeline/trospium vs placebo: 1.5% vs 0.3%), and no clinically meaningful changes from baseline to week 5 were observed in any of the extrapyramidal symptom scales. The pathophysiology of akathisia, the most commonly observed motor symptom in this analysis, is believed to be distinct from other extrapyramidal motor symptoms such as dyskinesia and dystonia in that the primary drivers are likely to involve mechanisms other than dopamine dysregulation.43,44 Some data support a potential role for cholinergic systems, although much of the evidence derives from findings that anticholinergic medications are helpful in alleviating akathisia.43–45 Akathisia can be difficult to distinguish from restlessness associated with agitation in psychosis.43,45 With 4 of the 8 reported cases of akathisia diagnosed at a single site employed in the EMERGENT-3 trial, the possibility exists that some reported cases were in fact misdiagnoses of acute psychosis-related agitation.
Weight gain is another problematic side effect, affecting 15%–72% of people with schizophrenia using antipsychotics.46 Increased weight exerts negative psychological impacts and contributes to excess cardiovascular mortality and shortened life expectancy in schizophrenia.9,12,47 Changes in weight were minor and comparable between xanomeline/trospium and placebo groups, and fewer participants in the xanomeline/ trospium group experienced clinically meaningful weight gain compared with placebo (5.2% vs 11.2%). Long-term studies are needed to confirm the persistence of this treatment advantage. Lastly, somnolence hinders social and workplace functioning as well as adherence among many people treated with antipsychotics; here, rates of somnolence were low and similar between treatment groups (xanomeline/trospium, 5.0%; placebo, 4.1%).
Patient characteristics may influence the response to treatment, and pooling the acute EMERGENT trial data permitted examination of xanomeline/trospium tolerability in subgroups.48,49 Common TEAEs that exhibited subgroup differences were largely gastrointestinal, with the addition of headache and insomnia. Female and Hispanic/Latino participants experienced more TEAEs than their male and non Hispanic/Latino counterparts, while race and BMI played a less consistent role, with members of the White and low BMI subgroups experiencing 2 of 3 of TEAEs at higher rates than those in the Black and high BMI groups, respectively. No differences in TEAEs based on age were reported, and the differences observed across subgroups are small and do not meet the standard of clinical significance. Overall, the absence of robust differences in side effects based on baseline clinical or demographic characteristics suggests xanomeline/ trospium is tolerable for a broad range of people living with schizophrenia.
Limitations of this analysis reflect those of the individual trials. First, the design of the 5-week EMERGENT trials lacked a comparator arm, an approach typical of early stage registrational trials and often used in antipsychotic research, thereby preventing direct comparisons of xanomeline/trospium with other antipsychotics.11,50,51 Second, the lack of weight gain and extrapyramidal motor symptoms cannot be fully addressed by the 5-week treatment duration examined here. Longer term trials such as the 52-week open-label EMERGENT-4 (NCT04659174) and EMERGENT-5 (NCT04820309) trials are needed to confirm the promise of xanomeline/trospium therapy regarding the absence of typical antipsychotic burdens. Lastly, the inpatient design of the EMERGENT trials mitigated issues of nonadherence and concomitant use of prescribed or recreational drugs and allowed for close attention to and follow-up for AEs at the initiation of treatment that could favorably impact treatment tolerability vs an outpatient setting.
In conclusion, post hoc pooled analyses confirm and extend the safety results of the acute EMERGENT trials in people with schizophrenia experiencing acute psychosis. The most common side effects observed with xanomeline/trospium were primarily gastrointestinal TEAEs, mild or moderate in intensity, and transient in nature. AEs often observed with antipsychotic use such as extrapyramidal motor symptoms, weight gain, and somnolence were not associated with xanomeline/ trospium use. These findings, together with efficacy results showing a clinically meaningful reduction in the symptoms of schizophrenia, support the potential of xanomeline/trospium to be first in a new class of antipsychotic medications based on muscarinic receptor agonism and an efficacious and well-tolerated alternative to currently available antipsychotics.19,20
Article Information
Published Online: February 26, 2025. https://doi.org/10.4088/JCP.24m15497
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 3, 2024; accepted October 3, 2024.
To Cite: Kaul I, Claxton A, Sawchak S, et al. Safety and tolerability of xanomeline and trospium chloride in schizophrenia: pooled results from the 5-week, randomized, double-blind, placebo-controlled EMERGENT trials. J Clin Psychiatry. 2025;86(1):24m15497.
Author Affiliations: Clinical Development, Bristol Myers Squibb, Princeton, New Jersey (Kaul, Claxton, Sawchak, Sauder); Medical Affairs, Bristol Myers Squibb, Princeton, New Jersey (Brannan, Marcus); Drug Safety Pharmacovigilance, Bristol Myers Squibb, Princeton, New Jersey (Raj); Biostatistics, Bristol Myers Squibb, Princeton, New Jersey (Ruan); Principal Investigator, Woodland International Research Group, Little Rock, Arkansas (Konis); Principal Investigator, Community Clinical Research, Austin, Texas (Brown); Department of Psychiatry and Behavioral Sciences, State University of New York Upstate Medical University, Syracuse, New York (Cutler).
Corresponding Author: Ronald Marcus, MD, Bristol Myers Squibb, 99 High St, Floor 26, Boston, MA 02110 ([email protected]).
Relevant Financial Relationships: Dr Brannan is the former Chief Medical Officer of Karuna Therapeutics and is currently a consultant of Bristol Myers Squibb. Drs Kaul, Claxton, Sawchak, Sauder, Raj, Ruan, and Marcus are employees of Bristol Myers Squibb. Dr Konis owns equity in Bristol Myers Squibb and is a consultant of Merck & Co. Drs Brown and Cutler have no conflicts or reportable financial relationships to disclose.
Funding/Support: The EMERGENT trials were funded by Karuna Therapeutics, a Bristol Myers Squibb company (Boston, MA, USA).
Role of the Sponsor: The funder had a role in the design and conduct of the study; collection, management, and analysis of the data; and the review of the manuscript.
Previous Presentation: Poster presented at the American College of Neuropsychopharmacology meeting; December 3–6, 2023; Tampa, Florida.
Acknowledgments: The authors thank the study participants and investigators for their roles in this research. Medical writing and editorial support were provided by Sarah Marshall, PhD, and Paula Stuckart of Apollo Medical Communications, part of Helios Global Group, and funded by Karuna Therapeutics, a Bristol Myers Squibb company. Dr Marshall and Ms Stuckart have no conflicts of interest to disclose.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Many antipsychotics are associated with intolerable side effects
- Xanomeline/trospium is the first in a new class of approved schizophrenia treatments based on muscarinic receptor agonism without direct D2 dopamine receptor activity
- Side effects experienced by people treated for schizophrenia with xanomeline/trospium were generally gastrointestinal disorders, transient, and mild or moderate in intensity
References (51)

- Paul SM, Yohn SE, Popiolek M, et al. Muscarinic acetylcholine receptor agonists as novel treatments for schizophrenia. Am J Psychiatry. 2022;179(9):611–627. PubMed
- Horan WP, Catalano LT, Green MF. An update on treatment of cognitive impairment associated with schizophrenia. Curr Top Behav Neurosci. 2023;63:407–436.
- Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388(10039):86–97. PubMed
- Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909. PubMed CrossRef
- Zipursky RB, Menezes NM, Streiner DL. Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res. 2014;152(2−3):408–414. PubMed CrossRef
- Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician. 2010;81(5):617–622.
- Divac N, Prostran M, Jakovcevski I, et al. Second-generation antipsychotics and extrapyramidal adverse effects. Biomed Res Int. 2014;2014:656370. PubMed CrossRef
- Kadakia A, Brady BL, Dembek C, et al. Burden of EPS in commercial patients with schizophrenia initiating atypical antipsychotics. Am J Manag Care. 2022;28(9):e315–e324. PubMed
- Townsend M, Pareja K, Buchanan-Hughes A, et al. Antipsychotic-related stigma and the impact on treatment choices: a systematic review and framework synthesis. Patient Prefer Adherence. 2022;16:373–401.
- Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. PubMed
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed CrossRef
- De Hert M, Dekker JM, Wood D, et al. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry. 2009;24(6):412–424. PubMed CrossRef
- Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2−3):225–233. PubMed CrossRef
- Allison DB, Mackell JA, McDonnell DD. The impact of weight gain on quality of life among persons with schizophrenia. Psychiatr Serv. 2003;54(4):565–567. PubMed CrossRef
- Arya D, Khan T, Margolius AJ, et al. Tardive dyskinesia: treatment update. Curr Neurol Neurosci Rep. 2019;19(9):69.
- Bodick NC, Offen WW, Levey AI, et al. Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol. 1997;54(4):465–473. PubMed CrossRef
- Shekhar A, Potter WZ, Lightfoot J, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165(8):1033–1039. PubMed CrossRef
- Thorn CA, Moon J, Bourbonais CA, et al. Striatal, hippocampal, and cortical networks are differentially responsive to the M4- and M1-muscarinic acetylcholine receptor mediated effects of xanomeline. ACS Chem Neurosci. 2019;10(8):3910. PubMed CrossRef
- Brannan SK, Sawchak S, Miller AC, et al. Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia. N Engl J Med. 2021;384(8):717–726. PubMed
- Kaul I, Sawchak S, Correll CU, et al. Efficacy and safety of the muscarinic receptor agonist KarXT (xanomeline-trospium) in schizophrenia (EMERGENT-2) in the USA: results from a randomised, double-blind, placebo-controlled, flexible-dose phase 3 trial. Lancet. 2024;403(10422):160–170. PubMed
- Kaul I, Sawchak S, Walling DP, et al. Efficacy and safety of xanomeline-trospium chloride in schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2024;81(8):749–756.
- Brannan SK, Walling DP, Tamminga CA, et al. Categorical response rates, time course of response, and symptom domains of response with KarXT (xanomeline–trospium) in the EMERGENT-3 trial. Presented at the 36th European College of Neuropsychopharmacology Annual Congress; Barcelona, Spain; Oct 7-10, 2023. Poster P.1199.
- Correll CU. Unleashing the power of pooled and subgroup analyses in psychiatry. Int Clin Psychopharmacol. 2022;37(5):223–224.
- Clinicaltrials.gov. A Study to Assess Efficacy and Safety of KarXT in Acutely Psychotic Hospitalized Adult Patients With Schizophrenia (EMERGENT-3). Accessed February 26, 2024. https://clinicaltrials.gov/study/NCT04738123
- Clinicaltrials.gov. A Study to Assess Safety and Efficacy of KarXT in Adult Patients With Schizophrenia (EMERGENT-1). Accessed February 26, 2024. https://www.clinicaltrials.gov/study/NCT03697252
- Clinicaltrials.gov. A Study to Assess Efficacy and Safety of KarXT in Acutely Psychotic Hospitalized Adult Patients With Schizophrenia (EMERGENT-2). Accessed February 26, 2024. https://clinicaltrials.gov/study/NCT04659161
- Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. PubMed CrossRef
- Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–676. PubMed
- Guy W. ECDEU assessment manual for psychopharmacology. Revised. US Department of Health, Education, and Welfare Publication (ADM). National Institute of Mental Health; 1976.76–338
- Citrome L, Eramo A, Francois C, et al. Lack of tolerable treatment options for patients with schizophrenia. Neuropsychiatr Dis Treat. 2015;11:3095–3104. PubMed CrossRef
- Mirza NR, Peters D, Sparks RG. Xanomeline and the antipsychotic potential of muscarinic receptor subtype selective agonists. CNS Drug Rev. 2003;9(2):159–186. PubMed CrossRef
- Baryakova TH, Pogostin BH, Langer R, et al. Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nat Rev Drug Discov. 2023;22(5):387–409.
- Indevus Pharmaceuticals. Sanctura (trospium chloride). Prescribing information; 2012. Accessed January 29, 2024. www.accessdata.fda.gov/drugsatfda_docs/ label/2012/021595s009lbl.pdf
- Huhn M, Arndt T, Schneider-Thoma J, et al. Effects of antipsychotics on heart rate in treatment of schizophrenia: a systematic review and meta-analysis. Ther Adv Psychopharmacol. 2022;12:20451253221097261. PubMed
- Sauder C, Vandell AG, Ramsay I, et al. Cardiovascular safety and tolerability of xanomeline and trospium chloride in people with schizophrenia: pooled results from the 5-week, randomized, double-blind, placebo-controlled EMERGENT trials. Presented at the Annual Meeting of the American College of Neuropsychopharmacology; Phoenix, AZ; Dec 8-11, 2024. Poster M273.
- Vandell AG, Sauder C. Effects of KarXT (xanomeline and trospium chloride) on ambulatory blood pressure: results rrom an open-label, multicenter trial in participants with schizophrenia. Presented at the Annual Meeting of the American College of Neuropsychopharmacology; Phoenix, AZ; Dec 8-11, 2024. Poster T284.
- Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo controlled trial. Am J Psychiatry. 2015;172(9):870–880. PubMed
- Durgam S, Starace A, Li D, et al. An evaluation of the safety and efficacy of cariprazine in patients with acute exacerbation of schizophrenia: a phase II, randomized clinical trial. Schizophr Res. 2014;152(2–3):450–457. PubMed CrossRef
- Maat A, Cahn W, Gijsman HJ, et al. Open, randomized trial of the effects of aripiprazole versus risperidone on social cognition in schizophrenia. Eur Neuropsychopharmacol. 2014;24(4):575–584. PubMed CrossRef
- Moller HJ, Riedel M, Jager M, et al. Short-term treatment with risperidone or haloperidol in first-episode schizophrenia: 8-week results of a randomized controlled trial within the German Research Network on Schizophrenia. Int J Neuropsychopharmacol. 2008;11(7):985–997. PubMed CrossRef
- Li P, Snyder GL, Vanover KE. Dopamine targeting drugs for the treatment of schizophrenia: past, present and future. Curr Top Med Chem. 2016;16(29):3385–3403.
- Kapur S, Zipursky R, Jones C, et al. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157(4):514–520. PubMed CrossRef
- Bratti IM, Kane JM, Marder SR. Chronic restlessness with antipsychotics. Am J Psychiatry. 2007;164(11):1648–1654. PubMed CrossRef
- Salem H, Nagpal C, Pigott T, et al. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789–798.
- Zareifopoulos N, Katsaraki M, Stratos P, et al. Pathophysiology and management of Akathisia 70 years after the introduction of the chlorpromazine, the first antipsychotic. Eur Rev Med Pharmacol Sci. 2021;25(14):4746–4756. PubMed
- De Hert M, Detraux J, van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8(2):114–126.
- Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172–1181.
- Jerome RN, Pulley JM, Sathe NA, et al. Exploring biologic predictors response disparities to atypical antipsychotics among blacks: a quasi-systematic review. Ethn Dis. 2020;30(suppl 1):229–240. PubMed CrossRef
- Schneider-Thoma J, Efthimiou O, Bighelli I, et al. Second-generation antipsychotic drugs and short-term somatic serious adverse events: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(9):753–765. PubMed CrossRef
- Leucht S, Tardy M, Komossa K, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–2071. PubMed CrossRef
- Schneider-Thoma J, Chalkou K, Dorries C, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta analysis. Lancet. 2022;399(10327):824–836. PubMed
This PDF is free for all visitors!