This Academic Highlights section of The Journal of Clinical Psychiatry presents the highlights of the Southwest Forum on Difficult to Treat Depression: Focus on Approach, Algorithms, and Access, which was held July 11-12, 2024, in Phoenix.
The forum was chaired by Jordan F. Karp, MD, Department of Psychiatry, College of Medicine, University of Arizona, Tucson. The faculty were Roberta D. Brinton, PhD, Center for Innovation in Brain Science, University of Arizona, Tucson, Arizona; Jay C. Fournier, PhD, Department of Psychiatry and Behavioral Health, The Ohio State University, Columbus, Ohio; Lisa Harding, MD, Yale University School of Medicine, New Haven, Connecticut, and Depression MD, Milford, Connecticut; Manish K. Jha, MD, Department of Psychiatry and Center for Depression Research and Clinical Care, University of Texas Southwestern Medical Center, Dallas, Texas; Eric J. Lenze, MD, Department of Psychiatry, Washington University, St. Louis, Missouri; Sanjay J. Mathew, MD, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, Texas; Samantha Meltzer-Brody, MD, MPH, Department of Psychiatry, School of Medicine, University of North Carolina at Chapel Hill; David C. Mohr, PhD, Department of Preventive Medicine and the Center for Behavioral Intervention Technologies, Northwestern University Feinberg School of Medicine, Chicago, Illinois; Patricio Riva-Posse, MD, Department of Psychiatry, Emory University, Atlanta, Georgia; Ilse Wiechers, MD, MPP, MHS, Office of Mental Health, Veterans Health Administration, Washington, DC, and Department of Psychiatry and Behavioral Sciences, San Francisco School of Medicine, University of California, San Francisco, California; and Nolan R. Williams, MD, Department of Psychiatry, Stanford University, Palo Alto, California.
Financial disclosures appear at the end of the article.
J&J Innovative Medicine Neuroscience provided unrestricted financial support for the forum on which this Academic Highlights is based. The faculty acknowledges Miriam Opara, PharmD, for editorial assistance in developing the manuscript. The opinions expressed herein are those of the faculty and do not necessarily reflect the views of the publisher, the University of Arizona College of MedicineTucson, or the commercial supporter.
J Clin Psychiatry 2024;85(4):psprmdd2408ah
Published Online: Nov. 25, 2024.
To Cite: Karp JF, Brinton RD, Fournier JC, et al. Difficult to treat depression: focus on approach, algorithms, and access. J Clin Psychiatry. 2024;85(4):psprmdd2408ah.
To Share: https://doi.org/10.4088/JCP.psprmdd2408ah
© 2024 Physicians Postgraduate Press Inc.
The pandemic refocused interest on the burden of depression across the lifespan; the increased efforts to prevent and treat depression are now a priority of health care systems, insurers, patient advocates, digital therapeutic engineers, telemedicine platforms, and community health agencies. However, the challenges of treating depression to remission in adult patients who do not respond to first, second, or third levels of oral pharmacotherapy remain. The increased prevalence of these conditions is at odds with the shrinking psychiatric workforce.
Since addressing difficult to treat depression is situated in a rapidly evolving treatment landscape, The University of Arizona College of Medicine-Tucson Department of Psychiatry organized and hosted the Southwest Forum on Difficult to Treat Depression: Focus on Approach, Algorithms, and Access in July 2024. The Forum convened 11 internationally renowned experts in the science and treatment of depression, in particular difficult to treat depression, for a day of teaching and discussion. Based on their expertise, participants were asked to address one of the following three themes:
- Novel Mechanism Approaches for Difficult to Treat Depression
- What Do I Do Next? Evidence-Informed Algorithms to Get Patients Better Faster
- Access: Providing Comprehensive Depression Care Across the Spectrum of Clinical Severity
Made possible by unrestricted support by J&J Innovative Medicine Neuroscience, the Forum’s mission is to disseminate knowledge about this disease state through this Academic Highlights article and in-depth videos with six of the experts. These “Insights” videos are available at Psychiatrist.com.
The authors hope that after learning from this Academic Highlights and reviewing the linked interviews with the experts, readers will:
- Feel more confident in their care of patients with difficult to treat depression.
- Consider the most strategic, cost-effective, and clinically useful sequencing of interventional treatments.
- Consider issues of social justice, medical complexity, and emerging biomarkers as they implement novel mechanism medications and brain stimulation treatments in patient and family-focused approaches to the care of difficult to treat depression.
Advanced Treatments, Limited Reach: Considering Access and Social Justice in Interventional Psychiatry
Lisa Harding, MD
Nearly one in five adults in the United States experience mental illness at some moment in their life. Major depressive disorder (MDD) continues to be one of the most significant health challenges globally and impacts nearly 9 percent of the population at some time in their life.1 In the Unites States, the estimated 12-month prevalence of medication-treated MDD is 8.9 million adults, with 2.8 million experiencing treatment-resistant depression (TRD). The overall annual economic burden of medication-treated MDD is approximately $92.7 billion, with $43.8 billion linked explicitly to TRD. These findings underscore the disproportionate healthcare costs and unemployment associated with TRD, indicating substantial economic and societal benefits from effective management strategies.2
Effective treatments reduce symptoms, healthcare utilization, and associated costs, but approximately 50% of those with MDD do not respond to their initial antidepressant treatment.1 A considerable number of these patients fail to benefit from subsequent treatment options, ultimately developing TRD. Although there is no universally accepted TRD definition, it is frequently defined as MDD that has not responded to at least 2 different antidepressants of adequate dose and duration.1 The Sequenced Treatment Alternatives to Relieve Depression (STAR-D) clinical trial taught us that switching between medication classes does not yield significant benefits, with one-third of patients continuing to not respond.3 With the emergence of new treatments with novel mechanisms and rapid onset of action, critical analysis of emerging science, safety, and limitations is necessary as these interventions are brought from the lab to the clinic.
With the advance of brain stimulation treatments and novel-mechanism medications, ensuring equitable access to these interventions is essential to uphold medical and social justice. However, accessing mental health treatments remains particularly challenging for marginalized groups, including minoritized, low-income, and immigrant communities.4 Common barriers to mental health care include stigma, lack of available and evidence-based services, and inability to afford services. Ensuring access to care involves providing all communities with timely access to appropriate services. Access to care is the ability to obtain necessary, affordable, convenient, acceptable, and effective health services promptly, including access to qualified, culturally competent providers providing screening, prevention, and treatment.
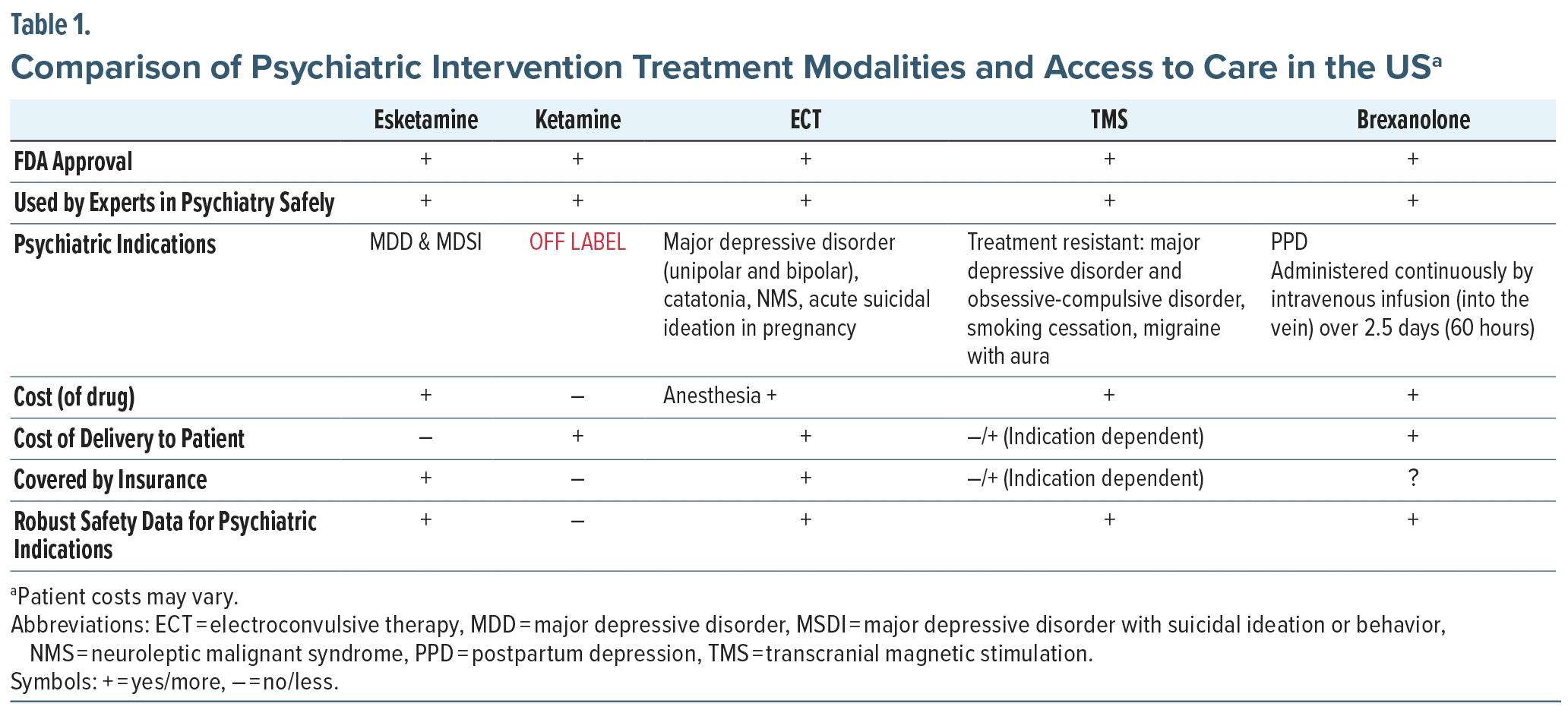
To meet these criteria of equitable access, each intervention must meet all of these criteria when addressing access to care. This is especially pertinent for interventional treatments for MDD, such as transcranial magnetic stimulation (TMS), esketamine, electroconvulsive therapy (ECT), intravenous ketamine, and brexanolone, particularly in relation to indications, medication costs, delivery expenses, and insurance coverage.
Table 1 lists the psychiatric indications, cost of drug, cost of delivery, insurance coverage status, and safety data that are part of the calculus of access and equity in treatment.
Health insurance coverage and formularies play a significant role in determining accessibility of various treatments, especially those treatments which require prior authorizations. Accessing off-label treatments, such as intravenous, intramuscular, and sublingual ketamine, or brain stimulation treatments that are not approved by insurers, presents particular challenges for patients with limited resources. Most insurance carriers, including Medicare and Medicaid, tend to favor coverage of oral medications over procedural interventions, and every insurer requires prior authorizations for these interventional approaches, mandating the documented failure of alternative, less expensive treatments before granting approval.
Additionally, insurers often adhere to outdated guidelines, such as the American Psychiatric Association’s depression guidelines, which have not been updated since 2015.5 This reliance on antiquated protocols further restricts access to newer, potentially more effective treatment options. Consequently, in our shared mission to advance personalized psychiatry and promote medical justice, a thorough understanding of healthcare affordability, effectiveness, and quality is crucial for recognizing both the opportunities and barriers to achieving equitable access to care.
Building the Bridge Between Primary Care and Interventional Psychiatry: The Roles for Patient Navigators and Measurement Based Care
Manish K. Jha, MD
The STAR*D study enrolled more than 4,000 participants, approximately 40% of whom were treated in primary care settings and 60% in psychiatric clinics. A key finding of STAR*D remains that the time it took for individuals to achieve remission was similar whether they received care in primary care or psychiatric settings. This teaches us that various strategies can be employed to manage depression effectively within primary care.6
Less than 20% of patients suffering from TRD achieve remission through the use of standard antidepressants or their combinations. One study revealed that 60% of individuals with TRD were initially prescribed selective serotonin reuptake inhibitors (SSRIs). Mirtazapine and bupropion emerged as the most frequently utilized medications for TRD, followed by escitalopram and venlafaxine. The median duration from the onset of the MDD episode until the index data for TRD was recorded was 552 days. Furthermore, the intervals between the first and second treatments and the second and third treatments were 165 days and 197 days, respectively.7
Approximately one-third of antidepressant prescriptions may be deemed inappropriate, primarily due to off-label usage or the lack of strong scientific evidence for such prescriptions.8 To achieve improved outcomes, it is essential to enhance the recognition of depression, ensure accurate diagnoses, and select suitable medications with appropriate dosages alongside sustained treatment that aligns with evidence-based guidelines. The limited availability of behavioral health resources has prompted the creation of various models that facilitate depression screening and subsequent care within primary care environments. By identifying and effectively managing clinical depression in these settings, both access to and the quality of behavioral healthcare can be enhanced, particularly for minority, low-income, and uninsured populations.8 This methodical approach can minimize clinical inertia and hasten the referral to interventional psychiatry programs for those patients who are not getting well with less intensive treatments.
One study examined treatment approaches and outcomes for outpatients suffering from depression who were treated in primary care settings compared to those in specialty care, utilizing citalopram treatment data from the STAR*D study.9 Participants received 5 recommended treatment visits, standardized pharmacotherapy according to a proscribed algorithm, and continuous support and guidance from a clinical research coordinator. Treatment was delivered using a measurement-based care (MBC) approach that included structured assessments of (1) depressive symptoms, (2) side effects, and (3) adherence at each appointment (with contingency clinical recommendations based on cutoff scores) and a centralized system for treatment monitoring and feedback. The findings of this analysis indicated that when identical approaches to treatment that followed the principles of MBC were administered, the remission and response rates were equivalent in primary and specialty care settings.9
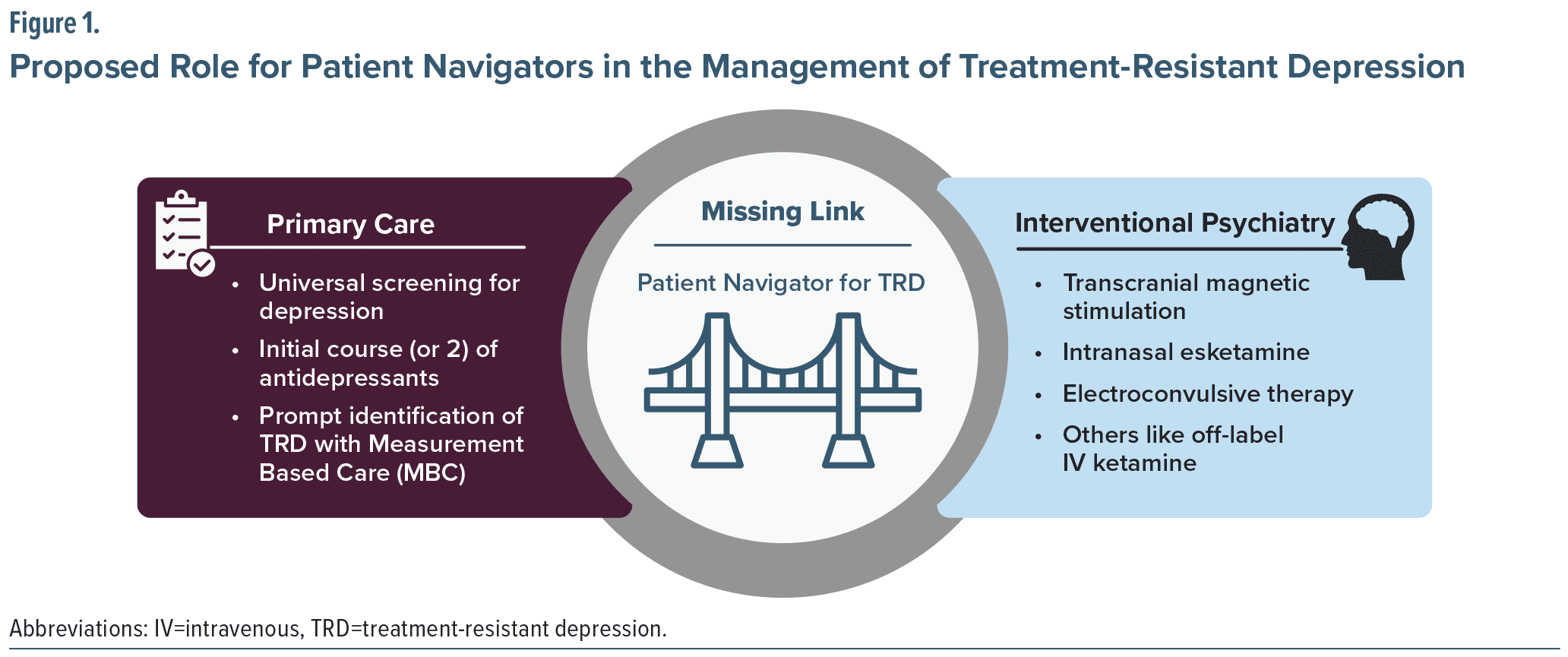
Reviewing the remission rates in the STAR*D trial, 24% of patients attained remission after a single treatment, and 41% achieved remission after 2 treatments. The remaining 60% of patients either did not achieve remission or relapsed as soon as they remitted. Of those who did not achieve sustained remission, 90% were diagnosed with TRD.9 Given that TRD may require alternative interventional psychiatry treatments such as ECT, IV ketamine, intranasal esketamine, and TMS, access to these specialty-clinic and hospital-based treatments creates additional challenges for primary care providers. Deciding which interventional approach to try requires an individualized approach based on patients’ priorities, risk factors, treatment history, and practical issues such as transportation and insurance status.
The implementation of screening tools for mental illness in primary care can be traced back to the 1970s. However, research utilizing these screening instruments in primary care has yielded inconsistent findings, with some evidence indicating that the advantages of diagnosis do not necessarily translate into enhanced outcome measures. In the 1990s, initiatives aimed at quality improvement emerged, concentrating on formulating treatment guidelines for primary care physicians. These guidelines encompassed medication protocols and psychotherapy suggestions. Nevertheless, the mere distribution of these practice guidelines to physicians did not result in universal enhancement of quality of care or improved patient outcomes. In response to relatively poor uptake of these clinical practice guidelines and to improve primary care provider clinical capacity and confidence, extensive efforts have been made in educating and training providers in the diagnosis and management of mental health disorders to improve patient outcomes.10
An alternative, and perhaps more efficient, approach to enhancing the delivery of mental health services within primary care involves augmenting the management of depression and anxiety by specialists. This can be achieved by increasing referrals to external resources or integrating mental health specialists within primary care facilities.11 Co-located care is characterized by two providers operating “in parallel under the same roof.” Collaborative care represents a multifaceted, healthcare system-level intervention that employs care managers to connect primary care providers, patients, and mental health specialists. This model aims to enhance routine screening and diagnosis of depressive disorders, promote evidence-based protocols for proactively managing diagnosed conditions, and bolster clinical and community support for active patient involvement in treatment goal-setting and self-management. Systematic review of randomized controlled trials has shown that collaborative care is superior to usual care in improvement of depression.12
However, efforts to implement collaborative care models in real-world clinical settings have been inconsistent. For example, a large study that implemented a collaborative care model in 75 primary care clinics found no significant difference in remission rates between clinics providing usual care versus those that utilized collaborative care.13 Although primary care providers may be able to provide appropriate care for the majority of patients with depression, especially those with mild to moderate severity, adopting methods to ensure that primary care providers can rapidly connect patients who require higher levels of care to interventional clinics when needed is essential. Patient navigators for TRD that implement an MBC approach may be the missing link to facilitate the seamless (and earlier) integration of interventional psychiatry approaches in the longer-term care of patients with TRD; see Figure 1.
Optimizing Recovery Across the Spectrum of Disease Severity via Comprehensive Care Pathways for Depression: Learning From the OSU Depression Recovery Center
Jay C. Fournier, PhD
Nationally, only a third of patients with diagnosed mental health conditions see a mental health specialist,93 and in a recent simulated patient study, researchers found that they could schedule a new patient visit with fewer than 30% of psychiatrists in a major insurance carrier’s database, with an average wait time for a first appointments of 25 days.94 The Ohio State University (OSU), with funding from the state’s Department of Medicaid, set out to reorganize and reconceptualize care pathways for depression in patients across the entirety of the outpatient severity spectrum. The OSU team developed their services at the Depression Recovery Center to achieve 3 goals: increase access to care, achieve response and remission more efficiently, and increase the sustained remission rate.
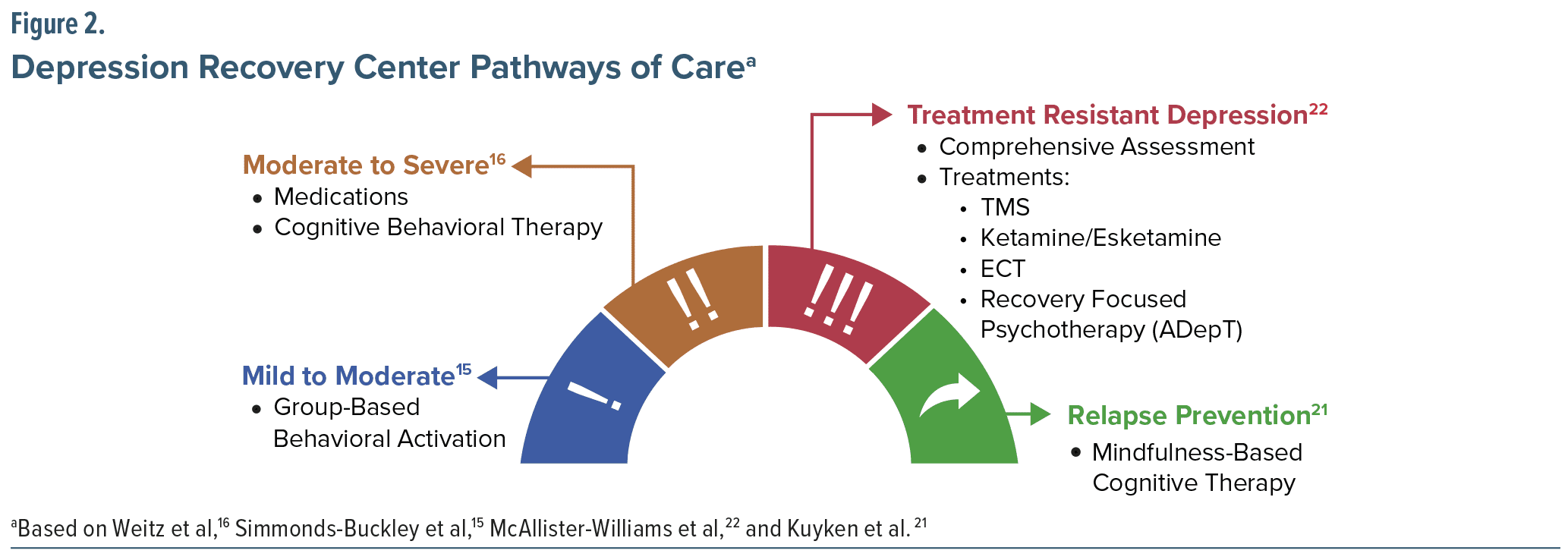
To re-conceptualize the care pathways for depression, the OSU team first described the standard pathway in which patients received standard first-line treatments with medication management, psychotherapy, or a combination. When patients did not respond to first-line treatments, interventional options, such as TMS, ketamine infusion, or ECT, were initiated. The OSU team reorganized the care pathway by breaking the acute treatment phase into 3 pathways: mild to moderate, moderate to severe, and TRD. A short-term relapse prevention intervention was added to increase the rate of sustained remission following acute treatment (Figure 2).
In the new pathway, treatment for mild to moderate depression includes behavioral activation, delivered in a group format. This recommendation is based on evidence from decades of placebo-controlled trials showing little-to-no specific benefit from active treatments compared to placebo for patients in this range.14 Comparatively, a recent meta-analysis suggested that group behavioral activation showed better results than waitlist and treatment as usual and equivalent results to other active treatments.15 Therefore, the most appropriate treatment for these patients is triaging them away from resource-intensive treatments and instead providing a group-based, time-limited, effective treatment with relatively few side effects.
Individualized medication management and psychotherapy are reserved for patients with moderate to severe depression. A meta-analysis comparing all head-to-head trials of standalone cognitive behavioral therapy (CBT) versus standalone medications revealed no difference in efficacy between CBT and medication.16 It also observed that the equivalency between CBT and medication is maintained across the severity spectrum.16 Therefore, medication treatment and CBT, both individually and in combination, are utilized for patients with moderate-to-severe depression.
Treatment of TRD was reorganized to start with a comprehensive re-assessment including psychodiagnostic, treatment history, personality, trauma history, functioning, cognitive ability, and medical evaluations. Once the comprehensive assessment is performed, psychologists and psychiatrists evaluate the results and make a consensus diagnosis and treatment recommendations. Treatment approaches include interventional therapies, like TMS, ketamine, ECT, and psychotherapy. There is growing evidence that CBT shows benefits in the TRD population.
Three studies have examined CBT for TRD, demonstrating that adding CBT increased remission rates 6 months later.17–19 Two of those studies followed patients for 12 months and found that the effect of CBT was maintained over 12 months.17,19 Several new psychotherapies, such as Augmented Depression Therapy (ADepT), specifically focus on patients with more chronic, anhedonic depression to help them increase positive affect, functional recovery, and well-being. A pilot study comparing CBT and ADepT in patients with TRD suggested that ADepT was at least as good as CBT at reducing depression and offered patients a 50% chance of increasing well-being more than did CBT.20
The addition of a targeted relapse prevention intervention as a final pathway out of the OSU Depression Recovery Center is important because depression tends to be a relapsing disorder. Group-delivered mindfulness-based cognitive therapy (MBCT) is recommended for relapse prevention. A recent meta-analysis showed that MBCT at the end of treatment does have a relapse prevention effect compared both to no MBCT and to other active treatment options.21
The OSU Depression Recovery Center is an example of the strategic use of evidence-based resources to improve depression care and perhaps is feasible only because (1) of the investment by the Ohio Medicaid program and (2) they are part of a relatively well-resourced tertiary care academic medical center. While this aspirational and comprehensive approach may not be feasible for many clinics and hospitals, especially in developing countries, it is a model from which payors, patient advocates, and providers may choose to implement certain components, as they strive to meet the depression care needs of their communities.
When All Else Fails to Provide Relief: The Case for Surgical Neuromodulation Options in Treatment-Resistant Depression
Patricio Riva-Posse, MD
Patients with TRD have higher rates of relapse, with 65% of patients relapsing within 3.1 months after 2 failed trials and 71% of patients relapsing within 3.3 months after three failed treatment trials.3 Following high-quality diagnostic assessments and failing first-line therapy, patients are directed toward various therapeutic alternatives, encompassing pharmacological suggestions, psychotherapeutic approaches, repetitive transcranial magnetic stimulation (rTMS), ECT, ketamine or esketamine therapies, and surgical neuromodulation. Because of two negative multisite trials (terminated for futility but with a number of methodological problems),23 stigma, safety, very limited access, and lack of training in the ongoing care of patients with neuromodulation systems for depression, there persists a reluctance to pursue surgical neuromodulation, with a preference to explore all other available options beforehand. Despite these challenges, deep brain neuromodulation and computer-brain technologies may offer hope for some patients with TRD.
In 2005, inspired by neuroimaging findings that showed increased metabolism in the subcallosal cingulate in depressed mood induction experiments as well as reduction in that metabolism with successful treatments, an initial trial of deep brain stimulation (DBS) implanted leads in that region in 6 patients. Stimulation of white matter tracts adjacent to the subgenual cingulate gyrus was associated with a striking and sustained remission of depression in 4 of 6 patients.24 Since then, DBS has been tested in different targets (eg, ventral capsule/ventral striatum or anterior limb of the internal capsule, nucleus accumbens, medial forebrain bundle, inferior thalamic peduncle) that reached clinical trials but have not yet provided solid evidence. DBS has been approved by the FDA for treatment-resistant OCD under a Humanitarian Device Exemption, and most data for DBS have demonstrated promising long-term data where stable response is maintained over several years.25–27
Vagus nerve stimulation (VNS) uses an electrode attached to the vagus nerve and a pulse generator implanted in the chest wall. VNS received FDA approval for treating depression in 2005 and is indicated for the long-term adjunctive treatment of chronic or recurrent depression in patients 18 years and older who are experiencing major depressive episodes and have not responded adequately to 4 or more appropriate antidepressant therapies. While the initial pivotal trial demonstrated a response rate of nearly 30%,28 the subsequent study noted a more modest response rate. These inconsistent results led to the Centers for Medicare and Medicaid Services revoking coverage for the procedure.
A 5-year observational study of patients with VNS compared with treatment as usual (TAU) showed VNS had better clinical outcomes than TAU, including a significantly higher 5-year cumulative response rate (67.6% compared with 40.9%) and a significantly higher remission rate (first-time remitters, 43.3% compared with 25.7%). VNS does not work acutely but over a period of time, and it is the stability that allows patients to regain their quality of life.29
RECOVER is a large, sham-controlled, randomized trial to evaluate the efficacy of adjunctive treatment with surgically implanted VNS therapy in improving depressive symptoms and health outcomes. Inclusion in RECOVER requires failure of 4 or more adequate antidepressant trials in the patient’s current major depressive episode. Patients included in the trial (n=493) had a mean duration of a current major depressive episode of 17.8 years, and 70.8% had received previous interventional psychiatric treatment, including TMS, ECT, ketamine, or combinations.30 Although results have not yet been published, a recent press release from the study sponsor informed that the primary endpoint concerning the duration of response between active VNS and sham VNS was not achieved.
The press release described, however, that a number of secondary endpoints were clinically significant.92 Medicare will evaluate the totality of evidence to determine coverage in 2025. Several additional surgical options are being investigated for the treatment of TRD, including implantable devices that work like TMS. These implanted devices carry the potential of being less invasive than DBS, invisible, and reversible, and of increasing access to these therapies. These surgical options have the potential to enable new paradigms for clinical therapy.
Surgical interventions for TRD are needed because despite the discovery of new treatment approaches, whether novel pharmacological options or refinement of established treatments, TRD has very high rates of recurrence. This makes the case for sustained continuous delivery of treatment that other noninvasive techniques (ie, TMS or ECT), or intermittent pharmacologic interventions (ie, esketamine), cannot provide. During the next couple of years, there will be clearer indications whether VNS and DBS offer sustained relief for a group of patients who continue to have significant symptomatology and reductions in their quality of life despite appropriate “noninvasive” care.
Managing Late-life Depression in the Era of Clinical Complexity
Eric J. Lenze, MD
The US population curve is shifting to the right, with greater numbers living to advanced age. This means that the practice of geriatric psychiatry is increasingly clinically complex: patients are likely to have co-occurring neurocognitive disorders (such as Alzheimer’s disease); have multiple medical comorbidities such as diabetes, cardiovascular disease, and cancer; and take numerous medications, including psychotropics and other co-prescribed medications (including CNS-active medications). These features of clinical complexity mean that finding an effective and safe psychiatric treatment is more challenging and more important than ever.
Late-life depression (LLD) is a major depressive illness in adults aged 60 and above. Approximately 30% of these patients have treatment-resistant late-life depression (TRLLD), defined as a major depressive episode that persists in spite of 2 or more antidepressant trials that are adequate in dose and duration.31 The features of clinical complexity described above are particularly salient here, as TRLLD is strongly associated with multimorbidity, accelerated cognitive decline, and biological and functional indicators of accelerated aging.31
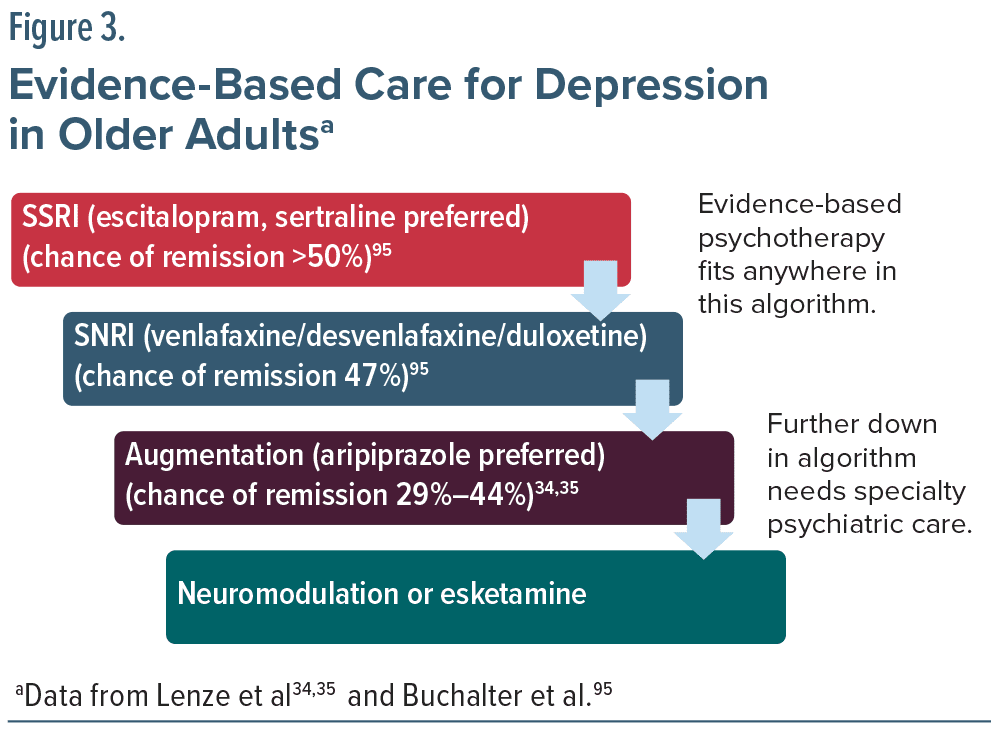
Studies in young or mixed-age adults have looked at antidepressant augmentation or switching strategies for treatment-resistant depression. Two large randomized controlled trials (RCTs) are particularly notable in this respect. First, in the VA Augmentation and Switching Treatments for Improving Depression Outcomes (VAST-D) trial, a large, randomized trial of veterans with treatment-resistant depression (mean age of 54.4 years), augmentation with either aripiprazole or bupropion was slightly more effective than a switch to bupropion.32 Second, the STAR*D trial reported remission rates of 13% to 14% after multiple unsuccessful medication trials.6 These studies included few older adults and those who were included tended to be younger and less medically ill and complex.
In older adults, there has been a concern that augmentation may lead to more adverse effects and a greater risk of drug interactions.33 This safety issue has led to studies focused on TRLLD. In the first, augmentation with aripiprazole was more effective than with placebo for reducing depression and suicidal ideation in individuals whose depression had failed to respond to an adequate trial of venlafaxine XR.34
In the second, the OPTIMUM trial evaluated the advantages and disadvantages of augmentation versus switching strategies for TRLLD.35 Remission rates were greater among patients who were augmented with either aripiprazole or bupropion versus those switched to bupropion, yielding rates of 29%, 28%, and 19%, respectively. Similarly, improvement in psychological well-being was greater with augmentation versus switching. For those patients who did not exhibit improvement in this phase, a second step randomized patients to either lithium augmentation or a switch to nortriptyline, resulting in remission rates of 19% and 21.5%, respectively. The relatively low rates of syndromal remission observed in both phases of the trial underscore the difficulties associated with treating depression following the failure of previous medications.35 In fact, for two of the treatment strategies tested–switch to bupropion in the first step and lithium augmentation in the second step–less than 10% of participants both remitted and stayed on the randomized strategy (eg, if randomized to bupropion switch, they were also still taking only bupropion at an adequate dose at the end of the 10-week step). This finding suggests that these two treatment strategies in particular may be futile for TRLLD.
Moreover, the low rates of remission after 3 failed trials (including 1 augmentation trial) suggest that higher-intensity interventions such as TMS, ketamine/esketamine, or ECT may be needed (Figure 3). The challenge of personalized medicine is to identify those patients earlier in their course of treatment to determine who should be offered brain stimulation or ketamine. Overall, the OPTIMUM trial yielded similar effectiveness findings as the VAST-D and STAR*D trials did in younger adults: there is a place for augmentation, but also low remission rates after multiple failed trials of oral antidepressant pharmacotherapy.
A major question in geriatric psychiatry is whether certain treatments have safety issues that are highly relevant to older adults, such as increasing the risk for falls. The OPTIMUM trial specifically tested safety outcomes and did not find that patients in the augmentation groups had an overall increased likelihood of adverse events than those in the switch groups. However, compared to aripiprazole augmentation, the rate of falls was higher with bupropion augmentation. Falls are a clinically salient outcome in older adults because they frequently lead to serious injuries or even death.
In conclusion, our increasing knowledge about how to treat TRLLD is creating a clinical pathway for better treatment outcomes. Antidepressant trials including augmentation can guide patients to remission using the best and safest treatment option. Still, many older adults with TRLLD, especially those with cognitive impairment and multimorbidity, do not achieve remission with oral medications and are thus at high risk for persistent suffering, suicide risk, and accelerated cognitive decline. These patients need better, and safer, treatment options, which should be the focus of emerging research.
Embracing Technology: Digital Mental Health Treatments for Depression
David C. Mohr, PhD
Digital mental health treatments (DMHTs) use commonly available technologies such as smartphones, browsers, or virtual reality to provide evidence-based psychological strategies to treat common mental health conditions, including depression. A large number of randomized controlled trials have consistently found DMHTs to be effective in treating depression. While fully automated DMHTs, delivered without human support, result in modest improvements, outcomes are significantly stronger when provided with human support and are not inferior to outcomes in psychotherapy.36
Because DMHTs can be accessed at any time, from anywhere, they have the potential to overcome many access barriers to traditional psychological treatments. However, if provided alone, continued use may require intrinsic motivation, which is often low for patients with anhedonia or depression. Dropout rates in RCTs are around 26% but are much higher in real-world use.37,38 Thus, the human support from digital care navigators is important for many patients to initiate engagement and maximize benefit.39 There is no significant difference in outcomes between support provided by trained lay coaches and mental health professionals.40
It is important to distinguish between wellness apps, which support lifestyle change but do not require evidence, and digital therapeutics, which aim to treat or prevent a disease or disorder and are supported by evidence. The FDA’s regulatory policy for digital mental health is evolving. Currently most mental health apps are considered low-risk and fall under “discretionary enforcement,” meaning review is not required. Many companies nevertheless are submitting their DMHTs for FDA approval and clearance. As of this writing, the Centers for Medicare and Medicaid Services have proposed reimbursement codes for DMHT products and human support services.
DMHTs are beginning to be implemented as cost-effective frontline treatments for depression in routine care.41,42 As with any treatment for depression, some patients will not respond adequately to DMHTs and must therefore be integrated into care pathways. DMHTs generally collect standardized assessments, such as the Patient Health Questionnaire-9 (PHQ-9), which can be integrated into electronic medical records and patient registries, facilitating care management. Thus, DMHTs can support measurement-based care, providing symptom assessment at regular intervals, revisions to the treatment plan as needed, and, for patients whose depression is not improving or is getting worse, triaging to higher levels of care.
Smartphones contain networked sensors, which generate and can continuously transmit data that reflect human behavior. Many of these behavioral markers have consistently been shown to be correlated with depression, including features derived from GPS such as time spent at home and number of locations visited and patterns of communication through text messaging.43
Notably, GPS features have shown a unidirectional association, wherein changes in movement patterns precede symptom change, while changes in symptoms do not lead to alterations in movement behaviors, suggesting a causal relationship.44 However, the effect sizes have been modest, in part due to the heterogeneity across populations. For example, while the amount of time spent at home is associated with increased likelihood of depression in many populations, the effect is reversed in low-income populations.45 Behavioral markers may also vary depending on weather, location (eg, urban vs rural, latitude), age, and culture. In addition, depression itself is heterogeneous, making it a difficult target to estimate. It is possible that with larger population-level data that can account for the heterogeneity, passive sensing of mental health conditions may become viable, reducing the reliance on self-report and thereby allowing more timely treatment.
However, passive sensing can detect well-defined behaviors related to depression, such as physical and geographic movement, digital communications, digital tool use, and sleep, which may be useful in DMHT and psychological treatments. Future research with DMHTs should include interventions personalized for those with severe and/or chronic symptoms of depression and studied in combination with brain stimulation and other interventional approaches.
Algorithms for TRD Treatment Success: Lessons from the Veterans Health Administration
Ilse Wiechers, MD, MPP, MHS
The Veterans Health Administration and the Department of Defense have established and refined an algorithm and clinical practice guidelines to identify and manage MDD. The initial segment of the treatment algorithm, Module A, emphasizes the importance of initial assessment and treatment, primarily within a primary care environment, and may include psychotherapy as monotherapy. Subsequently, Module B addresses advanced care management, offering treatment alternatives for patients who have not responded to adequate treatment trials.46
The recommendations prioritize engaging in discussions with patients and making clinical decisions tailored to individual patient characteristics rather than adhering to a generalized recommendation. It is essential to comprehend the challenges and barriers faced by patients to provide optimal treatment options, particularly when considering recommendations for ECT, TMS, ketamine infusions, and emerging novel-mechanism drugs such as psilocybin.46
Although the literature describing head-to-head comparison of interventions for TRD is sparse, a recent study merits note. This project, sponsored by the Patient-Centered Outcomes Research Institute (PCORI), included patients with TRD (without psychosis) who were assigned to receive either 3 weeks of ECT (3 times per week) or IV ketamine (0.5 mg/kg of body weight 2 times per week). Although the study was designed and powered as a noninferiority trial to determine if IV ketamine was as good as ECT for nonpsychotic TRD, the study observed that 55.4% of the patients in the ketamine group met criteria for response (defined as a decrease of at least 50% from baseline in the score on the 16-item Quick Inventory of Depressive Symptomatology–Self-Report) compared to 41.2% of those receiving ECT.47 These results support the effectiveness of IV ketamine for these patients, but do not address the question of what to do next for patients who did not respond to either IV ketamine or ECT. Another PCORI-sponsored noninferiority study is currently underway to evaluate the effectiveness of racemic ketamine versus esketamine in treating depression among individuals with TRD. This study will randomize participants in a 1:1 ratio and monitor them over a 5-year period.48
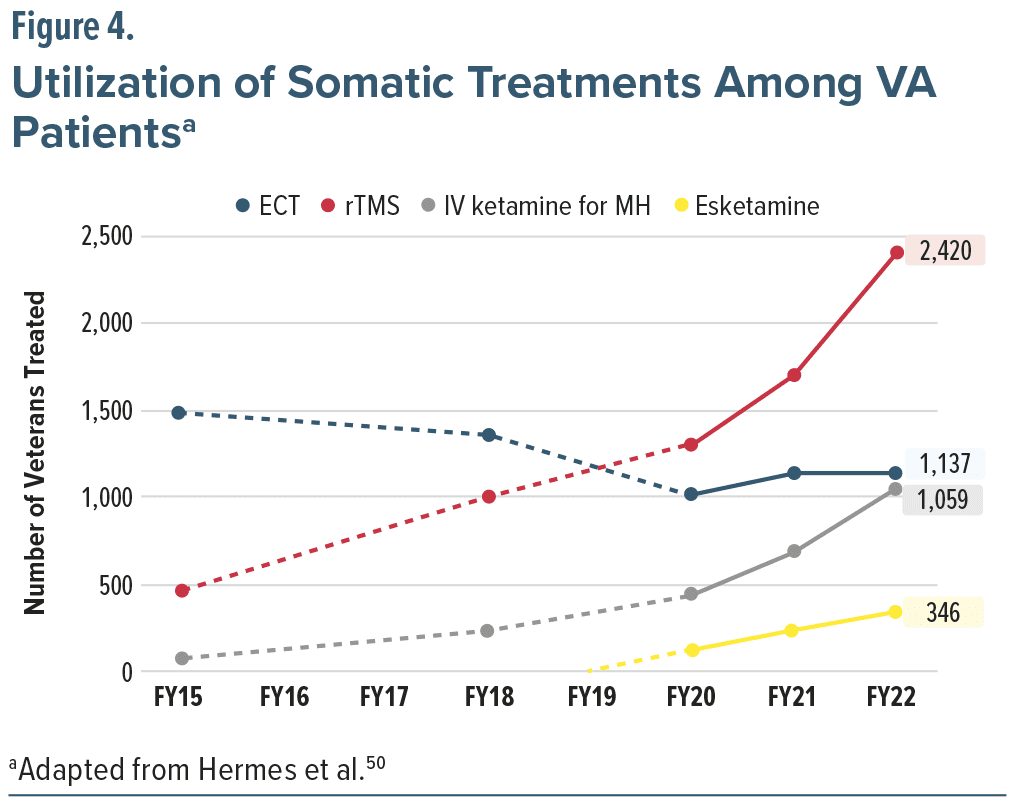
The VA recently completed a national survey to evaluate the availability of somatic treatments for TRD within VA facilities. The emerging patterns over the past several years indicate an increase in the use of TMS, IV ketamine, and esketamine, contrasted with a decline in the use of ECT (see Figure 4). This suggests that patients are asking for these treatments, and clinicians are selecting them instead of ECT. Durability of treatment response, transitions from TMS and ketamine/esketamine to ECT because of relapse or recurrence, and longer-term safety reports are needed to guide iterative refinement of the above-described algorithm.
This work to appreciate the increasing use of ketamine in VA settings is ongoing. An example is a recently published VA study of clinical outcomes associated with IV ketamine treatment for depression. This study reviewed data from 215 patients, who presented with a mean baseline PHQ-9 score of 18.6. These patients had received an average of 2 trials of antidepressant medications in the preceding year and a total of 6 trials over the 2 decades prior to their initial ketamine infusion. These were high-utilizers of healthcare who were living with moderate to severe symptoms: on average, these patients had attended 39 mental health appointments in the 6 months leading up to their first IV ketamine treatment, with 22% requiring psychiatric hospitalization. The patients received an average of 18 ketamine infusions, with approximately 50% demonstrating significant improvement and 26% achieving response. Although only a small proportion of patients treated with IV ketamine for depression attained response or remission, the symptom improvements noted within the initial 6 weeks were maintained for at least 6 months, accompanied by a reduction in the frequency of infusions.49
As the VA is the largest integrated healthcare system in North America, with relatively high prevalence of neuropsychiatric conditions, the leadership of the VA has identified behavioral medicine as a programmatic priority. But to do this in the most patient-centered, safe, and cost-effective way, more research is required to advance treatment algorithms for depression, including TRD, that moves beyond evidence-informed to a truly evidence-based approach to providing depression care for veterans.
Emerging Biomarkers to Advance Precision Psychiatry: EEG Gamma Oscillations as a Prognostic Marker for IV Ketamine in Treatment-Resistant Depression
Sanjay J. Mathew, MD
Ketamine has been recognized as an effective antidepressant; however, there is considerable variability in individual responses to both ketamine and esketamine, with most studies indicating response rates ranging from 35% to 60%. This variability underscores the necessity for a more stratified approach in psychiatry to identify patients who are most likely to benefit from ketamine infusions. At present, there are no established clinical or biological predictors that can reliably forecast a patient’s response to ketamine, leading to clinical practice that often depends on a trial-and-error methodology.51 Previous research has suggested several potential predictive markers for ketamine response, including the severity of depressive symptoms, history of suicide attempts, early onset of depression, a chronic and treatment-resistant course of the disorder, and the presence of dissociative side effects during and after infusion. However, these findings have yielded mixed results.52 While neuroimaging biomarkers for ketamine response remain elusive, three consistent brain-based predictors identified post-treatment include enhanced functional connectivity within the prefrontal cortex, increased activation in the striatum (as measured by arterial spin labeling and task-based functional magnetic resonance imaging [fMRI]), and heightened gamma power measured with electroencephalogram (EEG) in frontoparietal regions. Furthermore, direct electrophysiological measures, such as EEG, provide a noninvasive and cost-effective method for assessing brain function compared to more complex neuroimaging techniques like fMRI and positron emission tomography (PET).52,53
A commonly accepted theory about how ketamine (an NMDA receptor antagonist) treats depression is through its inhibition of activity at GABAergic interneurons, resulting in the disinhibition of GABA activity and a subsequent increase in presynaptic glutamate release. The released glutamate interacts with AMPA receptors, leading to AMPA receptor potentiation and downstream effects on neuroplasticity. This surge in glutamate appears to be a crucial pathway for the acute effects of ketamine. The inhibition of NMDA receptors results in the suppression of GABAergic interneurons, followed by the disinhibition associated with the glutamate surge. This disinhibition can be observed through increases in gamma band power, indicating that gamma serves as a marker for the peak plasma concentration of ketamine.54
The auditory steady-state response is a passive approach to assessing gamma potentiation. An auditory click train lasting 1,000 milliseconds triggers a response that results in a 40-hertz gamma oscillation. Clinical findings have consistently shown that a 0.5 mg per kilogram dosage of ketamine is optimal. During a 40-minute infusion in patients with treatment-resistant depression, monitoring electrodes placed in the frontal region revealed a rapid and significant increase in frontal gamma potentiation, which subsequently normalized over 4 hours.55
Additional studies suggest that ketamine not only increases the amplitude of gamma oscillations but also reduces the activity of theta and alpha waves. In the prefrontal regions, a decrease in depression severity was linked to a reduction in low-frequency neural activity alongside an elevation in high-frequency activity.56 A new study is exploring the relationship between baseline gamma power prior to a course of ketamine treatments and the within-subject effects of ketamine on gamma compared to saline infusions. Low baseline gamma levels may indicate deficits in neuroplasticity. The study aims to assess gamma power during the first and fourth infusions to establish the stability of this biomarker.
Decoding the severity of depression through neural activity deepens our fundamental understanding of its manifestation in the human brain and provides a distinct neural signature for tailored neuromodulation treatments. EEG is utilized to assess target engagement and advance the administration of various medications for mood disorders. Ongoing research seeks to examine the potential of the gamma band response induced by ketamine as a biomarker linked to both rapid and sustained therapeutic effects.
Neurosteroids and Postpartum Depression: The Brexanolone and Zuranolone Journey from Bench to Bedside
Samantha Meltzer-Brody, MD, MPH
Postpartum depression (PPD) is one of the most common complications of childbirth that can profoundly impact both the mother and her infant, affecting approximately 1 in 8 women. The precise etiology of PPD remains unclear and is likely influenced by multiple factors. Tragically, suicide ranks among the leading causes of mortality during the postpartum period.57,58
Various theories regarding the pathophysiology of PPD suggest contributions from endocrine, genetic, epigenetic, synaptic transmission, neural network, inflammatory, neurosteroid, and stress-related mechanisms.59-65
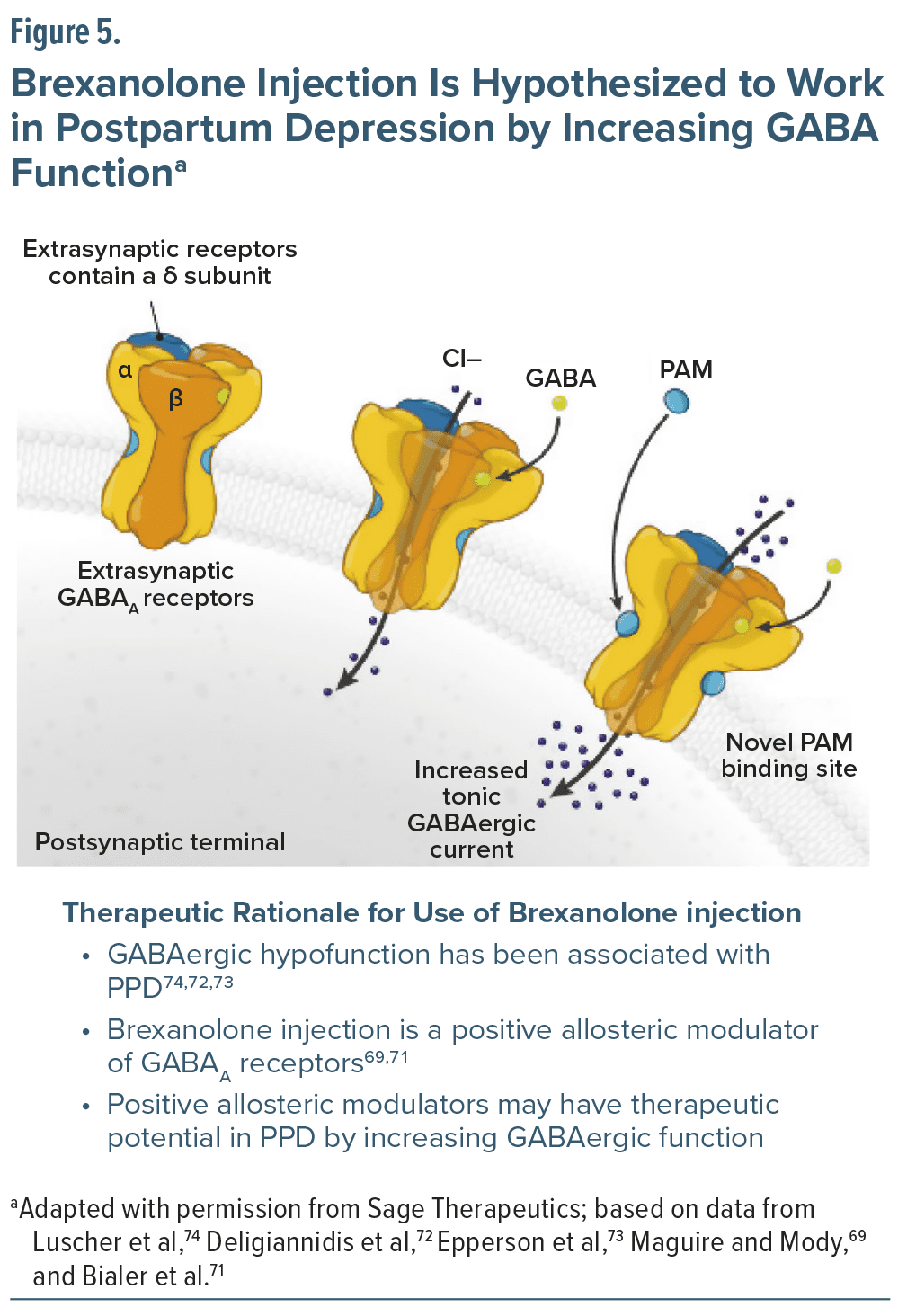
The efficacy of traditional first-line medication treatments for PPD is often limited for patients with PPD, as their therapeutic effects generally manifest after a duration of 4 to 6 weeks. This delay has created a significant demand for innovative pharmacologic therapies that can offer a quicker onset of action and sustained remission of depressive symptoms.66,67 One of the underlying hypotheses of PPD has been GABAergic hypofunction, which developed from the literature on allopregnanolone, the neuroactive metabolite of progesterone and a positive allosteric modulator of GABAA receptors. Brexanolone is a proprietary formulation of allopregnanolone, and the rapid onset of action of the antidepressant effects observed with this novel neuroactive steroid (NAS), GABAA positive allosteric modulator, offers great promise in the treatment of PPD. Specifically, NAS medications aim to address the underlying pathophysiology of PPD by normalizing GABA and NAS levels (Figure 5), thereby alleviating anxiety and symptoms associated with depression.68 Consequently, the observed rapid antidepressant effects and efficacy of brexanolone led to approval by the FDA in March 2019, followed by subsequent development of zuranolone, which received FDA approval for PPD in 2023.
Brexanolone injection, delivered via a 60-hour peripheral IV infusion, is hypothesized to work in PPD by increasing GABA function. Brexanolone has shown a swift reduction in symptoms of PPD across the 3 HUMMINGBIRD trials that employed nearly identical methodologies. These investigations revealed that a single 60-hour infusion of brexanolone led to rapid and statistically significant enhancements in depressive symptoms, as measured by the 17-item Hamilton Rating Scale for Depression (HAM-D) when compared to placebo. Furthermore, brexanolone maintained its efficacy on the HAM-D even after 30 days post-treatment.68,69
The administration of brexanolone is only via an IV infusion and is accessible with a restricted risk evaluation and mitigation strategy (REMS) program, which requires that administration of brexanolone must occur under the supervision of a qualified healthcare professional. This has made uptake of this drug limited due to the complexity and the cost of administration. Adverse reactions observed in brexanolone placebo-controlled studies included excessive sedation and sudden loss of consciousness. Some patients experienced sedation and somnolence that necessitated either a dose interruption or a dose reduction during the infusion. The duration for full recovery from any loss or alteration of consciousness following a dose interruption varied between 15 and 60 minutes. Due to the risk of excessive sedation, the FDA has issued a black box warning, mandating that patients be monitored for 12 hours post-administration of brexanolone.70
The efficacy observed with brexanolone for treatment of PPD provided the critical foundation for development of the oral neuroactive steroid zuranolone. Zuranolone is very similar in structure to brexanolone but has been slightly modified for oral administration. Zuranolone represents the first oral treatment approved for PPD and is a much more convenient formulation for patients compared to the IV administration of brexanolone. Zuranolone is administered once daily for 14 days. The efficacy of zuranolone at 30 mg and 50 mg was established through 2 randomized, placebo-controlled trials known as ROBIN and SKYLARK, respectively. Both studies indicated a statistically significant decrease in 17-item HAM-D score from baseline to 15 days following treatment initiation with zuranolone compared to the placebo group. In the ROBIN study, zuranolone demonstrated a rapid reduction of symptoms as soon as day 3 of therapy. Zuranolone was generally well tolerated, with the most frequently reported adverse effects being somnolence, dizziness, and sedation. There were no indications of loss of consciousness, withdrawal symptoms, or heightened suicidal thoughts associated with its use.75,76
In summary, brexanolone and zuranolone are the first antidepressant medications targeting endocrine perturbations associated with the period after childbirth that have FDA approval for PPD. They have demonstrated efficacy via a new mechanism of action for PPD and provide an effective new treatment option. The ease of administration of the oral drug, zuranolone, given once daily for 14 days, is a major benefit and has led to much wider use since FDA approval. NAS therapy demonstrates a quicker onset of action compared to conventional antidepressants, which is a great benefit during the vulnerable postpartum period.
Hastening Remission Using Personalized Medicine: The Future of Interventional Neuropsychiatry
Nolan R. Williams, MD
Major depressive disorder (MDD) is a leading cause of disability worldwide, affecting nearly 300 million people and resulting in over 700,000 suicides annually.77 Effectively managing MDD is complex, as an estimated 30%-65% of patients fail to achieve remission and are diagnosed with TRD.78
Accelerated, targeted, personalized medicine is transforming neuropsychiatry by offering faster and more precise treatments for individuals with TRD. Tailoring treatment based on an individual’s brain networks may offer more rapid, effective relief in a shorter period of time.
Conventional repetitive transcranial magnetic stimulation (rTMS) is a non-invasive brain stimulation technique with proven effectiveness in modulating brain circuits. rTMS for the treatment of TRD has historically been applied over the course of 6-9 weeks and directed toward the left dorsolateral prefrontal cortex (L-DLPFC) using scalp-based landmarks. This approach has resulted in an effective antidepressant treatment for some patients but with an overall low remission rate of about 35% in moderately treatment-resistant depression, falling to 17% in more treatment-resistant depression.79 Additionally, for patients experiencing a psychiatric emergency, the average inpatient hospital stay is limited to just 1 week, which consequently hinders the use of rTMS in severe cases of TRD, where rapid intervention and initiation of a safe treatment with fast onset of clinical benefit are crucial.80
There have been several recent advancements in the delivery of rTMS for the treatment of TRD. Intermittent theta burst stimulation (iTBS) is a more advanced form of high-frequency rTMS, delivering similar results in a significantly shorter timeframe while proving equally effective in reducing depressive symptoms with similar safety and tolerability. iTBS offers a more efficient option for both clinicians and patients. 81 Further, functional MRI (fMRI) has been implemented to guide targeting and ensure treatment is precisely delivered to the brain region implicated in both symptoms and recovery. Depression is associated with increased functional connectivity between the default mode network (DMN) and the subgenual anterior cingulate (sgACC), and the degree of treatment resistance appears to be associated with a higher degree of sgACC-DMN connectivity. Growing evidence suggests that targeting the left DLPFC reduces hyperactivity in the sgACC and decreases overactivity in the DMN. Precise targeting of this region with rTMS using imaging-based personalized medicine approaches decreases the risk of off-target effects and may maximize clinical benefit.82
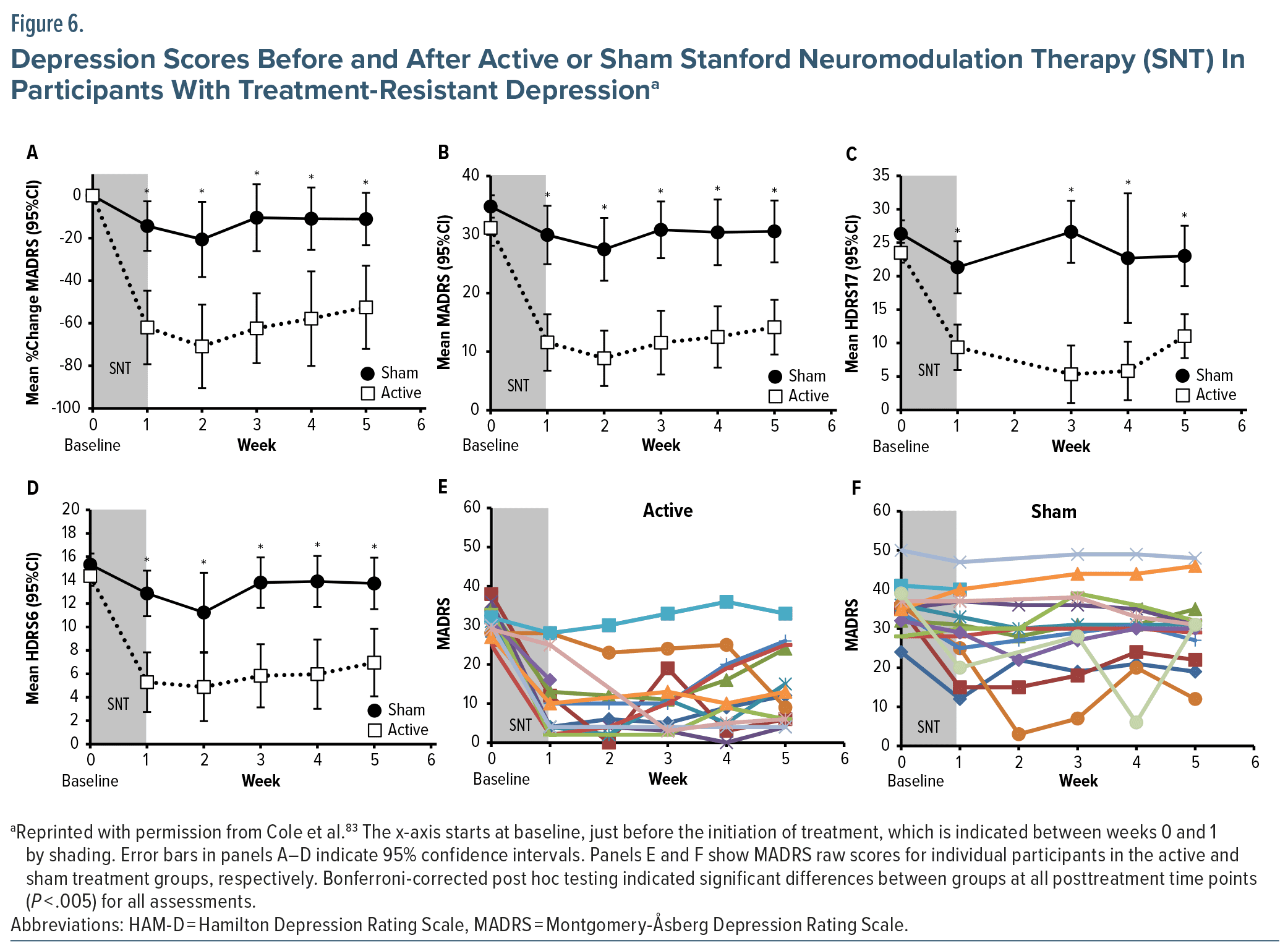
Building on these advances, research at the Stanford Brain Stimulation Lab has resulted in the FDA clearance of an innovative personalized, fMRI-guided TMS treatment for TRD termed Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT). By incorporating individualized brain mapping, SAINT targets specific neurocircuit nodes within the left DLPFC with precision to restore connectivity with the sgACC. As described earlier, in people with MDD, these areas show disrupted connectivity. SAINT has demonstrated high remission rates from depression of 79%-90% (RCT83 and open-label,84 respectively) (Figure 6) and 100% remission from suicidality in patients with TRD following 5 days or fewer of treatment.
SAINT therapy exemplifies the shift toward accelerated, targeted, and personalized treatment in neuropsychiatry. Interventions such as SAINT not only speed up recovery but also enable each patient to receive personalized care specific to their brain networks. This marks a new era in treating TRD as we endeavor to offer more effective relief for patients facing severe and intractable neuropsychiatric conditions.
Transition States and Reprogramming Neural Systems: Lessons from the Midlife Female Brain to Understand the Intersection of Endocrinological Aging, Brain Health, and Depression
Roberta D. Brinton, PhD
Neurological aging is commonly perceived as a straightforward decline; however, it is, in fact, a complex and non-linear phenomenon. This complexity is particularly evident in the female brain during midlife, which is marked by 3 distinct phases: the early chronological phase (pre-menopause), the endocrinological phase (perimenopause), and the late chronological phase (post-menopause). Each of these phases exhibits a unique gene transcription profile. The endocrinological transcriptomic profile has the most significant change in the hippocampus, showing a 10-fold increase compared to changes observed in the hypothalamus. During this period of endocrine aging, the hippocampus experiences substantial transformations in the biological systems that govern bioenergetics.85,86
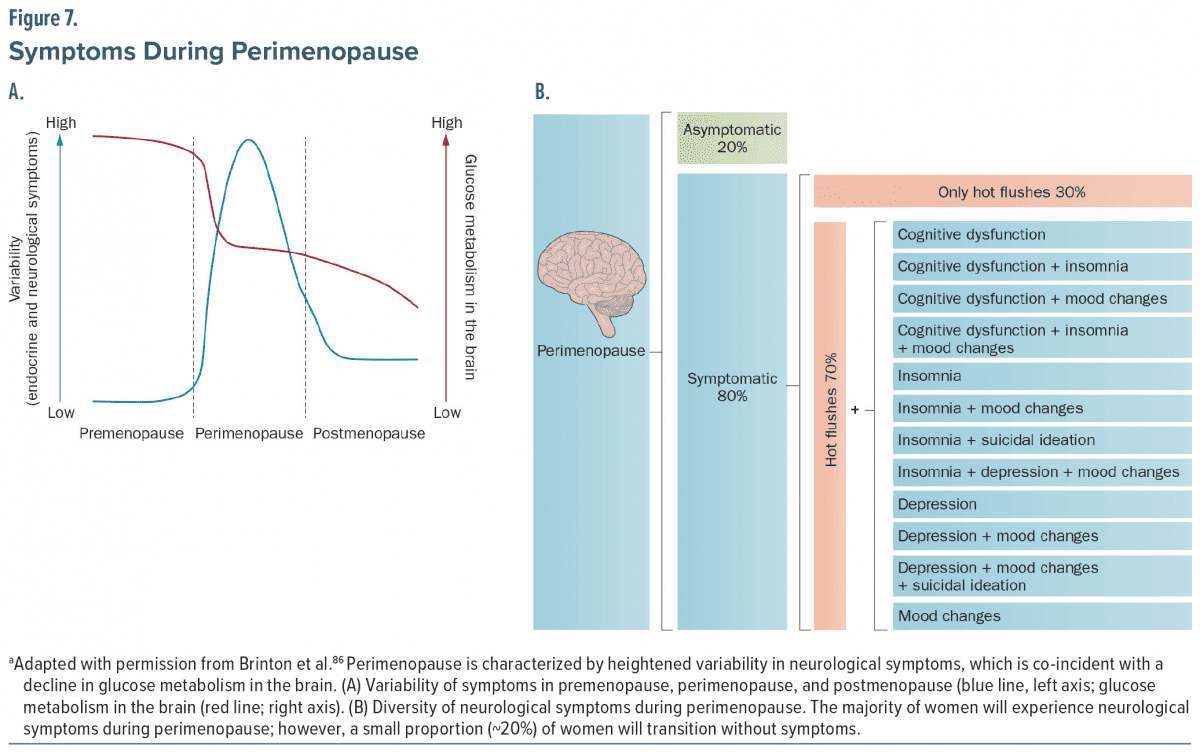
In the pre-menopause phase, variability in brain responses is low. In contrast, perimenopause is characterized by heightened variability in neuropsychiatric symptoms, which coincides with activation of the innate immune system followed by a reduction in brain glucose metabolism, prompting a compensatory mechanism that utilizes alternative energy sources, such as lipids and ketone bodies (Figure 7). The shift in fuel reliance places the brain’s largest reservoir of local fatty acids, namely white matter, at risk of being catabolized as lipids that may be used to produce ketone bodies via astrocytic beta-oxidation. This process leads to the generation of myelin debris and triggers a response from microglia, which recognize this debris as foreign, leading to activation of the adaptive immune system, infiltration of peripheral immune cells, and an autoimmune profile in the brain. During the menopausal transition, the brain undergoes metabolic and immune reprogramming that places the brain at risk for neuropsychiatric disorders such as depression and cognitive impairment.85,87,88 While the majority of women experience some neuropsychiatric symptoms during the menopausal transition, approximately 20% of women will transition asymptomatically.86 A goal of the clinical study of bioenergetics and neural inflammation during transition states is to learn how to make neuropsychiatric symptoms during this phase of life the exception, not the rule. Among emerging developments from our group is the development of an estrogen-receptor-beta–targeting nutraceutical, PhytoSERM (NCT06186531, NCT05664477). Activating estrogen receptor beta promotes estrogen action in the brain while inhibiting activation of estrogenic signaling in the breast, which is key to addressing women’s concerns regarding estrogen therapy and risk of breast cancer. Relevant to a neuropsychiatric condition that disproportionately impacts women, estrogen receptor beta is associated with prevention and decrease of depressive symptoms. The combination of activating estrogen response in brain while inhibiting estrogen action in the breast has the dual impact of promoting brain health to potentially reduce the risk of menopause-related depression and later-life Alzheimer’s while simultaneously sustaining breast health. Additionally, we are developing the neurosteroid allopregnanolone as a regenerative therapeutic that may promote neurogenesis and neuroregeneration. More research is needed to determine if fluctuating levels of allopregnanolone during perimenopause contribute to insufficient plasticity of GABA-A receptors and increased risk for depression.
Research suggests that endocrinological aging may be a “tipping point” during midlife, potentially triggering the onset of the prodromal phase of late-onset Alzheimer’s disease (AD). The prodrome of AD often includes behavioral changes, in particular depression, anxiety, and circadian rhythm changes.89 The presence of the APOE4 genotype can accelerate the menopausal process. Interventions aimed at addressing both metabolic and immune changes associated with midlife aging may have the potential to modify the risk trajectory for both prodromal behavioral changes and the incidence of Alzheimer’s in later life. Additionally, for the advancement of precision medicine in Alzheimer’s disease (which must also consider behavioral and emotional symptoms, and not just cognitive changes), it is essential to consider chromosomal sex as a vital factor alongside APOE genotype, other genetic risk factors, and the stage of the disease.85 Neuropsychiatric disorders exhibit pathological characteristics commonly associated with both prodromal and syndromal AD, such as heightened oxidative stress, inflammation, disruption of excitatory and inhibitory signals, protein aggregation, and both beta-amyloid accumulation and tau hyperphosphorylation have been linked to conditions like depression, insomnia, and epilepsy.90,91 Endocrine changes associated with aging, evolving bioenergetics, and “inflammaging” all may serve as keys to unlocking the mysteries of the intersection of gender and depression.
Financial Disclosures
Dr Karp is an employee of University of Arizona; has received grant/research support from J&J Innovative Neuroscience, National Institutes of Health, and PCORI; has received honoraria from Journal of Clinical Psychiatry and American Journal of Geriatric Psychiatry; and has been on advisory boards for J&J Innovative Neuroscience and Otsuka. Dr Brinton is an employee of University of Arizona; spouse’s salary and defined benefit plan are from University of Southern California; is a consultant for the Advanced Research Projects Agency for Health; has received grant/research support from the National Institute on Aging (NIA) and National Institutes of Health (NIH); has received honoraria from Banner Hospital Foundation and NIA Board of Scientific Counselors (BSC); is on scientific advisory boards for Vial CRO, T3D, and WndrHLTH and is on the Women’s Health Matters (WHAM!) Advisory Board, NIA BSC, NIH ACD, Working Group on Diversity, and Brigham/Harvard Center ROSA External Advisory Board NIH-funded U54; and is President and Founder, Neutherapeutics. Dr Fourier receives royalties from Guilford Press. Dr Harding has received grant/research support from PCORI and has been on the J&J Neuroscience Advisory Board on Depression. Dr Jha has been a consultant for Boehringer Ingelheim; has received grant/research support from Neurocrine Bioscience, Navitor/Supernus, and Janssen Research & Development; has received honoraria to serve guest editor for Psychiatric Clinics of North America from Elsevier and for educational presentations from North American Center for Continuing Medical Education, Medscape/WebMD, Clinical Care Options, Physicians’ Education Resource, and H.C. Wainwright & Co; and has received fees to serve on Data Safety and Monitoring Boards for Worldwide Clinical Trials (Eliem and Inversargo), Vicore Pharma, and IQVIA (Click). Dr Mathew has been a consultant for Abbott, Autobahn Therapeutics, Boehringer-Ingelheim, Clexio Biosciences, Delix Therapeutics, Douglas Pharmaceuticals, Engrail Therapeutics, Freedom Biosciences, Liva Nova, Merck, Motif Neurotech, Neumora, Relmada Therapeutics, Sunovion, and Xenon Pharmaceuticals and has received grant/research support from Boehringer-Ingelheim, Neumora, Engrail Therapeutics, and Sage Therapeutics. Dr Meltzer-Brody has been a clinical advisor and professional corporation owner for Modern Health; has received grant/research support from Electromedical Products International and Sirtsei Pharmaceuticals and sponsored grant/research support from Sage Therapeutics; and has been on scientific advisory boards for Seaport Therapeutics and EmbarkNeuro. Dr Mohr has received honoraria from Boehringer-Ingelheim and Clinical Care Options; is a stock shareholder in Adaptive Health; and has received royalties from Oxford Press.Dr Riva-Posse has been a consultant for Abbott, LivaNova, Motif, and Johnson & Johnson. Dr Williams is an employee of Stanford Medicine, a subdivision of Stanford University; receives or has received within the last 12 months research support from the National Institutes of Health, Wellcome, the Pritzker Foundation, and New Venture Fund; has served on scientific advisory boards for Otsuka, Soneira Bio, Salma Health, and Magnus Medical as a paid advisor; holds equity/stock options in Magnus Medical, Salma Health, Soneira Bio, Tara Mind, Neurawell Therapeutics, and Humanity Neurotech; and is a named inventor on Stanford-owned intellectual property relating to accelerated TMS pulse pattern sequences and neuroimaging-based TMS targeting. He is a named inventor on a patent application (no. 18/467,324) related to the safety of ibogaine administration and on a patent application (no. 18/467,343) related to the use of ibogaine to treat disorders associated with brain aging. Drs Lenze and Wiechers report no relevant financial relationships.
References (95)

- Amos TB, Tandon N, Lefebvre P, et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression: a matched-cohort study using a US commercial claims database. J Clin Psychiatry. 2018;79(2).
- Zhdanava M, Pilon D, Ghelerter I, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82(2).
- Rush AJ, Fava M, Wisniewski SR, et al. Sequenced Treatment Alternatives to Relieve Depression (STAR*D): rationale and design. Control Clin Trials. 2004;25(1):119-142.
- Alegría M, Canino G, Shrout PE, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165(3):359-369.
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association Publishing; 2010.
- Gaynes BN, Warden D, Trivedi MH, et al. What did STAR*D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60(11):1439-1445.
- Lundberg J, Cars T, Lööv S, et al. Association of treatment-resistant depression with patient outcomes and health care resource utilization in a population-wide study. JAMA Psychiatry. 2023;80(2):167-175.
- Trivedi MH, Jha MK, Kahalnik F, et al. VitalSign(6): A Primary Care First (PCP-First) Model for Universal Screening and Measurement-Based Care for Depression. Pharmaceuticals (Basel). 2019;12(2).
- Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551-560.
- Jha MK, Grannemann BD, Trombello JM, et al. A structured approach to detecting and treating depression in primary care: VitalSign6 Project. Ann Fam Med. 2019;17(4):326-335.
- Szymanski BR, Bohnert KM, Zivin K, et al. Integrated care: treatment initiation following positive depression screens. J Gen Intern Med. 2013;28(3):346-352.
- Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:Cd006525.
- Solberg LI, Crain AL, Maciosek MV, et al. A stepped-wedge evaluation of an initiative to spread the collaborative care model for depression in primary care. Ann Fam Med. 2015;13(5):412-420.
- Stone MB, Yaseen ZS, Miller BJ, et al. Response to acute monotherapy for major depressive disorder in randomized, placebo controlled trials submitted to the US Food and Drug Administration: individual participant data analysis. Bmj. 2022;378:e067606.
- Simmonds-Buckley M, Kellett S, Waller G. Acceptability and efficacy of group behavioral activation for depression among adults: a meta-analysis. Behav Ther. 2019;50(5):864-885.
- Weitz ES, Hollon SD, Twisk J, et al. Baseline depression severity as moderator of depression outcomes between cognitive behavioral therapy vs pharmacotherapy: an individual patient data meta-analysis. JAMA Psychiatry. 2015;72(11):1102-1109.
- Nakagawa A, Mitsuda D, Sado M, et al. Effectiveness of supplementary cognitive-behavioral therapy for pharmacotherapy-resistant depression: a randomized controlled trial. J Clin Psychiatry. 2017;78(8):1126-1135.
- Watkins ER, Mullan EG, Wingrove J, et al. Rumination-focused cognitive-behavioural therapy for residual depression: phase II randomised controlled trial. Br J Psychiatry. 2011;199 4:317-322.
- Wiles N, Thomas L, Abel A, et al. Cognitive behavioural therapy as an adjunct to pharmacotherapy for primary care based patients with treatment resistant depression: results of the CoBalT randomised controlled trial. Lancet. 2013;381(9864):375-384.
- Dunn BD, Widnall E, Warbrick L, et al. Preliminary clinical and cost effectiveness of augmented depression therapy versus cognitive behavioural therapy for the treatment of anhedonic depression (ADepT): a single-centre, open-label, parallel-group, pilot, randomised, controlled trial. EClinicalMedicine. 2023;61:102084.
- Kuyken W, Warren FC, Taylor RS, et al. Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry. 2016;73(6):565-574.
- McAllister-Williams RH, Arango C, Blier P, et al. The identification, assessment and management of difficult-to-treat depression: an international consensus statement. Journal of Affective Disorders. 2020;267:264-282.
- Richardson RM, Ghuman AS, Karp JF. Results of the first randomized controlled trial of deep brain stimulation in treatment-resistant depression. Neurosurgery. 2015;77(2):N23-24.
- Mayberg HS, Lozano AM, Voon V, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45(5):651-660.
- Crowell AL, Riva-Posse P, Holtzheimer PE, et al. Long-term outcomes of subcallosal cingulate deep brain stimulation for treatment-resistant depression. Am J Psychiatry. 2019;176(11):949-956.
- Hitti FL, Cristancho MA, Yang AI, et al. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression: a decade of clini-cal follow-up. J Clin Psychiatry. 2021;82(6).
- Holtzheimer PE, Husain MM, Lisanby SH, et al. Subcallosal cingulate deep brain stimulation for treatment-resistant depression: a multisite, randomised, sham-controlled trial. Lancet Psychiatry. 2017;4(11):839-849.
- George MS, Rush AJ, Marangell LB, et al. A one-year comparison of vagus nerve stimulation with treatment as usual for treatment-resistant depression. Biol Psychiatry. 2005;58(5):364-373.
- Aaronson ST, Sears P, Ruvuna F, et al. A 5-year observational study of patients with treatment-resistant depression treated with vagus nerve stimulation or treatment as usual: comparison of response, remission, and suicidality. Am J Psychiatry. 2017;174(7):640-648.
- Conway CR, Aaronson ST, Sackeim HA, et al. Clinical characteristics and treatment exposure of patients with marked treatment-resistant unipolar major depressive disorder: A RECOVER trial report. Brain Stimul. 2024;17(2):448-459.
- Subramanian S, Oughli HA, Gebara MA, et al. Treatment-resistant late-life depression: a review of clinical features, neuropsychology, neurobiology, and treatment. Psychiatr Clin North Am. 2023;46(2):371-389.
- Mohamed S, Johnson GR, Chen P, et al. Effect of antidepressant switching vs augmentation on remission among patients with major depressive disorder unresponsive to antidepressant treatment: The VAST-D randomized clinical trial. JAMA. 2017;318(2):132-145.
- Srifuengfung M, Pennington BRT, Lenze EJ. Optimizing treatment for older adults with depression. Ther Adv Psychopharmacol. 2023;13:20451253231212327.
- Lenze EJ, Mulsant BH, Blumberger DM, et al. Efficacy, safety, and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised, double-blind, placebo-controlled trial. Lancet. 2015;386(10011):2404-2412.
- Lenze EJ, Mulsant BH, Roose SP, et al. Antidepressant augmentation versus switch in treatment-resistant geriatric depression. N Engl J Med. 2023;388(12):1067-1079.
- Moshe I, Terhorst Y, Philippi P, et al. Digital interventions for the treatment of depression: A meta-analytic review. Psychol Bull. 2021;147(8):749-786.
- Baumel A, Muench F, Edan S, et al. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res. 2019;21(9):e14567.
- Torous J, Lipschitz J, Ng M, et al. Dropout rates in clinical trials of smartphone apps for depressive symptoms: A systematic review and meta-analysis. J Affect Disord. 2020;263:413-419.
- Jaso-Yim B, Eyllon M, Sah P, et al. Evaluation of the impact of a digital care navigator on increasing patient registration with digital mental health interventions in routine care. Internet Interventions. 2024;38:100777.
- Titov N, Andrews G, Davies M, et al. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLoS One. 2010;5(6):e10939.
- Mordecai D, Histon T, Neuwirth E, et al. How Kaiser Permanente created a mental health and wellness digital ecosystem. NEJM Catalyst. 2021;2(1).
- Youn SJ, Jaso B, Eyllon M, et al. Leveraging implementation science to integrate digital mental health interventions as part of routine care in a practice research network. Admin Policy Mental Health Mental Health Serv Res. 2024;51(3):348-357.
- De Angel V, Lewis S, White K, et al. Digital health tools for the passive monitoring of depression: a systematic review of methods. NPJ Digit Med. 2022;5(1):3.
- Meyerhoff J, Liu T, Kording KP, et al. Evaluation of changes in depression, anxiety, and social anxiety using smartphone sensor features: longitudinal cohort study. J Med Internet Res. 2021;23(9):e22844.
- Adler DA, Stamatis CA, Meyerhoff J, et al. Measuring algorithmic bias to analyze the reliability of AI tools that predict depression risk using smartphone sensed-behavioral data. npj Mental Health Research. 2024;3(1):17.
- McQuaid JR, Buelt A, Capaldi V, et al. The management of major depressive disorder: synopsis of the 2022 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med. 2022;175(10):1440-1451.
- Anand A, Mathew SJ, Sanacora G, et al. Ketamine versus ECT for nonpsychotic treatment-resistant major depression. N Engl J Med. 2023;388(25):2315-2325.
- Wilkinson S, Sanacora G. Comparative Effectiveness of Racemic Ketamine versus S-Ketamine for Depression. 2023. Accessed August 20, 2024. https://www.pcori.org/research-results/2023/comparative-effectiveness-racemic-ketamine-versus-s-ketamine-depression.
- Pfeiffer PN, Geller J, Ganoczy D, et al. Clinical outcomes of intravenous ketamine treatment for depression in the VA health system. J Clin Psychiatry. 2024;85(1).
- Hermes E, Parillo L, Van Engelen L, et al. Availability and Utilization of Somatic Treatments in the Veterans Health Administration Fiscal Year 2022. VA Office of Mental Health and Suicide Prevention. Northeast Program Evaluation Center; 2023.
- Price RB, Kissel N, Baumeister A, et al. International pooled patient-level meta-analysis of ketamine infusion for depression: in search of clinical moderators. Mol Psychiatry. 2022;27(12):5096-5112.
- Medeiros GC, Matheson M, Demo I, et al. Brain-based correlates of antidepressant response to ketamine: a comprehensive systematic review of neuroimaging studies. Lancet Psychiatry. 2023;10(10):790-800.
- Ip C-T, de Bardeci M, Kronenberg G, et al. EEG-vigilance regulation is associated with and predicts ketamine response in major depressive disorder. Translational Psychiatry. 2024;14(1):64.
- Sanacora G, Smith MA, Pathak S, et al. Lanicemine: a low-trapping NMDA channel blocker produces sustained antidepressant efficacy with minimal psychotomimetic adverse effects. Mol Psychiatry. 2014;19(9):978-985.
- Lijffijt M, Murphy N, Iqbal S, et al. Identification of an optimal dose of intravenous ketamine for late-life treatment-resistant depression: a Bayesian adaptive randomization trial. Neuropsychopharmacology. 2022;47(5):1088-1095.
- Xiao J, Provenza NR, Asfouri J, et al. Decoding depression severity from intracranial neural activity. Biol Psychiatry. 2023;94(6):445-453.
- ACOG. Treatment and Management of Mental Health Conditions During Pregnancy and Postpartum: ACOG Clinical Practice Guideline No. 5. Obstet Gynecol. 2023;141(6):1262-1288.
- Ghaedrahmati M, Kazemi A, Kheirabadi G, et al. Postpartum depression risk factors: a narrative review. J Educ Health Promot. 2017;6:60.
- Bloch M, Daly RC, Rubinow DR. Endocrine factors in the etiology of postpartum depression. Compr Psychiatry. 2003;44(3):234-246.
- Fiorelli M, Aceti F, Marini I, et al. Magnetic resonance imaging studies of postpartum depression: an overview. Behav Neurol. 2015;2015:913843.
- Guintivano J, Arad M, Gould TD, et al. Antenatal prediction of postpartum depression with blood DNA methylation biomarkers. Mol Psychiatry. 2014;19(5):560-567.
- Licheri V, Talani G, Gorule AA, et al. Plasticity of GABAA receptors during pregnancy and postpartum period: from gene to function. Neural Plast. 2015;2015:170435.
- Osborne LM, Monk C. Perinatal depression--the fourth inflammatory morbidity of pregnancy? Theory and literature review. Psychoneuroendocrinology. 2013;38(10):1929-1952.
- Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2015;20(1):48-59.
- Schüle C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. 2014;113:79-87.
- Cox EQ, Sowa NA, Meltzer-Brody SE, et al. The perinatal depression treatment cascade: baby steps toward improving outcomes. J Clin Psychiatry. 2016;77(9):1189-1200.
- Molyneaux E, Howard LM, McGeown HR, et al. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. 2014;2014(9):Cd002018.
- Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058-1070.
- Maguire J, Mody I. Steroid hormone fluctuations and GABA(A)R plasticity. Psychoneuroendocrinology. 2009;34 Suppl 1(Suppl 1):S84-90.
- Brexanolone [package insert]. Sage Therapeutics; 2019.
- Bialer M, Johannessen SI, Levy RH, et al. Progress report on new antiepileptic drugs: a summary of the Eleventh Eilat Conference (EILAT XI). Epilepsy Res. 2013;103(1):2-30.
- Deligiannidis KM, Kroll-Desrosiers AR, Mo S, et al. Peripartum neuroactive steroid and ?-aminobutyric acid profiles in women at-risk for postpartum depression. Psychoneuroendocrinology. 2016;70:98-107.
- Epperson CN, Gueorguieva R, Czarkowski KA, et al. Preliminary evidence of reduced occipital GABA concentrations in puerperal women: a 1H-MRS study. Psychopharmacology (Berl). 2006;186(3):425-433.
- Luscher B, Shen Q, Sahir N. The GABAergic deficit hypothesis of major depressive disorder. Mol Psychiatry. 2011;16(4):383-406.
- Deligiannidis KM, Meltzer-Brody S, et al. Effect of zuranolone vs placebo in postpartum depression: a randomized clinical trial. JAMA Psychiatry. 2021;78(9):951-959.
- Deligiannidis KM, Meltzer-Brody S, Maximos B, et al. Zuranolone for the treatment of postpartum depression. Am J Psychiatry. 2023;180(9):668-675.
- Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517.
- Olgiati P, Bajo E, Bigelli M, et al. Challenging sequential approach to treatment resistant depression: cost-utility analysis based on the Sequenced Treatment Alternatives to Relieve Depression (STAR?D) trial. Eur Neuropsychopharmacol. 2013;23:1739-1746.
- Liston C, Chen AC, Zebley BD, et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol Psychiatry. 2014;76(7):517-526.
- Ballou S, Mitsuhashi S, Sankin LS, et al. Emergency department visits for depression in the United States from 2006 to 2014. Gen Hosp Psychiatry. 2019;59:14-19.
- Blumberger DM, Vila-Rodriguez F, Thorpe KE, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391(10131):1683-1692.
- Siddiqi SH, Schaper F, Horn A, et al. Brain stimulation and brain lesions converge on common causal circuits in neuropsychiatric disease. Nat Hum Behav. 2021;5(12):1707-1716.
- Cole EJ, Phillips AL, Bentzley BS, et al. Stanford Neuromodulation Therapy (SNT): a double-blind randomized controlled trial. Am J Psychiatry. 2022;179(2):132-141.
- Cole EJ, Stimpson KH, Bentzley BS, et al. Stanford Accelerated Intelligent Neuromodulation Therapy for treatment-resistant depression. Am J Psychiatry. 2020;177(8):716-726.
- Mishra A, Wang Y, Yin F, et al. A tale of two systems: lessons learned from female mid-life aging with implications for Alzheimer’s prevention & treatment. Ageing Res Rev. 2022;74:101542.
- Brinton RD, Yao J, Yin F, et al. Perimenopause as a neurological transition state. Nat Rev Endocrinol. 2015;11(7):393-405.
- Mishra A, Shang Y, Wang Y, et al. Dynamic neuroimmune profile during mid-life aging in the female brain and implications for Alzheimer risk. iScience. 2020;23(12):101829.
- Mosconi L, Berti V, Quinn C, et al. Perimenopause and emergence of an Alzheimer’s bioenergetic phenotype in brain and periphery. PLoS One. 2017;12(10):e0185926.
- Brommelhoff JA, Gatz M, Johansson B, et al. Depression as a risk factor or prodromal feature for dementia? Findings in a population-based sample of Swedish twins. Psychol Aging. 2009;24(2):373-384.
- Cordone S, Annarumma L, Rossini PM, et al. Sleep and ?-amyloid deposition in alzheimer disease: insights on mechanisms and possible innovative treatments. Front Pharmacol. 2019;10:695.
- Van der Mussele S, Mariën P, Saerens J, et al. Behavioral syndromes in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis. 2014;38(2):319-329.
- LivaNova provides update on RECOVER clinical study evaluating VNS therapy for treatment-resistant depression in unipolar patients. LivaNova. June 26, 2024. Accessed November 6, 2024. https://investor.livanova.com/news-releases/news-release-details/livanova-provides-update-recover-clinical-study-evaluating-vns
- Davenport S, Darby B, Gray TJ, et al. Access Across America: State-by-State Insights Into the Accessibility of Care for Mental Health and Substance Use Disorders. Milliman, Inc; 2023.
- Malowney M, Keltz S, Fischer D, et al. Availability of outpatient care from psychiatrists: a simulated-patient study in three US cities. Psychiatr Serv. 2015;66(1): 94–96.
- Buchalter ELF, Oughli HA, Lenze EJ, et al. Predicting remission in late-life major depression: a clinical algorithm based upon past treatment history. J Clin Psychiatry. 2019;80(6):18m12483.
This PDF is free for all visitors!