Abstract
Objective: There are few established treatments for negative symptoms in schizophrenia, which persist in many patients after positive symptoms are reduced. Oxidative stress, inflammation, and epigenetic modifications involving histone deacetylase (HDAC) have been implicated in the pathophysiology of schizophrenia. Sulforaphane has antioxidant properties and is an HDAC inhibitor. We conducted a 24-week, double-blind, placebo-controlled study, in Hunan, China, to assess the effect of high-dose sulforaphane (Nutramax extra strength sulforaphane tablets glucoraphanin content 30 mg/ tablet) on reducing negative symptoms in antipsychotic-treated patients with schizophrenia.
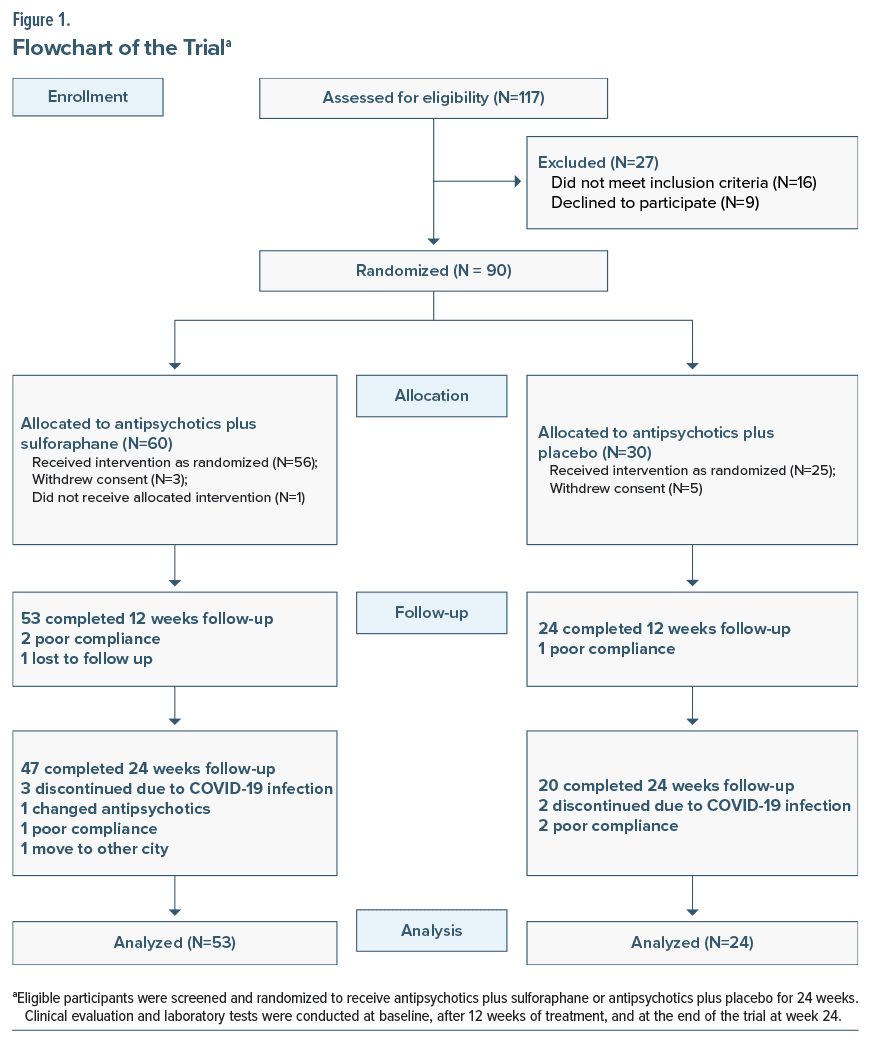
Methods: Participants were recruited from August 2020 to August 2022 and met DSM-5 criteria for schizophrenia. Participants were randomly assigned (2:1) to receive antipsychotics plus sulforaphane (1,700 mg Avmacol Extra Strength sulforaphane daily) or antipsychotics plus placebo for 24 weeks. Fifty-three patients treated with sulforaphane and 24 patients treated with placebo who had at least 1 postintervention clinical scale evaluation were analyzed. The primary outcome measure was change in the Positive and Negative Syndrome Scale (PANSS) negative symptoms.
Results: Sulforaphane-treated patients showed a significantly greater decrease in PANSS negative symptom total score (P = .01) and PANSS negative factor score (P = .02) than placebo-treated patients, with the most prominent difference occurring at 24 weeks (P ≤ .001) with a large effect size at this time point (d = 0.8). Sulforaphane’s effect on decreasing negative symptoms was not mediated by changes in scores of depression or cognitive factors on the PANSS.
Conclusions: The results of this study suggest that add-on high-dose sulforaphane may reduce negative symptoms in patients with schizophrenia. The clinical significance of this reduction in negative symptoms needs further evaluation.
Trial Registration: ClinicalTrials.gov identifier: NCT04521868.
J Clin Psychiatry 2025;86(1):24m15272
Author affiliations are listed at the end of this article.
Schizophrenia is a severe mental illness, characterized by recurrent positive symptoms, persistent negative symptoms, and marked cognitive deficits,1 with a prevalence of approximately 1%.2 Antipsychotics, the mainstay of treatment, act predominantly on the dopaminergic system and show amelioration of positive symptoms. However, antipsychotics have lower efficacy in treating negative symptoms, which emerge during the prodromal phase and persist the entire lifespan and result in functional disability. The etiology of negative symptoms is complex and unknown; they can be primary to the disease itself, or be secondary to positive symptoms or depressive symptoms, or worsened by antipsychotic-induced side effects.3–5 Although amisulpride, cariprazine, and blonanserin show advantages over other antipsychotics in alleviating negative symptoms,4,6,7 to date no medication has been approved for the treatment of negative symptoms by the FDA.
Sulforaphane (SFN), as a plant-active substance, has antioxidant and anti-inflammatory, neuroprotective, and metabolic regulation effects. Both animal and clinical studies revealed that SFN has the potential to improve symptoms, behaviors, and cognitive impairment in psychiatric diseases.8,9 Though the pathogenesis of schizophrenia remains unclear, inflammation and oxidative stress appear to play an important role in the pathology of schizophrenia.10 Cell-mediated immune activation was found in schizophrenia patients. Maes et al11 reported that the plasma concentrations of the inflammatory cytokine interleukin-6 were significantly higher in schizophrenia patients than in healthy participants. In a positron emission tomography brain imaging study, participants with subclinical symptoms at ultra-high risk of psychosis and patients with schizophrenia were found to show elevated microglial activity.12 Meta-analyses showed that some oxidative stress markers (thiobarbituric reactive substances and nitric oxide) were increased, while antioxidant markers (superoxide dismutase and glutathione) were decreased in schizophrenia patients.13,14 These results were consistent with 1 large meta-analysis which concluded that patients with schizophrenia have a lower antioxidant capacity and increased proinflammatory state.15
Animal studies have provided evidence of the therapeutic effects of SFN on schizophrenia. In a phencyclidine (PCP)-induced schizophrenia mice model, the dendritic spine density and the proportion of PV positive cells were decreased in the medial prefrontal cortex and hippocampal CA1 of the schizophrenia mouse models, while the proportion of 8-hydroxy-2’- deoxyguanosine (a marker of DNA oxidative damage)–positive cells were increased in the above 2 brain regions.16 This study further observed that the above changes induced by PCP can be attenuated by pretreatment with SFN. Early intervention using SFN may reduce the onset of subsequent transition to schizophrenia.16,17 However, our previous study evaluating SFN’s effects in first-episode schizophrenia patients or early episode with acute exacerbation of symptoms did not show statistically significant differences in the Positive and Negative Syndrome Scale (PANSS) positive or negative symptoms between SFN and placebo treatment.18 Another study in patients with schizophrenia also failed to show a difference in PANSS scores.19 However, these previous studies did not set inclusion criteria based on the specific symptoms and used relatively lower doses of SFN in Nutramax tablets compared with a higher dose tablet available more recently. Further, randomized clinical trials may need to be conducted to explore the effects of SFN in specific clinical subsets of schizophrenia and find optimal therapeutic doses.
The primary objective of this study was to investigate the efficacy of SFN in the treatment of negative symptoms in schizophrenia patients. The study also assessed the safety of SFN treatments through clinical and laboratory evaluations.
METHODS
Study Design and Participants
The study was a randomized, double-blind, placebo controlled study. Participants were recruited from August 2020 to August 2022 at the Second Xiangya Hospital of Central South University. The inclusion criteria were as follows: (1) met the criteria for schizophrenia of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5); (2) aged 18–50 years old; (3) disease duration ≤10 years; (4) total score greater than or equal to 20 on the sum of the 7 items constituting the PANSS negative symptoms; at least 1 item of PANSS negative symptoms with a score of >3; (5) taking 2 or fewer antipsychotics; (6) with antipsychotic medication remaining unchanged during the study period.
The exclusion criteria were as follows: (1) have a history of substance dependence or abuse or whose symptoms are caused by other diagnosable mental disorders; (2) have a history of traumatic brain injury, seizures, or other known neurological diseases of the central nervous system; (3) take antidepressants, stimulants, or mood stabilizers or received modified electroconvulsive therapy20 or repetitive transcranial magnetic stimulation during the past 3 months; (4) have current suicidal or homicidal thoughts or any safety concern by research staff that cannot be managed during the trial; (5) take dementia-related drugs, minocycline, and other drugs that may affect cognitive function; (6) laboratory tests indicated significant abnormalities in blood routine, liver and kidney function, or other metabolic results; (7) pregnant or lactating women.
The study was approved by the local ethics committee, written informed consent was obtained, and the study was registered at ClinicalTrials.gov (identifier: NCT04521868).
SFN and Placebo Administration
Participants were randomly assigned (2:1) to receive antipsychotics plus SFN or antipsychotics plus placebo using a computer-based random number generator. Both the clinical evaluators and patients as well as treatment team members were blinded to the treatment. Patients in the SFN group received 1,700 mg Avmacol Extra Strength SFN (obtained from Nutramax though a Chinese supplier) once daily as an add-on treatment for 24 weeks; measured glucoraphanin content was more than 30 mg/tablet in each tablet, and the SFN group received 2 tablets once daily. Each Avmacol Extra Strength tablet contains ≥30 mg glucoraphanin and has an SFN potential of at least 12 mg (approximately 68 µmol) of SFN per tablet. Therefore, participants in this study received ≥60 mg glucoraphanin with an SFN potential of 24 mg (approximately 136 µmol) of SFN daily if they followed study procedures (see Supplementary Material for statement on quality control). Patients in the placebo group received placebo tablets (matched in color and size) once daily as an add on treatment for 24 weeks. Adherence to medication was calculated as the percentage of the actual drug dose to the total administered dose. An independent research staff member counted the pill counts distributed and returned and contacted the participants for follow-up visits. Although it is possible there could be differences in taste between the SFN and placebo pills, the independent researcher, who had no role in the evaluations, dispensed the pills, and any complaints regarding taste could be directed solely to her. Once contacted by phone, participants attended one-on-one follow-up without opportunities for interaction among themselves. The antipsychotic medications remained at a fixed dose as baseline levels throughout the course of treatment. We set 3 time points for assessment: baseline, week 12, and week 24. Clinical evaluations and blood tests were included at each time point. Psychopathology was assessed using the PANSS21 and the Clinical Global Impression Scale (CGI).22,23 The Treatment-Emergent Symptom Scale (TESS)24 was used to monitor treatment safety to evaluate adverse events at each clinic visit.
Outcome Measures
The primary outcome measures were the PANSS negative symptoms, both the PANSS negative sum score and the 5-factor PANSS negative symptom score (sum of N1, N2, N3, N4, and N6) at the relevant time points. The 5-factor PANSS scores were derived from factor analysis described in previous studies.25,26 Secondary outcome measures were the PANSS total score, PANSS 5-factor scores except negative factor (positive, excitement, depression, and cognitive). Additional outcome measures were the CGI scale, and the safety and tolerability evaluation included reporting adverse events, electrocardiogram, laboratory tests, and Treatment Emergent Symptom Scale (TESS) scale.
Statistical Analysis
Statistical analysis utilized SPSS 25, SAS 9.4, and R programs for a mediation analysis. The main analysis of PANSS scale outcome data utilized mixed model analysis using SAS 9.4 process mixed, to deal with missing data from dropouts or other causes. The main analysis of PANSS scores was a mixed model analysis of difference scores from baseline with baseline scores ratings, duration of illness, sex, age, and converted antipsychotic equivalent dose as covariates or factors. Additional analyses used mixed model original values at baseline, 12 weeks’, and 24 weeks’ time points with duration of illness, sex, age, and converted antipsychotic equivalent dose as covariates or factors. Comparison of baseline characteristics between SFN and placebo groups used t tests, Mann-Whitney U, and χ2. Details of statistical analysis and sample size calculation are shown in Supplementary Material.
RESULTS
Participant Characteristics
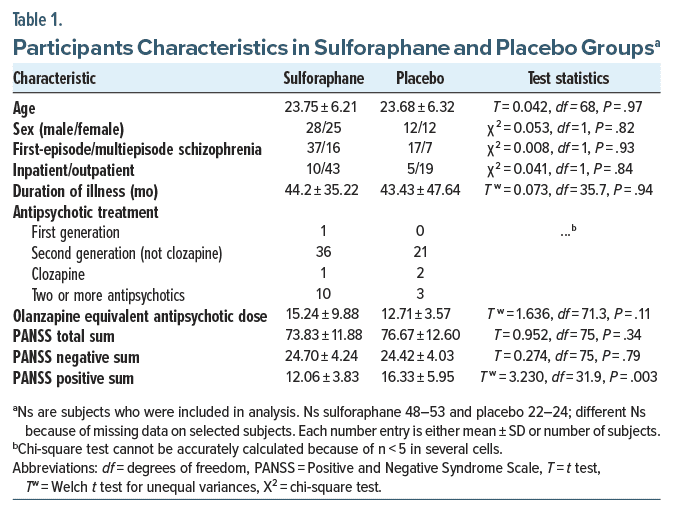
There were no differences in demographic and related characteristics (age, sex, and duration of illness) of the participants assigned to SFN or placebo (Figure 1; Table 1). The sample included both patients with first episode schizophrenia (70%) and multiepisode schizophrenia (30%), but there were no differences in the distribution between SFN and placebo participants. The patients had mean total PANSS scores of 74–77 in the 2 groups and a mean PANSS total negative symptom score of 24–25 in both groups; 95% of participants had higher total negative symptoms than positive symptoms and 84% having a negative symptom score ≥21. There was no significant difference in PANSS total or negative symptom scores between the 2 groups, but the placebo patients had higher positive symptoms (mean 16) than the SFN-treated patients (mean 12). The patients were treated with a variety of antipsychotic drugs, and the most frequently used antipsychotic medication administered was risperidone (see Supplementary Material for antipsychotic drug treatment distribution). However, there was no significant difference in the calculated olanzapine equivalent antipsychotic dose between the placebo and SFN groups.
Effects of SFN on PANSS Scores
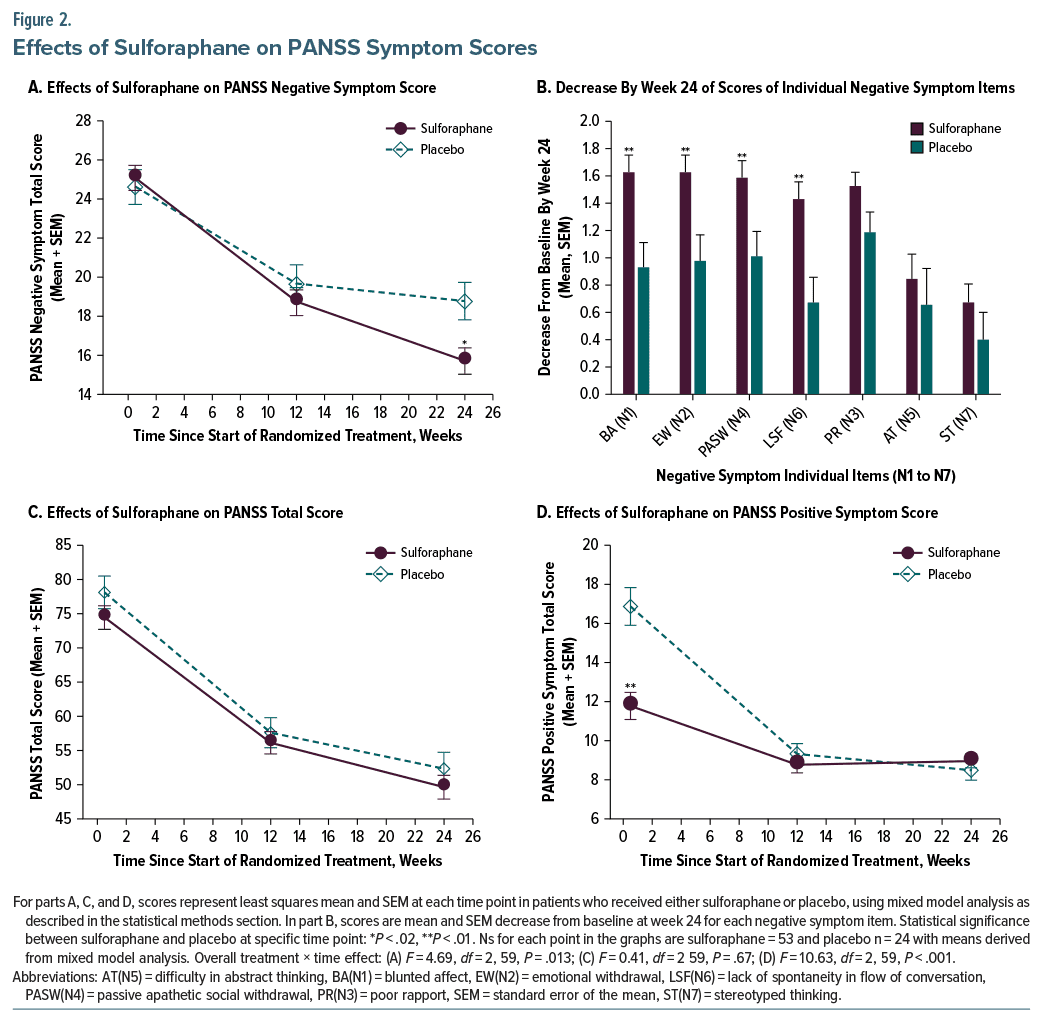
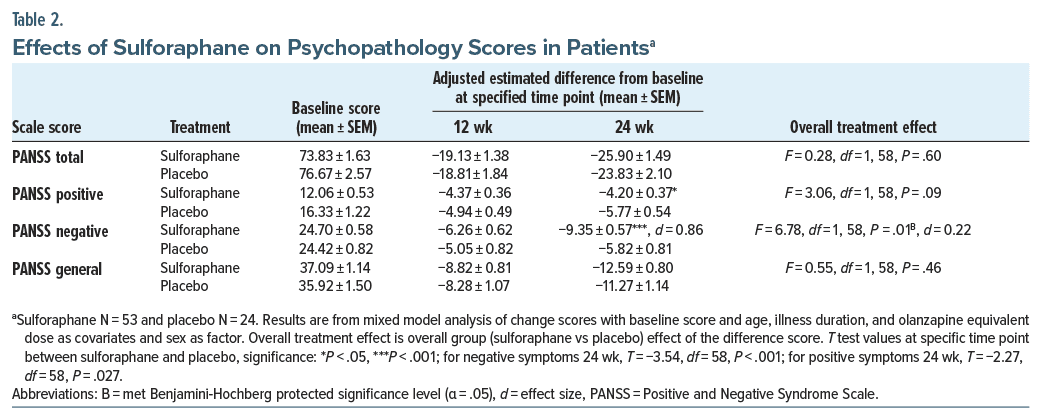
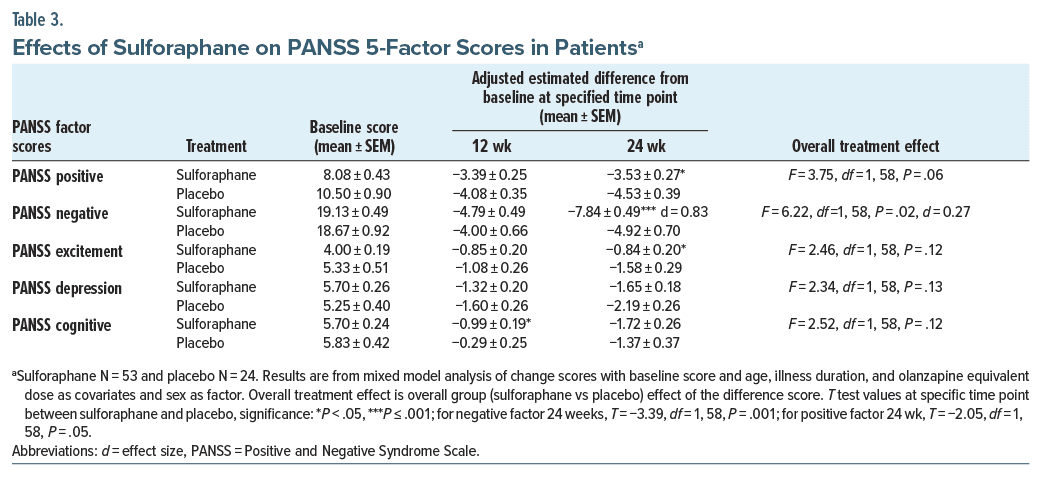
The SFN-treated group showed a significantly greater reduction in negative symptoms than the placebo group, and this effect was prominent at the 24-week treatment time point (see Figure 2 and Tables 2 and 3). This was evident in the analysis of PANSS negative symptom estimated mean scores at the evaluated time points (Figure 2, treatment × time overall effect F = 4.69, df = 1, 59, P = .01) and the analysis of the estimated mean decrease in scores from baseline (Tables 2 and 3). Both the decreases in PANSS negative symptom sum scores and the PANSS 5-factor negative symptom scores showed significant overall treatment effects (PANSS negative symptom sum score F = 6.78, df = 1, 58, P = .01 and PANSS 5-factor negative symptom score F = 6.22, df = 1, 58, P = .02). At the 24-week time point, the difference between SFN and placebo groups was highly significant (P ≤ .001) with about a 3-point greater decrease in the SFN group than in the placebo group. Effect size at the 24-week time point was high (d = 0.83–0.86). There was no difference in drug vs placebo effects on PANSS total scores, but there was a trend (P < .10) for positive symptoms to decrease more in the placebo group than in the SFN-treated group with a significant (P < .05) difference at the 24-week time point. Although PANSS 5-factor excitement and cognitive factors did not show overall drug effects, there were some significant differences between SFN and placebo groups at 12 or 24 weeks. There was a correlation between the decrease in PANSS negative and cognitive factor scores at 24 weeks (r = 0.40, P < .01) suggesting that decreases in cognitive deficits may accompany decreases in negative symptoms. However, a mediation analysis of the 5-factor PANSS negative symptom score showed that neither PANSS depression factor nor PANSS cognitive factor significantly mediated the decrease in negative symptom decrease at the 24-week time point ([Average Causal Mediation Effect] ACMEs Ps > .57).
Previous studies and meta-analysis showed that amisulpride had a significant effect on reducing negative symptoms in schizophrenia,4,6 and there was an imbalance in this antipsychotic treatment in the 2 groups in the current study. Seventeen patients in the SFN-treated group had amisulpride as their main or accessory antipsychotic, whereas only 1 patient in the placebo group was treated with amisulpride. We therefore performed additional statistical analyses to try to determine whether amisulpride treatment influenced the effect of SFN on negative symptoms. Results of a mediation analysis that we performed showed that amisulpride did not mediate the effects of SFN on reducing negative symptoms (PANSS negative sum difference at 24-week ACME= 0.56, P = .30 and PANSS negative factor difference at 24-week ACME= 0.19, P = .68). In additional mixed model analyses, in which amisulpride treatment was added as a factor, the amisulpride × group × time effect was not significant. Furthermore, in the SFN-treated patients, those not treated with amisulpride had a greater decrease in negative symptoms by week 24 than those treated with amisulpride (PANSS negative sum difference at 24 weeks [mean ± SD], participants not on amisulpride −9.59 ± 4.63, participants on amisulpride −6.18 ± 3.76, t test T = 2.58, df = 44, P = .01). These results support the contention that amisulpride was not a confounding factor explaining SFN’s effect on negative symptoms, but the marked imbalance in the number of participants on amisulpride in the SFN group vs placebo group may create problems in interpreting the statistical analyses and make our conclusions less certain.
We also examined whether SFN treatment affects some types of negative symptoms more than others. Comparing the difference in decrease in scores at 24 weeks, compared to baseline, items assessing blunted affect, emotional withdrawal, passive apathetic social withdrawal, and lack of spontaneity in flow of conversation showed a significant (P < .05) effect of SFN vs placebo group; poor rapport, difficulties in abstract thinking, and stereotyped thinking showed no significant effect of SFN (see Figure 2).
Safety and Tolerability
SFN was well tolerated compared to placebo as evaluated by the TESS scale and metabolic measures (see Supplementary Material for details).
DISCUSSION
The treatment of negative symptoms remains a challenge in the management of schizophrenia. These symptoms can be the most persistent, intractable, and disabling element of the illness for many patients. This study showed a significant effect of SFN compared to placebo on reducing negative symptoms in patients with schizophrenia. The effect on decreasing negative symptoms occurred with longer term treatment and was prominent at 24 weeks, but not 12 weeks of SFN treatment, with a large effect size at the 24-week time point. The SFN effect appeared to be specific for negative systems as measured by the PANSS. There were no changes in the overall global improvement as assessed by the CGI scale, and the decrease in negative symptoms was not mediated by changes in depression or cognitive symptoms or differences in amisulpride treatment. The placebo group had significantly higher positive symptoms at baseline than the SFN group, and this may have influenced the effects on their greater decrease in positive symptoms. The covariate of baseline positive symptoms was statistically significant in the mixed model analysis. However, since the analysis controlled for baseline positive symptoms and still found a decrease in positive symptoms in the placebo group, the higher baseline positive symptoms in this group cannot be the entire explanation for the greater decrease in the placebo group.
The relationship between decreases in negative symptoms and changes in cognition could not be fully evaluated because we did not employ more comprehensive measures of cognitive function and only could utilize the cognitive factor from the 5-factor PANSS. Although there was a positive correlation between decreases in the PANSS negative factor and cognitive factors, additional medication analysis showed that changes in the cognitive factor scores did not mediate decreases in negative symptoms.
The results of the current study differ from the findings of our earlier report of SFN effects in first- or early episode schizophrenia.18 In that study, we reported no effects of SFN on any PANSS scale measure. The differences in effect may be due to several differences between the 2 studies. The sample characteristics were different—a mixture of multiepisode schizophrenia and first-episode schizophrenia in this study, acute exacerbation with more severe total PANSS scores in the original study sample (approximately 90 in that earlier sample vs 73–76 in the current sample), and slightly higher baseline negative symptom scores in the current sample. Thus, the current sample had lower total and lower positive psychotic symptoms on the PANSS, and most of the participants had negative symptom scores higher than the positive symptom scores although they may not have met all criteria for the designation as predominantly negative symptom patients. The patients in this sample also likely received a much higher dose of SFN produced by the Extra Strength Avmacol SFN tablets used in this study (estimated SFN content ingested approximately 136 µmol/day) than in the previous SFN study (estimated SFN content ingested in the low-dose and high-dose SFN groups approximately 66 and 99 μmol/day). The treatment phase in the current study was slightly longer, and the main effect on decreasing negative systems was most prominent at the 24-week time point.
Two second-generation antipsychotic medications, cariprazine and amisulpride, have relatively strong evidence for having an effect on reducing negative symptoms in schizophrenia according to a recent meta analysis.6 The mean difference of approximately 3 points greater decrease in PANSS negative symptoms by SFN compared to placebo in this study is greater than the 1.46 difference in negative symptom decrease in the cariprazine vs risperidone study,27 which could suggest a larger effect of SFN augmentation in our study. However, we cannot fully assess whether the 3-point difference in our study is clinically meaningful. In the Nemeth et al27 study, the patients on cariprazine also showed improvement in CGI and in several functional outcome measures on the Personal and Social Performance Scale (PSP), whereas the current study showed no significant improvement in CGI-I or CGI-S scales, and we did not include additional measures for assessing functional outcomes. The fact that in the current study, global evaluation of improvement and total PANSS symptoms did not change more in the SFN group than in the placebo group, and the fact that positive symptoms decreased slightly more in the placebo group raises potential questions about the overall clinical benefit of the high-dose SFN.
Side effects of SFN were low compared to placebo, and only drowsiness decreased less in the SFN group from baseline to week 24. Items on the TESS scale related to extrapyramidal symptoms (akathisia, tremor, motor symptoms, etc) showed no significant change compared to the placebo, and this supports the contention that the change in negative symptoms was not related to changes in extrapyramidal symptoms.
This study has several limitations that may influence the interpretation of results. Although we had procedures for blinding patients and evaluations of the placebo or SFN medication administration, we did not have a questionnaire evaluation assessing the effectiveness of the blinding. Our choice of only 3 time points for measurements of symptoms during the course of the 24-week study may be insufficient to capture full fluctuations in PANSS measures. We did not include quantitative scales measuring EPS symptoms (such as the Simpson-Angus Scale or Barnes Akathisia Scale) which would have allowed a better assessment of the changes in extrapyramidal symptoms and their relationship to changes in negative symptoms. A lack of functional outcome measures such as the PSP makes it more difficult to assess the clinical meaning of the statistically significant decrease in negative symptoms. Although all patients’ medications remained unchanged during the trial, we did not collect precise data on doses of anticholinergic EPS medications on our patients. Moreover, the Avmacol Extra Strength SFN tablets also contain additional elements (Moringa leaves and β-glucans), so we cannot be certain that the total effect on decreasing negative symptoms was only due to SFN. Furthermore, we did not measure the concentration of SFN in plasma or blood cells. We did not control the diets of our participants, and it is possible that some participants consumed foods with broccoli extracts. However, the strong heating of the food before consumption, which is common in China, would likely destroy this SFN content in the diet.
CONCLUSIONS
The results of the current study showed that high dose SFN had statistically significant effect in reducing negative symptoms in patients with schizophrenia. The changes induced by SFN in negative symptoms were not mediated by changes in depression or cognition changes as assessed from the PANSS 5-factor scale. However, the substantial clinical import of this decrease in negative symptoms is tempered by the lack of SFN’s effect on measures of global improvement and the slightly greater decrease in positive symptoms in the placebo group. Additional studies are needed to confirm SFN’s effects and its clinical treatment implications.
Article Information
Published Online: January 20, 2025. https://doi.org/10.4088/JCP.24m15272
© 2025 Physicians Postgraduate Press, Inc.
Submitted: February 5, 2024; accepted October 30, 2024.
To Cite: Huang J, Chen A, Jin H, et al. A randomized controlled trial of the efficacy and safety of sulforaphane added to antipsychotics for the treatment of negative symptoms of schizophrenia. J Clin Psychiatry. 2025;86(1):24m15272.
Author Affiliations: Department of Psychiatry, and National Clinical Research Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, P. R. China (Huang, Teng, Xiao, Wu, Zhao, Shao); Columbia University Mailman School of Public Health, New York, New York (Chen); Department of Psychiatry, University of California San Diego and Psychiatric Service, VA San Diego Healthcare System, San Diego, California (Jin); Department of Neurosurgery, Xiangya Hospital, Central South University, Changsha, P. R. China (Liu); Department of Psychiatry, The First Affiliated Hospital of Zhengzhou University, Henan, China (Hei); Department of Psychiatry, University of Illinois, Chicago, Illinois (Davis); Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York, and Department of Psychiatry, New York University School of Medicine, New York, New York (Smith).
Corresponding Authors: Robert C. Smith, MD, PhD, Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York, and Department of Psychiatry, New York University School of Medicine, New York, NY ([email protected]); Ping Shao, MD, PhD, Department of Psychiatry, The Second Xiangya Hospital of Central South University, 139 Renmin Middle Rd, Changsha 410011, China ([email protected]).
Author Contributions: Data curation and writing–original draft: Huang; methodology, statistical analysis, and writing–review and editing: Chen; supervision and conceptualization: Jin and Wu; methodology: Liu; data curation: Hei, Teng, and Xiao; supervision: Zhao; supervision, methodology, and writing–review and editing: Davis; supervision and writing–review and editing: Shao; formal statistical analysis, graphs, methodology, writing–extensive revisions, and editing: Smith.
Relevant Financial Relationships: The authors report no financial or other relationship relevant to this article.
Funding/Support: This research was supported by a grant to Dr Huang from the Natural Science Foundation of Hunan (Grant No. 2022JJ40691) and the Science and Technology Innovation Program of Hunan Province (2024RC3055).
Role of the Sponsor: The funders had no role in the design, analysis, interpretation, or publication of this study. The products were procured by the research team from Nutramax through a Chinese company. The Nutramax Laboratories Consumer Care, Inc, played no part in the design of the study or interpretation of results.
Data Availability: The data and statistical analysis that support the findings of this study are available on request from the corresponding authors, primarily Dr Robert Smith.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Antipsychotics exhibit substantial efficacy in treating positive symptoms but have limited efficacy in treating negative symptoms.
- Sulforaphane, in higher doses, can be added as a safe and viable supplement to improve negative symptoms, but its effect should be evaluated during several months of treatment.
Editor’s Note: We encourage authors to submit papers for consideration as a part of our Early Career Psychiatrists section. Please contact Joseph F. Goldberg, MD, at psychiatrist.com/contact/goldberg.
References (27)

- McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia: an overview. JAMA Psychiatry. 2020;77(2):201–210.
- Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. CrossRef
- Bobes J, Arango C, Garcia-Garcia M, et al. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS study. J Clin Psychiatry. 2010;71(3):280–286. PubMed CrossRef
- Danion JM, Rein W, Fleurot O. Improvement of schizophrenic patients with primary negative symptoms treated with amisulpride. Amisulpride Study Group. Am J Psychiatry. 1999;156(4):610–616. PubMed CrossRef
- Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578–583. PubMed CrossRef
- Krause M, Zhu Y, Huhn M, et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta analysis. Eur Arch Psychiatry Clin Neurosci. 2018;268(7):625–639. CrossRef
- Davidson M, Saoud J, Staner C, et al. Efficacy and safety of roluperidone for the treatment of negative symptoms of schizophrenia. Schizophr Bull. 2022;48(3):609–619. PubMed CrossRef
- Vanduchova A, Anzenbacher P, Anzenbacherova E. Isothiocyanate from broccoli, sulforaphane, and its properties. J Med Food. 2019;22(2):121–126. PubMed CrossRef
- Elkashty OA, Tran SD. Sulforaphane as a promising natural molecule for cancer prevention and treatment. Curr Med Sci. 2021;41(2):250–269. PubMed CrossRef
- Leonard BE, Schwarz M, Myint AM. The metabolic syndrome in schizophrenia: is inflammation a contributing cause? J Psychopharmacol. 2012;26(5 suppl):33–41. PubMed CrossRef
- Maes M, Bosmans E, Calabrese J, et al. Interleukin-2 and interleukin-6 in schizophrenia and mania: effects of neuroleptics and mood stabilizers. J Psychiatr Res. 1995;29(2):141–152. PubMed CrossRef
- Bloomfield PS, Selvaraj S, Veronese M, et al. Microglial activity in people at ultra high risk of psychosis and in schizophrenia: an [(11)C]PBR28 PET brain imaging study. Am J Psychiatry. 2016;173(1):44–52. PubMed CrossRef
- Zhang M, Zhao Z, He L, et al. A meta-analysis of oxidative stress markers in schizophrenia. Sci China Life Sci. 2010;53(1):112–124. CrossRef
- Das TK, Javadzadeh A, Dey A, et al. Antioxidant defense in schizophrenia and bipolar disorder: a meta-analysis of MRS studies of anterior cingulate glutathione. Prog Neuropsychopharmacol Biol Psychiatry. 2019;91:94–102. PubMed CrossRef
- Fraguas D, Díaz-Caneja CM, Ayora M, et al. Oxidative stress and inflammation in first-episode psychosis: a systematic review and meta-analysis. Schizophr Bull. 2019;45(4):742–751. PubMed CrossRef
- Shirai Y, Fujita Y, Hashimoto R, et al. Dietary intake of sulforaphane-rich broccoli sprout extracts during juvenile and adolescence can prevent phencyclidine-induced cognitive deficits at adulthood. PLoS One. 2015;10(6):e0127244. PubMed CrossRef
- Hashimoto K. Recent advances in the early intervention in schizophrenia: future direction from preclinical findings. Curr Psychiatry Rep. 2019;21(8):75. PubMed CrossRef
- Hei G, Smith RC, Li R, et al. Sulforaphane effects on cognition and symptoms in first and early episode schizophrenia: a randomized double-blind trial. Schizophr Bull Open. 2022;3(1):sgac024. PubMed CrossRef
- Dickerson F, Origoni A, Katsafanas E, et al. Randomized controlled trial of an adjunctive sulforaphane nutraceutical in schizophrenia. Schizophr Res. 2021;231:142–144. PubMed CrossRef
- Wang J, Jiang Y, Tang Y, et al. Altered functional connectivity of the thalamus induced by modified electroconvulsive therapy for schizophrenia. Schizophr Res. 2020;218:209–218. PubMed CrossRef
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. CrossRef
- Guy W. ECDEU Assessment Manual for Psychopharmacology. US Department of Health, Education, and Welfare, Public Health Service; 1976.
- Berk M, Ng F, Dodd S, et al. The validity of the CGI severity and improvement scales as measures of clinical effectiveness suitable for routine clinical use. J Eval Clin Pract. 2008;14(6):979–983. PubMed CrossRef
- Health NIM. TESS (treatment emergent symptom scale-write-in). Psychopharmacol Bull. 1985;21:1069–1072. PubMed
- Davis JM, Chen N. The effects of olanzapine on the 5 dimensions of schizophrenia derived by factor analysis: combined results of the North American and international trials. J Clin Psychiatry. 2001;62(10):757–771. PubMed CrossRef
- Jiang J, Sim K, Lee J. Validated five-factor model of positive and negative syndrome scale for schizophrenia in Chinese population. Schizophr Res. 2013;143(1):38–43. PubMed CrossRef
- Nemeth G, Laszlovszky I, Czobor P, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomised, double-blind, controlled trial. Lancet. 2017;389(10074):1103–1113. PubMed CrossRef
This PDF is free for all visitors!