Abstract
Objective: To investigate the efficacy, safety, and tolerability of brexpiprazole in combination with sertraline and as monotherapy for posttraumatic stress disorder (PTSD).
Methods: The trial comprised a 1-week placebo run-in period followed by an 11-week, randomized, double-blind, active-referenced, placebo-controlled, parallel-arm treatment period (with 14-day follow-up). The trial ran from January 2017–November 2018 at 48 clinical trial sites in the United States. Adult outpatients with PTSD (DSM-5) were randomized (1:1:1:1) to oral brexpiprazole + sertraline, brexpiprazole + placebo, sertraline + placebo, or placebo + placebo. Doses were flexible (brexpiprazole 1–3 mg/d; sertraline 100–200 mg/d). The primary endpoint was change in Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) total score from randomization (Week 1) to Week 10. Safety assessments included adverse events.
Results: Among 321 randomized participants, completion rates were 58/82 (70.7%) for brexpiprazole + sertraline, 50/75 (66.7%) for brexpiprazole +placebo, 59/81 (72.8%) for sertraline + placebo, and 64/83 (77.1%) for placebo+placebo. At Week 10, brexpiprazole + sertraline demonstrated greater improvement in CAPS-5 total score (randomization, 35.7; least-squares [LS] mean change, −16.4; n = 77) vs sertraline + placebo (randomization, 36.5; LS mean change, −11.4; n = 75) with LS mean difference, −5.08 (95% CI, −8.96 to −1.20; P= .011), and also vs brexpiprazole + placebo and vs placebo+ placebo.
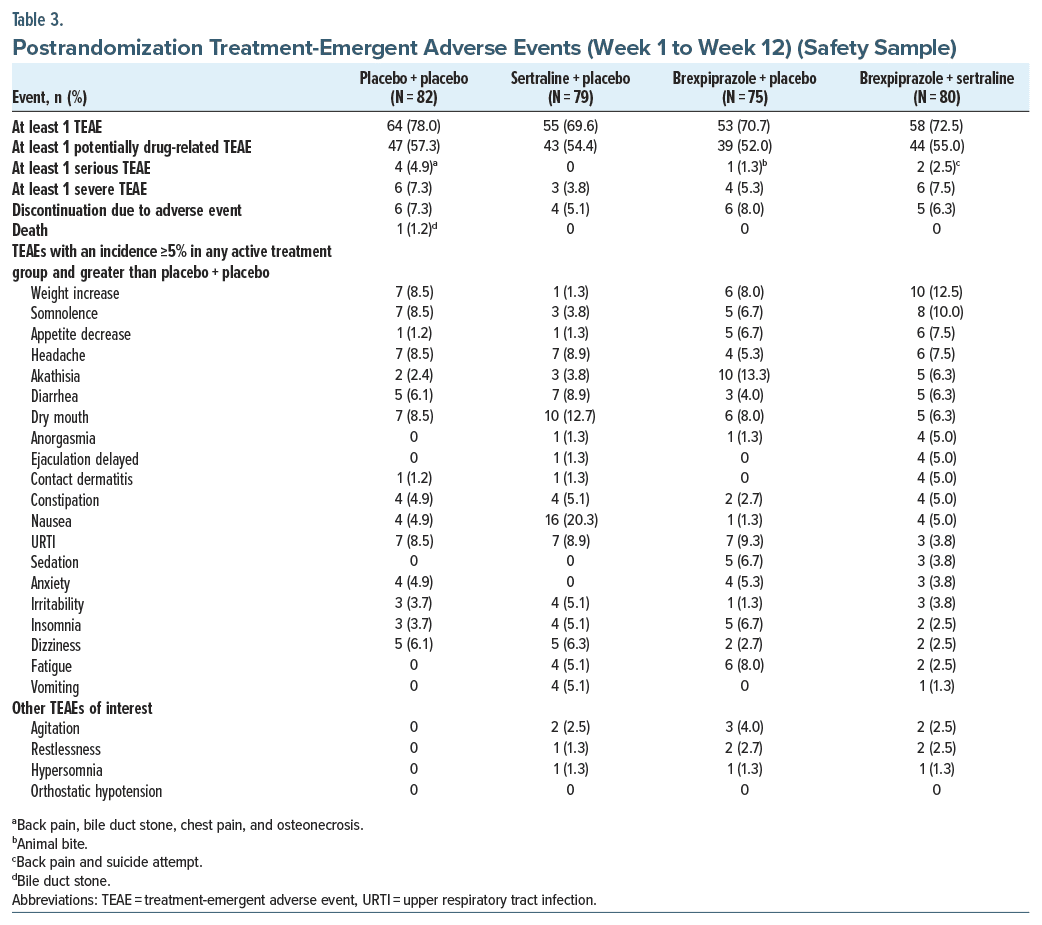
Brexpiprazole + placebo and sertraline + placebo did not differ from placebo + placebo. Treatment emergent adverse events with incidence ≥10% were weight increased (12.5%) and somnolence (10.0%) for brexpiprazole + sertraline, akathisia (13.3%) for brexpiprazole + placebo, and nausea (20.3%) and dry mouth (12.7%) for sertraline + placebo.
Conclusions: Brexpiprazole in combination with sertraline (but not as monotherapy) has potential to be a new efficacious treatment for PTSD, with a safety profile consistent with brexpiprazole in approved indications.
Trial Registration: ClinicalTrials.gov identifier: NCT03033069.
J Clin Psychiatry 2025;86(1):24m15577
Author affiliations are listed at the end of this article.
Posttraumatic stress disorder (PTSD) is a potentially chronic and disabling mental health condition that can develop following exposure to a traumatic event.1 The lifetime prevalence of PTSD is estimated at 4% globally and 6%–7% in US total/civilian populations, with a higher prevalence in women than in men.2–4 Despite a public perception that PTSD predominantly affects military populations, most PTSD cases occur in the general population due to reasons such as sexual and physical violence.5
Symptoms of PTSD can be categorized into 4 clusters: intrusion (re-experiencing the trauma as recurrent memories or dreams), avoidance (of activities, people, or places associated with the trauma), negative cognitions and mood, and marked alterations in arousal and reactivity.1 PTSD is associated with impairments in relationships, work/academic performance, and finances6; increased suicidality7,8; and comorbid psychiatric disorders.9 The estimated economic burden of PTSD in the US is $232 billion annually.10
Many patients with PTSD do not seek treatment due to stigma, shame, and fear of negative social consequences.2,11 For those who do seek treatment, PTSD is often misdiagnosed or diagnosed after a delay, which can lead to greater symptomatic burden.12,13 US Food and Drug Administration-approved pharmaceutical options for PTSD are limited to the selective serotonin reuptake inhibitors (SSRIs) sertraline and paroxetine.14 Sertraline and paroxetine have demonstrated efficacy in PTSD, with meta-analyses showing response in 50%–59% of patients15 and small but clinically significant effect sizes vs placebo (0.3–0.4).16 Off-label polypharmacy with other antidepressants, benzodiazepines, and atypical antipsychotics is common,17,18 despite a lack of established efficacy and safety.19 There is an urgent need for new pharmacologic treatments for PTSD.19
Brexpiprazole acts as an antagonist at noradrenaline α1B/α2C and serotonin 5-HT2A receptors, and as a partial agonist at serotonin 5-HT1A and dopamine D2 receptors,20 thereby acting on systems implicated across PTSD symptom clusters.21–23 Brexpiprazole has demonstrated efficacy, and is approved in various regions, for the treatment of schizophrenia,24,25 the treatment of agitation in Alzheimer’s dementia,26–28 and the adjunctive treatment of major depressive disorder.29–32 The aim of the present Phase 2 trial was to investigate the efficacy, safety, and tolerability of brexpiprazole as combination treatment with sertraline and as monotherapy in adults with PTSD.
METHODS
This was a Phase 2, multicenter, 12-week, randomized, double-blind, placebo- and active-controlled, parallel-arm trial of brexpiprazole in patients with PTSD. The trial was registered at ClinicalTrials.gov (identifier: NCT03033069), where the protocol and statistical analysis plan are available. The trial was conducted in accordance with the International Council for Harmonisation Good Clinical Practice Consolidated Guideline and local regulatory requirements. The trial protocol was approved by the governing institutional review board for each investigational site. All participants provided written electronic informed consent after trial procedures and possible side effects were fully explained, and they were reimbursed for time and travel.
Participants and Study Design
Participants (a volunteer sample) were screened by investigators at 48 sites in the US (sites and principal investigators are listed in Supplementary Table 1). Key inclusion criteria were as follows: outpatient status; age 18–65 years; diagnosis of PTSD as defined by DSM-5 criteria33 and confirmed by the Mini-International Neuropsychiatric Interview version 7,34 with symptoms for ≥6 months prior to screening; and a Clinician Administered PTSD Scale for DSM-5 (CAPS-5)35,36 total score ≥33 at screening and baseline (Day 0). Key exclusion criteria were as follows: receiving disability payments or being engaged in compensation litigation related to PTSD or another psychiatric disorder; an index traumatic event before age 16 or >15 years before screening; a traumatic event within 3 months of screening; considered psychotropic-treatment resistant/ refractory by history in the investigator’s opinion; currently receiving sertraline with adequate dose and duration; any previous exposure to brexpiprazole; a change in PTSD treatment within 28 days of screening; a current DSM-5 major depressive episode; a current or recent (within 6 months of screening) anxiety disorder that has been the primary focus of psychiatric treatment; a current or recent (within 120 days of screening) DSM 5 substance/alcohol use disorder; at significant risk of committing suicide; or any other psychiatric or medical condition as listed in the protocol.
After a 3–14-day screening/washout period, eligible participants entered a 1-week, double-blind, placebo run-in period (Period A), followed by an 11-week, double-blind, active-treatment period (Period B) in which participants were randomized 1:1:1:1 to brexpiprazole + sertraline, brexpiprazole + placebo, sertraline + placebo, or placebo + placebo. To reduce potential bias in efficacy outcomes, aspects of the trial design (illustrated in Supplementary Figure 1) were blinded to participants and trial site personnel. In the blinded protocol, the existence of the placebo run-in period, the timing and nature of randomization (ie, parallel treatment arms and randomization ratio), and the timing of the primary efficacy endpoint (Week 10) were not revealed, such that the trial appeared to comprise a single, 12-week, double-blind treatment period (with 14-day follow-up). Visits occurred weekly from baseline to Week 4, then every 2 weeks.
Brexpiprazole and sertraline were flexibly dosed at 1–3 mg/d and 100–200 mg/d, respectively (titration was over 2–3 weeks, with details in Supplementary Figure 1). Study drugs were taken orally, together, at the same time each day (once daily), without regard to meals. Brexpiprazole tablets (or matching placebo) and sertraline capsules (or matching placebo) were provided by the sponsor or designated agent in blister cards. Treatments were assigned to participants via a fixed block (block size 4) computer-generated randomization code provided by the sponsor and stratified by site and type of trauma (combat-related: yes/no). Treatment assignments were blinded to participants, investigators, and sponsor personnel, including those involved in data analysis. Prohibited medications, including psychotropic agents (antipsychotics, antidepressants, etc.), were washed out during the screening period. Benzodiazepines and nonbenzodiazepine sleep aids were prohibited except when used in the short term to manage emergent agitation/anxiety and insomnia, respectively. Psychotherapy was permitted provided it was ongoing for ≥28 days prior to screening, and the participant committed to continue the therapy during the trial.
Assessments
Participant demographics and medical history were recorded at the screening visit. Sex, race, and ethnicity were self-reported using US Census Bureau classifications. The Life Events Checklist for DSM-537 was used to identify index traumatic events. The Emory Treatment Resistance Interview for PTSD38 was used to collect information on prior PTSD treatments.
The CAPS-5,35,36 an extensively validated structured interview,39 was used to assess PTSD diagnostic status and symptom severity. The CAPS-5 includes 20 DSM-5 PTSD-symptom items that are each scored from 0 (absent) to 4 (extreme/incapacitating); total score is calculated by summing the 20 items, and symptom cluster scores by summing specific items: Intrusion (items 1–5); Avoidance (items 6–7); Negative cognitions and mood (items 8–14); and Arousal and reactivity (items 15–20).35,36 The CAPS-5 Past Month version was completed at screening, and the Past Week version at baseline (Day 0) and Weeks 1, 3, 6, 10, and 12, by trained raters. PTSD symptom severity was also assessed using the clinician-reported Clinical Global Impression–Severity of illness (CGI-S) scale,40 the clinician-reported Symptoms of Trauma Scale (SOTS),41 and the patient-reported PTSD Checklist for DSM-5 (PCL-5).42 Patient-reported anxiety and depression symptom severity were assessed using the Hospital Anxiety and Depression Scale (HADS).43
Safety was assessed via standard variables including treatment-emergent adverse events (TEAEs), body weight, laboratory tests, vital signs, electrocardiograms, the Columbia-Suicide Severity Rating Scale (C-SSRS),44 and 3 extrapyramidal symptom rating scales: Simpson–Angus Scale (SAS),45 Abnormal Involuntary Movement Scale (AIMS),40 and Barnes Akathisia Rating Scale (BARS).46
Statistical Analysis
The primary efficacy endpoint was change from randomization (Week 1) to Week 10 (ie, 9 weeks of active treatment) in CAPS-5 total score in the efficacy sample. Comparisons (mean difference between treatment arms) were made for brexpiprazole + sertraline vs brexpiprazole + placebo, vs sertraline + placebo, and vs placebo + placebo; brexpiprazole + placebo vs placebo + placebo; and sertraline + placebo vs placebo + placebo (for assay sensitivity). No testing hierarchy or adjustment for multiplicity was prespecified, and thus P values were tested at a nominal .05 level (2-sided). Using the hypothetical strategy that all participants tolerated and adhered to treatment,47 missing data were considered missing at random and handled using a mixed model for repeated measures (MMRM) approach based on observed data. Details of the sample size calculation and MMRM are provided in the Supplementary Methods. Prespecified subgroup analyses of the primary efficacy endpoint were performed by sex, race, age, Period A response, trauma type, psychosocial support, previous PTSD pharmacotherapy, and time since index traumatic event. Missing-not-at-random sensitivity analyses were performed.
“Other” efficacy endpoints (CAPS-5 symptom clusters, CGI-S, SOTS total, HADS Anxiety, HADS Depression, and PCL-5 total scores; and CAPS-5 response rate [≥30% or >11-point improvement from Week 1]) were tested at a nominal .05 level (2-sided).
RESULTS
Participants
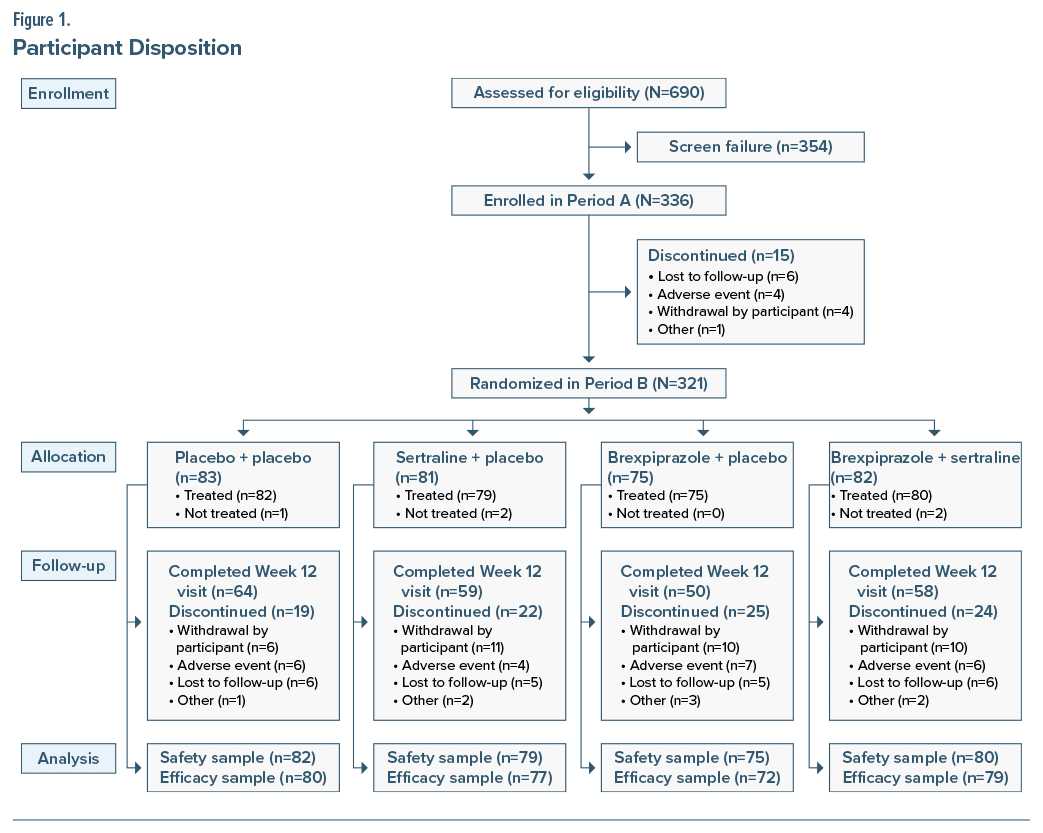
The trial was conducted between January 26, 2017, and November 12, 2018. Of 336 participants who entered Period A, 321 entered Period B and were randomized to brexpiprazole + sertraline (N = 82), brexpiprazole + placebo (N = 75), sertraline + placebo (N = 81), or placebo + placebo (N = 83) (Figure 1). Period B completion rates were 58/82 (70.7%) for brexpiprazole + sertraline, 50/75 (66.7%) for brexpiprazole + placebo, 59/81 (72.8%) for sertraline + placebo, and 64/83 (77.1%) for placebo + placebo. The most common reasons for discontinuation postrandomization were withdrawal by the participant, lost to follow-up, and adverse event (Figure 1). The safety sample comprised 316 treated participants. The efficacy sample comprised 308 participants; however, 299 patients were included in the primary efficacy analysis since 9 patients who discontinued did not have a CAPS-5 value within the permitted window.
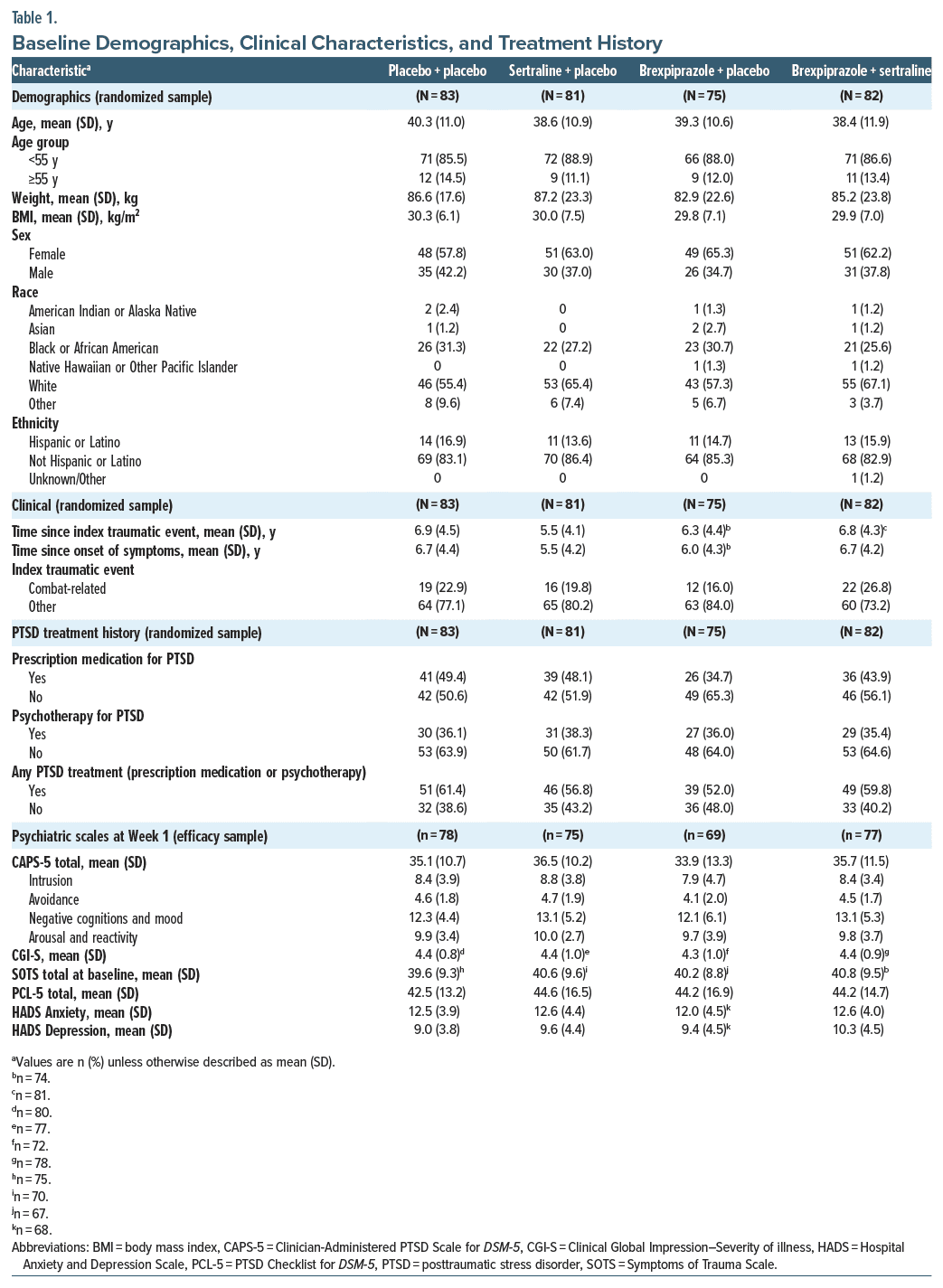
Baseline demographics, clinical characteristics, and treatment history were similar between treatment groups (Table 1). Overall, the randomized sample had a mean (SD) age of 39.2 (11.1) years, 199/321 (62.0%) participants were female, and 197 (61.4%) were White, with a mean (SD) of 6.4 (4.3) years since the index trauma. Psychiatric disorders with incidence >5% by history (MedDRA preferred terms) were major depression (n = 74, 23.1%), insomnia (n = 28, 8.7%), anxiety (n = 17, 5.3%), and depression (n = 17, 5.3%). Overall, 142/321 (44.2%) participants had previously received any prescription medication for PTSD (Table 1), of whom 78 (24.3%) had previously received an SSRI.
During the placebo run-in period, mean (SD) CAPS-5 total score change from baseline (Day 0) to randomization (Week 1) was −7.7 (9.3) points (n = 308).
By group, the mean dose at each participant’s last visit was brexpiprazole 2.2 mg + sertraline 161 mg (n = 80), brexpiprazole 2.1 mg + placebo (n = 75), and sertraline 158 mg + placebo (n = 79).
Efficacy
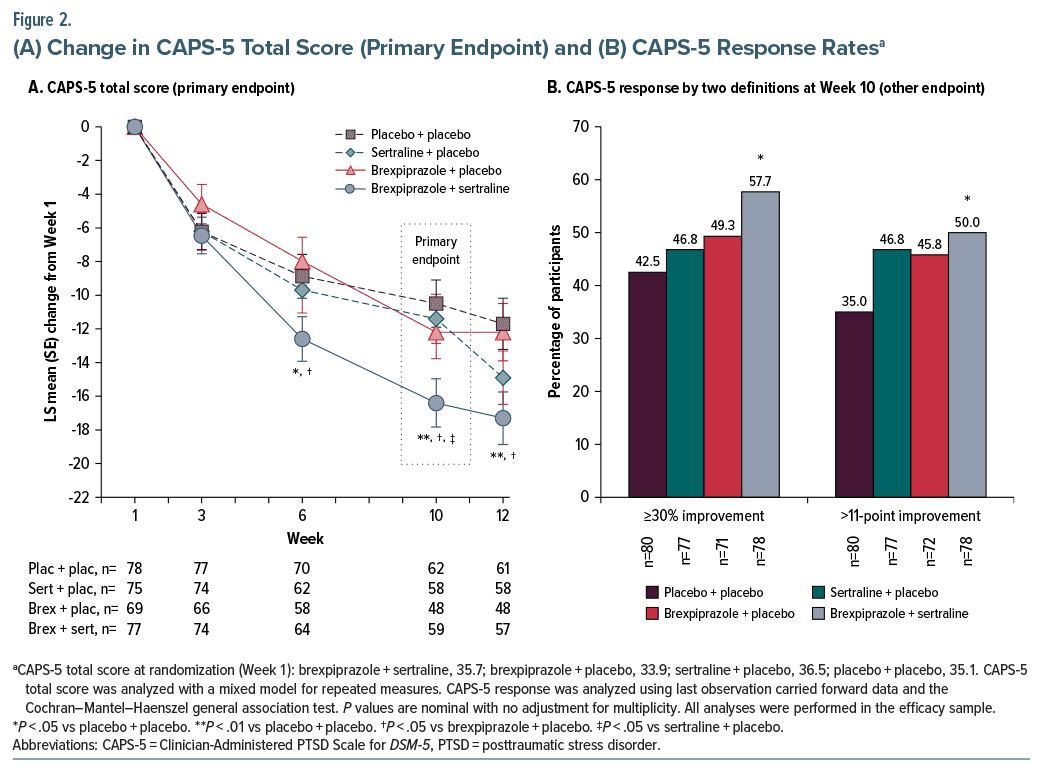
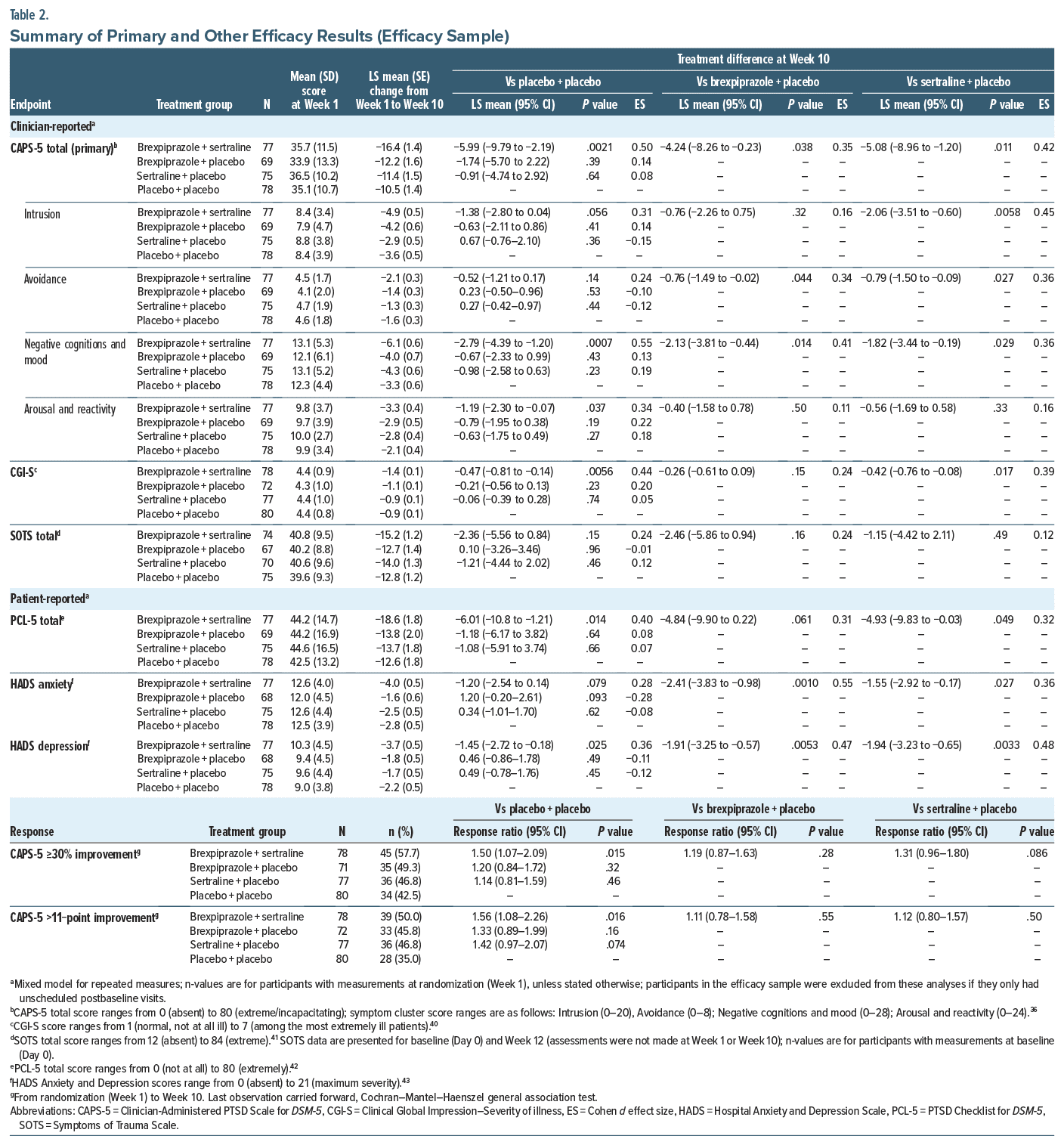
Primary endpoint. Brexpiprazole + sertraline demonstrated greater improvement vs sertraline + placebo, vs brexpiprazole + placebo, and vs placebo + placebo on the LS mean change in CAPS-5 total score from randomization (Week 1) to Week 10, with treatment differences of −5.08 (95% CI, −8.96 to −1.20; P=.011), −4.24 (95% CI, −8.26 to −0.23; P=.038), and −5.99 (95% CI, −9.79 to −2.19; P=.0021), respectively. Greater improvement (P <.05) for brexpiprazole+sertraline vs brexpiprazole+placebo and vs placebo+placebo was observed from Week 6 onwards (Figure 2A). Neither brexpiprazole+placebo nor sertraline+placebo differed from placebo+placebo at Week 10, with treatment differences of −1.74 (95% CI, −5.70 to 2.22; P=.39) and −0.91 (95% CI, −4.74 to 2.92; P=.64), respectively. Subgroup analyses are presented in Supplementary Figure 2; notably, nonresponse in the placebo run-in period led to greater treatment difference at Week 10. Missing-not-at-random sensitivity analyses indicated that primary endpoint results were robust (Supplementary Table 2).
Other efficacy endpoints. Brexpiprazole+sertraline showed greater improvement (P <.05) vs sertraline+placebo on the following efficacy endpoints at Week 10: CAPS-5 Intrusion, Avoidance, and Negative cognitions and mood symptom cluster scores; CGI-S score; PCL-5 total score; HADS Anxiety score; and HADS Depression score (Table 2). Brexpiprazole+sertraline showed greater improvement (P <.05) vs brexpiprazole+placebo and vs placebo+placebo on various efficacy endpoints, as presented in Table 2, Figure 2B, and Supplementary Figures 3 and 4.
Safety
Postrandomization, TEAEs were reported by 230/316 (72.8%) participants overall, with similar incidence between treatment groups (Table 3). TEAEs with incidence ≥10% were weight increased and somnolence for brexpiprazole + sertraline, akathisia for brexpiprazole + placebo, and nausea and dry mouth for sertraline + placebo (details in Table 3). Most TEAEs were mild or moderate in severity. Extrapyramidal symptom-related TEAEs were reported by 13 (16.3%) participants on brexpiprazole + sertraline, 12 (16.0%) on brexpiprazole+placebo, 11 (13.9%) on sertraline+placebo, and 4 (4.9%) on placebo+placebo. No specific TEAE led to discontinuation in >2 participants in any treatment group. One participant died during the trial, on placebo + placebo, from a bile duct stone.
Mean change in body weight from randomization (Week 1) to each participant’s last visit was +1.4 kg for brexpiprazole+sertraline, +0.7 kg for brexpiprazole + placebo, −0.2 kg for sertraline+placebo, and +0.3 kg for placebo+placebo (details in Supplementary Table 3). At last visit, weight gain ≥7% from Week 1 was experienced by 4/80 (5.0%) participants on brexpiprazole+sertraline, 4/75 (5.3%) on brexpiprazole+placebo, 1/79 (1.3%) on sertraline+placebo, and 2/82 (2.4%) on placebo+placebo. The corresponding values for weight loss ≥7% were 1/80 (1.3%), 1/75 (1.3%), 2/79 (2.5%), and 3/82 (3.7%), respectively.
No clinically meaningful differences between treatment groups were observed for changes from baseline to last visit in laboratory test parameters, vital signs, or electrocardiograms, except that triglycerides increased by a greater amount in the 2 sertraline groups (Supplementary Table 3). One participant (1.3%) on sertraline + placebo and 2 participants (2.4%) on placebo + placebo reported TEAEs of suicidal ideation; 1 participant (1.3%) on brexpiprazole + sertraline survived a suicide attempt and withdrew from the trial. C-SSRS findings suggested treatment-emergent suicidal ideation at any visit for 4/80 (5.0%) participants on brexpiprazole + sertraline, 6/75 (8.0%) on brexpiprazole + placebo, 9/79 (11.4%) on sertraline + placebo, and 8/82 (9.8%) on placebo + placebo, and treatment-emergent suicidal behavior at any visit for 1/79 (1.3%) participant on sertraline + placebo (0 in the other treatment groups). Changes in SAS, AIMS, and BARS scores were minimal in all treatment groups (Supplementary Table 3).
DISCUSSION
In this randomized clinical trial, brexpiprazole and sertraline combination treatment improved the symptoms of PTSD vs sertraline + placebo, vs brexpiprazole + placebo, and vs placebo + placebo on the primary efficacy endpoint of change in CAPS-5 total score at Week 10. Although this trial had no prespecified adjustment for multiplicity, the statistical significance of brexpiprazole + sertraline vs sertraline + placebo (P = .011 for primary endpoint) was indicated by 3 retrospective procedures to adjust for multiplicity: Bonferroni (tested at 0.0167 level), Holm step-down (0.025 level), and Hochberg step-up (0.025 level). Other efficacy endpoints were generally supportive of the primary efficacy endpoint, with brexpiprazole + sertraline showing improvement vs sertraline + placebo on overall symptoms (clinician reported CGI-S and patient-reported PCL-5), 3 of 4 PTSD symptom clusters, and anxious and depressive symptoms (HADS). In contrast, there was no efficacy signal in the brexpiprazole + placebo or sertraline + placebo arms. Sertraline has been extensively studied in PTSD, and, while a number of randomized clinical trials support its efficacy on overall PTSD symptoms,48–51 several did not demonstrate significant efficacy vs placebo,52–55 meaning that the lack of efficacy for sertraline + placebo in the present trial is not unanticipated.
There were no unexpected safety events with brexpiprazole and sertraline combination treatment in the present trial, and the safety profile of brexpiprazole was comparable to that in approved indications.56–62 Weight increase was highest in the brexpiprazole + sertraline group (+1.4 kg; reported as a TEAE by 12.5%); moderate weight gain has been noted with brexpiprazole in other indications.56,57 Akathisia, a concern with some antipsychotics,63 was reported as a TEAE by 6.3% on brexpiprazole + sertraline and 13.3% on brexpiprazole + placebo but was not identified by objective rating scales. The incidence of somnolence was comparable for brexpiprazole + sertraline (10.0%) and placebo + placebo (8.5%). Sertraline + placebo was associated with nausea (20.3%) and dry mouth (12.7%); these are known side effects of sertraline treatment.64 There were no clinically meaningful changes in metabolic parameters or prolactin across groups, in line with brexpiprazole in other indications.56–60,65 Rates of discontinuation due to adverse events were similar between active treatment groups (5.1–8.0%) and placebo (7.3%) (indicating that most participants tolerated treatment) and were slightly lower than in prior 10–12-week randomized clinical trials of sertraline in PTSD (9.8% in a meta-analysis).15
Brexpiprazole and sertraline combination treatment may improve PTSD symptoms via synergistic activity in the amygdala. In PTSD, high noradrenaline levels can increase fear response via overactivation of α1 receptors in the amygdala, while low serotonin levels can prevent regulation of amygdala activity.21,66–68 With combination treatment, sertraline may increase serotonin levels to help regulate amygdala activity,69–71 while brexpiprazole acts via blockade of α1 and 5-HT2A receptors and partial agonism of serotonin 5-HT1A and D2 receptors to help to normalize fear processing.20,72
A strength of this trial is the use of a blinded placebo run-in period to reduce the bias (placebo response) that can occur when participants enter a clinical trial (reflected by a mean 7.7-point CAPS-5 total score improvement during Period A), thereby allowing for a more accurate assessment of the efficacy in the randomized period.73 Other strengths are the full-factorial design with an active reference, the exclusion of patients with a current major depressive episode, and the concurrent use of clinician and patient-reported outcomes. This trial also demonstrated the value of blinding the timing of the primary efficacy endpoint, since brexpiprazole+sertraline had P<.05 vs sertraline+placebo at Week 10 but not at Week 12 (attributed to an end-of-trial improvement in the sertraline+placebo group, rather than a loss of improvement in the brexpiprazole+sertraline group).
Limitations include the lack of prespecified adjustment for multiplicity (addressed retrospectively) and the lack of efficacy in the sertraline + placebo assay sensitivity arm. Both brexpiprazole and sertraline were flexibly dosed, which reflects clinical practice but may limit conclusions in the combination treatment arm. Participant selection criteria and restrictions surrounding concomitant medications and comorbidities mean that results may not be generalizable to a broader patient population. An established CAPS-5 meaningful within-patient change threshold is needed to help interpret clinical relevance.
In conclusion, this clinical trial suggests that brexpiprazole in combination with sertraline (but not as monotherapy) has the potential to be a new efficacious treatment for PTSD. Improvement was shown on overall PTSD symptoms, as well as anxious and depressive symptoms. No new safety signals were identified for brexpiprazole, and rates of discontinuation due to adverse events suggested that brexpiprazole and sertraline combination treatment was tolerated by most participants. Results of this trial need to be replicated, and a larger trial has recently provided further evidence for the efficacy and tolerability of brexpiprazole in combination with sertraline in PTSD.74
Article Information
Published Online: February 19, 2025. https://doi.org/10.4088/JCP.24m15577
© 2025 Physicians Postgraduate Press, Inc.
Submitted: August 23, 2024; accepted December 4, 2024.
To Cite: Hobart M, Chang D, Hefting N, et al. Brexpiprazole in combination with sertraline and as monotherapy in posttraumatic stress disorder: a full-factorial randomized clinical trial. J Clin Psychiatry. 2025;86(1):24m15577.
Author Affiliations: Otsuka Pharmaceutical Development & Commercialization Inc., Princeton, New Jersey (Hobart, Chang); H. Lundbeck A/S, Valby, Denmark (Hefting); Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham Heersink School of Medicine, Birmingham, Alabama (Davis).
Corresponding Author: Mary Hobart, PhD, 508 Carnegie Center Drive, Princeton, NJ 08540 ([email protected]).
Relevant Financial Relationships: Drs Hobart and Chang are full-time employees of Otsuka Pharmaceutical Development & Commercialization Inc. Mr Hefting is a full-time employee of H. Lundbeck A/S. Dr Davis has received consulting fees from Otsuka/ Lundbeck, Boehringer Ingelheim, and Signant Health and honorarium from Clinical Care Options.
Funding/Support: This research was supported by Otsuka Pharmaceutical Development & Commercialization Inc. (Princeton, NJ, USA) and H. Lundbeck A/S (Valby, Denmark).
Role of the Sponsors: The sponsors were involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication.
Previous Presentation: Poster presented at the American Society of Clinical Psychopharmacology annual meeting; May 28–31, 2024; Miami Beach, Florida.
Data Sharing Statement: The trial protocol and statistical analysis plan are available from https://clinicaltrials.gov/study/NCT03033069. Requests for trial data can be submitted at the Otsuka Pharmaceutical Clinical Trial Data Transparency website (https://clinical-trials.otsuka.com/). Requests for the clinical study report, analytical code, and anonymized individual participant data will be considered for researchers who provide a methodologically sound proposal for use of this information. Data will be available immediately following publication of this manuscript, with no anticipated end date.
Acknowledgments: Writing support was provided by Chris Watling, PhD, and colleagues of Cambridge (a division of Prime, Knutsford, UK) and funded by Otsuka Pharmaceutical Development & Commercialization Inc. and H. Lundbeck A/S.
ORCID: Nanco Hefting: https://orcid.org/0000-0003-3310-3439
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- There is an urgent need for new effective pharmacologic treatments for PTSD.
- The combination of brexpiprazole and sertraline has the potential to be an effective and tolerated new treatment for people with PTSD.
References (74)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Ed. Text Rev. American Psychiatric Association; 2022.
- Koenen KC, Ratanatharathorn A, Ng L, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med. 2017;47(13):2260–2274. PubMed CrossRef
- Kessler RC, Rose S, Koenen KC, et al. How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. World Psychiatry. 2014;13(3):265–274. PubMed CrossRef
- Schein J, Houle C, Urganus A, et al. Prevalence of post-traumatic stress disorder in the United States: a systematic literature review. Curr Med Res Opin. 2021;37(12):2151–2161.
- Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. Trauma and PTSD in the WHO World Mental Health Surveys. Eur J Psychotraumatol. 2017;8(Suppl 5):1353383. PubMed CrossRef
- Rodriguez P, Holowka DW, Marx BP. Assessment of posttraumatic stress disorder-related functional impairment: a review. J Rehabil Res Dev. 2012;49(5):649–665. PubMed CrossRef
- Nepon J, Belik SL, Bolton J, et al. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress Anxiety. 2010;27(9):791–798. PubMed CrossRef
- Fox V, Dalman C, Dal H, et al. Suicide risk in people with post-traumatic stress disorder: a cohort study of 3.1 million people in Sweden. J Affect Disord. 2021;279:609–616.
- Qassem T, Aly-ElGabry D, Alzarouni A, et al. Psychiatric co-morbidities in post traumatic stress disorder: detailed findings from the Adult Psychiatric Morbidity Survey in the English population. Psychiatr Q. 2021;92(1):321–330.
- Davis LL, Schein J, Cloutier M, et al. The economic burden of posttraumatic stress disorder in the United States from a societal perspective. J Clin Psychiatry. 2022;83(3):21m14116. PubMed
- Kantor V, Knefel M, Lueger-Schuster B. Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: a systematic review. Clin Psychol Rev. 2017;52:52–68. PubMed CrossRef
- Gagnon-Sanschagrin P, Schein J, Urganus A, et al. Identifying individuals with undiagnosed post-traumatic stress disorder in a large United States civilian population – a machine learning approach. BMC Psychiatry. 2022;22(1):630.
- Davis LL, Urganus A, Gagnon-Sanschagrin P, et al. Patient journey of civilian adults diagnosed with posttraumatic stress disorder – a chart review study. Curr Med Res Opin. 2024;40(3):505–516.
- Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. PubMed CrossRef
- Williams T, Phillips NJ, Stein DJ, et al. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2022;3(3):CD002795. PubMed
- Hoskins MD, Bridges J, Sinnerton R, et al. Pharmacological therapy for post traumatic stress disorder: a systematic review and meta-analysis of monotherapy, augmentation and head-to-head approaches. Eur J Psychotraumatol. 2021;12(1):1802920. PubMed
- Davis LL, Urganus A, Gagnon-Sanschagrin P, et al. Patient journey before and after a formal post-traumatic stress disorder diagnosis in adults in the United States – a retrospective claims study. Curr Med Res Opin. 2023;39(11):1523–1532.
- Holder N, Woods A, Neylan TC, et al. Trends in medication prescribing in patients with PTSD from 2009 to 2018: a national veterans administration study. J Clin Psychiatry. 2021;82(3):20m13522. PubMed
- Krystal JH, Davis LL, Neylan TC, et al. It is time to address the crisis in the pharmacotherapy of posttraumatic stress disorder: a consensus statement of the PTSD Psychopharmacology Working Group. Biol Psychiatry. 2017;82(7):e51–e59. PubMed CrossRef
- Maeda K, Sugino H, Akazawa H, et al. Brexpiprazole I: in vitro and in vivo characterization of a novel serotonin–dopamine activity modulator. J Pharmacol Exp Ther. 2014;350(3):589–604. PubMed CrossRef
- Krystal JH, Neumeister A. Noradrenergic and serotonergic mechanisms in the neurobiology of posttraumatic stress disorder and resilience. Brain Res. 2009;1293:13–23. PubMed CrossRef
- Davis LL, Suris A, Lambert MT, et al. Post-traumatic stress disorder and serotonin: new directions for research and treatment. J Psychiatry Neurosci. 1997;22(5):318–326. PubMed
- Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(Pt B):181–195. PubMed CrossRef
- Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo controlled trial. Am J Psychiatry. 2015;172(9):870–880. PubMed
- Kane JM, Skuban A, Ouyang J, et al. A multicenter, randomized, double-blind, controlled Phase 3 trial of fixed-dose brexpiprazole for the treatment of adults with acute schizophrenia. Schizophr Res. 2015;164(1–3):127–135. PubMed CrossRef
- Grossberg GT, Kohegyi E, Mergel V, et al. Efficacy and safety of brexpiprazole for the treatment of agitation in Alzheimer’s dementia: two 12-week, randomized, double blind, placebo-controlled trials. Am J Geriatr Psychiatry. 2020;28(4):383–400.
- Lee D, Slomkowski M, Hefting N, et al. Brexpiprazole for the treatment of agitation in Alzheimer dementia: a randomized clinical trial. JAMA Neurol. 2023;80(12):1307–1316. PubMed
- Otsuka Pharmaceutical Co. Ltd. Rexulti® (Brexpiprazole) tablets, for oral use, Prescribing information [United States]. 2024. Accessed June 3, 2024. https:// www.otsuka-us.com/media/static/Rexulti-PI.pdf
- Thase ME, Youakim JM, Skuban A, et al. Efficacy and safety of adjunctive brexpiprazole 2 mg in major depressive disorder: a Phase 3, randomized, placebo controlled study in patients with inadequate response to antidepressants. J Clin Psychiatry. 2015;76(9):1224–1231. PubMed CrossRef
- Thase ME, Youakim JM, Skuban A, et al. Adjunctive brexpiprazole 1 and 3 mg for patients with major depressive disorder following inadequate response to antidepressants: a Phase 3, randomized, double-blind study. J Clin Psychiatry. 2015;76(9):1232–1240. PubMed CrossRef
- Hobart M, Skuban A, Zhang P, et al. A randomized, placebo-controlled study of the efficacy and safety of fixed-dose brexpiprazole 2 mg/d as adjunctive treatment of adults with major depressive disorder. J Clin Psychiatry. 2018;79(4):17m12058. PubMed
- Hobart M, Skuban A, Zhang P, et al. Efficacy and safety of flexibly dosed brexpiprazole for the adjunctive treatment of major depressive disorder: a randomized, active-referenced, placebo-controlled study. Curr Med Res Opin. 2018;34(4):633–642. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–57.
- Weathers FW, Blake DD, Schnurr PP, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) – Past Month [Measurement instrument]. 2018. Accessed March 13, 2024. https://www.ptsd.va.gov
- Weathers FW, Blake DD, Schnurr PP, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) – Past Week [Measurement instrument]. 2018. Accessed March 13, 2024. https://www.ptsd.va.gov/
- Weathers FW, Blake DD, Schnurr PP, et al. The Life Events Checklist for DSM-5 (LEC-5) – Extended. [Measurement instrument]. 2018. Accessed March 13, 2024. https://www.ptsd.va.gov
- Dunlop BW, Kaye JL, Youngner C, et al. Assessing treatment-resistant posttraumatic stress disorder: the Emory Treatment Resistance Interview for PTSD (E-TRIP). Behav Sci. 2014;4(4):511–527. PubMed CrossRef
- Weathers FW, Bovin MJ, Lee DJ, et al. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol Assess. 2018;30(3):383–395. PubMed CrossRef
- Guy W. ECDEU Assessment Manual for Psychopharmacology, Revised. National Institute of Mental Health; 1976.
- Ford JD, Mendelsohn M, Opler LA, et al. The Symptoms of Trauma Scale (SOTS): an initial psychometric study. J Psychiatr Pract. 2015;21(6):474–483. PubMed CrossRef
- Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL 5) – Extended Criterion A [Measurement instrument]. 2023. Accessed March 13, 2024. https://www.ptsd.va.gov
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Posner K, Brown GK, Stanley B, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. PubMed CrossRef
- Simpson GM, Angus JWS. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. PubMed CrossRef
- Barnes TRE. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–676. PubMed CrossRef
- U.S. Food and Drug Administration. E9(R1) statistical principles for clinical trials: addendum: estimands and sensitivity analysis in clinical trials. Guidance for Industry. 2021.
- Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837–1844. PubMed CrossRef
- Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry. 2001;58(5):485–492. PubMed CrossRef
- Panahi Y, Moghaddam BR, Sahebkar A, et al. A randomized, double-blind, placebo-controlled trial on the efficacy and tolerability of sertraline in Iranian veterans with post-traumatic stress disorder. Psychol Med. 2011;41(10):2159–2166. PubMed CrossRef
- Li W, Ma YB, Yang Q, et al. Effect and safety of sertraline for treat posttraumatic stress disorder: a multicenter randomised controlled study. Int J Psychiatry Clin Pract. 2017;21(2):151–155. PubMed CrossRef
- Zohar J, Amital D, Miodownik C, et al. Double-blind placebo-controlled pilot study of sertraline in military veterans with posttraumatic stress disorder. J Clin Psychopharmacol. 2002;22(2):190–195. PubMed CrossRef
- Tucker P, Potter-Kimball R, Wyatt DB, et al. Can physiologic assessment and side effects tease out differences in PTSD trials? A double-blind comparison of citalopram, sertraline, and placebo. Psychopharmacol Bull. 2003;37(3):135–149. PubMed
- Davidson J, Rothbaum BO, Tucker P, et al. Venlafaxine extended release in posttraumatic stress disorder: a sertraline- and placebo-controlled study. J Clin Psychopharmacol. 2006;26(3):259–267. PubMed CrossRef
- Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711–720. PubMed CrossRef
- Newcomer JW, Eriksson H, Zhang P, et al. Changes in metabolic parameters and body weight in patients with major depressive disorder treated with adjunctive brexpiprazole: pooled analysis of Phase 3 clinical studies. J Clin Psychiatry. 2019;80(6):18m12680. PubMed
- Newcomer JW, Eriksson H, Zhang P, et al. Changes in metabolic parameters and body weight in brexpiprazole-treated patients with acute schizophrenia: pooled analyses of Phase 3 clinical studies. Curr Med Res Opin. 2018;34(12):2197–2205. PubMed CrossRef
- Newcomer JW, Meehan SR, Chen D, et al. Changes in metabolic parameters and body weight in patients with prediabetes treated with adjunctive brexpiprazole for major depressive disorder: pooled analysis of short- and long-term clinical studies. J Clin Psychiatry. 2023;84(5):23m14786. PubMed
- Clayton AH, Ivkovic J, Chen D, et al. Effect of brexpiprazole on prolactin and sexual functioning: an analysis of short- and long-term study data in major depressive disorder. J Clin Psychopharmacol. 2020;40(6):560–567.
- Ivkovic J, Lindsten A, George V, et al. Effect of brexpiprazole on prolactin: an analysis of short- and long-term studies in schizophrenia. J Clin Psychopharmacol. 2019;39(1):13–19.
- Kane JM, Skuban A, Hobart M, et al. Overview of short- and long-term tolerability and safety of brexpiprazole in patients with schizophrenia. Schizophr Res. 2016;174(1-3):93–98. PubMed CrossRef
- Thase ME, Zhang P, Weiss C, et al. Efficacy and safety of brexpiprazole as adjunctive treatment in major depressive disorder: overview of four short-term studies. Expert Opin Pharmacother. 2019;20(15):1907–1916. PubMed CrossRef
- Citrome L. Activating and sedating adverse effects of second-generation antipsychotics in the treatment of schizophrenia and major depressive disorder: absolute risk increase and number needed to harm. J Clin Psychopharmacol. 2017;37(2):138–147.
- Almatica Pharma LLC, Sertraline hydrochloride capsules, for oral use, Prescribing information [United States]; 2023. Accessed May 24, 2024. https://www. sertralinecaps.com/static/documents/prescribing-information.pdf
- Weiss C, Weiller E, Baker RA, et al. The effects of brexpiprazole and aripiprazole on body weight as monotherapy in patients with schizophrenia and as adjunctive treatment in patients with major depressive disorder: an analysis of short-term and long-term studies. Int Clin Psychopharmacol. 2018;33(5):255–260. PubMed CrossRef
- Arnsten AFT. Stress weakens prefrontal networks: molecular insults to higher cognition. Nat Neurosci. 2015;18(10):1376–1385. PubMed CrossRef
- Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Dialogues Clin Neurosci. 2011;13(3):263–278. PubMed
- Ferry B, Roozendaal B, McGaugh JL. Involvement of α1-adrenoceptors in the basolateral amygdala in modulation of memory storage. Eur J Pharmacol. 1999;372(1):9–16. PubMed CrossRef
- MacQueen G, Born L, Steiner M. The selective serotonin reuptake inhibitor sertraline: its profile and use in psychiatric disorders. CNS Drug Rev. 2001;7(1):1–24. PubMed CrossRef
- de Paula BB, Leite-Panissi CRA. Distinct effect of 5-HT1A and 5-HT2A receptors in the medial nucleus of the amygdala on tonic immobility behavior. Brain Res. 2016;1643:152–158. PubMed CrossRef
- Li X, Inoue T, Abekawa T, et al. 5-HT1A receptor agonist affects fear conditioning through stimulations of the postsynaptic 5-HT1A receptors in the hippocampus and amygdala. Eur J Pharmacol. 2006;532(1–2):74–80. PubMed CrossRef
- Cohen H, Zohar J, Kaplan Z, et al. Adjunctive treatment with brexpiprazole and escitalopram reduces behavioral stress responses and increase hypothalamic NPY immunoreactivity in a rat model of PTSD-like symptoms. Eur Neuropsychopharmacol. 2018;28(1):63–74. PubMed CrossRef
- Chen YF, Yang Y, Hung HM, et al. Evaluation of performance of some enrichment designs dealing with high placebo response in psychiatric clinical trials. Contemp Clin Trials. 2011;32(4):592–604. PubMed CrossRef
- Davis LL, Behl S, Lee D, et al. Brexpiprazole and sertraline combination treatment in posttraumatic stress disorder: a Phase 3 randomized clinical trial. JAMA Psychiatry. Published online December 18, 2024. doi:10.1001/jamapsychiatry. 2024.3996 CrossRef
This PDF is free for all visitors!