Abstract
Objective: To provide proof-of-concept (PoC), dose-range finding, and safety data for BI 1358894, a TRPC4/5 ion channel inhibitor, in patients with borderline personality disorder (BPD).
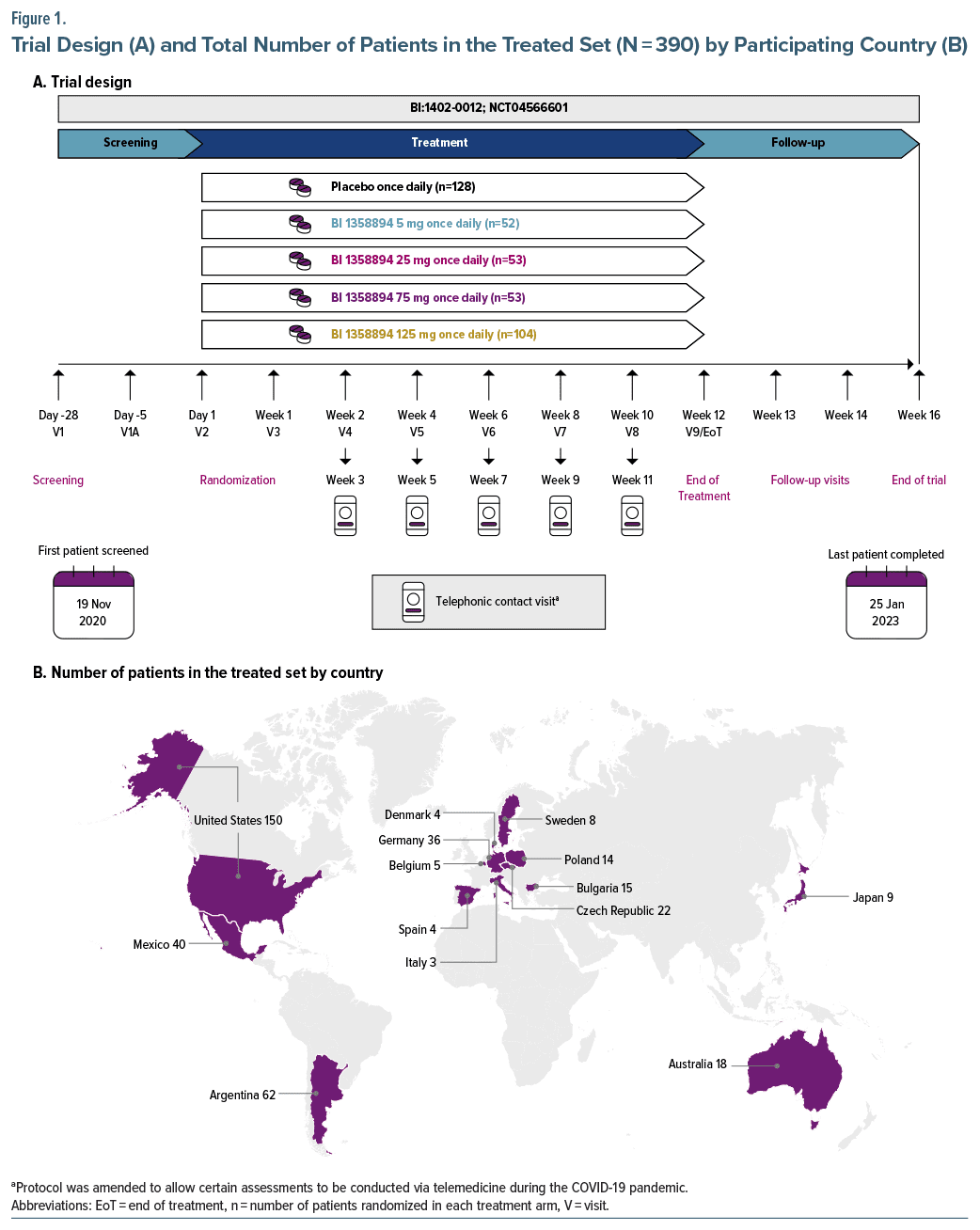
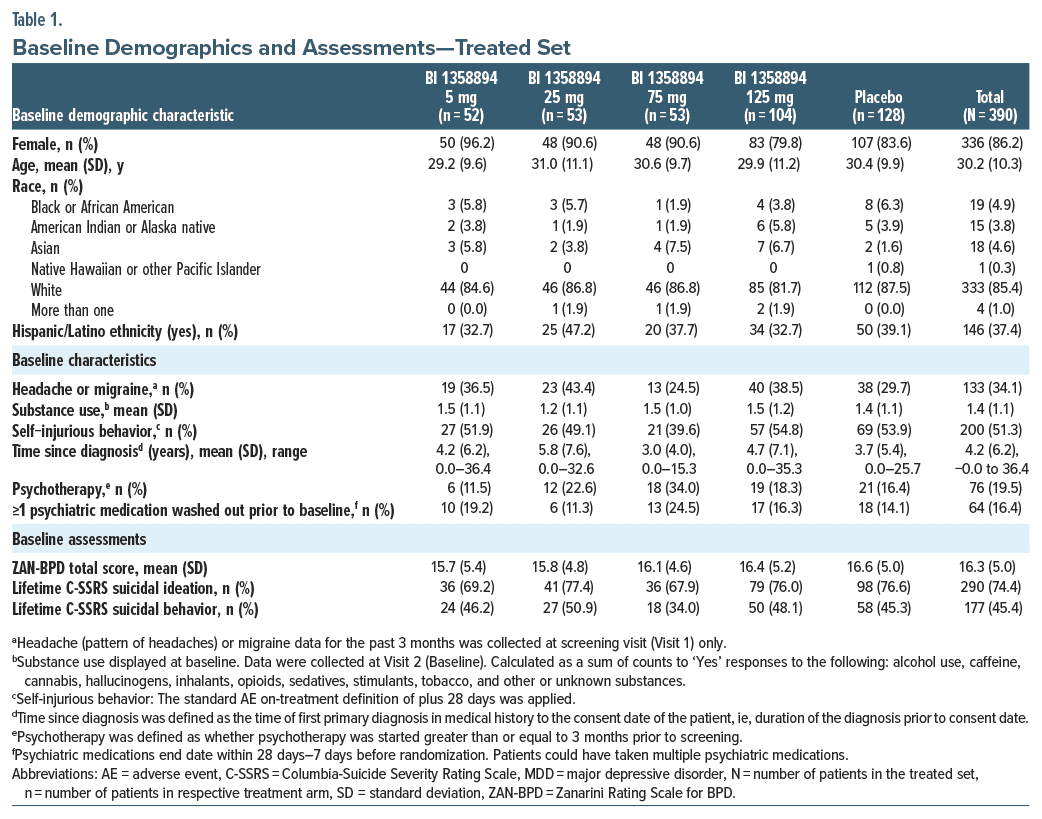
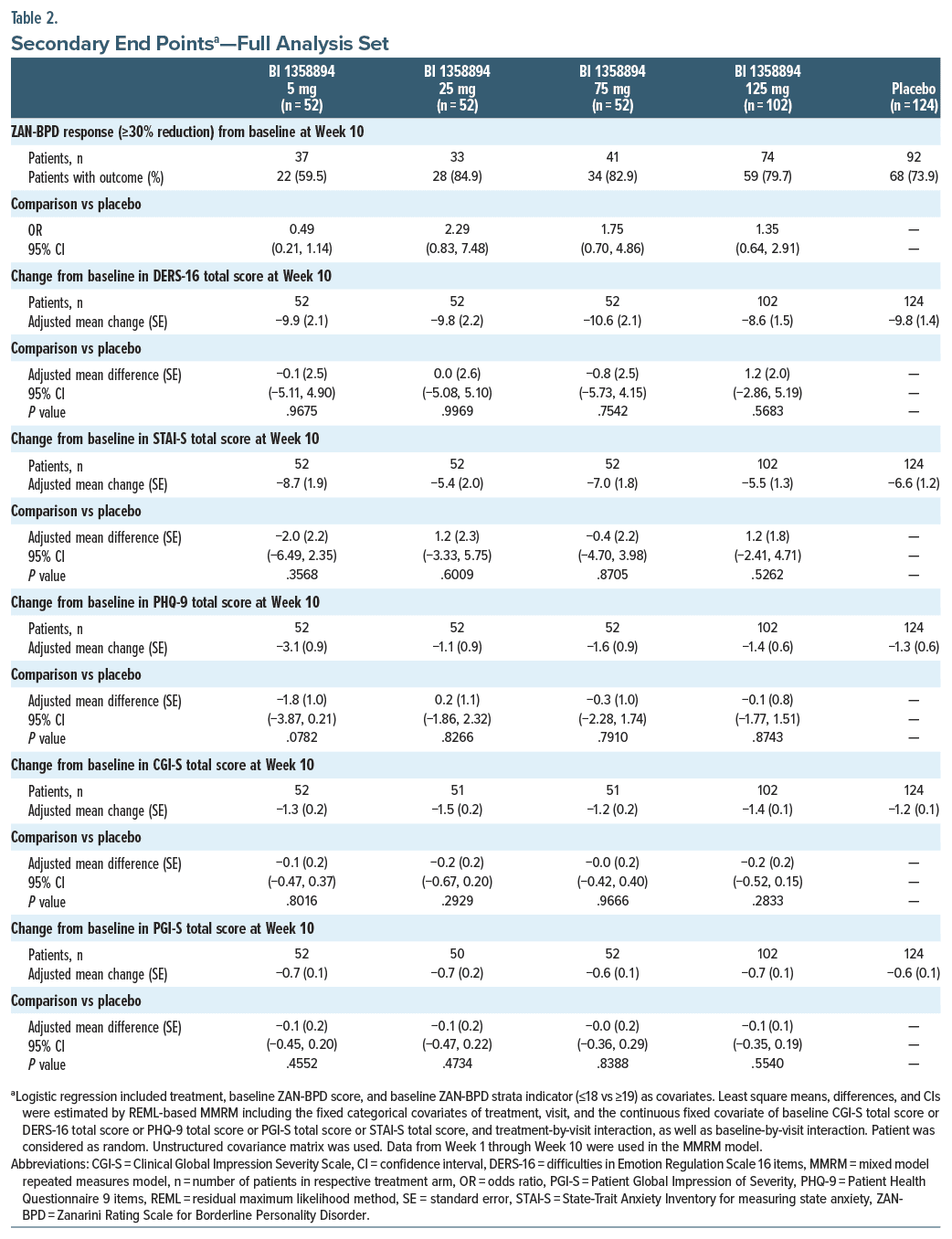
Methods: This was a phase 2, multinational, randomized, double-blind, placebo controlled trial. Patients were randomized to oral placebo or BI 1358894 (5 mg, 25 mg, 75 mg, or 125 mg) once daily in a 2.5:1:1:1:2 ratio for 12 weeks. The primary end point was change from baseline in the Zanarini Rating Scale for BPD (ZAN BPD) total score at Week 10. Secondary end points included ≥30% ZAN-BPD reduction response from baseline at Week 10, change from baseline at Week 10 in the Difficulties in Emotion Regulation Scale-16 item total, State-Trait Anxiety Inventory–State Anxiety total, Patient Health Questionnaire-9 total, Clinical Global Impressions–Severity, and Patient Global Impression–Severity scores.
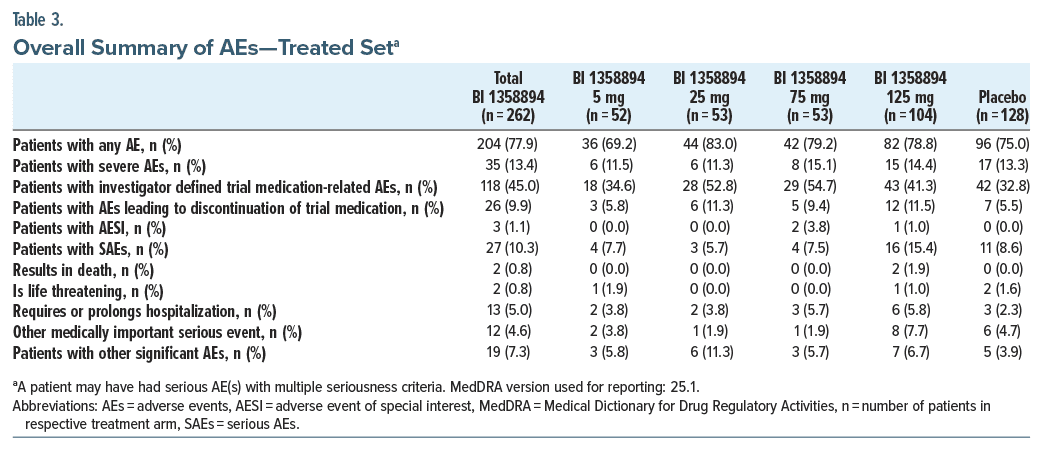
Results: Of 655 enrolled patients, 390 were randomized and 323 (82.8%) completed the trial. For primary and secondary end points, no differences were observed between treatment and placebo; therefore, PoC was not established. The proportion of patients with adverse events (AEs, BI 1358894 overall vs placebo: 77.9% vs 75.0%) and serious AEs (SAEs; 10.3% vs 8.6%) was comparable between treatments. The proportion of patients with an SAE of suicidal ideation was 4.2% (BI 1358894 overall) and 6.3% (placebo).
Conclusions: Although the primary end point was not met, BI 1358894 was well tolerated with no increase in self harm or suicidality. More targeted populations, alternative outcome assessments, and additional measures to minimize placebo effects should be considered for future trials.
Trial Registration: ClinicalTrials.gov identifier: NCT04566601.
J Clin Psychiatry 2025;86(1):24m15523
Author affiliations are listed at the end of this article.
Borderline personality disorder (BPD) is a serious mental illness with a prevalence of 1.8–5.9%.1,2 BPD is characterized by pervasive instability in affect regulation, self-image, cognition, interpersonal relationships, and impulse control.3 Additionally, diagnosed patients often have psychiatric comorbidities, such as mood, anxiety, substance use, and trauma-related or eating disorders.4,5 BPD psychopathology severity and associated impairment in social and occupational functioning can lead to reduced quality of life (QoL).6–8 It is estimated that 2–10% of patients with BPD die by suicide,9,10 and those who do not achieve recovery are at higher risk of premature death.11
Despite the clear disease burden, there are currently no Food and Drug Administration-approved pharmacotherapies for BPD.12,13 However, pharmacotherapy is often used off-label to target symptoms.13,14 Although medications show specific core symptoms improvement in some cases, there is no evidence of overall severity improvement.15,16 The current clinical guidelines for BPD recommend structured psychotherapy, such as dialectical behavior therapy and mentalization-based therapy17–19; however, there is limited availability of trained professionals to care for treatment-seeking individuals.20 While some evidence exists that psychotherapy is superior to treatment-as usual conditions, there is limited evidence to differentiate between psychotherapy types and to determine optimal duration.17 As such, there is a clear unmet need for novel BPD treatments.21
Emotional dysregulation is a core feature of BPD which has been linked to amygdala hyperreactivity in patients with BPD.22–24 Transient receptor potential canonical ion channels 4 and 5 (TRPC4/5) are expressed in the brains of both animals and humans, predominantly in areas of the corticolimbic system that regulate emotion and mood, such as the amygdala.25,26 Therefore, the inhibition of TRPC4/5 ion channels may provide a novel mechanism of attenuating amygdala hyperreactivity to improve BPD.27 BI 1358894, a novel TRPC4/5 inhibitor, has demonstrated attenuation of amygdala hyperreactivity in people with major depressive disorder27 and reduction in cholecystokinin-induced panic symptoms in healthy controls.28 Phase 1 studies have demonstrated that BI 1358894 is generally safe and well-tolerated at doses up to 200 mg in healthy male volunteers, with a favorable pharmacokinetic profile.29,30
This trial aimed to provide proof-of-concept (PoC) for TRPC4/5 ion channel inhibition and dose-ranging data for BI 1358894 vs placebo in patients with BPD to support dose selection for pivotal studies and establish BI 1358894 safety in this population.
METHODS
Trial Design, Randomization, and Blinding
In this phase 2, multinational, randomized, double blind, placebo-controlled, parallel-group trial (ClinicalTrials.gov identifier: NCT04566601), patients with BPD across 67 centers in 17 countries (Figure 1) were randomized via interactive response technology to receive placebo or BI 1358894 (5 mg, 25 mg, 75 mg, or 125 mg) orally, once daily in a 2.5:1:1:1:2 ratio for 12 weeks. Randomization was stratified by the baseline Zanarini Rating Scale for BPD (ZAN-BPD) total score (≤18 vs ≥19). The trial encompassed a screening period of 2 visits, a minimum of 5 phone call visits and 8 in person visits during treatment, and 3 visits during the 4-week follow-up. The chosen BI 1358894 doses were intended to explore potential exposure-response curves over a broad dose range.
Using a multiple comparison procedure with modelling (MCPMod) approach, a total sample size of approximately 355 patients was needed to determine PoC with 81% average power across models, with one sided 10% α level, assuming 285 evaluable patients across treatment arms and 20% dropout rate.
The trial was conducted in accordance with the Declaration of Helsinki, the International Council for Harmonization of Good Clinical Practice guidelines, applicable regulatory requirements, and Boehringer Ingelheim standard operating procedures. The trial protocol and informed consent form were reviewed by the Independent Ethics Committees and/or Institutional Review Boards of the participating centers. Study protocol is available through the clinicaltrials.gov portal.
Patients
The trial included patients aged 18–65 years, with a confirmed BPD diagnosis (per Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [DSM-5]-Personality Disorders) at screening who provided informed consent at Visit 1. Patients were required to have a ZAN-BPD total score ≥9 with an Affective Instability score of ≥2 at screening and randomization. Patients with a current diagnosis of paranoid, schizoid, schizotypal personality disorders or a lifetime diagnosis of schizophrenia, schizoaffective or schizophreniform disorder, bipolar disorder, or delusional disorder were excluded. Patients were also excluded if they had another major psychiatric disorder that was the primary focus of treatment in the previous 6 months, any suicidal behavior in the previous year, suicidal ideation of type 4/5 (Columbia-Suicide Severity Rating Scale [C-SSRS]) in the previous 3 months, or hospitalization due to nonsuicidal self-injury or BPD worsening within the previous 3 months. Patients could not be on any ongoing psychotropic comedication for at least 7 days prior to randomization or, per investigator discretion, a washout of at least 3 half-lives must have been completed at least 7 days prior to randomization. Patients could continue any ongoing psychotherapy, provided there was no initiation or change in type or frequency in the 3 months prior to screening. The full eligibility criteria are included in the Supplementary Methods.
End Points and Assessments
Primary end point. The primary end point of change from baseline in ZAN-BPD total score was evaluated at Week 10 of 12 to avoid any potential issues related to perceived abandonment at the end-of-treatment period. The ZAN-BPD is a clinician-administered scale for the assessment of change in DSM-5 borderline psychopathology over time.31 The subgroup analyses of the primary end point were carried out for baseline disorder severity (ie, ZAN-BPD total score strata indicator [≤18 vs ≥19]), video-confirmed adherent subgroups, US vs non-US patients, region, ethnicity and race, and Asian vs non-Asian patients.
Secondary end points. The secondary end points were response, defined as ≥30% ZAN-BPD reduction from baseline at Week 10, change from baseline at Week 10 in the Difficulties in Emotion Regulation Scale-16 item version total score, the State-Trait Anxiety Inventory–State Anxiety total score, the Patient Health Questionnaire-9 total score, the Clinical Global Impressions–Severity score, and the Patient Global Impression–Severity scores.
Selected exploratory end points. The selected exploratory end points include the change from baseline in ZAN-BPD total score over time, response defined as ≥30% ZAN-BPD reduction from baseline over time, and patient-reported outcomes related to QoL at Week 10 (change from baseline in EuroQol 5-Dimensions 5-Levels [EQ-5D-5L], Sheehan Disability Scale [SDS], and Patient Global Impression–Impact [PGI-I] scales).
Safety. Safety was assessed through percentage of patients with adverse events (AEs), serious AEs (SAEs), AEs of special interest (AESI; protocol-specified AESI was hepatic injury, ie, an elevation of aspartate transaminase [AST] and/or alanine transaminase [ALT] ≥3-fold upper limit of normal [ULN] combined with total bilirubin elevation ≥2-fold ULN measured in the same blood sample, or aminotransferase [ALT and/or AST] elevations ≥10-fold ULN), and trial discontinuations due to AEs. Occurrences of any clinically significant abnormalities in vital signs, electrocardiogram, laboratory tests, and suicidality (frequency of suicidal ideation, suicidal behavior, and self injurious behavior without suicidal intent as assessed by C-SSRS) were also reported.
Statistical Analysis
The primary end point was analyzed via hypothetical estimand, focusing on the treatment effect assuming that trial medication was taken as directed and excluding intercurrent events. The primary end point analysis included all on-treatment data collected from first to last trial medication dose plus 7 days. Any data collected after a patient discontinued treatment was censored and not included in the primary analysis. The primary analysis utilized the MCPMod for dose finding, which enabled simultaneous evaluation of various potential dose response patterns, while minimizing false positives (probability of type I error) using a one-sided α level of 10%. For the MCPMod analysis, a mixed model repeated measures model (MMRM) analysis was used to generate covariate-adjusted estimates of mean change from baseline to Week 10 in ZAN-BPD total score and associated covariance matrices. The secondary end point of ZAN-BPD response was analyzed through a logistic regression model; other secondary end points were analyzed using the MMRM model to obtain adjusted change from baseline at Week 10 for each treatment arm vs placebo. Efficacy was evaluated in the full analysis set (ie, all randomized patients who had a baseline and ≥1 evaluable postbaseline measurement for the primary end point), and safety was evaluated descriptively in the treated set (ie, all randomized patients who received ≥1 dose of trial medication).
RESULTS
Patient Disposition and Demographics
Of 655 enrolled patients, 390 patients were randomized and 323 (82.8%) completed the trial, while 287 (73.6%) completed trial medication administration (Supplementary Figure 1). The mean (standard deviation [SD]) patient age was 30.2 (10.3) years, and the majority (86.2%) were female. The mean (SD) [range] time since BPD diagnosis was 4.2 (6.2) [0.0–36.4] years and included some patients diagnosed at study entry or after consent date. The use of previous psychiatric medications, washed out before baseline, was low (n = 64; 16.4%); the frequency of previous psychiatric medication use was higher in the BI 1358894 5 mg, 75 mg, and 125 mg arms vs placebo, but less frequent in the BI 1358894 25 mg arm vs placebo. Overall, 76 (19.5%) patients were attending psychotherapy sessions at baseline (Table 1). Of the randomized patients, 383 had pill count data available (as per case report forms), and median overall compliance was 99% over the 12-week treatment period.
Efficacy
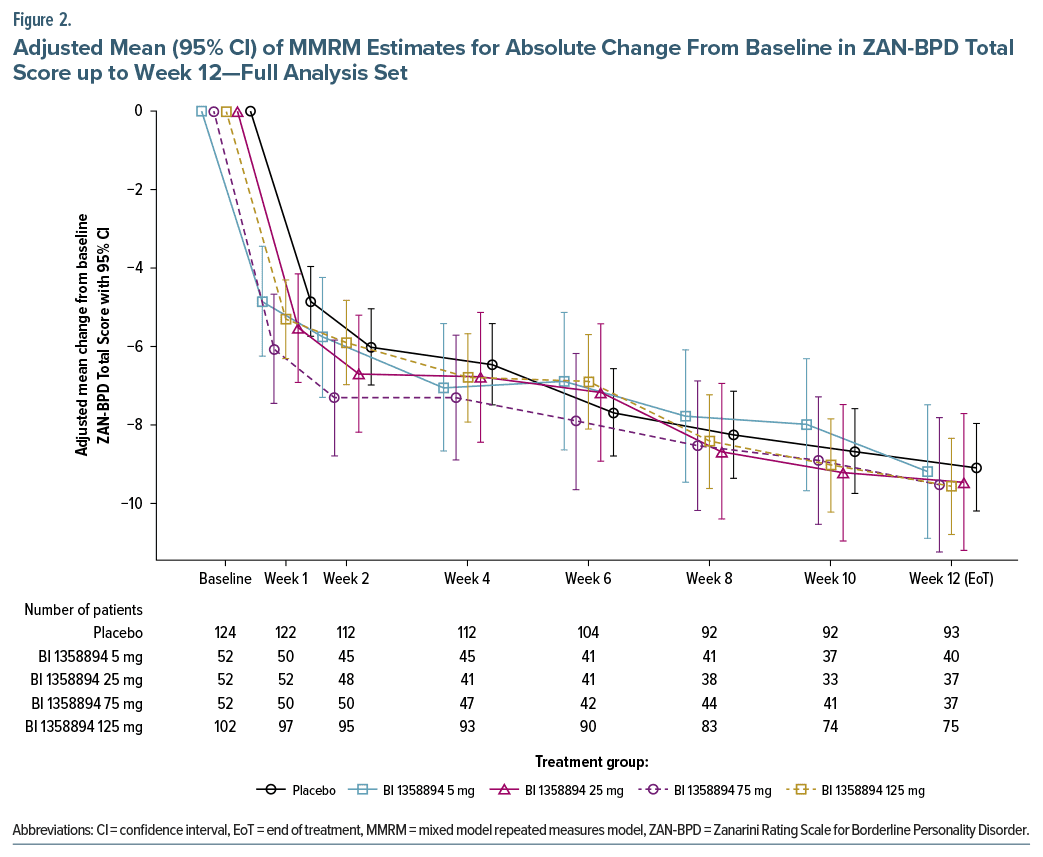
Primary end point. BPD symptoms improved in all treatment arms, including placebo, as indicated by decreases in ZAN-BPD total score from baseline to Week 10 (Figure 2) with no significant group difference. Thus, the trial did not meet its primary end point criterion. The adjusted mean (SE) change from baseline to Week 10 in ZAN-BPD total score was between −8.0 and −9.2 across BI 1358894 dose groups and −8.7 in placebo group (Supplementary Table 1). A substantial placebo response was observed, with a rapid reduction of 5.3 points in the mean ZAN-BPD total score at Week 1 and a further slower reduction of 9.8 points continuous over time from baseline at Week 12 (Supplementary Table 2). For PoC testing, the adjusted P value of the multiple contrast test was not significant for any of the candidate models in MCPMod analysis (Supplementary Table 3). Further, no subgroup analyses revealed any differences between treatment arms and placebo, except for the subgroup by baseline disorder severity wherein higher severity (ZAN-BPD total score ≥19) subgroup had a higher placebo response vs lower severity subgroup (ZAN-BPD total score ≤18; Supplementary Figure 2). However, patients receiving concomitant psychotherapy showed lower placebo responses vs those who did not (Supplementary Figure 3). There were no discernible differences between the subgroup of patients who completed prior washout of psychotropic medications and those who did not (Supplementary Figure 4).
Secondary end points. Treatment with BI 1358894 (all doses) had a similar effect to placebo with no significant differences observed between treatment groups for any of the secondary end points (Table 2).
Exploratory end points. Across treatment arms, the mean ZAN-BPD total score improved from moderate at baseline (mean [SD] total score of 16.26 [5.07]) to mild at Week 10 (7.24 [5.45]; Supplementary Table 2). Overall, the frequency of responders increased from baseline up to Week 12 (Supplementary Figure 5). Regarding overall well-being, there were no improvements observed in the mean change from baseline in EQ-5D-5L index and EQ-5D-5L VAS scores over the 10 weeks; however, the SDS and PGI-I scale scores decreased (improved) from baseline to Week 10 (Supplementary Table 4).
Safety. AEs were reported by 77.9% of patients receiving BI 1358894 across all doses and 75.0% receiving placebo. Proportion of patients with severe AEs (BI 1358894 vs placebo: 13.4% vs 13.3%), SAEs (10.3% vs 8.6%), AEs leading to discontinuation (9.9% vs 5.5%), and other significant AEs (7.3% vs 3.9%) was generally comparable between treatment arms (Table 3). The most common AEs leading to discontinuation were suicidal ideation (BI 1358894 vs placebo: 1.1% vs 1.6%), headache (1.1% vs 0.8%), and somnolence (1.1% vs 0.0%). AEs related to trial drug occurred more frequently with BI 1358894 vs placebo; however, they were not dose dependent. Headache was the most frequently reported AE for BI 1358894 compared with placebo (34.0% vs 25.0%). There were no clinically relevant changes from baseline for vital signs or any safety laboratory parameters, except for the AESI observed in 3 patients (hepatitis A and hepatic enzyme increase in 2 patients with BI 1358894 75 mg and cholestatic jaundice in 1 patient with BI 1358894 125 mg). The most common SAE was suicidal ideation (BI 1358894: 4.2%; placebo: 6.3%).
Based on C-SSRS, the frequency of suicidal ideation was numerically lower for BI 1358894 across all doses compared with placebo (38.5% vs 44.5%). The frequency of suicidal behavior was low throughout the trial (BI 1358894: 1.9%; placebo: 0.8%), and both treated and placebo-controlled patients had similar frequencies of self-injurious behavior without suicidal intent (BI 1358894: 17.2%; placebo: 16.4%). Two patients treated with BI 1358894 125 mg died due to 3 fatal SAEs (1 patient with fatal opioid overdose, and another with severe esophageal varices hemorrhage and a myocardial infarction). However, these deaths were assessed as unrelated to the trial medication by the investigator. There were no completed suicides during this trial.
DISCUSSION
This phase 2 trial evaluated the efficacy and safety of 12-week BI 1358894 treatment vs placebo in patients with BPD. The trial did not meet the primary end point as there were no significant differences between treatment groups and placebo. This was observed in most scales used and in all subgroup analyses. The PoC was not established, and so the dose-response modeling was not carried out.
BI 1358894 was well tolerated, with a safety profile consistent with previous clinical studies.28,29 A relatively high rate of AEs (BI 1358894: 204 [77.9%]; placebo: 96 [75.0%]) was observed in all treatment arms including placebo, suggesting a nocebo effect. However, there was no worsening of symptoms hypothesized as an “abandonment effect” at the last timepoint of efficacy assessment (Week 12) unlike a prior BPD trial.32
Given the high placebo response and the absence of a suitable positive control, it is difficult to interpret whether lack of separation between treatment and placebo reflects the absence of treatment efficacy or methodological issues leading to trial failure. Placebo response was substantial, with a 5.0 point reduction in mean ZAN-BPD total score from baseline to Week 1. The average ZAN-BPD score at Week 10 fell in the mild range for all groups; therefore, a ceiling effect for improvement may obscure full interpretation of any treatment effects or lack thereof. While significant placebo responses have been observed in some studies (decrease from baseline in ZAN-BPD total score at Week 10 of −6.8 and −6.25 in olanzapine studies33,34 and −6.25 in brexpiprazole studies),32 the present trial had a higher placebo response than previously published studies.
Several factors may explain a high placebo response in this trial. The lack of approved BPD therapies may have led patients and clinicians to have optimistic expectations for this new treatment.35 The large number of treatment arms may have increased the perceived likelihood of receiving treatment vs placebo, further increasing expectations.36 The trial also had high intensity visit schedules, which patients with BPD may have found supportive. Moreover, the trial period’s coincidence with the COVID-19 pandemic may have intensified this effect, considering social contact and structure can be more therapeutically impactful after isolation. Since many patients were not receiving any other medication at the time of randomization, the clinician-patient bonds formed through regular, high-quality interaction during the trial may have enhanced the nonspecific therapeutic effects of trial participation.37
Despite psychotherapy being the most effective current treatment for BPD,38 only 19% of trial participants were attending psychotherapy sessions at baseline. Interestingly, these patients had a lower placebo response vs those who did not receive psychotherapy. One hypothesis that these data generate is that patients with background psychotherapy were already receiving professional attention via their therapist and, therefore, were less likely to experience therapeutic gains related to the nonspecific effects of trial participation. Psychiatric medication use in this patient sample was also low (16.4% conducted a medication washout before the trial), which is a departure from real-world assessments of BPD treatment, in which off-label psychiatric medication prescribing is frequent.39 This departure from real-world patients who have higher medication use generates several hypotheses. Given considerable burdens in access to mental health care for BPD,20 it is possible that lack of medication reflects treatment seeking patients unable to access timely psychiatric care, ie, if these patients had access to care, they may have been prescribed off-label medication. Furthermore, for patients with high severity of BPD at trial entry, those actively seeking treatment may be more likely to have a significant therapeutic benefit from the connection to care within the trial, as supported by the higher placebo response observed in patients with an entry ZAN-BPD score >19. However, when patients who conducted a washout were compared with those who did not, no significant differences were found. Finally, gaining psychoeducation about BPD following diagnosis has been shown to lead to symptomatic improvements,40 which could have affected overall symptomatic improvement for patients diagnosed upon enrollment or previously unable to access care.
This trial is one of the largest conducted in patients with BPD with retention numbers (82.8%) closer to those seen in psychotherapy trials (78% overall)41 than in medication trials (65%).33 Moreover, there were no documented suicides during this trial. However, this trial has significant limitations. Foremost, patient and investigator expectations were not measured, so no data address the hypothesis that observed placebo responses may be due to high expectations in newly diagnosed patients or those not receiving any medication outside of the trial. Second, it may be difficult to show further improvement in the drug treated groups given the substantial improvement in ZAN-BPD scores of the placebo-treated patients and the low levels of BPD symptoms at Week 10, ie, a ceiling effect.
Since individuals with BPD may present very heterogenous symptoms, future trials in BPD may consider enriching the patient population for the symptom domain of interest, aligned with the expected mechanism of action of the drug. Additionally, implementing strategies to mitigate the placebo effect may be beneficial. The mitigation of the placebo effect is an important and complex issue in clinical trials for all mental health conditions,42 but perhaps particularly so for BPD, a condition in which the quality of therapeutic relationships is an important factor in predicting treatment outcomes.43 Traditional clinical trial design approaches aimed at mitigating the placebo effect in psychiatry, such as placebo lead-ins, have not been successful in improving treatment effect sizes, as they tend to reduce both the placebo response and the therapeutic response to the investigational compound.44 Therefore, a multipronged approach to placebo mitigation should be considered for future BPD trials to reduce the risk of ceiling effects observed in the current trial. Potential strategies may include design features (eg, lead-ins or habituation to study procedures and study staff prior to baseline), ensuring the use of clinical outcome assessments with adequate room for change, and providing tailored placebo response training for study sites, informed by the lived experiences of individuals with BPD.
In conclusion, this phase 2 trial aimed to evaluate the efficacy and safety of a 12-week treatment with BI 1358894 compared with placebo in patients with BPD. Although efficacy was not demonstrated, BI 1358894 was well tolerated with no increase in self-harm or suicidality.
Article Information
Published Online: January 13, 2025. https://doi.org/10.4088/JCP.24m15523
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 17, 2024; accepted October 10, 2024.
To Cite: Dwyer JB, Schmahl C, Makinodan M, et al. Efficacy and safety of BI 1358894 in patients with borderline personality disorder: results of a phase 2 randomized, placebo controlled, parallel group dose-ranging trial. J Clin Psychiatry. 2025;86(1):24m15523.
Author Affiliations: Boehringer Ingelheim Pharmaceuticals, Ridgefield, Connecticut (Dwyer); Department of Psychosomatic Medicine and Psychotherapy, Central Institute of Mental Health, Medical Faculty Mannheim, Heidelberg University, Germany (Schmahl); Department of Psychiatry, Fujita Health University School of Medicine, Aichi, Japan (Makinodan); Department of Psychiatry, Nara Medical University School of Medicine, Nara, Japan (Makinodan); Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Fineberg); Global Regulatory Affairs, Boehringer Ingelheim International GmbH, Ingelheim am Rhein, Germany (Sommer); Biostatistics & Data Sciences, Boehringer Ingelheim Pharmaceuticals, Ridgefield, Connecticut (Wruck, Adeniji); Clinical Development & Operations, Boehringer Ingelheim Pharmaceuticals, Ridgefield, Connecticut (Jelaska); Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York (Goodman); Clinical Research, James J. Peters VA Medical Center, Bronx, New York (Goodman).
Corresponding Author: Jennifer B. Dwyer, MD, PhD, Boehringer Ingelheim Pharmaceuticals, 900 Ridgebury Rd, Ridgefield, CT 06877 ([email protected]).
Relevant Financial Relationships: Drs Dwyer and Jelaska and Ms Wruck are employees of Boehringer Ingelheim Pharmaceuticals, Inc. Dr Schmahl has served as a consultant to and received research support from Boehringer Ingelheim International GmbH and Atai Life Sciences. Drs Makinodan and Goodman have served as consultants to Boehringer Ingelheim International GmbH. Dr Fineberg has served as a consultant to Boehringer Ingelheim International GmbH, Oryzon, and Atai Life Sciences. Dr Sommer is an employee of Boehringer Ingelheim International GmbH. Dr Adeniji is a consultant for Boehringer Ingelheim Pharmaceuticals, Inc.
Funding/Support: This trial was funded by Boehringer Ingelheim International GmbH, Ingelheim am Rhein, Germany (BI trial number: 1402-0012; ClinicalTrials.gov identifier: NCT04566601).
Role of the Sponsor: Boehringer Ingelheim International GmbH contributed to the concept, study design, data collection, and analysis. The sponsor was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Acknowledgments: Editorial support in the form of initial preparation of the outline based on input from all authors and collation and incorporation of author feedback to develop subsequent drafts, assembling tables and figures, copyediting, and referencing was provided by Arshjyoti Singh, MPharm, of Avalere Health Global Limited, and was funded by Boehringer Ingelheim International GmbH.
ORCID: Jennifer B. Dwyer: https://orcid.org/0000-0001-8666-1050; Christian Schmahl: https://orcid.org/0000-0003-0141-0821; Manabu Makinodan: https://orcid.org/0000-0003-4339-9413; Sarah K. Fineberg: https://orcid.org/0000-0001-6024-6721; Jan Wruck: https://orcid.org/0009-0009-7810-8058; Abidemi Adeniji: https://orcid.org/0000-0002-8882-5079; Marianne Goodman: https://orcid.org/0000-0002-5465-9527
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Despite the burden of untreated BPD on patients and health care systems, no pharmacotherapies are approved, and off-label medications are often used to target symptoms.
- This study showed a strong placebo response, which emerged at week 1 and persisted throughout the trial. The robust placebo effect and the absence of a positive control make it difficult to draw firm conclusions about the efficacy of BI 1358894.
- Future trials in BPD should consider targeting specific populations within BPD, assessing a range of outcomes, and including measures to minimize placebo effects.
References (44)

- Bilgin A, Chanen AM, Furtado V, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. 2019;216(2):69–78.
- Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008 Apr;69(4):533–545. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Shah R, Zanarini MC. Comorbidity of borderline personality disorder: current status and future directions. Psychiatr Clin North Am. 2018;41(4):583–593.
- Slotema CW, Blom JD, Niemantsverdriet MBA, et al. Comorbid diagnosis of psychotic disorders in borderline personality disorder: prevalence and influence on outcome. Front Psychiatry. 2018;9:84.
- IsHak WW, Elbau I, Ismail A, et al. Quality of life in borderline personality disorder. Harv Rev Psychiatry. 2013;21(3):138–150. PubMed CrossRef
- Wilks CR, Korslund KE, Harned MS, et al. Dialectical behavior therapy and domains of functioning over two years. Behav Res Ther. 2016;77:162–169. PubMed CrossRef
- Stefanatou P, Xenaki LA, Konstantakopoulos G, et al. Psychopathological determinants of quality of life in people with borderline personality disorder. J Clin Med. 2022;12(1):30.
- Paris J. Suicidality in borderline personality disorder. Med Kaunas Lith. 2019;55(6):223.
- Álvarez-Tomás I, Ruiz J, Guilera G, et al. Long-term clinical and functional course of borderline personality disorder: a meta-analysis of prospective studies. Eur Psychiatry. 2019;56:75–83. PubMed CrossRef
- Temes CM, Frankenburg FR, Fitzmaurice GM, et al. Deaths by suicide and other causes among patients with borderline personality disorder and personality disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80(1):18m12436. PubMed
- Chapman J Jr, Fleisher C. Borderline personality disorder [Updated 2023 Jun 2]. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Yadav D. Prescribing in borderline personality disorder – the clinical guidelines. Prog Neurology Psychiatry. 2020;24(2):25–30.
- Pascual JC, Arias L, Soler J. Pharmacological management of borderline personality disorder and common comorbidities. CNS drugs. 2023;37(6):489–497.
- Stoffers-Winterling JM, Storebø OJ, Pereira Ribeiro J, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2022;11(11):Cd012956. PubMed
- Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4–12. PubMed CrossRef
- American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. Am J Psychiatry. 2001;158(Suppl 10):1–52.
- Igo M, Yusa Y, Ikeda A, et al. Assessment and psychotherapy of borderline personality disorders in Japan: results from a cross-sectional survey of psychologists. Int J Ment Health. 2024:1–22. doi:10.1080/00207411.2023.2300567 CrossRef
- National Institute for Health and Care Excellence, Clinical Guideline for Borderline Personality Disorder: Recognition and Management. 2009. Accessed March, 2024. https://www.nice.org.uk/guidance/cg78
- Iliakis EA, Sonley AKI, Ilagan GS, et al. Treatment of borderline personality disorder: is supply adequate to meet public health needs?. Psychiatr Serv. 2019;70(9):772–781. PubMed CrossRef
- Woodbridge J, Townsend M, Reis S, et al. Non-response to psychotherapy for borderline personality disorder: a systematic review. Aust N Z J Psychiatry. 2022;56(7):771–787.
- Mitolo M, D’Adda F, Evangelisti S, et al. Emotion dysregulation, impulsivity and anger rumination in borderline personality disorder: the role of amygdala and insula. Eur archives Psychiatry Clin Neurosci. 2023;274(1):109–116. PubMed
- Donegan NH, Sanislow CA, Blumberg HP, et al. Amygdala hyperreactivity in borderline personality disorder: implications for emotional dysregulation. Biol Psychiatry. 2003;54(11):1284–1293. PubMed CrossRef
- Levine SM, Merz K, Keeser D, et al. Altered amygdalar emotion space in borderline personality disorder normalizes following dialectical behaviour therapy. J Psychiatry Neurosci. 2023;48(6):E431–E438.
- Fowler MA, Sidiropoulou K, Ozkan ED, et al. Corticolimbic expression of TRPC4 and TRPC5 channels in the rodent brain. PLoS ONE. 2007;2(6):e573. PubMed CrossRef
- Riccio A, Medhurst AD, Mattei C, et al. mRNA distribution analysis of human TRPC family in CNS and peripheral tissues. Brain Res Mol Brain Res. 2002;109(1):95–104. PubMed CrossRef
- Grimm S, Keicher C, Paret C, et al. The effects of transient receptor potential cation channel inhibition by BI 1358894 on cortico-limbic brain reactivity to negative emotional stimuli in major depressive disorder. Eur Neuropsychopharmacol. 2022;65:44–51.
- Goettel M, Fuertig R, Mack SR, et al. Effect of BI 1358894 on cholecystokinin tetrapeptide (CCK-4)-Induced anxiety, panic symptoms, and stress biomarkers: a phase I randomized trial in healthy males. CNS Drugs. 2023;37(12):1099–1109.
- Fuertig R, Goettel M, Herich L, et al. Effects of single and multiple ascending doses of BI 1358894 in healthy male volunteers on safety, tolerability and pharmacokinetics: two phase I partially randomised studies. CNS drugs. 2023;37(12):1081–1097.
- Goettel M, Fuertig R, Wiebe S, et al. P.447 Multiple rising doses of oral BI 1358894 in healthy male volunteers: a phase I study investigating safety, tolerability and pharmacokinetics. Eur Neuropsychopharmacol. 2020;40:S254–S255.
- Zanarini MC, Vujanovic AA, Parachini EA, et al. Zanarini rating scale for borderline personality disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Pers Disord. 2003;17(3):233–242. PubMed CrossRef
- Grant JE, Valle S, Chesivoir E, et al. A double-blind placebo-controlled study of brexpiprazole for the treatment of borderline personality disorder. Br J Psychiatry. 2021;220(2):1–6.
- Zanarini MC, Schulz SC, Detke HC, et al. A dose comparison of olanzapine for the treatment of borderline personality disorder: a 12-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2011;72(10):1353–1362. PubMed CrossRef
- Schulz SC, Zanarini MC, Bateman A, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193(6):485–492. PubMed CrossRef
- Rutherford BR, Roose SP. A model of placebo response in antidepressant clinical trials. Am J Psychiatry. 2013;170(7):723–733. PubMed CrossRef
- Papakostas GI, Fava M. Does the probability of receiving placebo influence clinical trial outcome? A meta-regression of double-blind, randomized clinical trials in MDD. Eur Neuropsychopharmacol. 2009;19(1):34–40. PubMed CrossRef
- Benedetti F. Mechanisms of placebo and placebo-related effects across diseases and treatments. Annu Rev Pharmacol Toxicol. 2008;48:33–60.
- Leichsenring F, Heim N, Leweke F, et al. Borderline personality disorder: a review. JAMA. 2023;329(8):670–679. PubMed
- Riffer F, Farkas M, Streibl L, et al. Psychopharmacological treatment of patients with borderline personality disorder: comparing data from routine clinical care with recommended guidelines. Int J Psychiatry Clin Pract. 2019;23(3):178–188. PubMed CrossRef
- Zanarini MC, Conkey LC, Temes CM, et al. Randomized controlled trial of web based psychoeducation for women with borderline personality disorder. J Clin Psychiatry. 2018;79(3):16m11153. PubMed
- Iliakis EA, Ilagan GS, Choi-Kain LW. Dropout rates from psychotherapy trials for borderline personality disorder: a meta-analysis. Personal Disord. 2021;12(3):193–206.
- Bschor T, Nagel L, Unger J, et al. Differential outcomes of placebo treatment across 9 psychiatric disorders: a systematic review and meta-analysis. JAMA Psychiatry. 2024;81(8):757–768. PubMed
- Bedics JD, Atkins DC, Harned MS, et al. The therapeutic alliance as a predictor of outcome in dialectical behavior therapy versus nonbehavioral psychotherapy by experts for borderline personality disorder. Psychother (Chic). 2015;52(1):67–77. PubMed CrossRef
- Scott AJ, Sharpe L, Quinn V, et al. Association of single-blind placebo run-in periods with the placebo response in randomized clinical trials of antidepressants: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79(1):42–49.
This PDF is free for all visitors!