Abstract
When studying how (eg) gestational exposure to antidepressant drugs influences the risk of (eg) autism spectrum disorder (ASD) in offspring, conventional observational studies adjust analyses for available covariates and confounds. In such analyses, a significant association between antidepressant exposure and ASD outcome can never be asserted to be causal because of the possibility of residual confounding arising from confounding by indication (or severity thereof), confounding by genetic risk factors, and confounding by environmental risk factors. Confounding by indication and severity thereof can sometimes be addressed through propensity score matching, but the adjustment can never be perfect. Additionally, adjustment for genetic and environmental risk factors is hard or impossible to do because these are inadequately measured, unmeasured, and/or unknown variables. Sibling comparison studies have recently emerged as an option to address the genetic and environmental risk factors. In such studies, sibs discordant for exposure are compared for risk of outcome (cohort design) or sibs discordant for outcome are compared for odds of exposure (case-control design). The assumption is that sibs share similar genetic and environmental risk factors and so, when sibs are compared, these risk factors cancel out whether they are measured or not, known or unknown. If antidepressant exposure remains significantly associated with ASD in sibling comparisons, a possible conclusion is that antidepressants and not genetic or environmental factors drive the ASD risk. If antidepressant exposure loses significance in the sibling comparisons, it suggests that shared genetic and/or environmental factors, rather than antidepressant exposure, explain the ASD risk. The interpretation, however, is nuanced. Strengths, limitations, and interpretations of sibling comparison studies are explained. To illustrate the usefulness of sibling comparisons, results are presented from a recent study of ASD risk after gestational or early infancy exposure to antibiotics.
J Clin Psychiatry 2025;86(2):25f15843
Author affiliations are listed at the end of this article.
Many maternal conditions and gestational exposures have independently been associated with an increased risk of autism spectrum disorder (ASD) in offspring. In this context, a recent study of 236 maternal exposures used sibling comparison analyses to suggest that, rather than the exposures, family level factors explain most of the associations.1
During the past decade, such sibling comparisons have often been included in epidemiological research; however, their strengths and limitations are not well known to many readers. This article therefore explains what sibling studies are and how sibling comparisons can strengthen or weaken causal hypotheses in observational studies. Gestational exposure to antidepressant drugs and risk of ASD in offspring is presented as an example of a situation in which sibling comparisons are appropriate; the explanations can be generalized to other contexts, as well. Finally, to illustrate a recent use of sibling comparisons, a study on gestational exposure to antibiotics and risk of ASD in offspring is briefly described.
Background
Depression is common, and depression may require treatment with antidepressant drugs. When depression requiring antidepressant treatment occurs during pregnancy, we pause to consider the benefits vs risks of treating vs withholding treatment because the antidepressant may effectively treat the depression but, perhaps, have an adverse impact on the pregnancy and on the developing fetus. It is also conceivable that an adverse impact may manifest as a condition such as autism spectrum disorder (ASD), during childhood.
Evidence is necessary to assist informed decision making. Randomized controlled trials (RCTs) generate the best evidence. However, it is ethically problematic to conduct an RCT of antidepressants vs placebo during pregnancy to determine whether or not antidepressants increase the risk of ASD in childhood. It would also be impractical; ASD is an uncommon outcome, and an adequately powered RCT that examines whether an assumed risk of 2% with placebo increases to 4% with antidepressant exposure could require a sample size of more than 2,000 offspring followed for at least 5 years.
Conventional Approaches
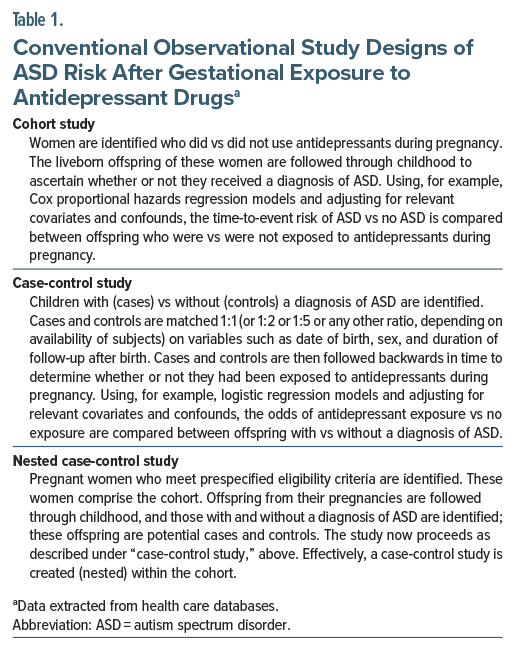
In lieu of RCTs, the neurodevelopmental risks associated with gestational exposure to antidepressants can be examined in retrospective observational studies that extract exposure, outcome, and other necessary data from health records such as insurance or health care databases, or national or other health registers. Examples of possible study designs are provided in Table 1. Readers unfamiliar with concepts referred to in the table can consult resources in this column2 and elsewhere3 for discussions on regression, covariates, confounds, and related topics; these concepts will repeatedly arise in the rest of this article.
Difficulties With Interpretation of Results
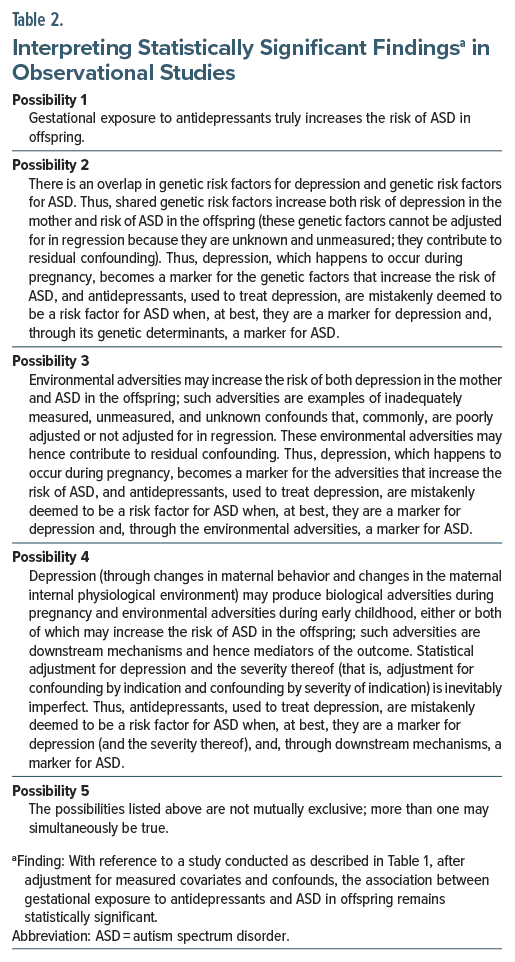
Observational studies, whatever the research design (Table 1), may identify a statistically significant association between antidepressant exposure and ASD, and the association may remain significant even after adjustment for measured covariates and confounds. On the surface, these results implicate antidepressant exposure as a risk factor for ASD. However, such an interpretation is problematic because other interpretations are possible, such as those related to residual confounding from genetic and environmental risk factors (Table 2). This is where sibling studies can help.
Sibling Studies
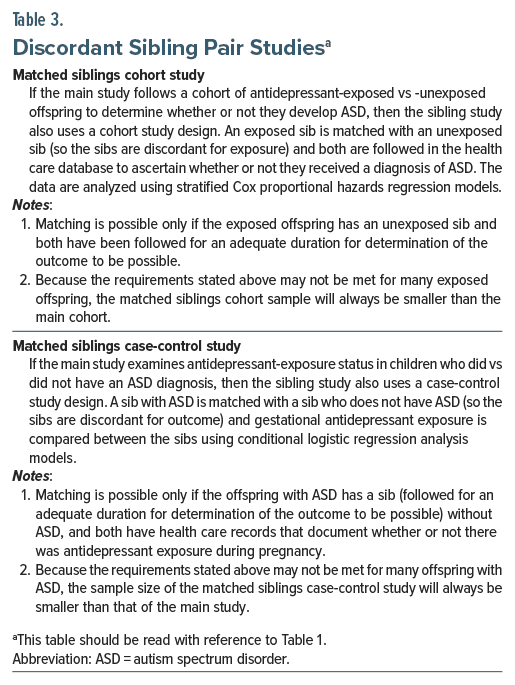
Sibling studies can help support or exclude some of the possibilities listed in Table 2. Such studies are generally conducted in addition to rather than instead of the conventional approaches presented in Table 1. Discordant sibling pair analysis is the most appropriate description of what is done, but sibling pair analysis, discordant sibling comparison, sibling comparison, and other terms are also used. Descriptions of what may be done are presented in Table 3.
Rationale for Sibling Studies
Sibs share the same parents, so genetic risk factors for ASD are likely to be similar in sibs, regardless of gestational exposure to antidepressants. Therefore, when comparing antidepressant-exposed and -unexposed sibs, the genetic risk factors cancel out; there is no need to know what these risk factors are, and there is no need to measure and adjust for them as is necessary but impossible to do in conventional studies. Thus, by design, sibling comparisons reduce confounding by genetic risk factors (Table 2, Possibility 2).
Sibs also share the same environment, including benefits and risks related to parenting, diet, lifestyle, health care, exposure to infections, exposure to environmental toxins, and other behavioral and socioeconomic determinants of health. Therefore, environmental risk factors for ASD are also likely to be similar in in sibs, regardless of gestational exposure to antidepressants. Hence, when comparing antidepressant exposed and -unexposed sibs, the shared environmental risk factors cancel out; there is no need to know what these risk factors are, and there is no need to measure and adjust for them as is necessary but hard or impossible to do in conventional studies (whereas parental education, income, substance use, comorbidities, and other variables can be measured and adjusted for, these are not necessarily the actual risk factors; and, postnatally, other risk factors may arise). Thus, by design, sibling comparisons reduce confounding by environmental risk factors (Table 2, Possibility 3).
Sibling studies do not perfectly control for genetic and environmental confounds; this is discussed in a later section.
Interpreting the Results of Discordant Sibling Pair Analysis
If the main study finds that antidepressant exposure is associated with ASD and if the sibling comparison obtains the same result, it suggests that antidepressant exposure is associated with ASD even after controlling for shared genetic and environmental risk factors. However, a causal relationship between antidepressant exposure and ASD cannot be definitively stated because residual confounding is possible even in sibling comparisons (see the next section), much as it is possible in the main analysis.
If the main study finds that antidepressant exposure is associated with ASD and if the sibling comparison finds that antidepressant exposure is not associated with ASD, it suggests that, after controlling for genetic and environmental risk factors, antidepressant exposure is no longer associated with ASD. That is, antidepressant exposure is unlikely to be a risk factor for ASD. However, the absence of a causal relationship between antidepressant exposure and ASD cannot be definitively stated because, for example, the sibling analysis may have been underpowered.
Drawing Wrong Conclusions About Shared Risks
It is important to recognize that the sibling analysis merely reduces confounding from unmeasured and unknown genetic and environmental risk factors when studying the effect of antidepressant exposure on ASD risk. If statistical significance associated with antidepressant exposure disappears in the sibling comparison, it does not indicate that the statistical significance should be assigned to genes and environment, instead. Absence of 1 statistically significant relationship does not prove the presence of another statistically significant relationship. Sibling groups that are “not significantly different” are not automatically “significantly similar.”
Whereas the disappearance of statistical significance in sibling comparisons can certainly support a hypothesis that genetic or environmental exposure may drive ASD, drawing conclusions about the significance of genetic or environmental risk factors for ASD would require different studies that are specifically designed to examine genetic or environmental risks.
Limitations of Sibling Studies
Sibs are not identical twins; therefore, whereas they may share some genetic risk factors for ASD, they may not share all the genetic risk factors. So, sibling studies reduce but cannot eliminate genetic confounds. Likewise, sibs share a similar environment; they do not share identical environments. As examples, their environments may have differed during intrauterine life, their environments may have differed postnatally because of differing birth order, and they may have been exposed to different adversities during early childhood both at home and outside the home. So, sibling studies can reduce but cannot eliminate environmental confounds, either.
Sibling studies also do not control for discordant and time-variant factors such as confounding by indication for antidepressant use and confounding by severity of indication, or risk factors that occur after birth. In fact, by reducing confounding from shared risk factors, sibling comparisons may increase the impact of confounding from nonshared risk factors.4,5 Thus, potential confounds will continue to require to be measured and adjusted for through statistical models, and the likelihood of residual confounding cannot be discounted.
The sample size in sibling comparisons is always smaller than the sample size in the main study; so, sibling comparisons may be underpowered. In this context, it should be remembered that health care records are imperfect; therefore, values for exposure and outcome are blurred rather than precise, making it harder to establish statistical significance. This is a big issue because when statistical significance is not established in sibling comparisons, statistical significance in main analyses is commonly and possibly wrongly rejected, as explained in an earlier section. Other limitations of sibling comparison studies have also been described.4–6
Antibiotic Exposure and Risk of Neurodevelopmental Disorders
Choi et al7 conducted a large, nationwide, population based, retrospective cohort study that examined whether children who had been exposed to antibiotics during pregnancy and infancy were at increased risk of neurodevelopmental disorders (NDDs). They supplemented their main analyses with sibling comparisons to better assist the interpretation of findings.
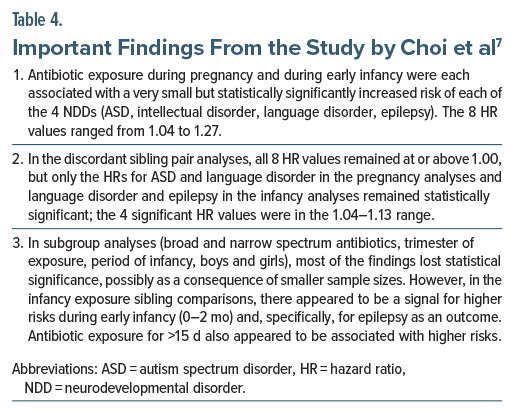
The data were drawn from a South Korean national health insurance service database. The sample comprised children born during 2009–2020 and followed until 2021 (median age, 7 years). The sample was 1: 1 propensity score-matched for children exposed vs unexposed to systemic antibiotics during pregnancy (n = 1,961,744) or infancy (age, 0–6 months; n = 1,609,774). Antibiotic exposure was assumed based on issue of at least 1 prescription. The NDD outcomes, extracted from records, were ASD, intellectual disorder, language disorder, and epilepsy. Discordant sibling pair analyses (n = 843,412 for pregnancy and n = 1,082,417 for infancy) were also conducted to control for shared genetic and time-invariant environmental risk factors; discordance was based on antibiotic exposure vs no exposure.
Important findings from the study are presented in Table 4. In summary, antibiotic exposure during pregnancy and early infancy were each associated with a small but statistically significant increase in the risk of each NDD (ASD, intellectual disorder, language disorder, and epilepsy); in sibling comparisons, some but not all risks lost statistical significance. Thus, whereas it appeared that a part of the risk may have been driven by shared genetic and environmental factors, the sibling comparisons did not rule out a role for antibiotics.
Observations on the Antibiotic-ASD Study7
The study had some unacknowledged limitations. For example, it is not clear how offspring with dual exposure (exposure during pregnancy as well as infancy) and controls with exposure in 1 but not the other study period were classified. However, the study is commendable for its very large sample size, including for the sibling pair analyses. Because the risks were not completely eliminated in the sibling pair analyses, it does seem that antibiotics, or the conditions for which they were prescribed (implying residual confounding by indication or by severity of indication), may have driven the risks. This interpretation notwithstanding, the risks were very small. Therefore, with specific regard to NDDs as outcomes, it may be justifiable to suggest an antibiotic during pregnancy or infancy, but only when the need to treat an infection is clear. Decision-making processes should be shared. Care should be taken to avoid prescribing antibiotics as knee jerk reactions to respiratory infections (which are often viral in etiology), especially in early infancy (age 0–2 months) and for periods >15 days.
Take-Home Messages
Sibling comparisons can assist causal inferences in observational studies but cannot support definitive conclusions. With specific regard to NDDs as outcomes, it may be justifiable to consider antibiotic treatment for a pregnant woman or infant, but only when the need to treat a potentially responsive infection is clear.
Parting Notes
In this article, discordant sibling pair analysis was explained in the context of gestational exposure to antidepressant drugs and ASD as the outcome in offspring; however, the explanations are valid for other exposures and outcomes in other contexts, as well.
In this article, both exposure and outcome were dichotomous variables; that is, antidepressant exposure could be “yes or no,” and ASD outcome could be “yes or no.” In some situations, exposure and/or outcome can be continuous variables. Examples are when dose of a drug is the exposure and when IQ is the outcome. In such situations, contrasts between sibling pairs can be enhanced using extremely discordant sibling pair analysis, as may be done in genetic studies.8 That is, sibs are matched for (eg) highest vs lowest quintile scores rather than for presence or absence of a criterion.
Sibling studies are not the only way to address unmeasured and unknown confounds in observational studies. With specific references to studies related to exposures during pregnancy, studies of prepregnancy exposure and studies of paternal exposure can also provide guidance towards interpretation of the findings of the main analyses.
Article Information
Published Online: March 17, 2025. https://doi.org/10.4088/JCP.25f15843
© 2025 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Discordant sibling pair comparisons in observational studies: a research design simply explained. J Clin Psychiatry 2025;86(2):25f15843.
Author Affiliations: Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India; Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India. Please contact Chittaranjan Andrade, MD, at Psychiatrist.com/contact/andrade.
References (8)

- Khachadourian V, Arildskov ES, Grove J, et al. Familial confounding in the associations between maternal health and autism. Nat Med. 2025. doi:10.1038/ s41591-024-03479-5. CrossRef
- Andrade C. Regression: understanding what covariates and confounds do in adjusted analyses. J Clin Psychiatry. 2024;85(4):24f15573.
- Andrade C. Confounding by indication, confounding variables, covariates, and independent variables: knowing what these terms mean and when to use which term. Indian J Psychol Med. 2024;46(1):78–80.
- Frisell T, Öberg S, Kuja-Halkola R, et al. Sibling comparison designs: bias from non-shared confounders and measurement error. Epidemiology. 2012;23(5):713–720.
- Frisell T. Invited commentary: sibling-comparison designs, are they worth the effort? Am J Epidemiol. 2021;190(5):738–741.
- Sjölander A, Frisell T, Kuja-Halkola R, et al. Carryover effects in sibling comparison designs. Epidemiology. 2016;27(6):852–858.
- Choi A, Lee H, Jeong HE, et al. Association between exposure to antibiotics during pregnancy or early infancy and risk of autism spectrum disorder, intellectual disorder, language disorder, and epilepsy in children: population based cohort study. BMJ. 2024;385:e076885.
- Risch N, Zhang H. Extreme discordant sib pairs for mapping quantitative trait loci in humans. Science. 1995;268(5217):1584–1589. PubMed CrossRef
This PDF is free for all visitors!