Behind the Manuscript: Listen to Dr. Sibley on The JCP Podcast
Abstract
Objectives: Recent studies report a fluctuating course of attention-deficit/ hyperactivity disorder (ADHD) across development characterized by intermittent periods of remission and recurrence. In the Multimodal Treatment of ADHD (MTA) study, we investigated fluctuating ADHD including clinical expression over time, childhood predictors, and between- and within-person associations with factors hypothesized as relevant to remission and recurrence.
Methods: Children with DSM-5 ADHD, combined type (N = 483), participating in the MTA adult follow-up were assessed 9 times from baseline (mean age = 8.46) to 16-year follow-up (mean age = 25.12). The fluctuating subgroup (63.8% of sample) was compared to other MTA subgroups on variables of interest over time.
Results: The fluctuating subgroup experienced multiple fluctuations over 16 years (mean = 3.58, SD = 1.36) with a 6- to 7-symptom within-person difference between peaks and troughs. Remission periods typically first occurred in adolescence and were associated with higher environmental demands (both between- and within-person), particularly at younger ages. Compared to other groups, the fluctuating subgroup demonstrated moderate clinical severity. In contrast, the stable persistent group (10.8%) was specifically associated with early and lasting risk for mood disorders, substance use problems in adolescence/ young adulthood, low medication utilization, and poorer response to childhood treatment. Protective factors were detected in the recovery group (9.1%; very low parental psychopathology) and the partial remission group (15.6%; higher rates of comorbid anxiety).
Conclusions: In the absence of specific risk or protective factors, individuals with ADHD demonstrated meaningful within-individual fluctuations across development. Clinicians should communicate this expectation and monitor fluctuations to trigger as-needed return to care. During remission periods, individuals with ADHD successfully manage increased demands and responsibilities.
Trial Registration: ClinicalTrials.gov identifier: NCT00000388
J Clin Psychiatry 2024;85(4):24m15395
Author affiliations are listed at the end of this article.
See commentary by Surman and Wilens
Attention-deficit/hyperactivity disorder (ADHD) is historically characterized as a chronic childhood neurodevelopmental disorder with approximately 50% persistence in adulthood.1 Several recent studies detected a fluctuating course of ADHD, challenging the notion that childhood ADHD either permanently remits or persists in adulthood.2–6 These studies raise a possibility that ADHD is trait-like and waxing and waning (like hypertension or obesity)7; still, the nature of fluctuating ADHD remains poorly understood.
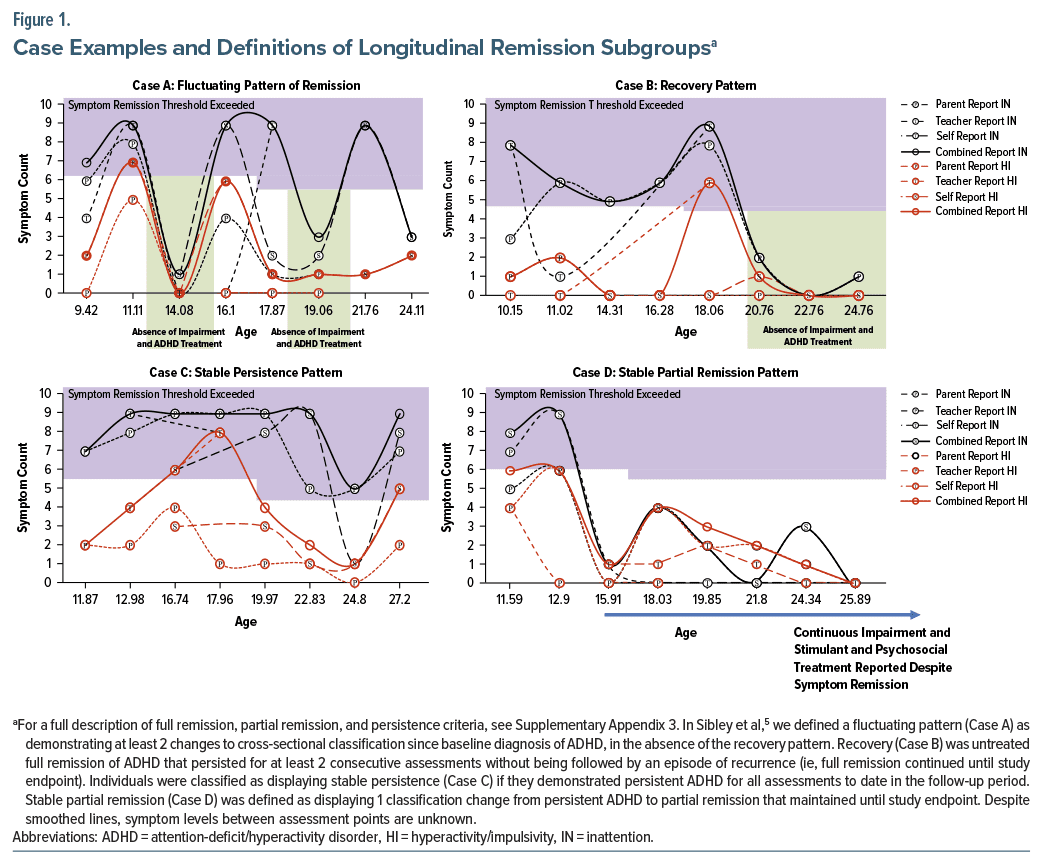
In the Multimodal Treatment of ADHD (MTA) long term follow-up,5 fluctuating ADHD occurred in 63.8% of the sample, characterized by alternating periods of remission and recurrence. Yet, the detailed experiences of fluctuating cases remain uncharacterized, including determinants of stable vs fluctuating ADHD. Childhood factors distinguishing endpoint-defined persistent vs remitted ADHD are numerous and include demographic, clinical (eg, childhood symptoms, comorbidities), and contextual factors (eg, parenting, negative events, psychosocial risks).8–10 However, these variables may not be predictive of varying courses of ADHD (stable persistent ADHD, stable partial remission, recovery, fluctuating; see Figure 1).5
Since ADHD often fluctuates, the field also must begin investigating variables that trigger symptom exacerbation and abatement (ie, do changes to one’s environment coincide with the onset of a fluctuation?). Some research suggests that ADHD severity intensifies under increased executive function burden.11,12 Other work suggests that adults with ADHD perceive that their symptoms are best managed in demanding, fast-paced, and stimulating environments.13,14 Such mixed findings indicate a need for complex analyses that model individual differences in remission (eg, disaggregating between- vs within-person trends), model bidirectionality, and moderators of effects and consider nonlinear relations in the data. Clarifying factors that predict ADHD course and fluctuations may signal novel person-specific intervention targets.
This study provides detailed comparison of the MTA’s fluctuating ADHD subgroup to the stable ADHD and remission subgroups. We examine correspondence between previously reported binary (endpoint) symptom persistence15 and longitudinal persistence classifications.5 We compare how longitudinal subgroups (1) express clinically and utilize treatment over time and (2) differ on childhood risk factors. Among fluctuators, we evaluate whether periods of remission/recurrence coincide with level of environmental demands and whether these relations are moderated by age. We expect new distal childhood predictors to emerge using longitudinal subgroups10 and hypothesize that fluctuators experiencing higher demands (across assessments) will be more likely to demonstrate remission periods (between-person effect) due to increased capacity for demanding environments; however, when demands are higher than usual for an individual (within-person effect), occurrence of ADHD will be more likely due to increased cognitive load.11
METHODS
The MTA16 originally compared 14-month pharmacological and behavioral treatments for 579 children (7.0–9.9 years old) with DSM-IV ADHD, combined type. Baseline characteristics are in Supplementary Table 1. The MTA continued for 14 additional years with prospective follow-ups approximately biennially (8 assessments) until 16 years after baseline.17–20
Participants
The current subsample (N = 483; 83.4% of original sample) includes participants with ADHD who had at least 1 follow-up assessment in adulthood (age 18 or older).
Procedures
Assessments were administered to participants and parents at baseline and 2-, 3-, 6-, 8-, 10-, 12-, 14-, and 16- years postbaseline by closely supervised bachelor’s-level staff. Teacher ratings were obtained in childhood and adolescence. For 2.3% of adult assessments, a parent was unavailable and ratings were collected from a nonparental informant (eg, partner and sibling).
Measures
ADHD symptoms. Child and adolescent symptoms were measured using the parent, teacher, and self-reported SNAP.21,22 Adult symptoms were measured using the parent- and self-report Conners Adult ADHD Rating Scale (CAARS).23 Both instruments measure DSM-IV-TR ADHD symptoms rated 0 (not at all) to 3 (very much). Scores of 2–3 on individual DSM-IV-TR symptoms indicated symptom presence.24
Impairment. In childhood and adolescence, impairment was measured using the parent-report Columbia Impairment Scale (CIS), which assesses 13 impairment domains on a 0–4 scale.25,26 In adulthood, the parent- and self-report Impairment Rating Scale (IRS) measured impairment globally and in eleven domains from 0=no problem to 6=extreme problem.27 Supplementary Appendix 1 describes impairment thresholding.
Mental health and substance use disorders. The Diagnostic Interview Schedule for Children (DISC)28 was administered via parent- and self-reports. Self-report began at the 6-year follow-up; the DISC was not administered at the 10-year follow-up. The DISC is a structured interview querying the presence of DSM criteria using screening questions and supplemental probes. Supplementary Appendix 1 lists included disorders. At each assessment, a comorbidity index was calculated by summing the total number of current diagnoses across reporters.10
Service utilization. The Services for Children and Adolescents Parent Interview29 was administered through the 10-year assessment. It assesses between-assessment estimates of daily dose and number of days treated for ADHD medications, as well as psychosocial and educational interventions, including frequency, duration, and type of services. Similar information was collected at 12 through 16 years using the Health Questionnaire, which queried therapy and medication, including doses, duration, and type of services.30
Distal childhood predictors. We used a set of childhood predictors similar to those previously examined in several longitudinal MTA analyses.10,31 These included baseline age, sex, race/ethnicity, parent- and teacher-rated ADHD symptom severity, a biological risk score reflecting pre and perinatal risks,32 a psychosocial risk index,33 parental psychopathology, alcohol use disorder, maternal depression, childhood physical health, childhood mental health, ODD/CD, anxiety and mood disorder diagnoses, dimensionally measured anxiety and depression, negative life events, full scale IQ, continuous performance test scores,34 initial randomized treatment group, response to initial randomized treatment (regardless of treatment group) at 36 months,31 prestudy medication, psychosocial treatment, and educational interventions, extracurricular activities, negative/ineffective parental discipline and positive parenting,35 and number of close friends. See Supplementary Appendix 2 for details about measurement of predictors.
Environmental demands. Based on available information at each assessment, environmental demands were coded at 6 adolescent/adult time points to reflect demands level across responsibilities domains. Points were aggregated for living situation (1=independent and 0= with adult caregivers), financial responsibility (1=full, 0.5=partial, and 0=dependent), employment (1=full work week, 0.5=partial work week, and none=0), and educational enrollment (1=full time student, 0.5=part time student, and 0=none) and has child(ren) (1=yes and 0=no).
Analytic Plan
Per Sibley et al,5 at each time point, participants were classified as fully remitted, partially remitted, or persistent ADHD considering symptom level, impairment, treatment utilization, and other disorders that better explain symptoms/impairments (see Supplementary Appendix 3 for more details). Full remission required symptoms to fall below the full remission threshold (3 symptoms of inattention [IN] and hyperactivity/impulsivity [HI]) according to all informants, absence of clinically significant impairment, and discontinuation of all ADHD intervention for at least a month prior to assessment. For persistent, we utilized a previously validated definition of persistence, which applied the DSM-5 symptom threshold (5 or 6 symptoms of either inattention or hyperactivity/impulsivity, depending on age) using the CAARS (or SNAP) and impairment threshold of “3 or higher” on the IRS (or CIS). Partially remitted cases met criteria for neither persistence nor full remission, typically because they had low symptoms but continued impairment, high symptoms but insufficient impairment, or met symptom and impairment criteria for full remission, but were currently treated. After classifying each participant’s cross-sectional remission status at each assessment, participants were classified into 4 longitudinal subgroups (fluctuating, stable persistence, stable partial remission, recovery; Figure 1).
Aim 1: characterize MTA longitudinal patterns of remission. Within each longitudinal subgroup, we examined rates of study endpoint-defined DSM-5 ADHD symptom persistence vs remission.15 We then calculated the average number of fluctuations, IN and HI symptom peak and trough count, age of first remission (partial or full), proportion of assessments with impairment, proportion of assessments receiving medication, and proportion of assessments receiving psychosocial treatment. General linear models were used to compare longitudinal remission status on each index. Cohen d and relative risk were calculated for continuous and categorical variables, respectively.
Aim 2: relations between childhood variables and longitudinal patterns of remission. For continuous childhood variables, general linear models examined associations between longitudinal remission pattern and each childhood variable. Six planned comparisons (comparing each group to all others) were conducted for each analysis with a significant between-group main effect. For categorical childhood variables, χ2 analyses and planned comparisons were conducted. The Benjamini-Hochberg false discovery rate correction was applied at the omnibus test level within domain (eg, comorbidity) and separately across planned paired comparisons.36 Cohen d and relative risk were calculated as described for Aim 1.
Aim 3: relations between environmental demands and ADHD fluctuations. Within the fluctuating group (n=335), using data from the 6 through 16-year follow-ups, we conducted a multilevel multinomial logistic regression with random intercepts and time-varying ADHD remission status (0=full remission, 1=partial remission, 2=persistent) as the outcome variable. A time-varying grand mean-centered age variable was included in the model as a covariate. We tested the effect of environmental demands on ADHD remission status and disaggregated within-person and between-person effects37,38 by modeling both a between-person environmental demands predictor (centered at the sample mean) and a within-person, time varying environmental demands predictor (centered at each subject’s individual mean across time).39,40 We also included an age×time-varying environmental demands interaction term to examine whether the effect of environmental demands on ADHD remission status varies by the person’s age. For this model, we used all available data from participants, with each participant on average contributing 5.04/6 possible data points (83.5% complete data). In a model with fewer datapoints, we also explored robustness of results to covarying comorbidity (see Supplementary Appendix 4). Analyses were conducted in SPSS 29.0 using the GENLINMIXED procedure and a logit link function.
RESULTS
Characterize MTA Longitudinal Patterns of Remission
The endpoint symptom persistent subgroup previously reported in Hechtman et al15 consisted of the following longitudinal patterns: 0.0% recovery, 4.4% sustained partial remission, 15.5% stable persistence, and 80.1% fluctuating. The endpoint symptom remission subgroup15 consisted of the following longitudinal patterns: 22.0% recovery, 15.7% sustained partial remission, 0.0% stable persistence, and 62.3% fluctuating. Similar proportions of longitudinal fluctuators met criteria for ADHD symptom persistence (56.6%) and remission (43.4%) at MTA endpoint.
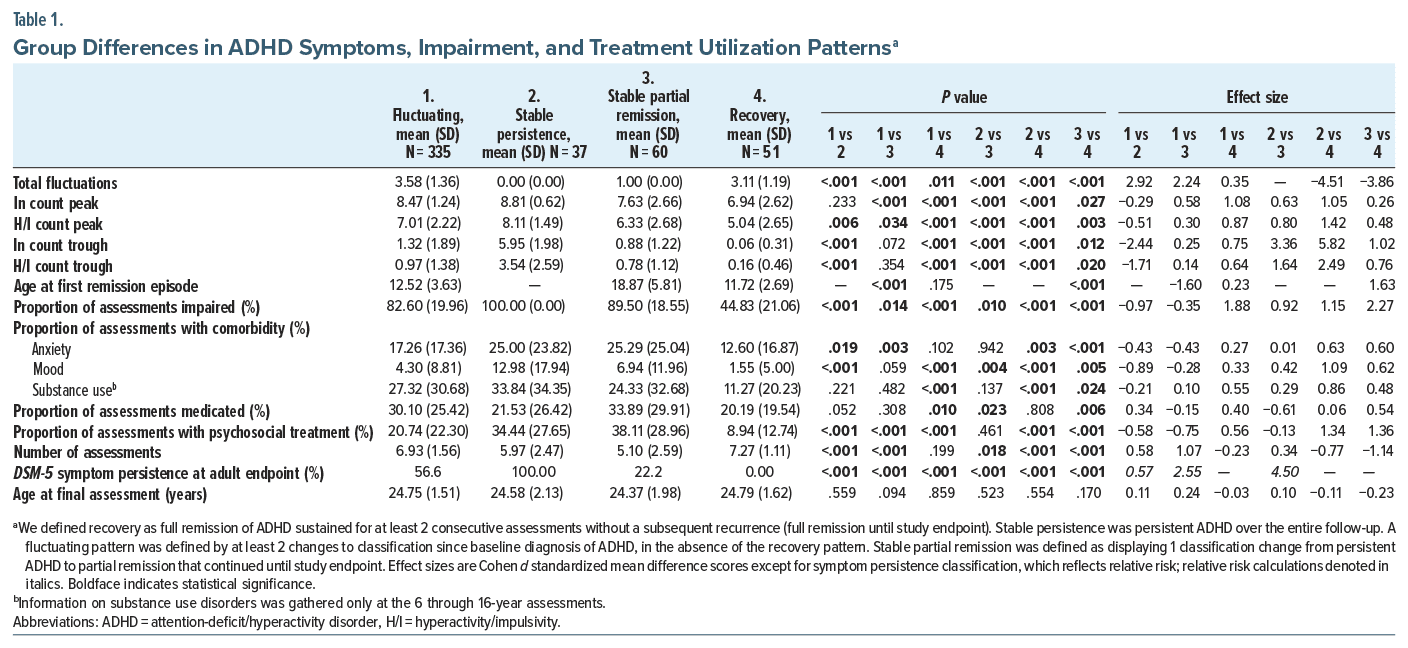
With few exceptions (see Table 1), longitudinal subgroups significantly differed from one another on all clinical variables. Because there were significant differences between groups in terms of number of assessments completed, we conducted sensitivity analyses restricting the sample to only those participants with 6 or more assessment points, which resulted in very minimal changes in the results reported below (see Supplementary Table 4).
The fluctuating group (N = 335; see Table 1) was characterized by the most ADHD classification changes over time (mean = 3.58, SD = 1.36), high ADHD symptom peaks paired with low troughs (∼6–7 symptom difference), average first remission in early adolescence (mean = 12.52, SD = 3.63), relatively stable impairment, and relatively moderate rates of comorbidity/substance use and treatment utilization over time.
The stable persistent group (N = 37) was characterized by no ADHD classification changes, high ADHD symptom peaks and troughs (∼2–4 symptom difference), relatively high and stable impairment, comorbidity, and substance use rates over time, relatively low medication use, and relatively high rates of psychosocial treatment utilization over time.
The stable partial remission group (N = 60) demonstrated one classification change (from ADHD to partially remitted), which occurred in adulthood on average (mean = 18.87, SD = 5.81). They exhibited a relatively high ADHD symptom peak paired with a low trough (∼6–7 symptom difference), relatively high levels of impairment, anxiety disorders, psychosocial treatment, and medication use, and relatively moderate incidence of mood and substance use disorders over time.
The recovery group (N=51) typically demonstrated several classification changes (mean=3.11, SD=1.19) prior to onset of sustained full remission, relatively moderate ADHD symptom peaks and very low symptom troughs (∼5–7 symptom difference), average first period of remission occurring in childhood (mean=11.72, SD=2.69), and relatively low levels of impairment, comorbidity/substance use, and treatment utilization over time.
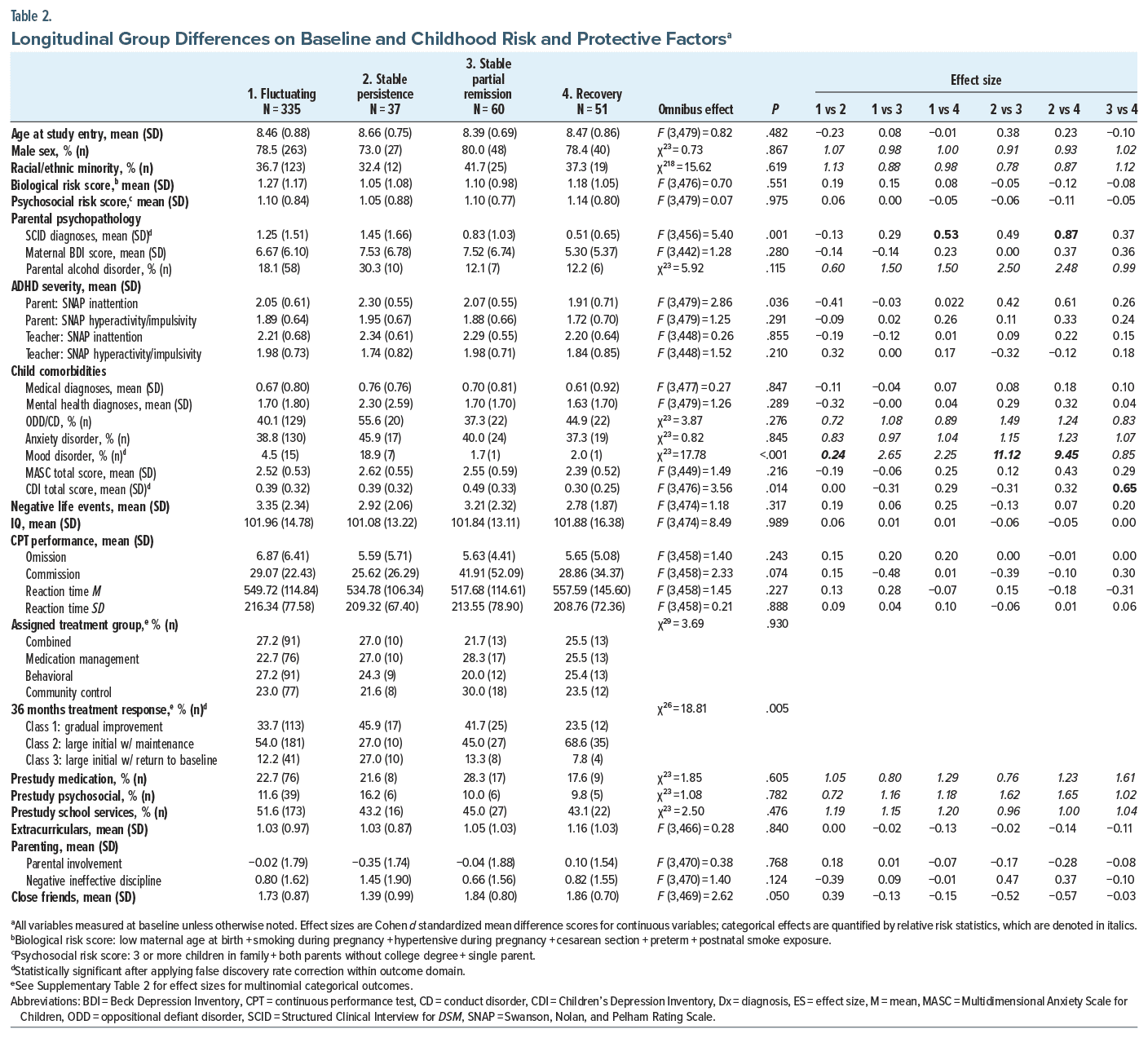
Childhood Predictors of Longitudinal Remission Patterns
See Table 2 for results. After applying the false discovery rate correction, parent SCID diagnoses, childhood mood disorder, childhood depression severity, and 36-month MTA treatment response predicted longitudinal subgroups. The fluctuating and stable persistence subgroups had more parent SCID diagnoses at baseline than the recovery subgroup. The fluctuating, stable remission, and recovery subgroups had lower rates of childhood mood diagnoses than the stable persistence subgroup. The recovery subgroup had lower severity childhood depression scores than the stable partial remission subgroup. For 36-month treatment response classes previously reported by Swanson et al,31 the fluctuating subgroup (and recovery subgroup) had a response pattern that was significantly more favorable than the stable persistent subgroup (see Supplementary Table 2 for details). Sensitivity analyses indicated no changes in significant results using the restricted sample of participants with 6 or more datapoints.
Relation Between Environmental Demands and ADHD Remission Status Within the Fluctuating Group
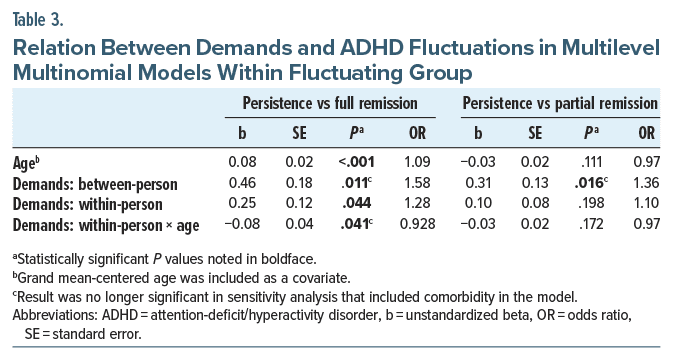
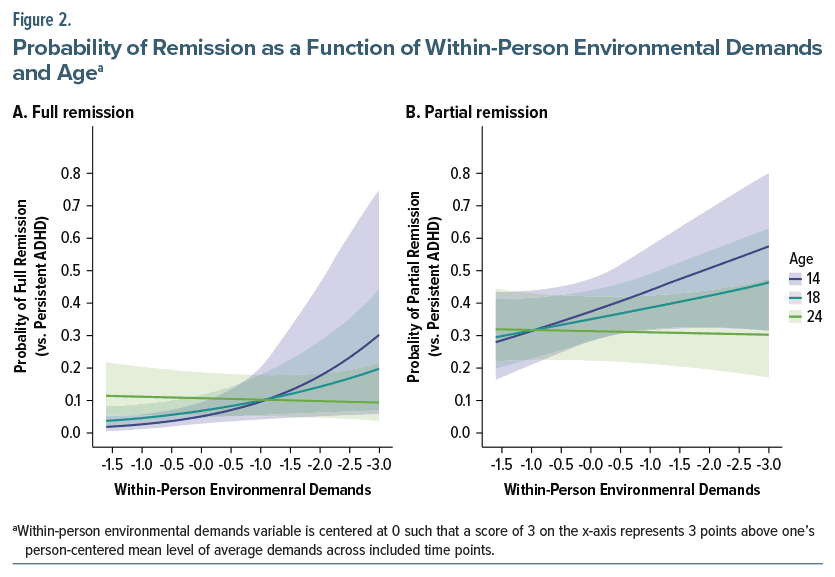
After statistically adjusting for age (see Table 3), significant between-person effects of environmental demands indicated that each added point in an individual’s average environmental demands score across time was associated with a 1.58 higher odds of experiencing a full remission period than a persistent period at any given time point—and a 1.36 higher odds of experiencing a partial remission period than a persistent period. For the full remission vs persistent comparison, there was also a significant within-person effect of environmental demands, indicating that for each point higher an individual scored at any given time point, compared to their own average level of environmental demands, they were 1.28 times more likely to be experiencing an episode of full remission vs an episode of persistence at that time point. A significant interaction between age and within-person environmental demands indicated that the increased odds of full remission that was associated with higher environmental demands was stronger at younger ages than at older ages (see Figure 2). Specifically, as individuals progressed through adulthood, the within-person associations between environmental demands and remission status were less closely related. There was not a significant within-person effect of environmental demands or a significant interaction between within-person environmental demands and age on the likelihood of experiencing a partial remission vs persistent period. Sensitivity analyses (see Supplementary Table 3) indicated that the between-person associations between environmental demands and remission status were not significant in a model including comorbidity as a covariate.
DISCUSSION
This research validates fluctuating ADHD and details its typical clinical characteristics including: 3 to 4 fluctuations over 16 years, 6- to 7-symptom differences between IN and H/I peaks and troughs, first remission periods in early adolescence, and greater stability in impairment level than symptoms. The fluctuating subgroup (63.8% of sample) tended to display moderate clinical severity and childhood risk (compared to other groups); thus, fluctuating ADHD may be the standard and common course of ADHD, in the absence of specific risk or protective factors (at least for those diagnosed as ADHD, combined type, in childhood). Among fluctuators, periods of remission (particularly full remission) were associated with higher environmental demands, particularly at younger ages.
This research confirms prominent instability within the fluctuating group, rebuffs criticisms that fluctuating ADHD is simply an artifact of categorizing a dimensional trait,5 and reveals an artifact within endpoint classification of ADHD persistence (ie, similar proportions of fluctuators were temporarily persisters vs remitters at MTA endpoint). ADHD’s fluctuating nature does not redesignate it as a state-like disorder with transitory episodes (eg, mood disorders). Other polygenic, chronic, trait-like disorders (eg, autism, personality, and schizophrenia) are also known to fluctuate.7
The high prevalence and moderate severity of fluctuating ADHD indicates that it may be the standard clinical course of ADHD—not a rare variant. Stable persistence appears to be a less common variant of ADHD (10.8% of sample) characterized by early and lasting risk for comorbid mood problems, elevated substance use, stable impairments, and low medication utilization relative to severity. The recovery (9.1%) and stable partial remission subgroups (15.6%) may be rare variants marked by milder ADHD and protective factors such as low parental psychopathology or elevated comorbid anxiety (see Table 1 and Table 2). Future work should compare common and rarer ADHD courses on both genetic and time-varying environmental factors. Stable partial remission is particularly intriguing given its positive association with anxiety comorbidity and psychosocial treatment utilization relative to other groups. Although longitudinal course was associated with response to childhood treatment and treatment persistence over time, these associations do not confirm a treatment effect on remission given
well-known bidirectional influences between treatment and ADHD severity in observational designs.30 Future work must disentangle complex relations between past and ongoing treatment and ADHD fluctuations.
Similar to other MTA investigations, we found protective and deleterious roles of internalizing symptoms as well as relations between ADHD persistence and parental psychopathology.10,41,42 These variables warrant continued study and may be important to screen for clinically. Contrary to MTA research on endpoint persistence, we did not find relations with baseline ADHD severity and longitudinal ADHD course.10 Thus, ADHD prognosis may need to reflect a holistic view of the child’s life beyond just symptom level during a single assessment.
Periods of remission were associated with higher between- and within-person environmental demands. Though fluctuations in demands and remission appear to coincide (particularly at younger ages), it remains unclear whether remission promotes entry into more demanding environments or greater demands facilitate symptom/impairment management. Perhaps there is a U-shaped demands-remission curve, bidirectional demands-remission relations, or individual differences in the directionality between these variables. The MTA data may be among the best available to investigate fluctuating ADHD; however, our environmental demands variable is an imperfect index measured at 2-year intervals. Data limitations prevented modeling of finer-grained, more complex statistical relations; nonetheless, establishing concurrent fluctuation of ADHD and environmental context is a critical green light for further exploration. Interestingly, higher within-person demands no longer temporally coincided with remission by the mid 20s (see Figure 2), suggesting a more complex influence of environment on ADHD severity as individuals age. It should be noted that some individuals experiencing high levels of ADHD symptoms paired with low levels of environmental demands may have displayed low impairment levels due to their undemanding context. In this scenario, an individual may have been classified as being partially remitted (rather than persistent) as a function of their low level of demands.
Although the MTA was representative of US demographics at study initiation, it includes fewer girls relative to boys and fewer participants with minoritized ethnic or racial identities relative to white identities, which may limit generalizability. Our multilevel models focused on concurrent fluctuation of remission and demands; future work might investigate timing of remission/recurrence (see Supplementary Appendix 5). Future work might also disentangle the relative contributions of demands levels to ADHD symptom vs impairment levels. Despite the clinical relevance of ADHD fluctuations to late-identified ADHD, long-term symptom monitoring, and expectations for return to care, variations in a trait over time (ie, regression to the mean and homeostatic processes) may be less prognostic than mean trait level. Though we previously documented that informant switching accounts for minimal variance in fluctuations,5 changes in how informants perceive an individual, rather than true behavioral differences, may explain some fluctuations. Clinicians also wrestle with this challenge.
CONCLUSIONS
ADHD fluctuations are common and substantive. This investigation shows that, when temporarily remitted, individuals with fluctuating ADHD can successfully manage increased responsibilities. Much remains unknown about fluctuating ADHD. Future research should investigate treatment optimization based on longitudinal course of ADHD, building datasets with finer-grained, prospective measurement of environmental and endogenous factors hypothesized as relevant to ADHD fluctuations, and patient’s lived experiences of fluctuating ADHD using qualitative methods. These research directions may reveal treatment targets that can help individuals with ADHD detect and manage fluctuations across the lifespan. Clinicians should emphasize that ADHD often fluctuates over time and patient monitoring of symptoms is imperative to trigger as-needed return to care. Clinicians also should partner and collaborate with individuals with ADHD and their families to leverage person-specific environmental factors that appear to positively influence functioning.
Article Information
Published Online: October 16, 2024. https://doi.org/10.4088/JCP.24m15395
© 2024 Physicians Postgraduate Press, Inc.
Submitted: April 19, 2024; accepted August 20, 2024.
To Cite: Sibley MH, Kennedy TM, Swanson JM, et al. Characteristics and predictors of fluctuating attention-deficit/hyperactivity disorder in the Multimodal Treatment of ADHD (MTA) study. J Clin Psychiatry. 2024;85(4):24m15395.
Author Affiliations: Department of Psychiatry & Behavioral Sciences, University of Washington School of Medicine, Seattle Children’s Research Institute, Seattle, Washington (Sibley); Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania (Kennedy); Child Development Center, School of Medicine, University of California, Irvine, Irvine, California (Swanson); Department of Psychiatry and Behavioral Health, Ohio State University, Nisonger Center, Columbus, Ohio (Arnold); The REACH Institute, New York, New York (Jensen); Division of Child Psychiatry, McGill University, Montreal Children’s Hospital, Montreal, Quebec, Canada (Hechtman); Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania (Molina); Department of Psychology, Carleton University, Ottawa, Ontario, Canada (Howard); Department of Psychiatry, University of California, San Francisco, San Francisco, California (Greenhill); Department of Psychology, University of Maryland, College Park, Maryland (Chronis-Tuscano); Department of Psychiatry & Behavioral Sciences, Duke University Medical Center, Durham, North Carolina (Mitchell); Departments of Psychiatry & Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York (Newcorn); ADHD Outpatient Program & Developmental Psychiatry Program, Hospital de Clinicas de Porto Alegre, Federal University of Rio Grande do Sul, Porto Alegre, Brazil (Rohde); Medical Council UniEduK, São Paulo, Brazil (Rohde); National Institute of Developmental Psychiatry & National Center for Innovation and Research in Mental Health, Porto Alegre, Brazil (Rohde); Department of Psychology, University of California, Berkeley, Berkeley, California (Hinshaw); Department of Psychiatry & Behavioral Sciences, University of California, San Francisco, San Francisco, California (Hinshaw).
Corresponding Author: Margaret H. Sibley, PhD, Department of Psychiatry & Behavioral Sciences, University of Washington School of Medicine, Seattle Children’s Research Institute, 1920 Terry Ave, Seattle, WA 98101 ([email protected]).
Relevant Financial Relationships: Dr Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire, and YoungLiving (as well as NIH and Autism Speaks), has consulted with or been on advisory boards for Gowlings, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, Shire, and Tris Pharma, and received travel support from Noven. Dr Chronis-Tuscano receives royalties from Oxford University Press and receives research funding from the National Institutes of Health. Dr Hechtman has received research support from, served on advisory boards for, and been a speaker for Eli Lilly, IronShore, Ortho Janssen, Purdue, and Shire. Dr Hinshaw has received royalties from Oxford University Press, Guilford Press, Wiley, and St. Martin’s Press Dr Jensen receives royalties from American Psychiatric Association Press, Inc, Oxford Press, Random House, and Guilford Press. Dr Rohde has received grant or research support from, served as a consultant to, and served on the speakers’ bureaus of Abdi Ibrahim, Abbott, Aché, Adium, Apsen, Bial, Knight Therapeutics, Medice, Novartis/Sandoz, Pfizer/ Upjohn/Viatris, and Shire/Takeda in the last 3 years. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr Rohde have received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Novartis/Sandoz and Shire/ Takeda. Dr Rohde has received authorship royalties from Oxford Press and ArtMed. Dr Mitchell has received book royalties from Guilford Press, has consulted for Keller Postman and MindFit, and has conducted research sponsored by Lumos Labs over the past 12 months. Dr Sibley receives book royalties from Guilford Press and research support from the National Institute of Health and Institute of Education Sciences. In the past 3 years, she has consulted with Supernus, Tris, and Tiefenbacher. Dr Swanson acknowledges research support, advisory board membership, speakers bureau membership, and/or consulting for Alza, Richwood, Shire, Celgene, Novartis, Celltech, Gliatech, Cephalon, Watson, CIBA, UCB, Janssen, McNeil, and Lilly. Dr Greenhill works as a salaried employee of The Permanente Medical Group. Dr Newcorn was a consultant/advisory board member for Adlon Therapeutics, Cingulate Therapeutics, Corium, Hippo T&C, Ironshore, Lumos, Medice, MindTension, Myriad, NLS, OnDosis, Otsuka, Rhodes, Shire/Takeda, Signant Health, and Supernus; received research support from Adlon, Otsuka, Shire, and Supernus and honoraria for disease state lectures from Otsuka and Shire; and served as a consultant for the US National Football League. The remaining authors have no conflicts to declare.
Funding/Support: The work reported was supported by cooperative agreement grants and contracts from NIMH and the National Institute on Drug Abuse (NIDA) to the following: University of California–Berkeley: U01 MH50461, N01MH12009, and HHSN271200800005-C; DA-8-5550; Duke University: U01 MH50477, N01MH12012, and HHSN271200800009-C; DA-8-5554; University of California–Irvine: U01MH50440, N01MH12011, and HHSN271200800006-C; DA-8-5551; Research Foundation for Mental Hygiene (New York State Psychiatric Institute/Columbia University): U01 MH50467, N01 MH12007, and HHSN271200800007-C; DA-8-5552; Long Island–Jewish Medical Center U01 MH50453; New York University: N01MH 12004, and HHSN271200800004-C; DA-8-5549; University of Pittsburgh: U01 MH50467, N01 MH 12010, and HHSN271200800008-C; DA-8-5553; DA039881; and McGill University N01MH12008, and HHSN271200800003-C; DA-8-5548.
Role of the Funder/Sponsor: The Multimodal Treatment Study of Children with ADHD (MTA) was a National Institute of Mental Health (NIMH) cooperative agreement randomized clinical trial, continued under an NIMH contract as a follow-up study and finally under a National Institute on Drug Abuse (NIDA) contract. These 2 funding agencies were not involved in study design and management of the trial or in the review or approval of this manuscript or other MTA manuscripts. However, under the terms of a federal cooperative agreement, several former NIMH staff were authorized to participate as “cooperating investigators” and to participate in the preparation, analysis, and writing of this and other MTA manuscripts.
Additional Contributions: The multimodal treatment study of children with ADHD (MTA) was a National Institute of Mental Health (NIMH) cooperative agreement randomized clinical trial, continued under an NIMH contract as a follow-up study and finally under a National Institute on Drug Abuse (NIDA) contract. Collaborators from NIMH: Benedetto Vitiello, MD (formerly with the Child & Adolescent Treatment and Preventive Interventions Research Branch); Joanne B. Severe, MS (formerly with the Clinical Trials Operations and Biostatistics Unit, Division of Services and Intervention Research); Peter S. Jensen, MD (formerly with the Office of the Director, NIMH, currently at REACH Institute and the University of Arkansas for Medical Sciences); L. Eugene Arnold, MD, MEd (currently at Ohio State University); and Kimberly Hoagwood, PhD (currently at NYU); previous contributors from NIMH to the early phases: John Richters, PhD (currently at National Institute of Nursing Research) and Donald Vereen, MD (currently at NIDA). Principal investigators and co-investigators from the sites are as follows: University of California, Berkeley/San Francisco: Stephen P. Hinshaw, PhD (Berkeley), Glen R. Elliott, PhD, MD (San Francisco); Duke University: Karen C. Wells, PhD, Jeffery N. Epstein, PhD (currently at Cincinnati Children’s Hospital Medical Center), Desiree W. Murray, PhD; previous Duke contributors to early phases: C. Keith Conners, PhD (deceased; former PI); John March, MD, MPH; University of California, Irvine: James M. Swanson, PhD, Timothy Wigal, PhD; previous contributor from UCLA to the early phases: Dennis P. Cantwell, MD (deceased); New York University: Howard B. Abikoff, PhD; Montreal Children’s Hospital/ McGill University: Lily T. Hechtman, MD; New York State Psychiatric Institute/Columbia University/Mount Sinai Medical Center: Laurence Greenhill, MD (currently at UCSF), Jeffrey H. Newcorn, MD (Mount Sinai School of Medicine). University of Pittsburgh: Brooke S. G. Molina, PhD, Betsy Hoza, PhD (currently at University of Vermont), William E. Pelham, PhD (deceased; PI for early phases, last at Florida International University). Follow-up phase statistical collaborators: Robert D. Gibbons, PhD (University of Illinois, Chicago); Sue Marcus, PhD (Mt. Sinai College of Medicine); Kwan Hur, PhD (University of Illinois, Chicago). Original study statistical and design consultant: Helena C. Kraemer, PhD (Stanford University). Collaborator from the Office of Special Education Programs/US Department of Education: Thomas Hanley, EdD Collaborator from Office of Juvenile Justice and Delinquency Prevention/Department of Justice: Karen Stern, PhD.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Recent studies suggest that attention-deficit/hyperactivity disorder (ADHD) may commonly fluctuate, but predictors of people who fluctuate and periods of fluctuation remain unclear.
- Long-term monitoring of patient ADHD symptoms and impairments is indicated to adjust treatment according to exacerbations and abatements.
- Strategically selecting life environments that promote ADHD management may benefit patients.
References (42)

- Sibley MH, Mitchell JT, Becker SP. Method of adult diagnosis influences estimated persistence of childhood ADHD: a systematic review of longitudinal studies. Lancet Psychiatry. 2016;3(12):1157–1165. PubMed CrossRef
- Ahlberg R, Du Rietz E, Ahnemark E, et al. Real-life instability in ADHD from young to middle adulthood: a nationwide register-based study of social and occupational problems. BMC psychiatry. 2023;23(1):1–8. PubMed
- Grevet EH, Bandeira CE, Vitola ES, et al. The course of attention-deficit/hyperactivity disorder through midlife. Eur Arch Psychiatry Clin Neurosci. 2022;9:1–2.
- Norman LJ, Price J, Ahn K, et al. Longitudinal trajectories of childhood and adolescent attention deficit hyperactivity disorder diagnoses in three cohorts. EClinicalMedicine. 2023;60:102021. PubMed CrossRef
- Sibley MH, Arnold LE, Swanson JM, et al. Variable patterns of remission from ADHD in the Multimodal Treatment Study of ADHD. Am J Psychiatry. 2022;179(2):142–151. PubMed CrossRef
- Van Meter AR, Sibley MH, Vandana P, et al. The stability and persistence of symptoms in childhood-onset ADHD. European Child & Adolescent Psychiatry;2023:1–8.
- Nordgaard J, Nielsen KM, Rasmussen AR, et al. Psychiatric comorbidity: a concept in need of a theory. Psychol Med. 2023;53:5902–5908. PubMed CrossRef
- Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. Guilford Press; 2010.
- Biederman J, Petty CR, Clarke A, et al. Predictors of persistent ADHD: an 11-year follow-up study. J Psychiatr Res. 2011;45(2):150–155. PubMed CrossRef
- Roy A, Hechtman L, Arnold LE, et al. Childhood factors affecting persistence and desistence of attention-deficit/hyperactivity disorder symptoms in adulthood: results from the MTA. J Am Acad Child Adolesc Psychiatry. 2016;55(11):937–944.e4. PubMed CrossRef
- Kofler MJ, Raiker JS, Sarver DE, et al. Is hyperactivity ubiquitous in ADHD or dependent on environmental demands? Evidence from meta-analysis. Clin Psychol Rev. 2016;46:12–24. PubMed CrossRef
- Turgay A, Goodman DW, Asherson P, et al. Lifespan persistence of ADHD: the life transition model and its application. J Clin Psychiatry. 2012;73(2):192–201. PubMed CrossRef
- Lasky AK, Weisner TS, Jensen PS, et al. ADHD in context: young adults’ reports of the impact of occupational environment on the manifestation of ADHD. Soc Sci Med. 2016;161:160–168. PubMed CrossRef
- Meaux JB, Green A, Broussard L. ADHD in the college student: a block in the road. J Psychiatr Ment Health Nurs. 2009;16(3):248–256. PubMed CrossRef
- Hechtman L, Swanson JM, Sibley MH, et al. Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. J Am Acad Child Adolesc Psychiatry. 2016;55(11):945–952.e2. PubMed CrossRef
- MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56(12):1073–1086. PubMed CrossRef
- Jensen PS, Arnold LE, Swanson JM, et al. 3-year follow-up of the NIMH MTA study. J Am Acad Child Adolesc Psychiatry. 2007;46(8):989–1002. PubMed CrossRef
- Molina BSG, Flory K, Hinshaw SP, et al. Delinquent behavior and emerging substance use in the MTA at 36 months: prevalence, course, and treatment effects. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1028–1040. PubMed CrossRef
- Molina BSG, Hinshaw SP, Swanson JM, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500. PubMed CrossRef
- Molina BSG, Hinshaw SP, Arnold LE, et al. Adolescent substance use in the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52(3):250–263. PubMed CrossRef
- Swanson JM. School-based Assessments and Interventions for ADD Students. KC Publications; 1992.
- Swanson JM, Schuck S, Porter MM, et al. Categorical and dimensional definitions and evaluations of symptoms of ADHD: history of the SNAP and the SWAN rating scales. Int J Educ Psychol Assess. 2012;10(1):51–70. PubMed
- Conners CK, Erhardt D, Sparrow E. Conner’s Adult ADHD Rating Scales: CAARS. MHS; 1999.
- Swanson JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40(2):168–179. PubMed CrossRef
- Bird HR, Shaffer D, Fisher P, et al. The Columbia Impairment Scale (CIS): pilot findings on a measure of global impairment for children and adolescents. Int J Meth Psy Res. 1993;3(3):167–176.
- Bird HR, Andrews H, Schwab-Stone M, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. Int J Meth Psy Res. 1996;6(4):295–307.
- Fabiano GA, Pelham WE Jr., Waschbusch DA, et al. A practical measure of impairment: psychometric properties of the Impairment Rating Scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. J Clin Child Adolesc Psychol. 2006;35(4):369–385. PubMed CrossRef
- Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. PubMed CrossRef
- Jensen PS, Hoagwood KE, Roper M, et al. The Services for Children and Adolescents–Parent Interview: development and performance characteristics. J Am Acad Child Adolesc Psychiatry. 2004;43(11):1334–1344. PubMed CrossRef
- Swanson JM, Arnold LE, Molina BSG, et al. Young adult outcomes in the follow-up of the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder: symptom persistence, source discrepancy, and height suppression. J Child Psychol Psychiatry. 2017;58(6):663–678. PubMed CrossRef
- Swanson JM, Hinshaw SP, Arnold LE, et al. Secondary evaluations of MTA 36- month outcomes: propensity score and growth mixture model analyses. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1003–1014. PubMed CrossRef
- Leffa DT, Caye A, Belangero SI, et al. The synergistic effect of genetic and environmental factors in the development of attention-deficit/hyperactivity disorder symptoms in children and adolescents. Dev Psychopathol. 2023;24:1–11.
- Rutter M, Cox A, Tupling C, et al. Attainment and adjustment in two geographical areas: I—the prevalence of psychiatric disorder. Br J Psychiatry. 1975;126(6):493–509. PubMed CrossRef
- Halperin JM, Wolf LE, Pascualvaca DM, et al. Differential assessment of attention and impulsivity in children. J Am Acad Child Adolesc Psychiatry. 1988;27(3):326–329. PubMed CrossRef
- Hinshaw SP, Owens EB, Wells KC, et al. Family processes and treatment outcome in the MTA: negative/ineffective parenting practices in relation to multimodal treatment. J Abnorm Child Psychol. 2000;28(6):555–568. PubMed CrossRef
- Benjamini Y, Hochberg Y. Multiple hypotheses testing with weights. Scand J Statistics. 1997;24(3):407–418.
- Thorndike EL. Measurement of intelligence. Psychol Rev. 1924;31(3):219–252.
- Molenaar PC. A manifesto on psychology as idiographic science: bringing the person back into scientific psychology, this time forever. Measurement. 2004;2(4):201–218.
- Curran PJ, Bauer DJ. The disaggregation of within-person and between person effects in longitudinal models of change. Annu Rev Psychol. 2011;62:583–619. PubMed CrossRef
- Wang LP, Maxwell SE. On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychol Methods. 2015;20(1):63–83. PubMed CrossRef
- Arnold LE, Roy A, Taylor E, et al. Predictive utility of childhood diagnosis of ICD-10 hyperkinetic disorder: adult outcomes in the MTA and effect of comorbidity. Eur Child Adolesc Psychiatry. 2019;28(4):557–570. PubMed CrossRef
- March JS, Swanson JM, Arnold LE, et al. Anxiety as a predictor and outcome variable in the Multimodal Treatment Study of Children with ADHD (MTA). J Abnorm Child Psychol. 2000;28(6):527–541. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!