Depression is one of the most common, debilitating psychiatric disorders, especially for treatment-resistant patients who do not receive an adequate response after 2 or more first-line treatments.1 While electroconvulsive therapy (ECT) has been the gold standard for treatment resistant depression (TRD) for many decades,2 ketamine has recently gained traction among patients and providers as a possible alternative.3
A previous meta-analysis suggested that ECT is likely superior to ketamine for patients in the acute phase4; however, this finding was based on a small number of studies with low sample sizes. Recently, the largest study to date directly compared ECT and intravenous (IV) ketamine.5 To better understand whether ECT or ketamine are better initial treatments for patients with TRD, we re-evaluated our previous meta-analysis with these newer data to determine if ECT or ketamine was associated with better outcomes (ie, improvement in depressive symptoms and response and remission rates).
Methods
We performed an updated systematic review and meta-analysis that compared ECT with IV ketamine.4 The study protocol was registered in PROSPERO database (#CRD42022338045). In this analysis, we included data from a large, newer trial that directly compared ECT to IV ketamine.5 We calculated Hedges g standardized mean differences (SMDs) to determine relative effectiveness of ECT and IV ketamine in treating depressive symptoms as well as on response and remission rates. Detailed methodologic strategies and analytical plans were reported in the earlier study.4
Results
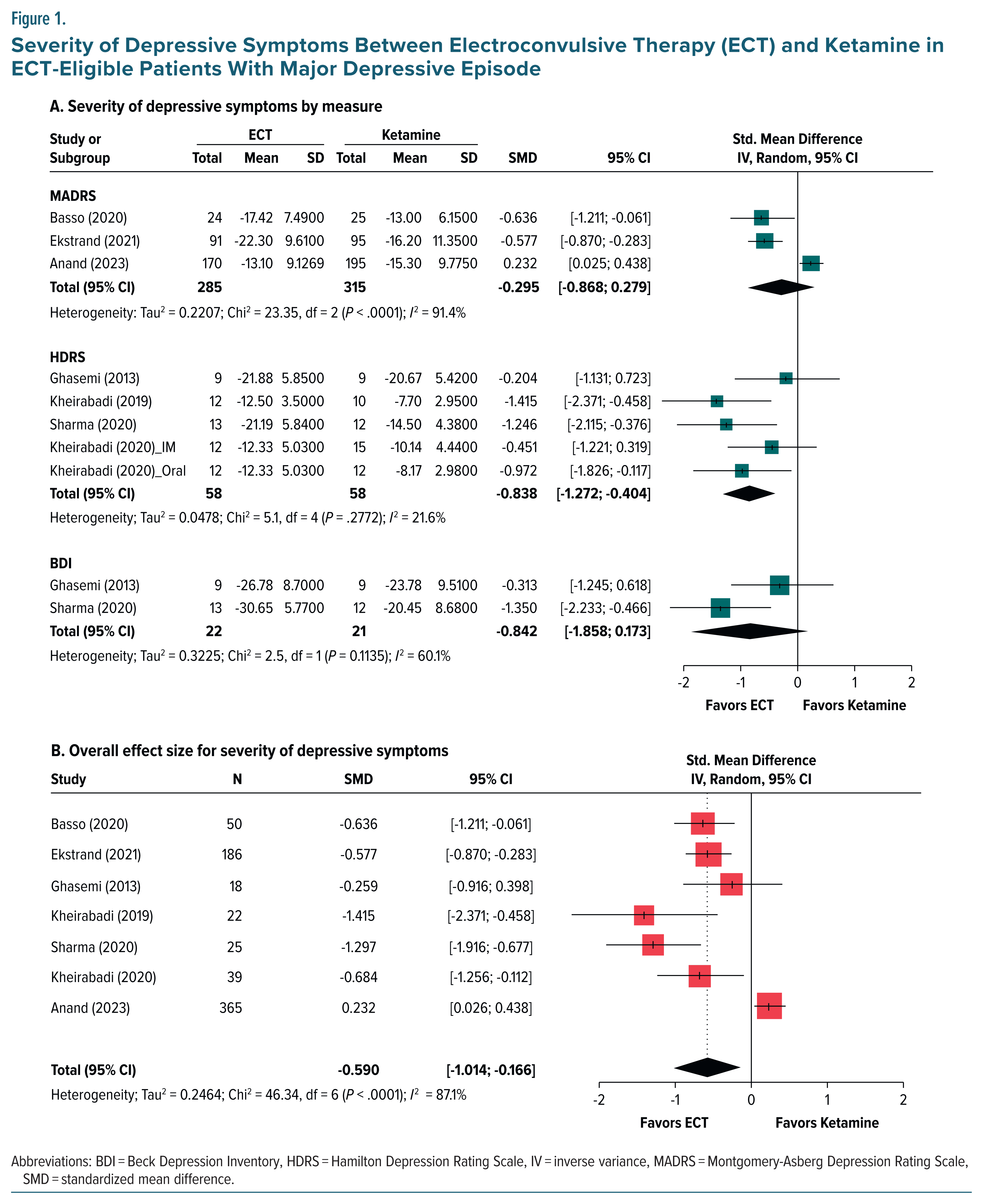
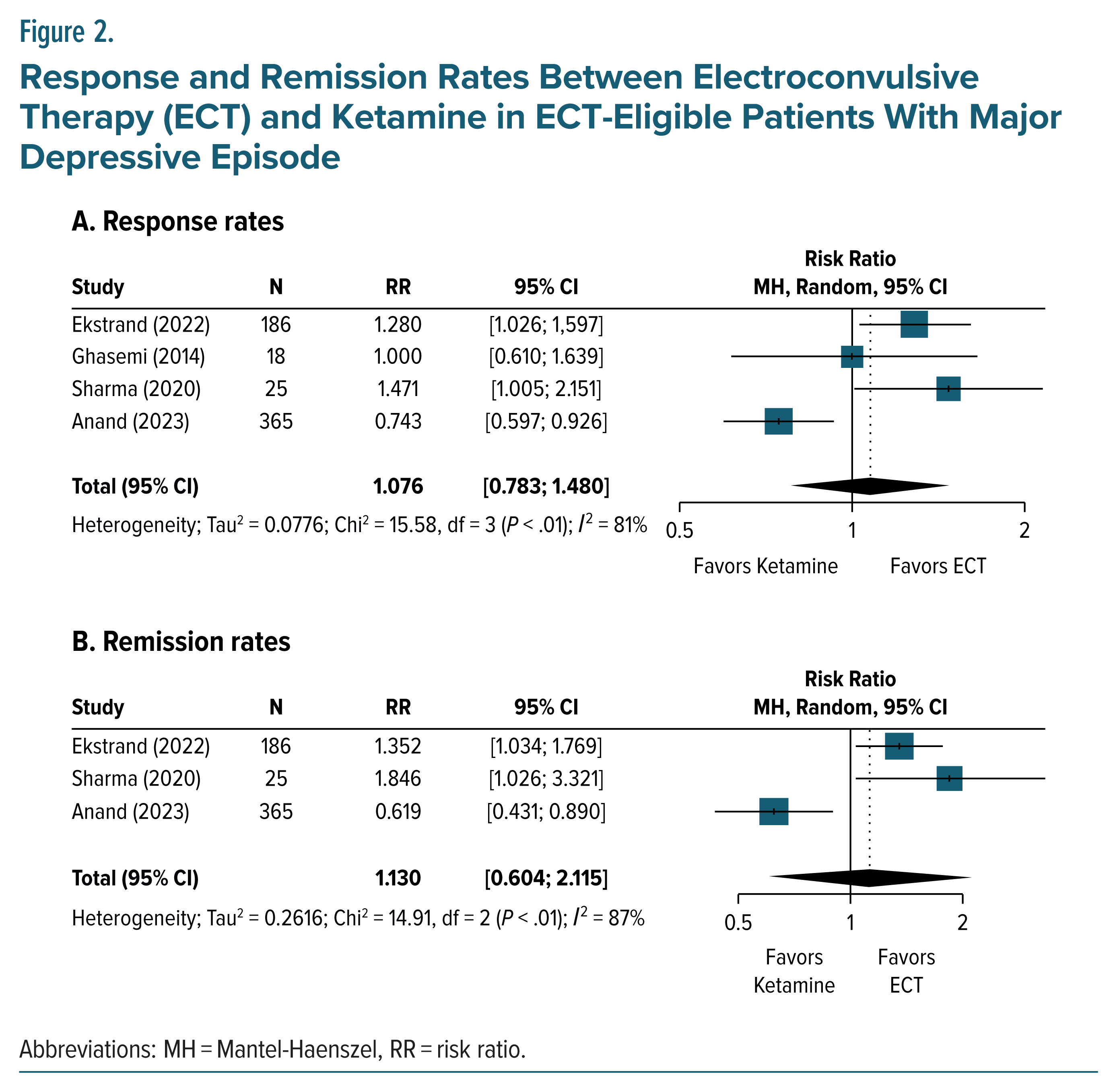
In total, 7 clinical trials comprising 705 patients (n = 332 for ECT and n = 373 for IV ketamine) were included in the meta-analysis.5–11 All of the study participants in these RCTs had severe depression and were eligible for ECT. The overall pooled SMD for depression severity for ECT when compared with ketamine was −0.59 (95% CI, −1.01 to −0.17), suggesting that ECT was more effective than ketamine in treating depression (Figure 1). However, we did not find any statistical differences in response and remission rates between ECT and ketamine (Figure 2).
Discussion
The present meta-analysis includes effect sizes for depression severity as well as response and remission rates from 7 studies that enrolled a total of 705 patients and is the most comprehensive meta-analysis comparing the efficacy of ECT to that of IV ketamine. Our findings are consistent with an earlier study,4 which favored ECT over IV ketamine in treating depression. Of the trials included in this meta-analysis, only 2 are well-powered, head-to-head comparisons.5,6 While the most recent study5 has suggested that ketamine may even be superior to ECT, the trial was not designed nor sufficiently powered to assess this potential outcome.
TRD is associated with increased suicide risk.12–15 Both ECT and ketamine may provide substantial reductions in suicidal ideation for patients with TRD. However, acute increases in suicidality during initial treatment remain a concern, especially for ketamine. Notably, one of the recent large head to-head trials examined suicidality as a secondary outcome via the clinician administered Columbia-Suicide Severity Rating Scale.5 In that study, patients reported a similar decrease in suicide risk when treated with ECT or ketamine. Consistent with this effect, 4 of 195 patients in the ketamine group and 2 of 170 patients in the ECT group reported suicidal ideation, with 1 person in the ketamine group attempting suicide. Similarly, in the other large head-to head trial,6 4 of 95 ketamine patients attempted suicide as did 5 of 91 patients in the ECT group, with 1 ECT patient dying by suicide 3 months after achieving remission during the trial. These data cumulatively suggest that ketamine and ECT carry similar risks in terms of acutely increasing suicidality.
Other differences in study design, setting, and TRD patient characteristics may further challenge direct comparisons on outcomes. Both large studies5,6 enrolled patients with moderate to severe depressive symptoms (ie, Montgomery Asberg Depression Rating Scale [MADRS] >20) who had tried multiple other treatments (including potentially ECT or ketamine) while excluding those who were living with psychotic symptoms. The 2 studies similarly provide the greatest insight to patients with cumbersome, persistent depression with no history of psychoses and may be less valuable to clinicians treating initial presentation of depression.
However, the ketamine-ECT (KetECT) trial6 utilized only hospitalized patients while the ketamine in patients with treatment resistant depression (ELEKT-D) trial5 utilized a predominately outpatient (89%) over inpatient (11%) population. Thus, the noninferiority of ketamine to ECT may also be most useful for clinicians treating major depressive disorder in the outpatient setting. Additionally, the ELEKT-D trial5 only utilized bilateral ECT if response was inadequate halfway through the treatment period to unipolar stimulation, which may decrease the apparent effectiveness of ECT.
Both studies found similar adverse events for both treatments that are consistent with prior clinical trials as well as reports from community practice. For ECT, cognitive impairment and musculoskeletal adverse events were more common than in ketamine treatment, which had higher rates of dissociation. While these disparate adverse events should and will likely inform clinical practice, it is notable that by the end of the primary follow-up phase, both groups returned to similar levels for all measures. For clinicians and patients choosing between treatments, it may be worthwhile to consider if avoiding acute cognitive impairment or dissociation is more desirable when deciding on treatment modality.
Unfortunately, these 2 studies5,6 represent the only well-powered studies to date, pointing to the need for studies comparing ketamine (in different formulations) and ECT (in different applications) across comparable populations and settings. Future trials comparing ECT and ketamine alongside placebo are crucially needed as well as increased follow-up periods to evaluate the long term efficacy of these different treatment modalities. Psychiatric trials, particularly for mood disorders, are dramatically altered by placebo and expectation effects. While ECT has been a mainstay of depression treatment with much bad publicity in the lay media, ketamine has enjoyed a conversely warm welcoming by many patients suffering with depression due in no small part to its popularity as a recreational drug. Such different baseline expectations for potential treatments may additionally make ketamine extremely effective. Understanding patients’ predisposition toward these treatments before randomization would help shed light on such expectancy effects. Increased follow up of patient outcomes for year(s) will also help clinicians guide clinical practice.
Future studies should focus on specific illness characteristics, symptom profiles, longer range outcomes, and patient populations. For example, separating patients based on age is appropriate since studies suggest ECT tends to be more efficacious in older populations than in younger ones. Conversely, younger and more anxious populations may respond better to ketamine than ECT. Lastly, given that ECT requires anesthesia, a natural question is: Does the use of ketamine as an anesthetic during ECT produce synergistic effects? A recent meta-analysis suggests that while ketamine may provide greater antidepressant effect than another common anesthetic (propofol), this effect is tempered by greater cognitive side effects.16 Our study is consistent with the earlier study4 that ECT may be superior to ketamine for improving depression severity in the acute phase. However, we did not find any difference in response or remission rates between these two treatment options. Clearly, studies are needed to better understand the unique applications of ECT and ketamine in the appropriate patient populations, clinical settings, and course of illness.
Article Information
Published Online: January 27, 2025. https://doi.org/10.4088/JCP.24br15655
© 2025 Physicians Postgraduate Press, Inc.
J Clin Psychiatry 2025;86(1):24br15655
Submitted: October 7, 2024; accepted November 19, 2024.
To Cite: Rhee TG, Shim SR, Davoudian PA, et al. Ketamine vs electroconvulsive therapy in the management of treatment-resistant depression: do we need more data? J Clin Psychiatry. 2025;86(1):24br15655.
Author Affiliations: Department of Psychiatry, School of Medicine, Yale University, New Haven, Connecticut (Rhee); Department of Public Health Sciences, School of Medicine, University of Connecticut, Farmington, Connecticut (Rhee); Department of Biomedical Informatics, College of Medicine, Konyang University, Daejeon, Republic of Korea (Shim); Medical Scientist Training Program, School of Medicine, Yale University, New Haven, Connecticut (Davoudian); Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle, Washington (Espinoza); Brain and Cognition Discovery Foundation, Toronto, Ontario, Canada (McIntyre); Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada (McIntyre).
Corresponding Author: Taeho Greg Rhee, PhD, Department of Public Health Sciences, University of Connecticut School of Medicine, 263 Farmington Ave, Farmington, CT 06030 ([email protected]). Rhee and Shim are co-first authors.
Notice of Correction 2/7/25: In Figure 1A (MADRS section only) and Figure 1B, the SD, SMD, and 95% CI values in the Anand, Total, and Heterogeneity rows have been corrected. In the first sentence of the Results, the total and subset numbers of patients have been corrected. To reflect the data corrections, changes have been made to the Results section and the first and last paragraphs of the Discussion to clarify that the findings, consistent with an earlier study, indicate that ECT may be superior to ketamine for improving depression severity in the acute phase, but treatments did not significantly differ in terms of response and remission as outcomes. (See letter of correction: https://dx.doi.org/10.4088/JCP.25lcx15827.)
Author Contributions: Study concept and design: Rhee; data acquisition and statistical analyses: Rhee and Shim; interpretation of data: all authors; drafting of manuscript: Rhee, Davoudian, and Shim; critical revision of manuscript for important intellectual content: all authors; supervision: Rhee. Rhee had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Relevant Financial Relationships: Each author completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and had none directly related to this article. Dr Rhee was supported in part by the National Institute on Aging (NIA) through Yale School of Medicine (#T32AG019134) in the past 3 years. Dr Rhee has also been funded by the NIA (#R21AG070666), National Institute of Mental Health (#R21MH117438) and Institute for Collaboration on Health, Intervention, and Policy (InCHIP) of the University of Connecticut. Dr Rhee serves as a review committee member for Patient Centered Outcomes Research Institute (PCORI) and Substance Abuse and Mental Health Services Administration (SAMHSA) and has received honoraria payments from PCORI and SAMHSA. Dr Rhee has also served as a stakeholder/consultant for PCORI and received consulting fees from PCORI. Mr Davoudian was supported in part by NIH/NIGMS medical scientist training grant T32GM007205 and NIH/NIDA Ruth L. Kirschstein National Research Service Award F30DA059437. Dr McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC) and the Milken Institute; speaker/ consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage,Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra Cellular, NewBridge Pharmaceuticals, Abbvie, Atai Life Sciences. Dr McIntyre is a CEO of Braxia Scientific Corp. Drs Shim and Espinoza report no relevant financial relationships.
Funding/Support: None.
Data Availability Statement: Data are publicly available.
References (16)

- McIntyre RS, Alsuwaidan M, Baune BT, et al. Treatment-resistant depression: definition, prevalence, detection, management, and investigational interventions. World Psychiatry. 2023;22(3):394–412.
- Espinoza RT, Kellner CH. Electroconvulsive therapy. N Engl J Med. 2022;386(7):667–672. PubMed
- Goldberg JF. Electroconvulsive therapy: still the gold standard for highly treatment-resistant mood disorders. CNS Spectr. 2022;27(5):525–526.
- Rhee TG, Shim SR, Forester BP, et al. Efficacy and safety of ketamine vs electroconvulsive therapy among patients with major depressive episode: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79(12):1162–1172.
- Anand A, Mathew SJ, Sanacora G, et al. Ketamine versus ECT for nonpsychotic treatment-resistant major depression. N Engl J Med. 2023;388(25):2315–2325. PubMed
- Ekstrand J, Fattah C, Persson M, et al. Racemic ketamine as an alternative to electroconvulsive therapy for unipolar depression: a randomized, open label, non-inferiority trial (KetECT). Int J Neuropsychopharmacol. 2022;25(5):339–349.
- Basso L, Bönke L, Aust S, et al. Antidepressant and neurocognitive effects of serial ketamine administration versus ECT in depressed patients. J Psychiatr Res. 2020;123:1–8.
- Ghasemi M, Kazemi MH, Yoosefi A, et al. Rapid antidepressant effects of repeated doses of ketamine compared with electroconvulsive therapy in hospitalized patients with major depressive disorder. Psychiatry Res. 2014;215(2):355–361. PubMed
- Kheirabadi G, Vafaie M, Kheirabadi D, et al. Comparative effect of intravenous ketamine and electroconvulsive therapy in major depression: a randomized controlled trial. Adv Biomed Res. 2019;8:25.
- Sharma RK, Kulkarni G, Kumar CN, et al. Antidepressant effects of ketamine and ECT: a pilot comparison. J Affect Disord. 2020;276:260–266. PubMed
- Kheirabadi D, Kheirabadi GR, Mirlohi Z, et al. Comparison of rapid antidepressant and antisuicidal effects of intramuscular ketamine, oral ketamine, and electroconvulsive therapy in patients with major depressive disorder: a pilot study. J Clin Psychopharmacol. 2020;40(6):588–593.
- Rhee TG, Bommersbach TJ, Rosenheck RA, et al. National trends and correlates of treatment resistance in major depressive episode and associated suicidal ideation and behaviors among adults in the United States. J Affect Disord. 2024;358:342–349. PubMed
- Rhee TG, Shim SR, Manning KJ, et al. Neuropsychological assessments of cognitive impairment in major depressive disorder: a systematic review and meta-analysis with meta regression. Psychother Psychosom. 2024;93(1): 8–23.
- Le GH, Wong S, Au H, et al. Association between rumination, suicidal ideation and suicide attempts in persons with depressive and other mood disorders and healthy controls: a systematic review and meta-analysis. J Affect Disord. 2025;368:513–527. PubMed
- Bommersbach TJ, Rosenheck RA, Rhee TG. Rising rates of suicidal behaviors and large unmet treatment needs among US adults with a major depressive episode, 2009 to 2020. Mayo Clin Proc. 2023;98(7):969–984.
- Rhee TG, Shim SR, Popp JH, et al. Efficacy and safety of ketamine-assisted electroconvulsive therapy in major depressive episode: a systematic review and network meta-analysis. Mol Psychiatry. 2024;29(3):750–759.
This PDF is free for all visitors!