Abstract
Background: Individuals experiencing major depression with psychotic features (MD-P) may respond better and have fewer cognitive effects with electroconvulsive therapy (ECT) than those without psychotic features (MD-NP). However, this may be due to differences in patient characteristics aside from psychotic symptoms. The objectives of this study were to (1a) compare ECT treatment response and (1b) adverse cognitive effects between patients with MD-P and MD-NP and (2a) explore factors associated with treatment response or (2b) adverse cognitive effects.
Methods: This was a retrospective cohort study of adult inpatients with MD-P or MD-NP treated with an acute course of ECT at an academic psychiatric hospital June 2010–September 2021 in Toronto, Canada. Logistic regression was used to account for differences in patient characteristics between groups. Outcomes were identified using the clinical global impression improvement and cognitive function scales.
Results: 542 patients were included, 115 (21%) with MD-P and 427 (79%) with MD-NP. MD-P patients were more likely to be rated “very much improved” with ECT (41% vs 27%, P = .003) while adverse cognitive effects were similar (21% MD-NP vs 24% MD-P; P > .05). However, after accounting for confounders, psychotic symptoms were not associated with response (adjusted odds ratio [AOR]: 1.04; 95% confidence interval [CI], 0.95–1.14) or adverse cognitive effects (AOR: 1.30; 95% CI, 0.78–2.18).
Conclusions: Individuals with MD-P had a higher rate of response and similar rates of adverse cognitive effects compared to patients with MD-NP with ECT treatment. However, after accounting for differences in patient characteristics, we no longer identified an association between psychotic symptoms and treatment response.
J Clin Psychiatry 2025;86(1):24m15399
Author affiliations are listed at the end of this article.
Major depressive disorder (MDD) is a common disabling mental health illness associated with increased morbidity and mortality and decreased quality of life.1,2 Psychotic depression is a more severe form of MDD where there is a combination of both depressed mood and psychotic symptoms. The estimated prevalence of psychotic depression is 4 per 1,000 people in the general population, increasing to 14–30 per 1,000 people over the age of 60.3–5 Of those with depression, 15% to 19% of patients also develop psychotic features.5,6
Major depression with psychosis (MD-P) is often under-recognized and inadequately treated.7,8 Without treatment, MD-P has a low rate of spontaneous recovery and high risk of suicide, with a 69% relative risk of increase in suicidal death compared to major depression nonpsychotic (MD-NP) patients.9 The results of pharmacologic trials suggest that the combination of an antidepressant with an antipsychotic is more effective than monotherapy with either one of them if the duration of treatment is adequate, achieving up to 77% response rate.10–13 Individuals with psychotic depression are often severely ill, and pharmacotherapy can take weeks before showing improvement.14 As a result, electroconvulsive therapy (ECT) is often recommended by guidelines as a first-line treatment for psychotic depression.15,16
ECT has been shown to have an overall response rate of 82%–90% for treating psychotic depression, which is superior to combination pharmacologic therapy.15,17 Some clinical trials and retrospective cohort studies also showed a better outcome for psychotic depression than nonpsychotic depression with ECT treatment.18,19 However, these studies had various limitations including small sample sizes,18 no use of right-unilateral (RUL) electrode placement,19 and often were conducted several decades ago using old ECT technologies such as sinusoidal pulse waves.20 Similarly, baseline differences in the characteristics of patients with and without psychotic depression were not accounted for in analyses of treatment outcomes in MD-P with ECT—such as older age and greater baseline severity among those with MD-P.19 Therefore, the commonly held view that ECT is more effective for MD-P compared to MD-NP may be related to these confounding factors, which is reflected in conflicting results from meta analyses regarding presence of psychosis as a predictor of outcome.21,22 In addition to uncertainty about efficacy, differences in tolerability between MD-P and MD-NP have not been examined in the literature for those treated with ECT. Given the importance of these side effects in the informed consent decision-making process, this is an important knowledge gap to address.23
As such, we hypothesized that patients with MD-P would respond better to ECT treatment compared to patients with MD-NP, while there would be no difference in adverse cognitive effects between the two groups. To address existing knowledge gaps and test our hypothesis, our study compared (1a) ECT treatment response and (1b) adverse cognitive effects between patients with MD-P and MD-NP while also accounting for differences in patient characteristics. We also aimed to explore potential factors associated with (2a) treatment response or (2b) adverse cognitive effect in these groups of patients following ECT.
METHODS
Study Design and Subjects
This study was conducted at the Centre for Addiction and Mental Health (CAMH), a tertiary psychiatric specialty hospital with approximately 550 inpatient beds, in Toronto, Canada. A chart review of all referrals to the CAMH ECT program from June 2010 to September 2021 was conducted. From the ECT referral forms completed by the referring psychiatrist, we obtained the following data: psychiatric diagnosis, psychotropic medications at time of referral, baseline clinical global impression of illness severity, admission status (voluntary vs involuntary), capacity, and ECT indication. This information was verified by a review of the patient’s medical record. The study was approved by the CAMH research ethics board.
Patients were included if they met the following criteria: (1) a diagnosis of MDD with or without the presence of psychotic symptoms and (2) they received at least 1 ECT treatment on the inpatient unit as part of an acute treatment course. Patients were excluded if they were diagnosed with bipolar disorder or any primary psychotic disorder (eg, schizophrenia).
ECT Technique
Electrode placement was determined by the ECT psychiatrist based on variables such as risk of adverse cognitive effects, need for rapid response, and previous treatment protocols. The majority of patients received general anesthesia with methohexital 0.5–1.0 mg/kg IV and succinylcholine 0.25–0.75 mg/kg IV as the paralytic agent. Occasionally, propofol or etomidate were used as anesthetic agents, though this occurred in <1% of procedures. Rescue medications were used as needed for hypertension, nausea, and agitation. The ECT machine used was a MECTA spectrum 5000Q. All protocols employed a fixed 800 milliamps parameter setting. For all bitemporal (BL) treatment sessions, a 1.0 millisecond (ms) pulse width was used. The majority of RUL treatment sessions used an ultrabrief pulse with of 0.3–0.37 ms, though a small number of treatment courses used a standard pulse width of 1.0 ms. The stimulus dose titration method was used to determine seizure threshold in all patients. For determination of threshold, an adequate seizure was defined as a seizure lasting at least 15 seconds based on motor manifestation to ensure the seizure had generalized. After the threshold was determined, stimulus intensity was set at 1.5 times the seizure threshold for BL and 6 times the seizure threshold for RUL treatments. Patients receiving treatment with lithium or anticonvulsant medications were advised to taper these prior to treatment, with the exception of patients with a seizure disorder for whom anticonvulsant medications were indicated.
Assessment of Treatment Response
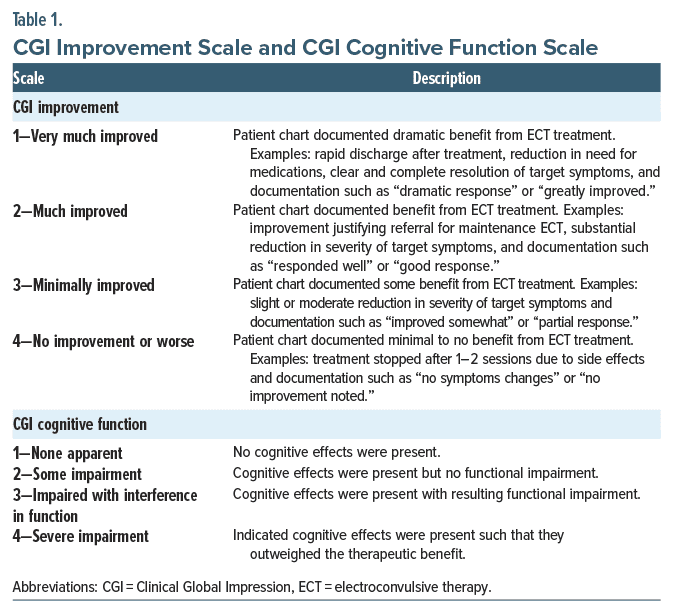
All patients who received at least 1 ECT treatment were eligible for assessment of treatment response. ECT response was determined based on referring clinician assessment of the Clinical Global Impression Improvement scale (CGI-I). Where this was not available, it was estimated using methods from previous work.24,25 Prior work assessing the reliability of between clinician and chart review CGI-I has demonstrated good agreement.24,25 Details regarding the CGI-I chart review methodology are available in Table 1.
Assessment of Adverse Cognitive Effects
Adverse cognitive effects were rated on a similar 4-point CGI scale of severity by referring physicians (Table 1). Where required, chart reviews for assessment of treatment cognitive effects were completed by the 2 primary authors (G.C.L. and R.S.K.).
Data Analysis
Descriptive analyses. We descriptively compared patient characteristics, clinical indications, admission status, patient capacity, ECT treatment characteristics, treatment response, and adverse cognitive effects in individuals with MD-P and MD-NP. We compared continuous data with a Student t test to compare means and categorical data with χ2 analysis or Fisher exact test (in the case of small sample sizes). Descriptive analyses were conducted using only the first course of ECT in the observation period.
Multivariable analyses. To determine the association between psychotic symptoms and treatment outcome while accounting for baseline characteristics that may also impact treatment outcomes (ie, confounders), we used logistic regression models. For treatment response, we defined the outcome variable using the CGI-I. Response was defined as a CGI-I score of 1 and treatment nonresponse as CGI score of 2, 3, or 4. This threshold was selected as a CGI-I score of 1 corresponds to remission in depression,26 which is the primary goal of depression treatment.27 For adverse cognitive effects, the outcome variable was defined as the presence (cognitive CGI of 3 or 4) or absence (cognitive CGI of 1 or 2) of clinically significant adverse cognitive effects. The covariates for both models were the same in that they included all available baseline characteristics that could serve as potential confounders. This included age, sex, presence of psychotic symptoms (yes/no), voluntary vs involuntary status, capable vs incapable to consent to treatment, presence of catatonia, symptom severity, intermittent or regular benzodiazepine use, antipsychotic use (yes/no), antidepressant use (yes/no), and indication for ECT (suicidality, pharmacologic noncompliance, intolerance to medications, failure of pharmacologic treatment, history of prior response to ECT, and patient preference). All categorical covariates were assessed for sparse data, and where required combined into larger groups or, if not possible, then removed from the regression model. We included repeat courses of ECT for the same individual by using a generalized estimating equation (GEE) approach with an exchangeable correlation structure to account for the correlation among outcomes arising from within the same patient. We conducted a complete case analysis given there was minimal missing data (<1%). We assessed for multicollinearity in our model to ensure variance inflation factor was <10 for all covariates included in the model. We also assessed model discrimination using the c statistic and model fit using the Hosmer-Lemeshow test. The regression model for this work was considered to be an explanatory, rather than predictive, model, and as such all covariates were included in the final model (ie, no variable selection procedures were performed) given their theoretical potential to confound the exposure (MD-P present or absent) and outcomes (treatment response or adverse cognitive effects).28 The primary covariate of interest from this model was the presence or absence of psychotic symptoms, which represents the effect of psychotic symptoms after accounting for all observed characteristics, though the effects of other covariates were reported as exploratory outcomes. As a sensitivity analysis, we also completed an analysis in which we adjusted for only 3 key confounders: age, sex, and hospitalization status.
All analyses were conducted using R (R Version 4.1.3 (2022-03-10)). Regression models were performed using the geepack package (Version 1.3.9).29 Results were reported as odds ratios (ORs), and an α of 0.05 was used. This study was reported in agreement with the STROBE guidelines (available from corresponding author upon request).
RESULTS
Demographics and Treatment Characteristics
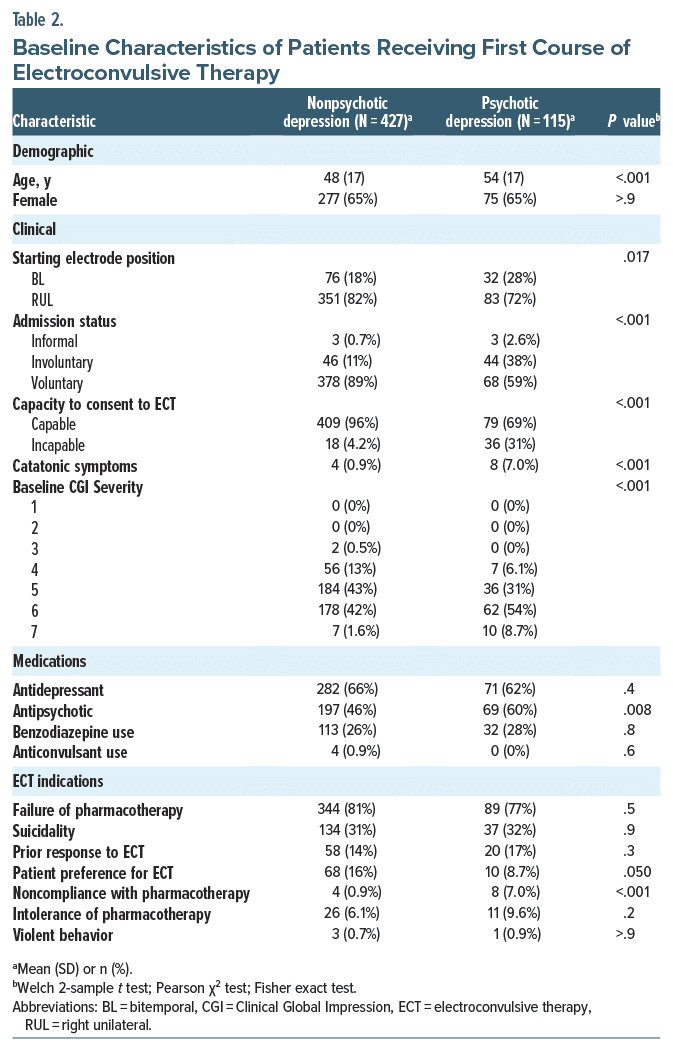
This study included 542 patients who received acute ECT as treatment for depression of which 115 (21%) had MD-P while 427 (79%) had MD-NP (Table 2). Individuals with MD-P compared to MD-NP were typically older (54 vs 48 years, respectively, P < .001), more likely catatonic (7.0% vs 0.9%, respectively, P < .001), involuntary (38% vs 11%, respectively, P < .001), more likely to be on antipsychotics (60% vs 46%, respectively, P = .008), and incapable to consent to ECT (31% vs 4%, respectively, P < .001). Individuals with MD-P also had higher baseline symptom severity as measured by the baseline CGI severity score. There was no statistically significant difference in terms of sex, antidepressant treatment, benzodiazepine use, or anticonvulsant use.
The primary reason for referral to ECT for both groups was failure of pharmacotherapy (77% MD-P and 81% MD-NP; P = .5). Individuals with MD-P were more likely to be referred due to medication noncompliance (7% vs 0.9%, respectively, P < .001) and receive bilateral electrode placement (28% vs 18%, respectively, P = .017). In contrast, individuals with MD-P were less likely to be referred due to patient preference (8.7% vs 16%, P = .05). There was no statistically significant difference between groups for other referral indications.
Descriptive Outcomes
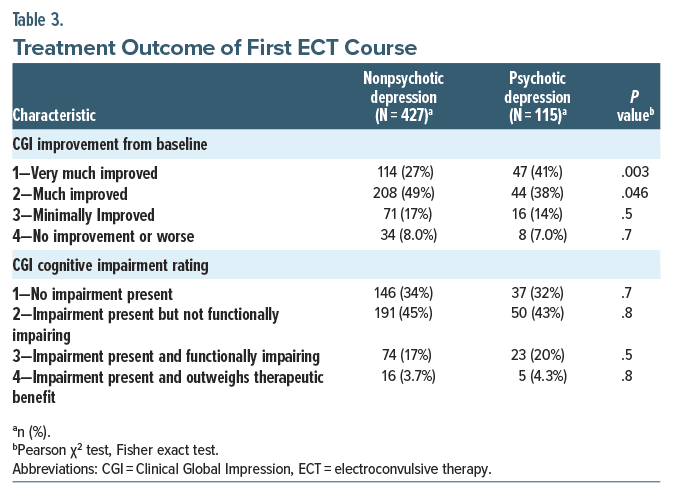
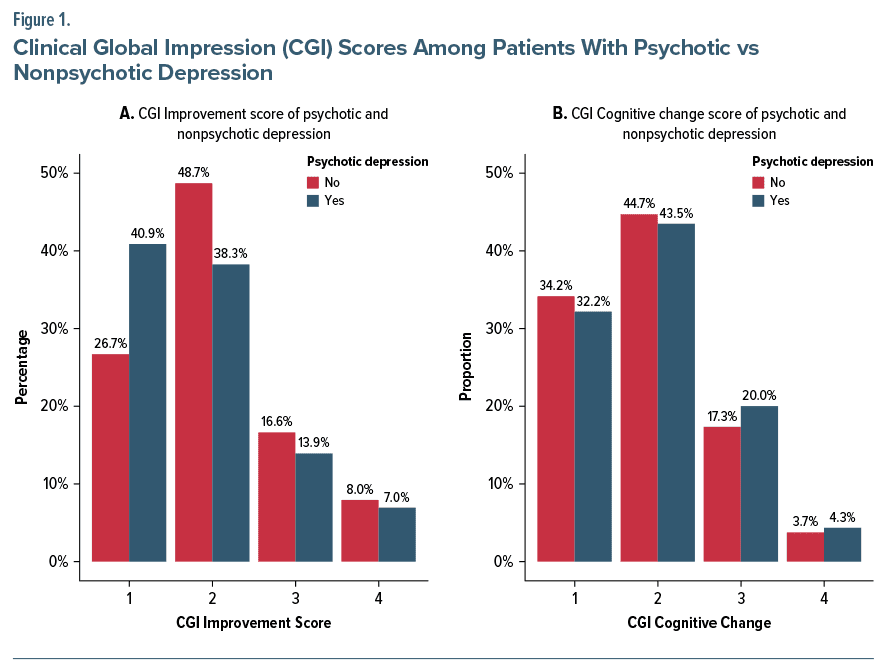
Table 3 displays the treatment and cognitive outcomes for individuals with and without psychotic depression receiving ECT. Individuals with MD-P were significantly more likely to achieve a CGI-I score of 1 (“very much improved”) (27% MD-NP vs 41% MD-P; P=.003), while individuals with MD-NP were significantly more likely to achieve a CGI-I score of 2 (“much improved”) (49% MD-NP vs 38% MD-P; P=.046). In contrast, adverse cognitive effects associated with ECT were similar in both groups, with clinically significant adverse cognitive effects (cognitive CGI of 3 or 4) being nearly identical in both groups (21% MD-NP vs 24% MD-P; P >.05). Refer to Figure 1 for a graphical depiction of the CGI improvement and cognitive scores among patients with psychotic vs nonpsychotic depression.
Multivariable Models
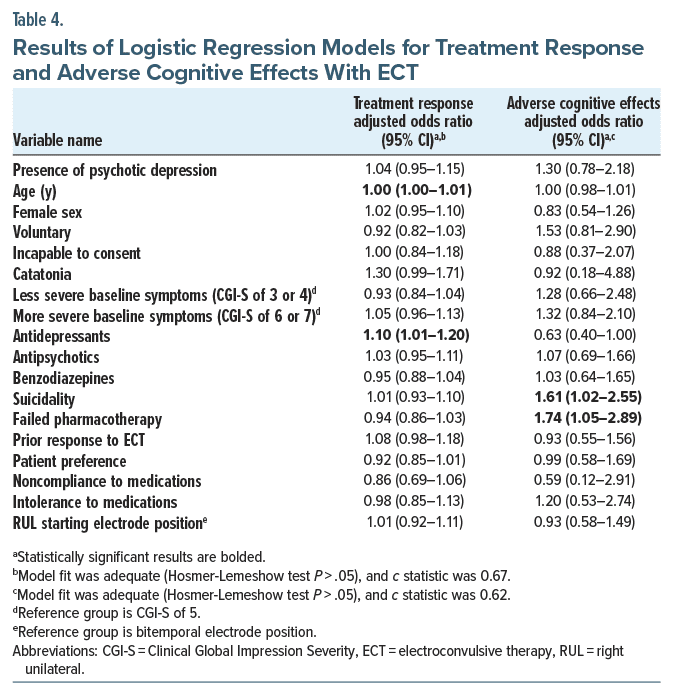
Treatment response. Table 4 presents the results from the multivariable regression model for treatment response. Presence of psychotic symptoms did not have a statistically significant impact on treatment response with ECT (adjusted OR [AOR]: 1.04; 95% CI, 0.95–1.14). In our sensitivity analysis using a model with only age, sex, and hospitalization status as confounders, we found a similar effect size estimate regarding the effect size of psychotic symptoms (AOR: 1.04; 95% CI, 0.96–1.14). In the complete model, age had a statistically significant, albeit minimal, impact on treatment response (AOR: 1.003; 95% CI, 1.00–1.005). The presence of antidepressant treatment was associated with increased odds of treatment response (AOR: 1.10; 95% CI, 1.01–1.20). The presence of catatonic symptoms was associated with increased odds of treatment response, though it was not statistically significant (AOR: 1.30; 95% CI, 0.99–1.71).
Adverse cognitive effects. Table 4 presents the results from the multivariable regression model for adverse cognitive effects from ECT. Presence of psychotic symptoms did not have a statistically significant impact on the adverse cognitive effects after ECT (AOR: 1.30; 95% CI, 0.78–2.18). In our sensitivity analysis using a model with only age, sex, and hospitalization status as confounders, we found a similar effect size estimate regarding the effect size of psychotic symptoms (AOR: 1.29; 95% CI, 0.80–2.09). In the complete model, there was an increased odds of adverse cognitive effects associated with the presence of suicidality (AOR: 1.61; 95% CI, 1.02–2.55) and failed pharmacotherapy (AOR: 1.74; 95% CI, 1.05–2.89).
DISCUSSION
In the largest cohort study to date comparing treatment outcomes between individuals with MD-P and MD-NP receiving ECT, our work identified several clinically important outcomes. We found that among those with MD-P compared to MD-NP, ECT is associated with higher rates of dramatic treatment responses with similar rates of adverse cognitive effects. However, once baseline group differences are accounted for, the presence of psychotic symptoms is no longer predictive of treatment response, and, instead, characteristics like age, antidepressant treatment, and potentially catatonic symptoms are more strongly associated with treatment response. Similarly, analyses accounting for group differences failed to find an association of psychotic symptoms with adverse cognitive effects.
The current work is consistent with the seminal study conducted by the CORE Group comparing MD-P and MD NP, which, in unadjusted analyses, found a significantly greater remission rate among those with MD-P compared to MD-NP (95% vs 83%, respectively).19 However, our study differed in that only 41% of those with MD-P and 27% of those with MD-NP achieved a CGI-I score corresponding to remission.26 This substantially lower remission rate may be a temporal effect, similar to what has been seen in studies examining pharmacotherapy clinical trials over time.30 Moreover, two recent high-profile trials using ECT have not been able to replicate the dramatic remission rates of older studies. The ELEKT-D study comparing ECT with ketamine found a 21.8% remission rate in ECT measured using the Montgomery-Asberg Depression Rating Scale (MADRS), and a study comparing ECT with magnetic seizure therapy found a 26% remission rate.31,32
Regarding the presence of psychotic symptoms, the prior study by Petrides et al,19 after adjusting for confounders, found that psychotic symptoms were significantly associated with remission status (AOR: 1.22, P < .001). This is distinct from the current study, which failed to find an effect of psychotic symptoms on clinical outcomes. This may be related to the limitations of the regression model used in prior work, which only accounted for age, baseline symptom severity, age at first onset of illness, and number of prior episodes.19 Moreover, a recently published study compared remission rates after ECT in MD-P and MD-NP in late life depression and found greater remission rates in MD-P (68.9 vs 51%). This study also found that presence of psychotic symptoms was significantly associated with remission after controlling for a limited number of confounders (ie, age, sex, and severity of baseline symptoms).23
In contrast, our work suggests that when a broader range of confounders are accounted for, psychotic symptoms alone no longer drive the association with treatment response to ECT. Similar to our findings, a study done in a geriatric population also found greater age, but presence of psychotic symptoms was not related to favorable ECT outcomes even after controlling for putative confounders.33 Consistent with prior work examining ECT responses and adverse cognitive effects, we also found that antidepressant treatment was positively associated with treatment response, which has been reported in other studies.34 Similarly, though not statistically significant likely due to a small sample size (N = 12), there were increased odds of treatment response when catatonic symptoms were present, which is consistent with prior work.35–37 Future work should examine the role of catatonia in response rates to ECT as it is one of the most common indications for ECT.37
It is important to note that despite utilizing a large clinically representative cohort, our study has several limitations. The retrospective design precludes causal interpretation between the variables and highlights the need for well-conducted prospective studies. Similarly, the inability to blind outcome assessment may introduce bias into the assessments. Another source of potential bias is unmeasured confounding (ie, variables not available in our dataset) that could have an important influence on our results such as the degree of treatment resistance. The outcome assessments used in this study were also global measures (eg, Clinical Global Impression scales)38 rather than other commonly used, clinician-rated, symptom-specific, depression scales including the Hamilton Depression Rating Scale or the MADRS. While this approach allows for use in routine clinical practice and facilitates large sample sizes, it does not allow for assessments of specific symptom domains such as affective symptoms or psychotic symptoms. Similarly, for measuring adverse cognitive effects, we relied on global subjective ratings reported by treating psychiatrists rather than validated, standardized assessment tools such as the ElectroConvulsive Therapy Cognitive Assessment tool.39
Clinical Implications
Our study provides clinically relevant evidence regarding the treatment of both MD-P and MD-NP. Our findings suggest that individuals with MD-P are more likely to display a significant treatment response, but that this effect may not necessarily be due to psychotic symptoms and may be related to associated patient and treatment factors such as age, concomitant medication treatment, and presence of catatonic symptoms. Encouragingly however, our findings indicate that the cognitive profile of ECT in both MD-P and MD-NP is similar. Taken together, our work supports the important role of ECT in the treatment of both MD-P and MD-NP. Further research consisting of prospective clinical trials using validated scales of symptom severity and cognitive assessments is warranted to better understand the underlying differences between MD-P and MD-NP and to refine treatment strategies for these distinct clinical entities.
Article Information
Published Online: January 29, 2025. https://doi.org/10.4088/JCP.24m15399
© 2025 Physicians Postgraduate Press, Inc.
Submitted: April 22, 2024; accepted November 1, 2024.
To Cite: Kelkar R, Liu GC, Goodman MS, et al. Clinical effectiveness of electroconvulsive therapy for psychotic vs nonpsychotic depression: a cohort study. J Clin Psychiatry. 2025;86(1):24m15399.
Author Affiliations: Department of Psychiatry, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada (Kelkar, Liu, Al-Hashemi, Blumberger, Kaster); Temerty Centre for Therapeutic Brain Intervention, Centre for Addiction and Mental Health, Toronto, Ontario, Canada (Kelkar, Goodman, Blumberger, Kaster); Department of Psychiatry, Yale University School of Medicine, New Haven, Connecticut (Rhee); VA New England Mental Illness, Research, Education and Clinical Center (MIRECC), VA Connecticut Healthcare System, West Haven, Connecticut (Rhee); Department of Public Health Sciences, University of Connecticut School of Medicine, Farmington, Connecticut (Rhee).
Corresponding Author: Daniel M. Blumberger, MD, MSc, Centre for Addiction and Mental Health, 1025 Queen St W, Toronto, ON M6J 1H4, Canada ([email protected]).
Kelkar and Liu are shared first authors.
Blumberger and Kaster are shared senior authors.
Relevant Financial Relationships: The authors declare that there are no conflicts of interest in relation to the subject of this study. Dr Rhee serves as a review committee member for Patient-Centered Outcomes Research Institute (PCORI) and Substance Abuse and Mental Health Services Administration (SAMHSA) and has received honoraria payments from PCORI and SAMHSA; has served as a stakeholder/consultant for PCORI and received consulting fees from PCORI; serves as an advisory committee member for International Alliance of Mental Health Research Funders (IAMHRF); is currently a co-editor-in-chief of Mental Health Science and has received honorarium payments annually from the publisher, John Wiley & Sons, Inc. Dr Blumberger receives research support from the Canadian Institutes of Health Research (CIHR), National Institutes of Health—US (NIH), Patient Centred Outcomes Research Institute (PCORI), Brain Canada Foundation, and the Temerty Family through the CAMH Foundation and the Campbell Family Research Institute; received research support and in-kind equipment support for an investigator-initiated study from Brainsway Ltd and was the site principal investigator for 3 sponsor-initiated studies for Brainsway Ltd; received in-kind equipment support from Magventure for investigator-initiated studies; received medication supplies for an investigator-initiated trial from Indivior; is a paid Scientific Advisor for Sooma Medical; has participated in an advisory board for Janssen; and has participated in an advisory board for Welcony Inc. Dr Kaster receives research support from the Canadian Institutes of Health Research (CIHR) and the AFP Innovation Fund. The other authors report no relevant financial relationships.
Funding/Support: This study was funded in part through the Ontario Ministry of Health and Long Term Care AFP Innovation Fund. Dr Rhee was supported in part by the National Institute on Aging (NIA) (#R21AG070666; R21AG078972), the National Institute of Mental Health (#R21MH117438), the National Institute on Drug Abuse (#R21DA057540), and the Institute for Collaboration on Health, Intervention, and Policy (InCHIP) of the University of Connecticut. Dr Blumberger was supported in part by #R01MH112185. Dr Kelkar was supported in part by #R01MH11285.
Role of the Funders/Sponsors: None of the supporting organizations were involved in the study planning, design, implementation, or reporting.
Clinical Points
- Individuals experiencing major depression with psychotic features (MD-P) had higher response rates to electroconvulsive therapy (ECT) than those without psychotic features (MD-NP) and similar rates of adverse cognitive effects.
- After adjustment for confounders, the presence of psychotic symptoms no longer predicted ECT treatment response, but rather was predicted by age and antidepressant treatment.
- ECT is effective for multiple forms of depression (MD-P and MD-NP), but the dramatic responses observed in MD-P may be at least partly related to confounders.
Editor’s Note: We encourage authors to submit papers for consideration as a part of our Early Career Psychiatrists section. Please contact Joseph F. Goldberg, MD at Psychiatrist.com/contact/goldberg.
References (39)

- Alonso J, Petukhova M, Vilagut G, et al. Days out of role due to common physical and mental conditions: results from the WHO World Mental Health surveys. Mol Psychiatry. 2011;16(12):1234–1246.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. PubMed
- Baldwin RC, Jolley DJ. The prognosis of depression in old age. Br J Psychiatry. 1986;149:574–583.
- Lebowitz BD, Pearson JL, Schneider LS, et al. Diagnosis and treatment of depression in late life. Consensus statement update. JAMA. 1997;278(14):1186–1190. PubMed
- Ohayon MM, Schatzberg AF. Prevalence of depressive episodes with psychotic features in the general population. Am J Psychiatry. 2002;159(11):1855–1861. PubMed
- Johnson J, Horwath E, Weissman MM. The validity of major depression with psychotic features based on a community study. Arch Gen Psychiatry. 1991;48(12):1075–1081.
- Andreescu C, Mulsant BH, Peasley-Miklus C, et al. Persisting low use of antipsychotics in the treatment of major depressive disorder with psychotic features. J Clin Psychiatry. 2007;68(2):194–200.
- Rothschild AJ, Winer J, Flint AJ, et al. Missed diagnosis of psychotic depression at 4 academic medical centers. J Clin Psychiatry. 2008;69(8):1293–1296. PubMed
- Gournellis R, Tournikioti K, Touloumi G, et al. Psychotic (delusional) depression and completed suicide: a systematic review and meta-analysis. Ann Gen Psychiatry. 2018;17:39.
- Farahani A, Correll CU. Are antipsychotics or antidepressants needed for psychotic depression? A systematic review and meta-analysis of trials comparing antidepressant or antipsychotic monotherapy with combination treatment. J Clin Psychiatry. 2012;73(4):486–496.
- Flint AJ, Meyers BS, Rothschild AJ, et al. Effect of continuing olanzapine vs placebo on relapse among patients with psychotic depression in remission: the STOP-PD II randomized clinical trial. JAMA. 2019;322(7):622–631. PubMed
- Meyers BS, Flint AJ, Rothschild AJ, et al. A double-blind randomized controlled trial of olanzapine plus sertraline vs olanzapine plus placebo for psychotic depression: the Study of Pharmacotherapy of Psychotic Depression (STOP-PD). Arch Gen Psychiatry. 2009;66(8):838–847.
- Wijkstra J, Burger H, van den Broek WW, et al. Long-term response to successful acute pharmacological treatment of psychotic depression. J Affect Disord. 2010;123(1–3):238–242.
- Leadholm AKK, Rothschild AJ, Nolen WA, et al. The treatment of psychotic depression: is there consensus among guidelines and psychiatrists? J Affect Disord. 2013;145(2):214–220.
- Dubovsky SL, Ghosh BM, Serotte JC, et al. Psychotic depression: diagnosis, differential diagnosis, and treatment. Psychother Psychosom. 2021;90(3):160–177.
- Milev RV, Giacobbe P, Kennedy SH, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. Neurostimulation treatments. Can J Psychiatry. 2016;61(9):561–575.
- Rothschild AJ. Challenges in the treatment of major depressive disorder with psychotic features. Schizophr Bull. 2013;39(4):787–796.
- Birkenhäger TK, Pluijms EM, Lucius SAP. ECT response in delusional versus non delusional depressed inpatients. J Affect Disord. 2003;74(2):191–195.
- Petrides G, Fink M, Husain MM, et al. ECT remission rates in psychotic versus nonpsychotic depressed patients: a report from CORE. J ECT. 2001;17(4):244–253.
- Kho KH, van Vreeswijk MF, Simpson S, et al. A meta-analysis of electroconvulsive therapy efficacy in depression. J ECT. 2003;19(3):139–147.
- Haq AU, Sitzmann AF, Goldman ML, et al. Response of depression to electroconvulsive therapy: a meta-analysis of clinical predictors. J Clin Psychiatry. 2015;76(10):1374–1384. PubMed
- van Diermen L, van den Ameele S, Kamperman AM, et al. Prediction of electroconvulsive therapy response and remission in major depression: meta analysis. Br J Psychiatry. 2018;212(2):71–80.
- Wagenmakers MJ, Oudega ML, Bouckaert F, et al. Remission rates following electroconvulsive therapy and relation to index episode duration in patients with psychotic versus nonpsychotic late-life depression. J Clin Psychiatry. 2022;83(5):21m14287. PubMed
- Kaster TS, Daskalakis ZJ, Blumberger DM. Clinical effectiveness and cognitive impact of electroconvulsive therapy for schizophrenia: a large retrospective study. J Clin Psychiatry. 2017;78(4):e383–e389. PubMed
- Kaster TS, Goldbloom DS, Daskalakis ZJ, et al. Electroconvulsive therapy for depression with comorbid borderline personality disorder or post-traumatic stress disorder: a matched retrospective cohort study. Brain Stimul. 2018;11(1):204–212.
- Leucht S, Fennema H, Engel R, et al. What does the HAMD mean? J Affect Disord. 2013;148(2–3):243–248.
- Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–1917. PubMed CrossRef
- Shmueli G. To explain or to predict? Stat Sci. 2010;25(3):289–310.
- Højsgaard S, Halekoh U, Yan J. The R package geepack for generalized estimating equations. J Stat Softw. 2006;15(2):1–11.
- Furukawa TA, Cipriani A, Atkinson LZ, et al. Placebo response rates in antidepressant trials: a systematic review of published and unpublished double blind randomised controlled studies. Lancet Psychiatry. 2016;3(11):1059–1066. PubMed
- Anand A, Mathew SJ, Sanacora G, et al. Ketamine versus ECT for nonpsychotic treatment-resistant major depression. N Engl J Med. 2023;388(25):2315–2325. PubMed
- Deng ZD, Luber B, McClintock SM, et al. Clinical outcomes of magnetic seizure therapy vs electroconvulsive therapy for major depressive episode: a randomized clinical trial. JAMA Psychiatry. 2024;81(3):240–249.
- Rhebergen D, Huisman A, Bouckaert F, et al. Older age is associated with rapid remission of depression after electroconvulsive therapy: a latent class growth analysis. Am J Geriatr Psychiatry. 2015;23(3):274–282.
- Sackeim HA, Dillingham EM, Prudic J, et al. Effect of concomitant pharmacotherapy on electroconvulsive therapy outcomes: short-term efficacy and adverse effects. Arch Gen Psychiatry. 2009;66(7):729–737.
- Hatta K, Miyakawa K, Ota T, et al. Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23(4):233–235.
- Raveendranathan D, Narayanaswamy JC, Reddi SV. Response rate of catatonia to electroconvulsive therapy and its clinical correlates. Eur Arch Psychiatry Clin Neurosci. 2012;262(5):425–430.
- Unal A, Altindag A, Demir B, et al. The use of lorazepam and electroconvulsive therapy in the treatment of catatonia: treatment characteristics and outcomes in 60 patients. J ECT. 2017;33(4):290–293.
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Rev. 1976. U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976.
- Hermida AP, Goldstein FC, Loring DW, et al. ElectroConvulsive therapy Cognitive Assessment (ECCA) tool: a new instrument to monitor cognitive function in patients undergoing ECT. J Affect Disord. 2020;269:36–42. PubMed
This PDF is free for all visitors!