Abstract
Objective: Evaluate long-term safety, tolerability, and durability of the effect of olanzapine/samidorphan (OLZ/SAM) for up to 4 years in patients with schizophrenia, schizophreniform disorder, or bipolar I disorder (BD-I).
Methods: This phase 3, multicenter, open-label, long-term extension (conducted June 2017–September 2023) assessed OLZ/SAM in patients completing the ENLIGHTEN clinical program. Patients received ≥2–4 years of additional treatment. Safety assessments included adverse event (AE) incidences and changes from baseline in body weight, waist circumference, and lipid/glycemic parameters. The durability of the effect was assessed using the Clinical Global Impressions–Severity (CGI-S) scale.
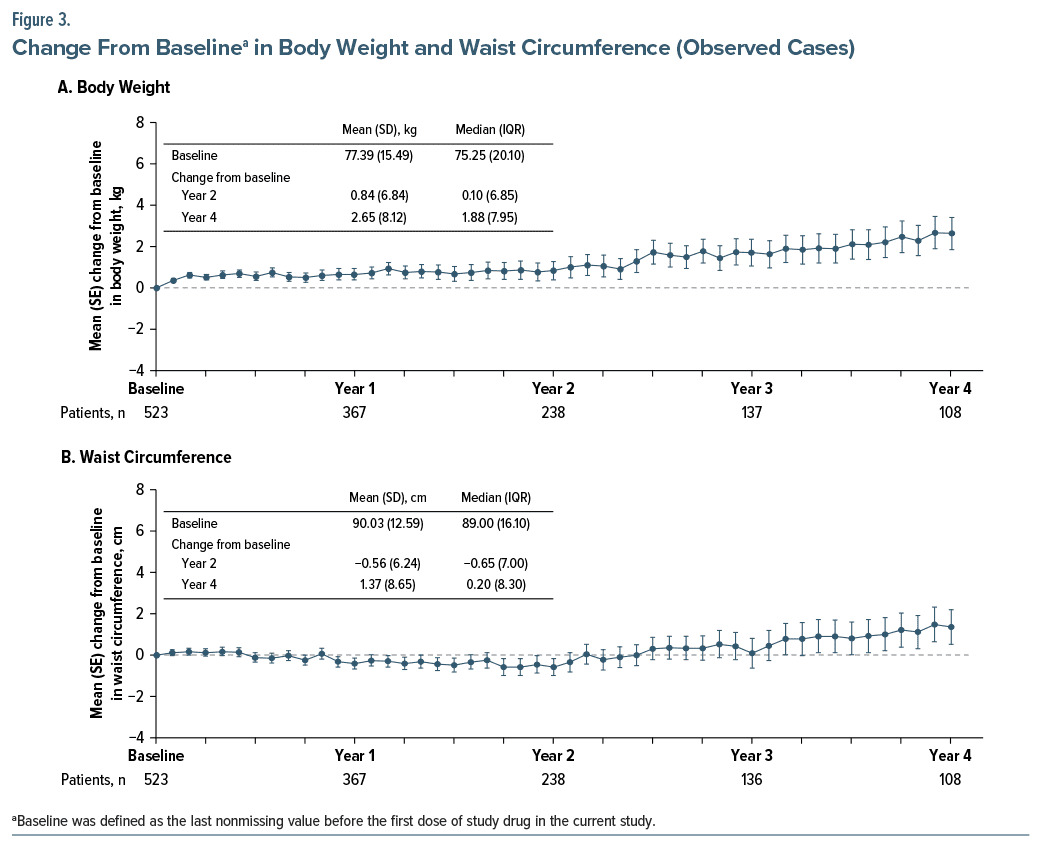
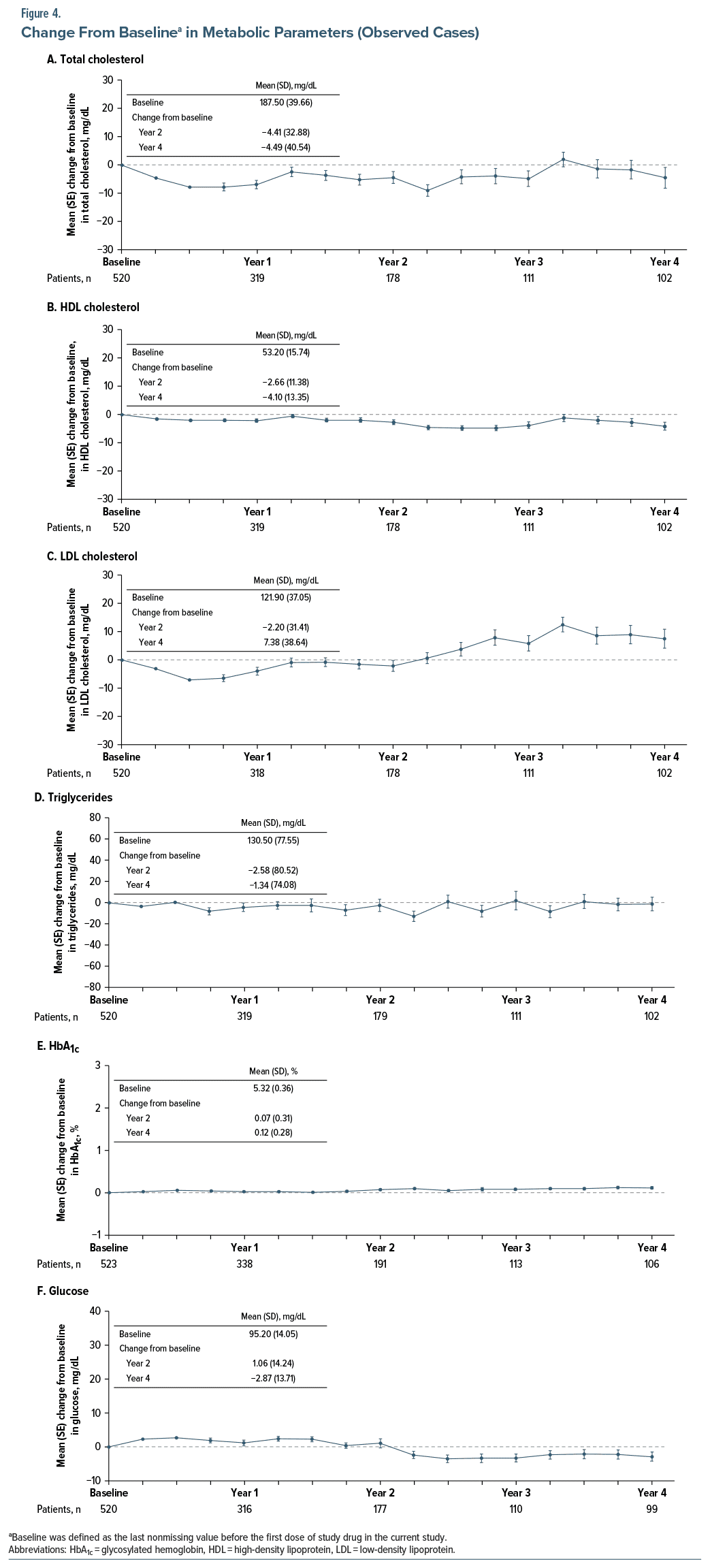
Results: Of 524 patients enrolled, 523 received ≥1 dose of OLZ/SAM. Of these, 460 (88%) patients had schizophrenia, 15 (3%) had schizophreniform disorder, and 48 (9%) had BD-I. Mean (SD) age was 35.1 (12.2) years. Mean (SD) OLZ/SAM exposure was 652.4 (454.8) days. Of 451 patients eligible for 2 years of treatment, 242 (53.7%) received it; of 335 patients eligible for 4 years, 109 (32.5%) received it. The most common AEs were weight increased (9.8%), headache (7.1%), anxiety (6.1%), insomnia (5.9%), somnolence (5.9%), nausea (5.7%), and weight decreased (5.7%). At 2 years, mean (SD) body weight change was 0.84 (6.84) kg; waist circumference change was −0.56 (6.24) cm. At 4 years, mean (SD) body weight change was 2.65 (8.12) kg; waist circumference change was 1.37 (8.65) cm. Changes in lipid/glycemic parameters were minimal. CGI-S scores remained stable.
Conclusion: OLZ/SAM maintained symptom control with a long-term safety profile over 4 years consistent with that of prior studies.
Trials Registration: ClinicalTrials.gov identifier: NCT03201757.
J Clin Psychiatry 2025;86(1):24m15511
Author affiliations are listed at the end of this article.
In this study, we assessed the safety, tolerability, and durability of up to 4 years of treatment with a combination of olanzapine and samidorphan (OLZ/SAM). Patients with schizophrenia, schizophreniform disorder, or bipolar I disorder enrolled after completing 1 of 3 previously conducted phase 3 clinical trials studying OLZ/SAM. During this study, OLZ/SAM was safe and well tolerated. Average changes in weight were small (with some patients gaining weight and others losing weight), average changes in waist size and measures related to cholesterol, triglycerides, and glucose in the bloodstream were minimal, and disease symptoms were stable for up to 4 years. These results highlight the utility of OLZ/SAM for long-term treatment of these conditions.
Antipsychotic medications are recommended treatments for the management of schizophrenia and bipolar I disorder (BD-I)1–4 because they confer several noted benefits, including reducing acute symptoms and lowering the risk of relapse and hospitalization.5–8 Many of these medications, however, are associated with weight gain and metabolic changes that raise safety and tolerability concerns,9–13 especially given that long-term treatment for these conditions is generally required. Olanzapine is among the most efficacious of the atypical antipsychotics used for the treatment of schizophrenia and BD-I, and its use is associated with reductions in relapse rates and hospitalizations.14–17 However, despite olanzapine’s well known benefits, the clinical utility of olanzapine has been limited by its propensity to cause weight gain and adverse cardiometabolic effects such as type 2 diabetes, dyslipidemia, and metabolic syndrome.9,12,18–23
A combination of olanzapine and samidorphan (OLZ/SAM) provides the established antipsychotic efficacy of olanzapine while mitigating olanzapine-associated weight gain.24,25 Based on results from the ENLIGHTEN clinical trial program and related open-label studies (see Supplementary Materials), OLZ/SAM treatment is associated with clinical symptom stability and with significantly less weight gain than with olanzapine monotherapy.24–27 A remaining question, however, was how well OLZ/SAM could provide symptom control and weight gain mitigation over an extended time, consistent with the long-term treatment needs of patients with schizophrenia or BD-I.
The current study represents the culmination of the ENLIGHTEN clinical trial program and builds on those earlier observations. The objective of this study was to evaluate the long-term safety, tolerability, and durability of treatment effect of OLZ/SAM, including characterization of its weight and metabolic profiles in patients with up to 4 years of open-label treatment.
METHODS
This study (ClinicalTrials.gov identifier: NCT03201757) was conducted from June 15, 2017, to September 6, 2023, in accordance with Good Clinical Practice principles (International Conference on Harmonisation, 1997) and ethical principles derived from the Declaration of Helsinki and in accordance with local regulations. The protocol and all amendments were approved by an institutional review board or ethics committee at each study site. All patients provided written informed consent before study entry.
Study Design and Treatments
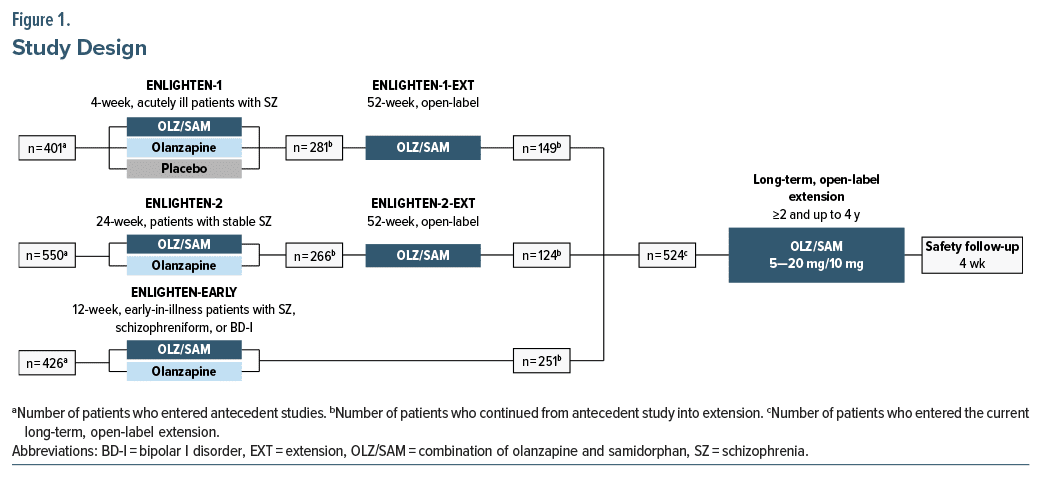
This phase 3, 2- to 4-year (48-month), multicenter, open-label study was conducted at a total of 90 sites: 45 sites within the United States and 45 sites in countries including Austria, Bulgaria, Ireland, Israel, Italy, Poland, Russia, Serbia, South Korea, Ukraine, and the United Kingdom. Eligible patients were enrolled within 7 days of completing 1 of 3 antecedent phase 3 clinical trials investigating OLZ/SAM (Figure 1). Two of the preceding studies26,27 (NCT02669758 and NCT02873208) were 52-week, open-label, rollover extensions of phase 3 pivotal randomized controlled trials in adults with schizophrenia (NCT02634346 and NCT02694328). The third study25 (NCT03187769) was a 12-week randomized controlled trial comparing OLZ/SAM with olanzapine in young adults with recent-onset schizophrenia, schizophreniform disorder, or BD-I.
This study was designed initially with a treatment period of 2 years; however, the protocol was subsequently amended to extend the potential OLZ/SAM treatment duration to 4 years. Maximum treatment duration also varied by patient, as the study end date was scheduled to occur 24 months after the date that the last patient was enrolled. Therefore, the treatment duration for which each patient was eligible depended on their enrollment date relative to that time point. Study visits were scheduled monthly. In some cases, visits were conducted remotely because of the COVID-19 pandemic or the Ukraine-Russia conflict, which disrupted patients’ ability to travel to certain study sites. However, the final visit was required to be in person. The 2- to 4-year treatment period was followed by a 4-week safety follow-up period.
Patients received daily oral OLZ/SAM for up to 4 years. The olanzapine dosage in OLZ/SAM was 5, 10, 15, or 20 mg; the dosage of samidorphan was fixed at 10 mg. Patients started the study taking the same daily oral dose of OLZ/SAM taken in their antecedent study or an OLZ/SAM dose that matched the olanzapine equivalent taken in the antecedent study. Dose adjustments were allowed after the start of the study at the investigator’s discretion.
Patients
All enrolled patients met the eligibility criteria of the OLZ/SAM randomized controlled trial that they had originally entered. The entry criteria for each are reported in detail in the primary publications for those respective trials (ENLIGHTEN-128; ENLIGHTEN-1 extension27; ENLIGHTEN-224; ENLIGHTEN-2 extension26; ENLIGHTEN-Early25) and in Supplementary Materials.
Assessments
The durability of the OLZ/SAM treatment effect was assessed using the change from baseline in the Clinical Global Impression–Severity (CGI-S) scale29 and the time to study discontinuation. Negative scores on the CGI-S indicate clinical symptom improvement.
Safety end points included the incidence and severity of adverse events (AEs) and changes from baseline in body weight and waist circumference, each assessed at monthly visits. Weight and waist circumference were measured at each in-person assessment. Quarterly laboratory evaluations included fasting lipid (high-density lipoprotein [HDL], low density lipoprotein [LDL], total cholesterol, and triglycerides) and glycemic (glucose and glycosylated hemoglobin [HbA1c]) parameters. Fasting status (≥8 hours before blood draw) was based on patient self-report. Additionally, vital signs and electrocardiograms (ECGs) were assessed quarterly. When visits were conducted remotely, data for in-person measures, including weight, waist circumference, and clinical laboratory parameters, were not available.
Statistical Analysis
All analyses were conducted on data from all enrolled patients who received ≥1 dose of OLZ/SAM. For each end point, baseline was defined as the last nonmissing assessment before the first dose of OLZ/SAM in the current study.
All results, including demographics and baseline clinical characteristics, were summarized using descriptive statistics on observed data with no imputation of missing values. Adverse events were coded using Medical Dictionary for Regulatory Activities (Version 26.0) preferred terms; incidence and severity of AEs, serious AEs (SAEs), and AEs leading to study discontinuation were summarized. Changes from baseline in metabolic parameters were summarized by quarterly visit. Changes from baseline in CGI-S scores, body weight, and waist circumference were summarized by monthly visit. Time to discontinuation was estimated using the Kaplan-Meier method.
RESULTS
Patients and Disposition
Of the 524 patients enrolled in the study, 523 received ≥1 dose of OLZ/SAM and were included in the analysis. Overall, 72 patients discontinued the study due to the Ukraine-Russia conflict, leaving a total of 451 patients who were eligible to receive at least 2 years of OLZ/SAM treatment, with 242 (53.7%) reaching that time point. A total of 335 patients were eligible to receive 4 years of treatment, and 109 (32.5%) reached that time point. The most common reasons for discontinuation were withdrawal by patient (25.4%), other (17.6%, including discontinuation due to the Ukraine-Russia conflict), AEs (8.4%), and lost to follow-up (7.1%). The mean (SD) duration of exposure to OLZ/SAM for all patients enrolled in the study was 652.4 (454.8) days (median, 588.0 days).
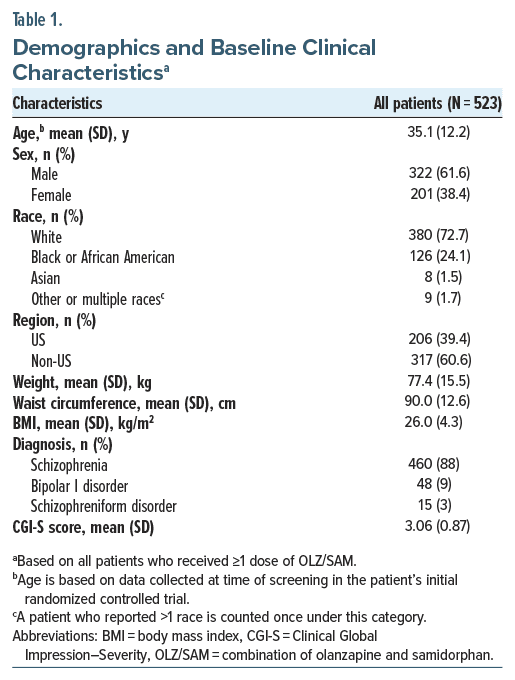
Demographic and baseline characteristics are presented in Table 1. Most patients were male (61.6%) and White (72.7%) and were enrolled predominantly from non-US sites (60.6%). Most patients who were enrolled were diagnosed with schizophrenia (88%) or BD-I (9%). The mean (SD) age at baseline was 35.1 (12.2) years. The mean (SD) baseline weight was 77.4 (15.5) kg (median [interquartile range (IQR)], 75.3 [20.1]), while that of waist circumference was 90.0 (12.6) cm (median [IQR], 89.0 [16.1]). Patients had a mean (SD) body mass index (BMI) of 26.0 (4.3) kg/m2 at study entry, with 1.9% being underweight (BMI <18.5 kg/m2), 44.2% of normal weight (BMI 18.5 to <25 kg/m2), 35.9% overweight (BMI ≥25 to <30 kg/m2), and 18.0% obese (BMI ≥30 kg/m2). Illness severity was mild at baseline, with a mean (SD) CGI-S score of 3.1 (0.9) (median [IQR], 3.0 [1.0]). The mean dose of OLZ/SAM was 14.1/10 mg/d. Overall, 45.3% of patients received a modal OLZ/SAM dose of 20/10 mg, and 29.2% received a modal dose of 10/10 mg.
Durability of Treatment Effect
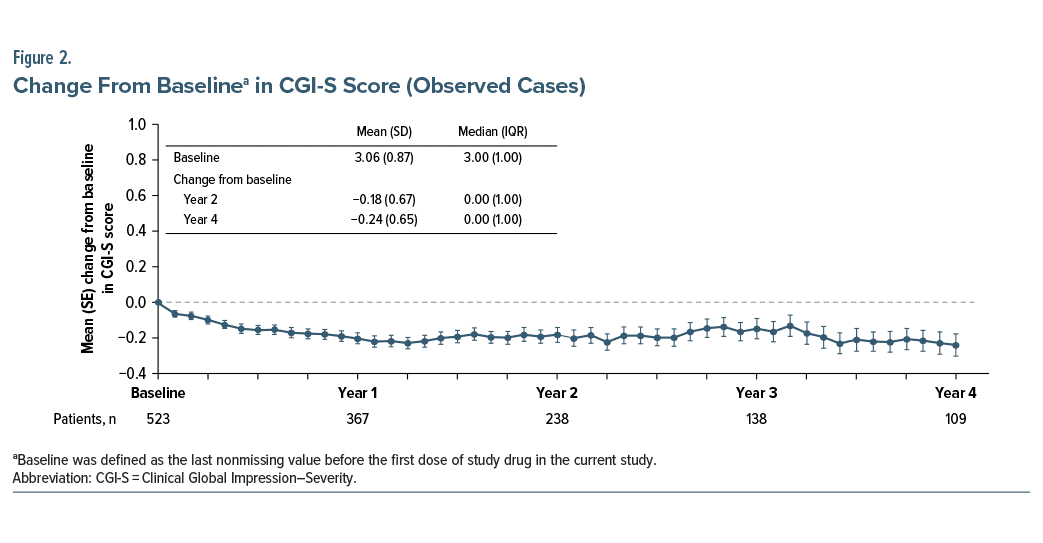
At 2 years, the mean (SD) change from baseline CGI-S score was −0.18 (0.7) (median [IQR], 0.0 [1.0]) and at 4 years was −0.24 (0.7) (median [IQR], 0.0 [1.0]) (Figure 2). The median (95% CI) time to study discontinuation was 588.0 (504.0, 672.0) days.
Safety
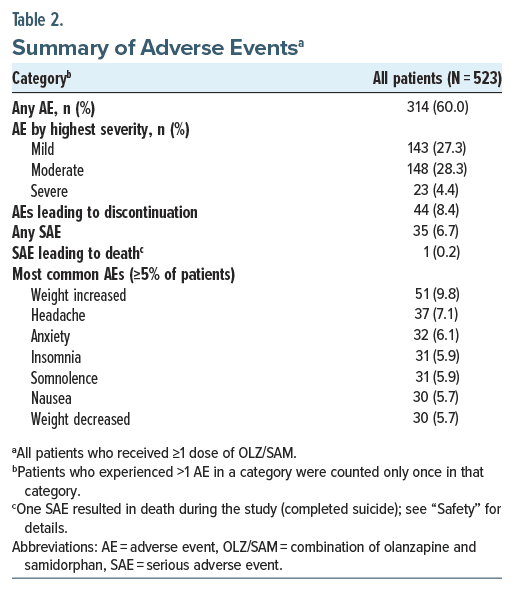
Adverse events. A summary of AEs that occurred in ≥5% of patients is presented in Table 2. Overall, 314/523 (60.0%) patients reported an AE during the treatment period. Most AEs were mild or moderate in severity. The most common AEs were weight increased (9.8%), headache (7.1%), anxiety (6.1%), insomnia (5.9%), somnolence (5.9%), nausea (5.7%), and weight decreased (5.7%). In total, 44 (8.4%) patients discontinued due to an AE. The most common AE leading to discontinuation was increased weight (8 [1.5%]), followed by HbA1c increased (6 [1.1%]) and exacerbation of schizophrenia (6 [1.1%]). Severe AEs were experienced by 23 (4.4%) patients. Except for exacerbation of schizophrenia, which occurred in 2 (0.4%) patients, no other severe AE was reported in >1 (0.2%) patient each.
In total, 35 (6.7%) patients experienced an SAE during the treatment period. The SAEs reported in >1 patient were exacerbation of schizophrenia (11 [2.1%]) and anxiety (2 [0.4%]).
Five (1.0%) patients experienced ≥1 AE involving the potential for suicidal ideation or behavior, including 2 (0.4%) with an AE of suicidal ideation and 1 (0.2%) each with an AE of suicidal depression, suicide attempt, or completed suicide. One patient, a 20-year-old white female with a diagnosis of schizophrenia, died by suicide. The patient missed OLZ/SAM doses for 3 consecutive days before the suicide occurred. The investigator assessed the completed suicide as not related to OLZ/SAM.
Weight change. For patients who contributed data to the 2-year assessment, the observed mean (SD) change in absolute body weight from baseline was 0.84 (6.8) kg (median [IQR], 0.10 [6.9]) kg (Figure 3A); the mean (SD) percent change in body weight was 1.12% (8.6%). The mean (SD) change in waist circumference was −0.56 (6.2) cm (median [IQR], −0.65 [7.0]) cm (Figure 3B). For patients who received 4 years of treatment, the observed mean (SD) change from baseline in body weight was 2.65 (8.1) kg (median [IQR], 1.88 [8.0]) kg (Figure 3A); the mean (SD) percent change in body weight was 3.54% (10.3%). The mean (SD) change in waist circumference was 1.37 (8.7) cm (median [IQR], 0.20 [8.3]) cm (Figure 3B).
Overall, the proportion of patients with a clinically significant weight gain of ≥7% at any time during the study was 32.7% (167/510), whereas the proportion of those withweight loss of ≥7% was 26.9% (137/510).
Lipid and glycemic parameters. Mean changes in lipid and glycemic parameters are shown in Figure 4. At 2 years, the mean (SD) change from baseline in total cholesterol was −4.41 (32.9) mg/dL, in HDL cholesterol was −2.66 (11.4) mg/dL, in LDL cholesterol was −2.20 (31.4) mg/dL, and in triglycerides was −2.58 (80.5) mg/dL. The mean (SD) change in HbA1c was 0.07% (0.3%) at 2 years, while that for fasting glucose concentration was 1.06 (14.2) mg/dL.
At 4 years, the mean (SD) change from baseline in total cholesterol was −4.49 (40.5) mg/dL, in HDL cholesterol was −4.10 (13.4) mg/dL, in LDL cholesterol was 7.38 (38.6) mg/dL, and in triglycerides was −1.34 (74.1) mg/dL. The mean (SD) change from baseline in HbA1c was 0.12% (0.3%) at 4 years, while that for fasting glucose concentration was 2.87 (13.7) mg/dL.
Clinical laboratory parameters and other safety measures. Mean changes in hematology parameters were small and not considered clinically meaningful. In assessments of liver function, no patients met Hy’s Law criteria. No unexpected clinically meaningful changes in vital signs or ECG results were observed.
DISCUSSION
In this open-label extension study, treatment with OLZ/SAM over a period of up to 4 years maintained symptom control in patients with schizophrenia, schizophreniform disorder, or BD-I, with a long-term safety profile that was consistent with that observed in previous studies in the ENLIGHTEN program.24–28 Overall, the majority of AEs were mild or moderate in severity, and SAEs were infrequent. OLZ/SAM was associated with small changes in body weight, minimal changes in waist circumference, and minimal changes in lipid and glycemic parameters. No unexpected clinically meaningful changes in laboratory parameters, vital signs, or ECG results were observed.
Treatment with OLZ/SAM was associated with a durable antipsychotic treatment effect. Approximately half of the patients in the current study enrolled after completing 52 weeks of open-label OLZ/SAM treatment, whereas the other half enrolled after completing 12 weeks of active treatment with either olanzapine or OLZ/SAM. Thus, patients’ clinical symptoms were generally well controlled at entry into the current study and remained so with continued OLZ/SAM treatment.
Importantly, patients stayed on OLZ/SAM for an extended period of time, with a median duration of exposure of 1.6 years. Previous studies have demonstrated longer patient retention on olanzapine compared with other antipsychotics, suggestive of its antipsychotic efficacy.14,30 In Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE), the rate of all-cause discontinuation with olanzapine was 64% over 1.5 years.14 Similarly, in a study of patients with first-episode psychosis, the discontinuation rate with olanzapine was 69% over 3 years.30 The rate of all-cause discontinuation with OLZ/SAM over 4 years in this study was 64%, although the observational period was longer than that of previous studies, thus providing a unique opportunity to assess the clinical benefits of OLZ/SAM treatment as maintenance therapy. Over half of the patients who were eligible for 2 years of treatment reached that time point, and nearly one third of the patients eligible for 4 years of treatment reached that time point, for a total OLZ/SAM exposure (current plus antecedent study) of 5 years or more for some patients. These retention rates are notable given the dual challenges of the COVID-19 pandemic and the Ukraine-Russia conflict that occurred during the study.
The small amount of weight gained and minimal waist circumference changes observed during treatment with OLZ/SAM, at both the 2- and 4-year exposure time points, are important results for both clinicians and patients, given the propensity of olanzapine monotherapy to cause weight gain.14,31,32 Most of the weight gain associated with OLZ/SAM exposure occurred in the antecedent studies (4-week pivotal study, mean +3.02 kg28; 24-week pivotal study, mean +3.18 kg24), with smaller changes at the 2- and 4-year exposure time points in the current study. In an analysis of studies ≥48 weeks long, the mean weight gained on olanzapine was 5.6 kg,33 more than double the amount observed with OLZ/SAM after 4 years in this study. Although there are no available studies in a similar population against which weight gain can be compared, a prospective study was identified that included over 120,000 US adults free of chronic diseases and not obese at baseline.34 In that study, where weight was assessed in 4-year increments between 1986 and 2006, participants gained an average of 1.52 kg (5th–95th percentiles, −1.9 to 5.6 kg) within each 4-year period.34
The minimal changes observed in metabolic parameters were generally consistent with those found in previous studies of OLZ/SAM.24–28 In a post hoc analysis of the 24-week ENLIGHTEN-2 study comparing OLZ/SAM with olanzapine, OLZ/SAM significantly reduced the risk of developing stage 1/2 hypertension by 52%, obesity by 48%, and metabolic syndrome by 45% compared with olanzapine.35 The small changes in lipid and glycemic parameters observed in the current study with OLZ/SAM treatment are encouraging because patients with serious mental illness are already at an increased risk of cardiovascular disease and metabolic abnormalities compared with the general population,3,36,37 and efforts to reduce this risk while still providing effective treatment are central to good clinical management of these serious conditions. These results indicate that OLZ/SAM maintained symptom control while mitigating weight gain and metabolic abnormalities, making OLZ/SAM a suitable long-term treatment option for people living with schizophrenia or BD-I.
Limitations
These results should be interpreted within the context of the study’s limitations. Because the study had an open label design, it did not include a comparator arm, which may limit interpretations of safety and efficacy data. Approximately half of patients discontinued before 2 years and about two-thirds before 4 years; thus, missing data may have affected the results reported here. In addition, patients with a less favorable outcome may have dropped out of their antecedent study, creating the potential for selection bias. Also, patient baseline characteristics in this study may be variable because of differences in the inclusion and exclusion criteria of the 3 antecedent studies. Lastly, fasting status was based solely on self-report and not confirmed.
CONCLUSION
In this open-label extension study lasting up to 4 years, OLZ/SAM treatment was well tolerated with a safety profile consistent with that of previous studies in the ENLIGHTEN clinical program. Despite the disruptions related to the global COVID-19 pandemic and the Ukraine Russia conflict, a significant number of patients remained on long-term treatment with OLZ/SAM. Treatment with OLZ/SAM resulted in small changes in body weight, minimal changes in metabolic parameters, and stability in clinical symptoms over the course of therapy. Overall, these results highlight the long-term safety and clinical benefits of OLZ/SAM for the maintenance treatment of schizophrenia and BD-I.
Article Information
Published Online: December 4, 2024. https://doi.org/10.4088/JCP.24m15511
© 2024 Physicians Postgraduate Press, Inc.
Submitted: July 12, 2024; accepted October 2, 2024.
To Cite: Ballon JS, Kahn RS, Arevalo C, et al. Long-term safety, tolerability, and durability of treatment effect of olanzapine and samidorphan: results of a 4-year open label study. J Clin Psychiatry. 2025;86(1):24m15511.
Author Affiliations: Department of Psychiatry, Stanford University, Stanford, California (Ballon); Department of Psychiatry and Behavioral Health System, Icahn School of Medicine at Mount Sinai, New York, New York (Kahn); Clinical Program Management, Alkermes, Inc, Waltham, Massachusetts (Arevalo); Biostatistics, Alkermes, Inc, Waltham, Massachusetts (Dunbar); Department of Neuroscience, Alkermes Pharma Ireland Ltd, Dublin, Ireland (McDonnell); Department of Psychiatry, Zucker Hillside Hospital, Glen Oaks, New York (Correll); Department of Psychiatry and Molecular Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/ Northwell, Hempstead, New York (Correll); Department of Child and Adolescent Psychiatry, Charité Universitätsmedizin, Berlin, Germany (Correll).
Corresponding Author: David McDonnell, MD, Alkermes Pharma Ireland Limited, Connaught House, 1 Burlington Rd, Dublin D04 C5Y6, Ireland ([email protected]).
Author Contributions: Study concept and design: McDonnell; acquisition of data: Ballon; analysis and interpretation of data, drafting the manuscript, revising the manuscript for intellectual content, and final approval of the completed manuscript: all authors.
Relevant Financial Relationships: Dr Ballon has been a consultant and/or advisor to Alkermes, Corcept, Indivior, Lundbeck, and Teva; has received grant support from Alkermes, Corcept, Janssen, Neurocrine, and Roche; and has received royalties from American Psychiatric Association Publishing. Dr Kahn has served as a consultant for and/or has received grants or speaking fees from Alkermes, Janssen-Cilag, Lundbeck, Merck, Minerva Neuroscience, Otsuka, Roche, Sunovion, and Teva. Drs Arevalo and Dunbar are or were employees of Alkermes, Inc, and may own stock/options in the company. Dr McDonnell is or was an employee of Alkermes Pharma Ireland Ltd and may own stock/options in the company. Dr Correll has been a consultant and/or advisor to or has received honoraria from AbbVie, Acadia, Adcock Ingram, Alkermes, Allergan, Angelini, Aristo, Biogen, Boehringer-Ingelheim, Bristol-Meyers Squibb, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Delpor, Denovo, Gedeon Richter, Hikma, Holmusk, Intra-Cellular Therapies, Jamjoom Pharma, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedinCell, Merck, MindPax, Mitsubishi Tanabe Pharma, MapLight, Mylan, Neumora, Neurocrine, Neurelis, Newron, Noven, Novo Nordisk, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Sage, Seqirus, SK Life Science, Sumitomo Pharma America, Sun Pharma, Sunovion, Supernus, Tabuk, Takeda, Teva, Tolmar, Vertex, and Viatris; has provided expert testimony for Janssen and Otsuka; served on a data safety monitoring board for Compass Pathways, Denovo, Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; has received grant support from Janssen and Takeda; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Küleon Bioscience, LB Pharma, MindPax, and Quantic.
Funding/Support: This study was sponsored by Alkermes, Inc.
Role of the Sponsor: The study sponsor was involved in the design, collection, and analysis of the data. Interpretation of the results was by the authors, and the decision to submit the manuscript for publication was made by the authors.
Previous Presentation: Presented as a poster at Schizophrenia International Research Society 2024; April 3–7, 2024; Florence, Italy. American Psychiatric Association Annual Meeting; May 4–8, 2024; New York, New York. American Society of Clinical Psychopharmacology Annual Meeting; May, 28–31; Miami Beach, Florida. Psych Congress Elevate; May 30–June 2, 2024; Las Vegas, Nevada. American Association of Nurse Practitioners National Conference; June 25–30, 2024; Nashville, Tennessee. Psych Congress; October 29–November 2, 2024; Boston, Massachusetts, and Neuroscience Education Institute Congress; November 7–10, 2024; Colorado Springs, Colorado.
Acknowledgments: Medical writing and editorial support were provided by Omar Cabrera, PhD; Noud van Helmond, MD, PhD; and John H. Simmons, MD, of Peloton Advantage, LLC, an OPEN Health company, and funded by Alkermes, Inc. The authors thank Mark S. Todtenkopf, PhD, of Alkermes, Inc., who assisted in the preparation and proofreading of the manuscript.
ORCID: Jacob Ballon: https://orcid.org/0000-0002-6157-4847; Christoph U. Correll: https://orcid.org/0000-0002-7254-5646
Supplementary Material: Available at Psychiatrist.com
Clinical Points
- In this open-label extension of 523 patients with schizophrenia (n = 460, 88%), schizophreniform disorder (n = 15, 3%), or bipolar I disorder (n = 48, 9%), clinical symptoms remained stable for up to 4 years of olanzapine/ samidorphan (OLZ/SAM) treatment.
- Treatment with OLZ/SAM was associated with small changes in body weight at 2 years (0.84 kg) and 4 years (2.65 kg).
- Changes in lipid/glycemic parameters were minimal.
References (37)

- American Psychiatric Association. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. American Psychiatric Association; 2021.
- Buchanan RW, Kreyenbuhl J, Kelly DL, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):71–93. PubMed CrossRef
- Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. PubMed
- Correll CU, Martin A, Patel C, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia (Heidelb). 2022;8(1):5. PubMed
- Kishimoto T, Robenzadeh A, Leucht C, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr Bull. 2014;40(1):192–213. PubMed CrossRef
- Leucht S, Tardy M, Komossa K, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–2071. PubMed CrossRef
- Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29823 patients with schizophrenia. JAMA Psychiatry. 2017;74(7):686–693. PubMed
- Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17(2):149–160. PubMed CrossRef
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed
- Bak M, Fransen A, Janssen J, et al. Almost all antipsychotics result in weight gain: a meta-analysis. PLoS One. 2014;9(4):e94112. PubMed CrossRef
- Correll CU, Lencz T, Malhotra AK. Antipsychotic drugs and obesity. Trends Mol Med. 2011;17(2):97–107. PubMed CrossRef
- De Hert M, Detraux J, van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2012;8(2):114–126.
- Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. PubMed CrossRef
- Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. PubMed CrossRef
- Taipale H, Mehtälä J, Tanskanen A, et al. Comparative effectiveness of antipsychotic drugs for rehospitalization in schizophrenia—a nationwide study with 20-year follow-up. Schizophr Bull. 2018;44(6):1381–1387. PubMed CrossRef
- Ascher-Svanum H, Zhu B, Faries D, et al. A comparison of olanzapine and risperidone on the risk of psychiatric hospitalization in the naturalistic treatment of patients with schizophrenia. Ann Gen Hosp Psychiatry. 2004;3(1):11. PubMed
- Haro JM, Novick D, Suarez D, et al. Remission and relapse in the outpatient care of schizophrenia: three-year results from the Schizophrenia Outpatient Health Outcomes study. J Clin Psychopharmacol. 2006;26(6):571–578. PubMed CrossRef
- Correll CU, Højlund M, Graham C, et al. Weight gain and metabolic changes in patients with first-episode psychosis or early-phase schizophrenia treated with olanzapine: a meta-analysis. Int J Neuropsychopharmacol. 2023;26(7):451–464. PubMed CrossRef
- Vancampfort D, Stubbs B, Mitchell AJ, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14(3):339–347. PubMed CrossRef
- Vancampfort D, Correll CU, Galling B, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry. 2016;15(2):166–174. PubMed CrossRef
- Kinon BJ, Basson BR, Gilmore JA, et al. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62(2):92–100. PubMed
- Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE ETP study. JAMA Psychiatry. 2014;71(12):1350–1363. PubMed CrossRef
- Correll CU, Detraux J, De Lepeleire J, et al. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015;14(2):119–136. PubMed CrossRef
- Correll CU, Newcomer JW, Silverman B, et al. Effects of olanzapine combined with samidorphan on weight gain in schizophrenia: a 24-week phase 3 study. Am J Psychiatry. 2020;177(12):1168–1178. PubMed CrossRef
- Kahn RS, Kane JM, Correll CU, et al. Olanzapine/samidorphan in young adults with schizophrenia, schizophreniform disorder, or bipolar I disorder who are early in their illness: results of the randomized, controlled ENLIGHTEN-Early study. J Clin Psychiatry. 2023;84(3):22m14674. PubMed CrossRef
- Kahn RS, Silverman BL, DiPetrillo L, et al. A phase 3, multicenter study to assess the 1-year safety and tolerability of a combination of olanzapine and samidorphan in patients with schizophrenia: results from the ENLIGHTEN-2 long-term extension. Schizophr Res. 2021;232:45–53. PubMed CrossRef
- Yagoda S, Graham C, Simmons A, et al. Long-term safety and durability of effect with a combination of olanzapine and samidorphan in patients with schizophrenia: results from a 1-year open-label extension study. CNS Spectr. 2021;26(4):383–392. PubMed CrossRef
- Potkin SG, Kunovac J, Silverman BL, et al. Efficacy and safety of a combination of olanzapine and samidorphan in adult patients with an acute exacerbation of schizophrenia: outcomes from the randomized, phase 3 ENLIGHTEN-1 study. J Clin Psychiatry. 2020;81(2):19m12769. PubMed CrossRef
- Guy W. Clinical Global Impressions. ECDEU Assessment Manual for Psychopharmacology. US Department of Health, Education, and Welfare, National Institute of Mental Health; 1976:217–222.
- Gómez-Revuelta M, Pelayo-Terán JM, Juncal-Ruiz M, et al. Antipsychotic treatment effectiveness in first episode of psychosis: PAFIP 3-year follow-up randomized clinical trials comparing haloperidol, olanzapine, risperidone, aripiprazole, quetiapine, and ziprasidone. Int J Neuropsychopharmacol. 2020;23(4):217–229. PubMed
- Zhang Y, Wang Q, Reynolds GP, et al. Metabolic effects of 7 antipsychotics on patients with schizophrenia: a short-term, randomized, open-label, multicenter, pharmacologic trial. J Clin Psychiatry. 2020;81(3):19m12785. PubMed CrossRef
- Spertus J, Horvitz-Lennon M, Abing H, et al. Risk of weight gain for specific antipsychotic drugs: a meta-analysis. NPJ Schizophr. 2018;4(1):12. PubMed
- Zyprexa [Package Insert]. Eli Lilly and Company; 2021.
- Mozaffarian D, Hao T, Rimm EB, et al. Changes in diet and lifestyle and long term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. PubMed CrossRef
- Correll CU, Stein E, Graham C, et al. Reduction in multiple cardiometabolic risk factors with combined olanzapine/samidorphan compared with olanzapine: post hoc analyses from a 24-week phase 3 study. Schizophr Bull. 2023;49(2):454–463. PubMed CrossRef
- Ignaszewski MJ, Yip A, Fitzpatrick S. Schizophrenia and coronary artery disease. B C Med J. 2015;57(4):154–157.
- Ringen PA, Engh JA, Birkenaes AB, et al. Increased mortality in schizophrenia due to cardiovascular disease: a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. 2014;5:137. PubMed CrossRef
This PDF is free for all visitors!