Abstract
Objective: This post hoc analysis of the ESCAPE-TRD trial compared work productivity loss (WPL) and related costs among patients with treatment-resistant depression (TRD) receiving esketamine nasal spray or quetiapine extended release in combination with an oral antidepressant.
Methods: Adults with TRD randomized to receive esketamine (56/84 mg) or quetiapine (150–300 mg) combined with ongoing antidepressant therapy were included. WPL was assessed using the Work Productivity and Activity Impairment questionnaire. Least squares (LS) mean WPL change versus baseline (treatment initiation date), and LS mean differences (MDs) between esketamine and quetiapine cohorts were reported at weeks 8–32 of treatment using mixed models for repeated measurements. Per patient productivity cost savings were estimated using mean 2021 weekly wages from US Bureau of Labor Statistics.
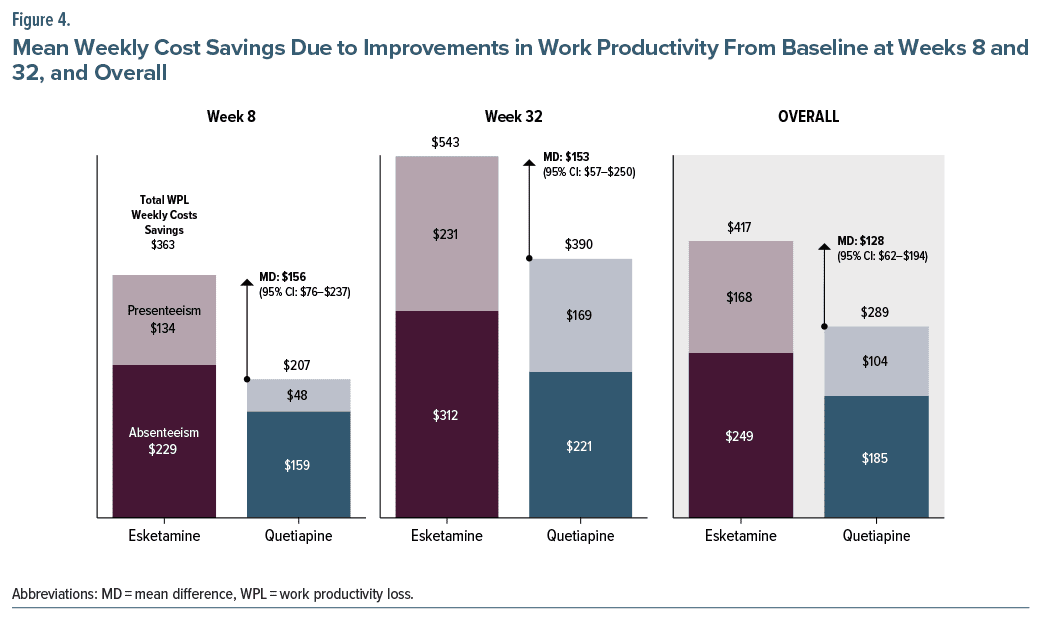
Results: The esketamine cohort included 165 patients, and quetiapine cohort included 156 patients. At baseline, total WPL was 77.0% and 72.5% in the esketamine and quetiapine cohorts, respectively. By week 8, total WPL decreased from baseline by 30.3 and 17.3 percentage points (pp) in the esketamine and quetiapine cohorts (MD = 13.0 pp; 95% confidence interval [CI], 6.3–19.8 pp), resulting in weekly cost savings of $363 and $207 (MD = $156; 95% CI, $76–$237), respectively. By week 32, total WPL decreased from baseline by 45.3 pp and 32.5 pp in the esketamine and quetiapine cohorts (MD = 12.7 pp; 95% CI, 4.7–20.7 pp), with weekly cost savings of $543 and $390 (MD = $153; 95% CI, $57–$250), respectively.
Conclusion: Among employed adults with TRD, esketamine treatment was associated with significantly larger improvements in WPL and related costs compared to quetiapine, suggesting greater benefits from patient well-being and employer perspectives.
J Clin Psychiatry 2025;86(1):24m15425
Author affiliations are listed at the end of this article.
Major depressive disorder (MDD) is among the most common chronic illnesses in the United States (US), with around 9 million adults receiving treatment for it in 2017.1 Treatment-resistant depression (TRD) is often defined as MDD that does not respond to ≥2 antidepressant treatment courses with adequate dosing and duration and affects approximately a third of treated adults with MDD.1,2 Unlike many other common chronic disorders, MDD and TRD affect a relatively young population, with the prevalence of major depressive episodes, particularly those with severe impairment, being the highest among adults both entering prime working age and of prime working age.3 It is thus unsurprising that these conditions are a major factor for disability and work productivity loss (WPL) in the US. The unemployment and productivity burden associated with pharmacologically treated MDD in the US is estimated to be $29.2 billion annually, with over 60% of the burden attributable to TRD.1 Attenuating these ramifications of MDD and TRD could have important societal gains.
In 2019, the US Food and Drug Administration approved esketamine, the S-enantiomer of ketamine, as a novel treatment for TRD.4 In contrast to typical antidepressants, which are taken orally and can take up to 8 weeks to reach full efficacy,5 esketamine is administered intranasally and provides rapid relief from depressive symptoms6 and thus has the potential to address the unmet medical needs of patients with TRD.7 Furthermore, relative to the standard of care, which is typically an antidepressant in combination with a second-generation antipsychotic (SGA),8 the combination of esketamine with an antidepressant was associated with superior treatment response and disease remission.9
Though the clinical benefit of esketamine in reducing depressive symptoms has been established, its societal benefit remains to be understood.9 To that end, this post hoc analysis of the ESCAPE-TRD trial was conducted to compare WPL outcomes collected based on the Work Productivity and Activity Impairment (WPAI) depression questionnaire10 and complimented with costs estimated from the US market perspective using the human capital approach,11–13 between patients treated with either esketamine or quetiapine, an extended release antipsychotic, both in combination with an ongoing antidepressant and dosed according to the US labels.
METHODS
Study Design and Sample Selection
The ESCAPE-TRD trial had an open-label, single blind (with raters unaware of cohort assignment), randomized, active-controlled design spanning 24 countries. It included 18- to 74-year-old participants with TRD, defined as a score of ≥34 on the 30-item Inventory of Depressive Symptomatology-Clinician Rated scale and failing (<25% reduction in symptoms) 2–6 consecutive treatments within the current major depressive episode, including their last treatment with a selective serotonin reuptake inhibitor (SSRI) or serotonin and norepinephrine reuptake inhibitor (SNRI).14 Participants were randomly assigned to receive esketamine nasal spray or extended-release quetiapine while continuing their last SSRI or SNRI; the randomization was stratified by participant age (18 to ≤64, ≥65) and number of past treatments failed (2, ≥3). The ESCAPE-TRD trial was conducted in accordance with the principles of the Declaration of Helsinki15; country-specific ethics review boards approved the trial.
The sample used for this post hoc analysis was restricted to adults between 18 and 64 years old from the ESCAPE-TRD trial who had received treatment consistent with US label dosing for esketamine (ie, 56/84 mg twice weekly for the first 4 weeks, then every 1 or 2 weeks) and quetiapine (ie, 150–300 mg daily) and had a score for absenteeism, presenteeism, or total WPL based on the WPAI questionnaire on the date of treatment initiation.
Outcome Measures
Patient-reported work productivity was evaluated based on the WPAI scores, which represented a supportive secondary end point in the ESCAPE-TRD trial. The WPAI questionnaire is a patient-filled survey based on a recall period of 7 days10 and contains the following questions: Q1 = currently employed (yes/no); Q2 = hours missed due to depression-related health problems; Q3 = hours missed due to other reasons; Q4 = hours actually worked; Q5 = degree depression related health affected productivity while working (0–10 rating scale [0: depression had no effect on my work; 10: depression symptoms completely prevented me from working]); and Q6 = degree depression-related health affected regular activities (0–10 rating scale [0: depression had no effect on my regular activities; 10: depression symptoms completely prevented me from my regular activities]).
The baseline WPAI scores corresponded to the date of study treatment initiation in the ESCAPE-TRD trial. During a 32-week treatment period comprising an initial treatment phase of 8 weeks and a maintenance phase of 24 weeks, the WPAI outcomes were reported every 4 weeks. The WPAI outcomes included in this post hoc analysis were those for which costs could be estimated from an employer’s perspective: absenteeism, defined as the percentage of time absent from work last week due to depression-related health problems (calculated as Q2/(Q2 + Q4) × 100%), presenteeism, defined as the degree health problems affected work productivity in the last week (calculated as (Q5/10) × 100%), and total WPL associated with depression in the prior week, defined as [absenteeism +(1−absenteeism) * presenteeism] × 100%. The costs associated with total WPL were estimated per patient in 2021 US dollars based on the average US weekly wages obtained from the US Bureau of Labor Statistics (BLS), whereby the mean annual wage in 2021 was $62,411 (based on the BLS Current Population Survey16) and the mean number of hours worked per week in 2021 in the United States was 40.5 hours (based on the BLS American Time Use Survey17), resulting in a mean hourly wage of $29.6.
Sensitivity analyses for hourly wage. Sensitivity analyses were conducted to account for the variation in mean hourly wages between males and females and full-time and part time employees. This was an important consideration as the majority of patients with TRD are known to be female18 and a higher proportion of patients with depression are likely to work part-time than the general US population.19 Therefore, costs of absenteeism, presenteeism, and total WPL were also estimated reweighting the mean hourly wage based on the proportion of females in the esketamine cohort (64.2%; resulting in a mean wage of $28.0/hour) and based on the proportion of both females and part-time workers among US adults with a major depressive episode (29.7%; $26.5/hour).19
Statistical Analyses
The mean change from baseline for the WPAI outcomes of interest at each visit was evaluated using mixed models for repeated measurements, which included the baseline score as a covariate, and the study intervention, age and number of treatment failures, visit, and visit-by-treatment interaction as fixed effects using an unstructured covariance matrix. The least squares (LS) mean change from baseline in WPAI outcomes and the corresponding LS mean difference (MD) in the change from baseline between patients receiving esketamine (ie, esketamine cohort) and those receiving quetiapine (ie, quetiapine cohort) were reported at weeks 8 and 32, as well as across all visits (ie, overall which was the mean of weeks 8, 12, 16, 20, 24, 28, and 32).
The costs associated with absenteeism and total WPL (ie, absenteeism and presenteeism combined) for the esketamine and quetiapine cohorts at each time point were calculated by multiplying the number of hours lost due to TRD during a given week (ie, absenteeism and total WPL scores multiplied by mean hours worked per week in the US, ie, 40.5 hours) by the mean hourly wages. The costs of presenteeism were then calculated as the difference between the total WPL costs and the absenteeism costs. The mean change in cost savings due to improvements in total WPL from baseline to weeks 8, 32, and overall, for the esketamine and quetiapine cohorts, and the MD in change in costs between the 2 cohorts were calculated as simple differences and reported per week. Results were annualized by multiplying the overall mean change in weekly cost savings and overall MD in change between the 2 cohorts by 52 weeks.
RESULTS
Baseline Characteristics
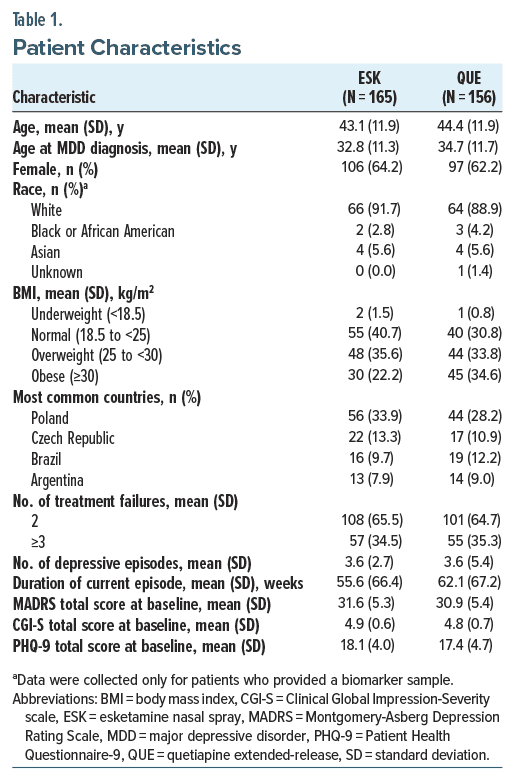
Of the 676 patients in the overall ESCAPE-TRD trial, 165 patients met the inclusion criteria for this post hoc analysis in the esketamine cohort and 156 patients in the quetiapine cohort (Table 1). The mean age was 43.1 years in the esketamine cohort and 44.4 years in the quetiapine cohort. In both cohorts, over 60% were female, and the vast majority were white (esketamine cohort: 91.7%; quetiapine cohort: 88.9%). Patients in both cohorts had been living with depression for 10 years on average, and a third of the participants in each cohort had ≥3 treatment failures prior to initiating esketamine or quetiapine. At baseline, the esketamine cohort reported 77.0% total WPL, 43.4% absenteeism, and 71.3% presenteeism, and the quetiapine cohort reported 72.5% total WPL, 37.5% absenteeism, and 66.2% presenteeism.
Work Productivity Loss
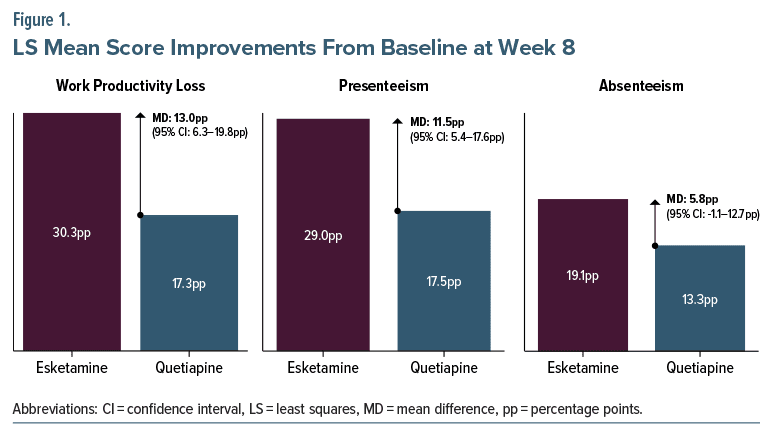
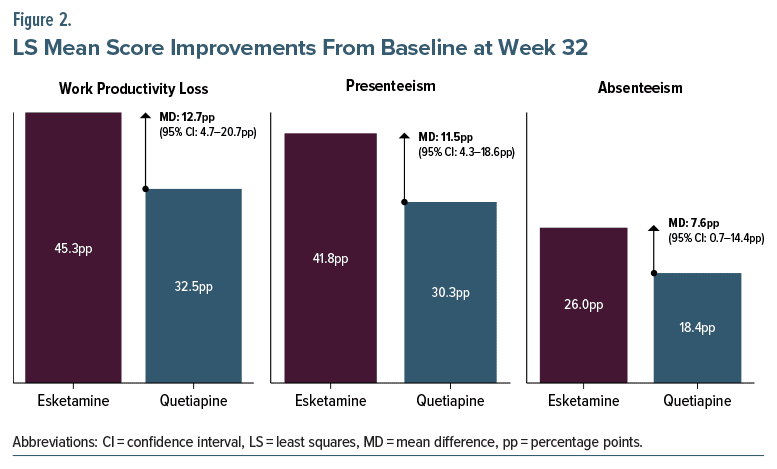
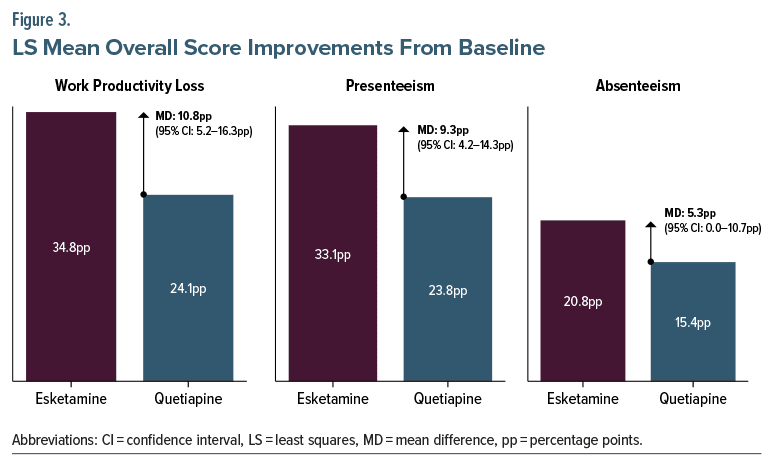
By week 8, LS mean total WPL improved from baseline by 30.3 percentage points (pp) in the esketamine cohort compared to 17.3 pp in the quetiapine cohort, with a MD of 13.0 pp additional improvement in the esketamine cohort over the quetiapine cohort (95% confidence interval [CI], 6.3–19.8 pp; Figure 1). By week 32, the LS mean total WPL improved from baseline by 45.3 pp in the esketamine cohort compared to 32.5 pp in the quetiapine cohort, corresponding to a MD of 12.7 pp in additional improvement among patients in the esketamine cohort than the quetiapine cohort (95% CI, 4.7–20.7 pp; Figure 2). Overall, the LS mean total WPL improved from baseline by 34.8 pp in the esketamine cohort compared to 24.1 pp in the quetiapine cohort; thus, patients in the esketamine cohort saw an improvement of 10.8 pp more than the quetiapine cohort across all visits (95% CI, 5.2–16.3 pp; Figure 3). Across all time points, patients in the esketamine cohort saw greater improvements in both absenteeism and presenteeism compared to the quetiapine cohort; presenteeism scores improved more than absenteeism scores in both cohorts.
Costs of Work Productivity Loss
The larger improvements in total WPL from baseline in the esketamine cohort compared to the quetiapine cohort translated to significantly higher weekly cost savings (Figure 4). At week 8, each patient in the esketamine cohort saved $363 per week due to improvements in total WPL which was $156 more than the quetiapine cohort (95% CI, $76–$237), and at week 32, the esketamine cohort saved $543 per patient week which was $153 more than the quetiapine cohort (95% CI, $57–$250). Overall, the esketamine cohort saved $417 per patient per week which was $128 more than the quetiapine cohort (95% CI, $62–$194).
Annualizing the weekly cost savings due to improvement in total WPL, treatment with esketamine was estimated to be associated with $21,694 in cost savings per patient per year, which was $6,670 more compared to treatment with quetiapine, both in combination with an antidepressant.
Despite the fact that presenteeism was the aspect of productivity loss that improved the most from baseline in both cohorts, total cost savings associated with each treatment were predominantly driven by improvements in absenteeism, accounting for ≥60% of the total savings observed in both cohorts. This was due to costs of absenteeism comprising a larger share of total costs of WPL at baseline.
Sensitivity Analyses
The findings remained consistent when the WPL costs were reweighted to account for the variation in mean hourly wages between males and females and between full-time and part-time workers. When reweighting by the proportion of females alone, the esketamine cohort had cost savings of $392 per week overall due to improvements in total WPL which was $121 more than the quetiapine cohort (95% CI, $58–$182). When reweighting by the proportion of females and part-time workers, the esketamine cohort saved $371 per patient per week overall due to improvements in total WPL, which was $114 more than the quetiapine cohort (95% CI, $55–$172). Annualizing these data, treatment with esketamine plus an antidepressant was associated with mean cost savings of $20,384 per patient, which was $6,292 more compared to treatment with quetiapine plus an antidepressant when reweighting hourly wages by the proportion of females only; the respective estimates were $19,292 and $5,928 when reweighting hourly wages by the proportion of both females and part-time workers.
DISCUSSION
Among employed adults with TRD, treatment with esketamine was associated with significantly greater improvements in total WPL compared to quetiapine, both in combination with an antidepressant, which translated to significantly larger cost savings. The comparative advantage of esketamine versus quetiapine in terms of cost savings remained robust in sensitivities accounting for variation in mean hourly wages between males and females and full-time and part-time employees. In 2021, the annual prevalence of TRD was estimated at 2.8 million adults,1 and the annual productivity burden of TRD was estimated at $9.3 billion in the United States.2 Based on the annual cost savings per patient due to improved productivity associated with esketamine in this study, treating even 15% of the population with TRD with esketamine could potentially offset the total productivity burden of TRD, not accounting for the cost of treatment.
In the WPAI questionnaire, absenteeism is reported based on the question “during the past seven days, how many hours did you miss from work because of problems associated with depression?” and it is specified that respondents should not include time missed due to participating in the study in this measure. Depending on how the question is understood, the hours of absenteeism may not include hours spent obtaining treatment for depression. Each esketamine dose may require 3 hours of patient time for administration, monitoring, and travel to and from a treatment center.20 Thus, 32 weeks of treatment will require 108 hours of patient time, assuming treatment sessions twice per week for the first 4 weeks (induction) and weekly sessions afterward. With the mean hourly wage of $29.6, this would translate into $3,197 of productivity loss over 32 weeks vs $4,096 of productivity cost savings due to treatment for net savings of $899. Therefore, even if the measure of absenteeism did not originally account for patient time necessary to receive esketamine treatment, there are still productivity benefits in using esketamine versus quetiapine, both in combination with an antidepressant. It should be noted that the cost of esketamine may be higher than generic augmentation medications; however, this analysis does not make any claims about the cost-effectiveness of esketamine, which was previously assessed elsewhere.20–22
This post hoc analysis used WPL data from the ESCAPE-TRD trial; costs associated with WPL were estimated using US labor market conditions, based on mean weekly wages and mean number of hours worked per week obtained from the US BLS.16,17 Similar methodology has been commonly used in published work across multiple chronic disease areas, including atopic dermatitis, irritable bowel syndrome, and psoriasis.11–13 The demographic characteristics of patients with TRD included in this post hoc analysis were largely consistent with those of patients included in prior real-world studies conducted in the US.18,23 The results from this study complement findings of a recent real-world claims-based study among patients with TRD in the US which showed greater reduction in disability days and costs 6 months after initiation of esketamine versus a SGA in combination with an antidepressant.24 SGAs, such as quetiapine, work across the class by blocking D2 dopamine receptors as well as serotonin receptor antagonist action. Thus, given the somewhat comparable mechanisms of action, it may be reasonable to expect comparable effects relative to augmentation with other SGAs. Together, the findings suggest that esketamine treatment is associated with greater benefits from patient’s well-being and employer’s perspectives compared to the standard of care, antipsychotic augmentation treatment.
In the real-world setting, patients undergo at least 2 lines of treatment on average, often with antipsychotic augmentation, after evidence of TRD and before they initiate esketamine.25 Some patients may also receive antipsychotic augmentation along with esketamine. The findings of this study suggest potential gains of initiating patients on esketamine earlier after evidence of TRD instead of letting them cycle through additional lines of antidepressants augmented with antipsychotics. Further, although esketamine is a rapidly acting medication, the results of this study highlight the importance of continued esketamine treatment according to the label for a cumulative durable treatment effect, as greater improvements in WPL were observed after 32 weeks of treatment relative to 8 weeks.
Limitations
The results of this study should be interpreted in light of certain limitations. First, the open-label design of the ESCAPE-TRD trial could have increased the risk of early discontinuation of the trial treatment due to the patient’s awareness of the treatment received. Nonetheless, a retrieved dropout analysis showed that the difference between the cohorts in the number of patients who discontinued the trial treatment had a minimal effect on end point results. Second, the results which were based on the WPAI questionnaire may have been subject to recall bias as well as a perceived treatment efficacy (ie, expectation bias) caused by the awareness of treatment assignment and the greater frequency of clinical interactions for patients in the esketamine cohort. However, the frequency of clinical interactions in the esketamine cohort reflected the expected frequency of interactions during treatment with esketamine in clinical practice while the frequency of interactions in the quetiapine cohort was greater than that in clinical practice. Third, for the annual cost savings calculation, mean cost savings over the first 32 weeks were assumed to be equal to the mean cost savings over the next 20 weeks. Fourth, both esketamine and quetiapine are associated with adverse events that may impact work productivity, such as sedation, dizziness, and nausea.26,27 Finally, as the ESCAPE-TRD trial included patients from multiple countries and costs were estimated from a US market perspective using the most recent labor data available (ie, 2021), WPAI outcomes may not be fully reflective of the entire US population and the most recent labor market conditions. Additionally, racial minorities may have been underrepresented in the study sample.
CONCLUSIONS
Among employed adults with TRD receiving esketamine or quetiapine, both in combination with an antidepressant, esketamine was associated with a significantly larger reduction in WPL, which translated to larger annual cost savings. Since esketamine relative to quetiapine augmentation therapy may yield larger benefits from a patient well-being and employer perspective, it may be recommended to initiate esketamine shortly after evidence of TRD instead of opting for augmentation with antipsychotics.
Article Information
Published Online: January 27, 2025. https://doi.org/10.4088/JCP.24m15425
© 2025 Physicians Postgraduate Press, Inc.
Submitted: May 10, 2024; accepted October 17, 2024.
To Cite: Clemens K, Teeple A, Zhdanava M, et al. Esketamine nasal spray vs quetiapine extended-release: examining work productivity loss and related costs in patients with treatment-resistant depression. J Clin Psychiatry. 2025;86(1):24m15425.
Author Affiliations: Right Solutions Mental Health, LLC, Gaithersburg, Maryland (Clemens); Janssen Scientific Affairs, LLC, a company of Johnson & Johnson, Titusville, New Jersey (Teeple, Joshi, Bowrey); Analysis Group, Inc, Montréal, Quebec, Canada (Zhdanava, Shah, Pilon); Janssen Pharmaceutica NV, Beerse, Belgium (Buyze); Janssen EMEA, Sofia, Bulgaria (Godinov).
Corresponding Author: Maryia Zhdanava, MA, Analysis Group, Inc, 1190 avenue des Canadiens-de-Montréal, Suite 1500, Montréal, QC H3B 0G7, Canada
([email protected]).
Relevant Financial Relationships: Ms Clemens has served on an advisory board for Janssen Pharmaceuticals, as a speaker for AbbVie, and as a consultant for Biogen and Sage. Drs Teeple, Buyze, Bowrey, and Godinov and Ms Joshi are employees and stockholders of Johnson & Johnson. Mss Zhdanava and Shah and Mr Pilon are employees of Analysis Group, Inc, a consulting company that has provided paid consulting services to Janssen Scientific Affairs, LLC, a company of Johnson & Johnson, which funded the development and conduction of this study.
Funding/Support: This study was funded by Janssen Scientific Affairs, LLC, a company of Johnson & Johnson.
Role of the Sponsor: Janssen Scientific Affairs, LLC, a company of Johnson & Johnson, was involved in several aspects of the research, including the study design, interpretation of data, and writing of the manuscript; the final decision to submit the manuscript for publication was the sole decision of the authors.
Previous Presentation: Part of the material in this article was presented in a poster at the Psych Congress 2023; September 6–10, 2023; Nashville, Tennessee.
Acknowledgments: Medical writing assistance was provided by professional medical writer, Loraine Georgy, PhD, MWC, an employee of Analysis Group, Inc, a consulting company that has provided paid consulting services to Janssen Scientific Affairs, LLC, a company of Johnson & Johnson, which funded the development and conduct of this study and manuscript.
Clinical Points
- This ESCAPE-TRD trial post hoc analysis compared work productivity loss and the related costs among employed adults with treatment-resistant depression receiving esketamine nasal spray or quetiapine extended-release combined with an oral antidepressant.
- Esketamine was associated with significant improvements in outcomes compared to quetiapine, which may correspond to greater benefits from the patient and societal perspectives, especially if initiated early.
References (27)

- Zhdanava M, Pilon D, Ghelerter I, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82(2):20m13699. PubMed
- U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Major Depressive Disorder: Developing Drugs for Treatment Guidance for Industry. 2018. Accessed January 10, 2024. https://www.fda.gov/media/113988/download
- Substance Abuse and Mental Health Services Administration, Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2022.
- US Food and Drug Administration. FDA approves new nasal spray medication for treatment-resistant depression; available only at a certified doctor’s office or clinic. 2019. Accessed January 10, 2024. https://www.fda.gov/news-events/pressannouncements/fda-approves-new-nasal-spray-medication-treatmentresistant-depression-available-only-certified
- Gelenberg AJ, Freeman MP, Markowitz JC, et al. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed; 2010:1–152.
- Bahr R, Lopez A, Rey JA. Intranasal esketamine (Spravato(TM)) for use in treatment-resistant depression in conjunction with an oral antidepressant. P T. 2019;44(6):340–375.
- Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428–438. PubMed
- Voineskos D, Daskalakis ZJ, Blumberger DM. Management of treatment resistant depression: challenges and strategies. Neuropsychiatr Dis Treat. 2020;16:221–234.
- Reif A, Yağcıoğlu AA, Luts A, et al. Esketamine nasal spray shows higher remission and response rates over 32 weeks of treatment compared with quetiapine extended-release in patients with treatment resistant depression: results from ESCAPE-TRD, a randomised, phase IIIb clinical trial. Eur Psychiatry. 2023;66(S1):S90–S91.
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365.
- Bloudek L, Eichenfield LF, Silverberg JI, et al. Impact of ruxolitinib cream on work productivity and activity impairment and associated indirect costs in patients with atopic dermatitis: pooled results from two phase III studies. Am J Clin Dermatol. 2023;24(1):109–117.
- Buono JL, Carson RT, Flores NM. Health-related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual Life Outcomes. 2017;15(1):35–38.
- Villacorta R, Teeple A, Lee S, et al. A multinational assessment of work related productivity loss and indirect costs from a survey of patients with psoriasis. Br J Dermatol. 2020;183(3):548–558. PubMed
- Clinicaltrials.gov (NCT04338321). A long-term comparison of esketamine nasal spray versus quetiapine extended release, both in combination with a selective serotonin reuptake inhibitor/serotonin-norepinephrine reuptake inhibitor, Participants With Treatment Resistant Major Depressive Disorder (ESCAPE-TRD); 2023. Accessed April 26, 2023. https://clinicaltrials.gov/study/NCT04338321
- World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013:2191–2194.
- PINC-10. Wage and Salary Workers—People 15 Years Old And Over by Total Wage and Salary Income, Work Experience, Race, Hispanic Origin, and Sex. 2021. Accessed April 26, 2023. https://www.census.gov/data/tables/time-series/demo/income-poverty/cps-pinc/pinc-10.html
- Average hours employed people spent working on days worked by day of week. 2021. Accessed April 26, 2023. https://www.bls.gov/charts/americantime-use/emp-by-ftpt-job-edu-h.htm
- Amos TB, Tandon N, Lefebvre P, et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression: a matched-cohort study using a US commercial claims database. J Clin Psychiatry. 2018;79(2):17m11725. PubMed
- National Survey of Drug Use and Health (NSDUH). 2021. Accessed April 26, 2023. https://www.samhsa.gov/data/sites/default/files/reports/rpt39441/NSDUHDetailedTabs2021/NSDUHDetailedTabs2021/NSDUHDetTabsSect6pe2021.htm
- Ross EL, Soeteman DI. Cost-effectiveness of esketamine nasal spray for patients with treatment-resistant depression in the United States. Psychiatr Serv. 2020;71(10):988–997.
- Desai U, Kirson NY, Guglielmo A, et al. Cost-per-remitter with esketamine nasal spray versus standard of care for treatment-resistant depression. J Comp Eff Res. 2021;10(5):393–407.
- Le HH, Zhang Q, Sheehan JJ. PMH23 Budget impact analysis of esketamine in treatment-resistant depression in the United States. Value Health. 2019;22:S229–S230.
- Pilon D, Sheehan JJ, Szukis H, et al. Medicaid spending burden among beneficiaries with treatment-resistant depression. J Comp Eff Res. 2019;8(6):381–392.
- Zhdanava M, Karkare S, Voegel A, et al. Mental-Health Related Disability Leave and Costs Among Patients with Treatment Resistant Depression Initiated on Esketamine and Conventional Therapies. 2023 NEI Congress; November 9–12, 2023; Colorado Springs, CO. Accessed January 10, 2024.
- Teeple A, Zhdanava M, Pilon D, et al. Access and real-world use patterns of esketamine nasal spray among patients with treatment-resistant depression covered by private or public insurance. Curr Med Res Opin. 2023;39(8):1167–1174. PubMed CrossRef
- Anderson IM, Sarsfield A, Haddad PM. Efficacy, safety and tolerability of quetiapine augmentation in treatment resistant depression: an open-label, pilot study. J Affect Disord. 2009;117(1–2):116–119. PubMed
- Williamson DJ, Gogate JP, Kern Sliwa JK, et al. Longitudinal course of adverse events with esketamine nasal spray: a post hoc analysis of pooled data from phase 3 trials in patients with treatment-resistant depression. J Clin Psychiatry. 2022;83(6):21m14318. PubMed
This PDF is free for all visitors!