Abstract
Cannabis is a psychoactive substance the availability and use of which, in various forms, has been liberalized in many countries across the world. Cannabis use, including by women of reproductive age, has become increasingly common, with (in some studies) >5% of women using the substance even during pregnancy to self treat nausea, vomiting, stress, anxiety, depression, insomnia, chronic pain, and other conditions. Women who use cannabis during pregnancy are more likely to have a medical or mental health condition; they are commonly unaware that cannabis is associated with pregnancy related risks. These risks arise from effects of cannabis on cannabinoid receptors in the placenta as well as from cannabis constituents that cross the placenta and act on receptors in the developing fetal brain; other mechanisms may also operate. This article examines recent cohort studies and meta-analyses on specific maternal and neonatal adverse outcomes associated with gestational exposure to cannabis. Maternal cannabis use during pregnancy is associated with small to moderately increased risks of gestational hypertension, gestational weight gain less than as well as greater than guidelines, and placental abruption. Maternal cannabis use during pregnancy is also associated with small to moderately increased risks of preterm birth (<36 weeks, <34 weeks, and <32 weeks), small for gestational age, low birth weight, neonatal intensive care unit admission, and fetal death. The risk of some of these adverse outcomes is greater with greater frequency of cannabis use. These adverse outcomes have been identified even in women who do not use other substances during pregnancy. Other adverse outcomes, such as major congenital malformations and neurodevelopmental disorders, are also reported (but are not discussed in this article). For these and other reasons, many professional bodies across the world are already discouraging women from using cannabis during pregnancy. It is important for pregnant women to be educated about cannabis and pregnancy related risks in a shared decision-making process.
J Clin Psychiatry 2024;85(4):24f15611
Author affiliations are listed at the end of this article.
Cannabis is legally available for recreational use, or has been decriminalized, or is available in medicinal forms in many parts of the world, including Canada, the Netherlands, Belgium, Portugal, Italy, Germany, Malta, Argentina, Peru, Uruguay, Thailand, New Zealand, and Australia, as well as in most of the US states.1,2 Attitudes towards cannabis, liberal in many parts of Europe, are becoming liberal in other parts of the world, as well. For example, using data from the General Social Survey, National Study of Drug Use and Health, and other sources, Felson et al3 showed that most Americans have begun to view cannabis use more favorably, regardless of their gender, education, ethnicity, religious affiliation, religious involvements, and political views.
Although more people consume alcohol than use cannabis, high-frequency cannabis use is becoming more common. In a study of data from the US National Survey on Drug Use and Health, Caulkins4 found that, in 2022, there were more daily and near-daily users of cannabis (17.7 M) than of alcohol (14.7 M).
Data from 543,195 subjects, aged 12 years and above, in the US 2013–2022 National Survey on Drug Use and Health showed that the prevalence of self-reported, past 30 days cannabis use increased from 7.6% to 11.5% between 2013 and 2019, and further increased to 15.1% by 2022; the prevalence among girls and women, which was 5.6% in 2013, rose to 13.0% by 2022.5
The increase in cannabis use by women has become a matter of concern.6 This article therefore examines the use of cannabis by women during their reproductive life span, the use of cannabis during pregnancy, and maternal and neonatal outcomes associated with gestational exposure to cannabis with special focus on 2 recent large population-based retrospective cohort studies.
Cannabis Use in Women and During Pregnancy
Women may use cannabis during pregnancy for pleasure, to address pregnancy-related problems such as nausea and vomiting, and to cope with stress7,8; many of such women appear to be unaware of the pregnancy related risks.9
Cannabis use is becoming frequent in women of reproductive age, including before and during pregnancy.6,10 As an example, in a study of the 2016 Behavioral Risk Factor Surveillance System data from 12 US states, 9.9% of 16,556 women of reproductive age reported current marijuana use.11 Cannabis use is also frequent before conception. For example, in a secondary analysis of data from the Effects of Aspirin in Gestation and Reproduction trial, conducted at 4 clinical centers in the US, 5% of 1,228 women reported cannabis use while trying to conceive.12 Cannabis use is frequent during pregnancy, as well. For example, in a study of 1,147 New Hampshire women in the 2016–2017 Pregnancy Risk Assessment Monitoring System, 5.5% reported use of cannabis during pregnancy, most commonly as an antiemetic.13
Data from a nationally representative sample of women of reproductive age (n = 381,199), drawn from the US National Surveys on Drug Use and Health, showed that the prevalence of cannabis use during the past 30 days rose from 6.8% in 2002–2005 to 10.1% in 2014–2017 and use during pregnancy during these periods rose from 3.2% to 4.5%. Use was highest in the first trimester (5.6%–8.1%), lower in the second trimester (2.7%–3.2%), and lowest in the third trimester (1.8%–2.5%).14 Similar findings were reported by Volkow et al.15
Women of reproductive age who have disabilities, relative to those without disabilities, are less likely to associate weekly cannabis use with risk of harm.16 In the 2015–2019 National Survey on Drug Use and Health, women of reproductive age (n = 76,765) with disabilities were twice as likely to report cannabis use during the past month than those without disabilities (21% vs 11%, respectively).17
Cannabis use was found to be more frequent in pregnant women with mental health conditions such as anxiety disorder, posttraumatic stress disorder, mood disorder, or personality disorder.10 Between 2002 and 2014, liberalization of medical marijuana resulted in an almost 5% increase in marijuana treatment admissions among pregnant women, as well as an increase in alcohol- and cocaine-related treatment admissions.18 In 2018, data from 35 US states showed that 2% of prenatal hospitalizations involved cannabis use disorder.19
These findings urge the study of maternal and offspring outcomes in women who use cannabis during pregnancy.
Reasons for Concern
Cannabis contains >550 chemical compounds, including >100 phytocannabinoids, among which Δ9- tetrahydrocannabinol (THC) and cannabidiol (CBD) are best known.20 It is very likely that at least some if not many of these substances will cross the placental barrier and affect the developing fetus.
Δ9-THC and CBD are already known to cross the placenta; they therefore have the potential to affect the developing fetal brain in which a significant density of cannabinoid receptors is already present by gestation week 19, localized to the same areas that express these receptors in adults.21 Also of concern, cannabinoid receptors are expressed throughout the placenta; through action on these receptors, and perhaps through other mechanisms, Δ9-THC, CBD, and other constituents of cannabis may affect placental development by compromising cell proliferation, angiogenesis, cell migration, and immune gene function.22,23
Cannabis exposure has also been shown to impair vascular development in rat24 and primate25 models, and through these mechanisms may predispose to fetal growth restriction, a consistent adverse outcome observed in human pregnancy studies. Finally, women who use cannabis during pregnancy may also be smoking, drinking, and using other substances,26 and cannabis use during pregnancy has been associated with mental health conditions10,27; smoking, alcohol use, other substance use, mental health disorders, and treatments for mental health disorders have all been associated with adverse gestational outcomes.
Maternal Adverse Outcomes Associated With Cannabis Use During Pregnancy
Young-Wolff et al28 studied 10 maternal adverse outcomes associated with cannabis use during pregnancy using 2011–2019 data from an integrated healthcare delivery system in Northern California. The sample comprised 250,221 women who had undergone 316,722 singleton pregnancies lasting ≥20 weeks. Most women were aged 25–30 (27.7%), 31–35 (35.7%), or >36 (21.1%) years. The sample was 37.4% White, 26.5% Asian/Pacific Islander, 26.3% Hispanic, and 6.3% Black. More than half the sample was overweight (26.3%) or obese (23.2%) before pregnancy. Parity was 0 (40.9%) to 1 (34.9%) in three-quarters of the sample. About 94% of women were judged to have had adequate antenatal care.
Exposure to substances during pregnancy included alcohol (9.3%), nicotine (4.5%), and opioids (7.0%). Mood disorder was present in 11.0% of women, substance use disorder in 3.5%, and other psychiatric disorders in 2.4%. Alcohol, opioid, nicotine, and stimulant exposures were 2–7 times as common in cannabis-exposed relative to unexposed pregnancies; and anxiety, mood, other mental health disorders, and other substance use disorders were about 2–6 times as common in exposed relative to unexposed pregnancies.
All pregnancies had been routinely screened for cannabis exposure at baseline by self-report and by urine THC toxicology testing. Self-report and urine testing identified cannabis use in 2.9% and 5.3% of women, respectively, with an overlap of 1.8%. Overall, 6.3% of women screened positive by one or both methods.
The analyses were adjusted for covariates and confounds that included age, ethnicity, parity, neighborhood deprivation index, prepregnancy body mass index, month of antenatal care initiation, noncannabis substance use, maternal medical and psychiatric comorbidities, and maternal medication use.
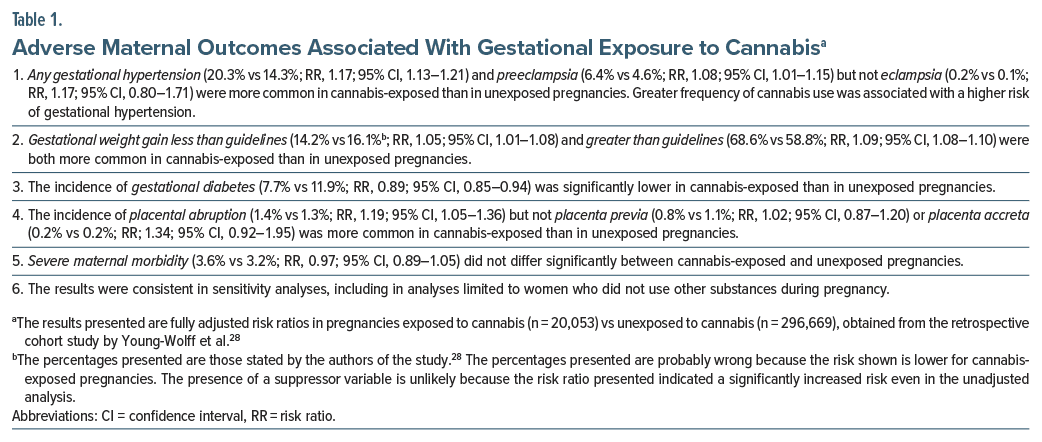
Important findings from the study28 are presented in Table 1. In summary, in fully adjusted analyses, gestational exposure to cannabis was associated with very small but statistically significant increases in the risk of gestational hypertension (including preeclampsia), gestational weight gain less than as well as greater than guidelines, and placental abruption; the risk ratios (RRs) lay in the 1.05–1.19 range. Gestational exposure to cannabis was associated with a small but significantly decreased risk of gestational diabetes (RR, 0.89). Gestational exposure to cannabis was not associated with a significant increase or decrease in the risk of eclampsia, placenta previa, placenta accreta, or severe maternal morbidity. Greater frequency of cannabis use was associated with a higher risk of gestational hypertension.
A specific strength of the study28 was the use of universal screening for cannabis that included urine toxicology testing. An important limitation of the study is that cannabis use was assessed only at weeks 8–9 (median); so, we do not know whether cannabis use continued during pregnancy and, if so, what the outcomes were in women who continued vs discontinued cannabis. For this reason, we also do not obtain an understanding of the effects of cannabis exposure in different trimesters of pregnancy. The most important limitation is that we do not know why the women were using cannabis; because these reasons were not assessed and adjusted for, we cannot understand whether the adverse outcomes were related to cannabis exposure or to the reasons responsible for cannabis exposure.
Neonatal Adverse Outcomes Associated With Cannabis Use During Pregnancy
In a study conducted on much the same sample and by much the same team of authors as in the study described in the previous section,28 Avalos et al29 examined 6 neonatal adverse outcomes associated with cannabis use during pregnancy using 2011–2020 data from the same integrated healthcare delivery system in Northern California. The sample comprised 279,921 women with 364,924 singleton offspring. There were 22,624 pregnancies exposed to cannabis and 342,300 unexposed pregnancies. The study methodology and sample characteristics were closely similar to that of Young-Wolff et al,28 and the details are therefore not repeated here.
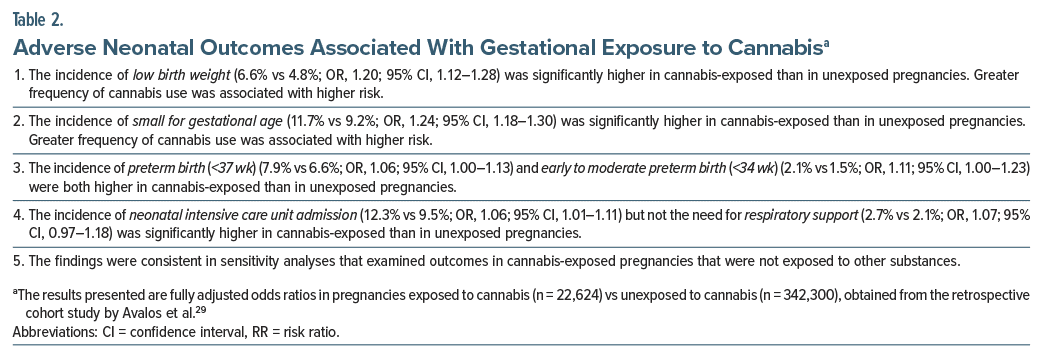
Important findings from the study29 are presented in Table 2. In summary, gestational exposure to cannabis was associated with an increased risk of low birth weight, small for gestational age, preterm birth, early-to moderate preterm birth, and neonatal intensive care unit admission, but not an increased risk of need for respiratory support. The absolute increase in risk was small in all cases, and adjusted odds ratios (ORs) lay in the 1.06–1.24 range. Higher frequency of cannabis use was associated with an increased risk of only low birth weight and small for gestational age. Strengths and limitations of this study are as discussed for Young-Wolff et al28 and as presented in the next section.
Noteworthy Observations
There are many noteworthy observations about the findings of Young-Wolff et al28 and Avalos et al.29 First, gestational exposure to cannabis was associated with an increased risk of 10 of the 16 maternal and neonatal adverse outcomes, but the absolute increase in risk was mostly small, and the effect sizes (RRs and ORs) were also small. This, however, does not detract from the population-level importance of the findings.
Second, dose-dependent associations (increased risk associated with increased frequency of prenatal cannabis use), commonly invoked when considering cause-effect relationships, were identified for only 3 of 16 outcomes: gestational hypertension, low birth weight, and small for gestational age.
Third, fully adjusted values for risk were mostly closely similar to unadjusted values, suggesting either that the findings were truly independent of covariates or that confounders were unidentified and so not adjusted for. The latter is likely because if, for example, insomnia, stress, mild anxiety and depression, chronic pain, lifestyle, and personality characteristics drive cannabis use, then none of these were measured and adjusted for in analyses. Therefore, the analyses cannot provide accurate conclusions about the nature and magnitude of the risk of adverse outcomes associated more specifically with gestational exposure to cannabis.
The above notwithstanding, it is important to note that the adverse maternal and neonatal outcomes were observed even in sensitivity analyses limited to pregnancies unexposed to other substances. These analyses could remove at least some of the sources of confounding referred to above. This suggests, at least, that cannabis, independent of other substance use (and, importantly, independent of the reasons for other substance use), was indeed associated with the adverse outcomes.
Other Studies
Very many other studies examining maternal and neonatal adverse outcomes have also been published; these are too many to review individually. However, 4 recent studies merit attention, and these are briefly summarized.
In the 8-center US Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be,30 610 (6.6%) of 10,038 women recruited during 2010–2013 were detected by urine testing to have used cannabis during pregnancy; 32% had first trimester exposure, and the rest had exposure continued into later pregnancy, as well. The risks of gestational hypertension, small for gestational age, medically indicated preterm birth, and stillbirth were examined as a composite outcome. This study is noteworthy because, in adjusted analysis, only continued cannabis use was significantly associated with the composite outcome (RR, 1.32; 95% CI, 1.09–1.60).
In a single-center Spanish study31 of 134 women with antenatal cannabis use and 12,504 controls, with 111 cannabis users propensity score–matched with 219 control women, small for gestational age (OR, 3.60), low birth weight (OR, 3.94), preterm birth, 37 weeks (OR, 2.07), and preterm birth, 32 weeks (OR, 4.13) were all significantly associated with antenatal cannabis use. In a subgroup analysis of 76 women who discontinued cannabis during pregnancy and who did not use other recreational drugs, risks remained statistically significant for only low birth weight and preterm birth, 37 weeks. This small study is noteworthy for the high values for risk that were closely similar in unadjusted as well as adjusted analyses.
In a retrospective population-based cohort study conducted in California, US,32 there were 23,007 women with a cannabis-related diagnosis and 10,312 women with a cannabis- as well as nicotine-related diagnosis among 3,129,259 pregnant women. A cannabis use diagnosis was associated with an increased risk of preterm delivery (12.2%), small for gestational age (14.3%), neonatal death (0.3%), infant death (0.7%), and severe maternal morbidity (2.3%). These risks were further elevated to 17.5%, 18.0%, 0.6%, 1.2%, and 2.6%, respectively, in women with both cannabis and nicotine use diagnoses. The risks were far lower at 6.6%, 8.5%, 0.2%, 0.3%, and 1.3%, respectively, in control women. This study is noteworthy for its examination of risks associated with combined cannabis nicotine diagnoses as well as for its presentation of offspring mortality and severe maternal morbidity risks.
In a small study of 791 women in the 2009–2013 Stress in Pregnancy longitudinal study, New York, US,33 a noteworthy finding was the markedly increased risk of fetal death (OR, 6.31) associated with gestational exposure to cannabis (n=104) vs no exposure (n=687). In this context, fetal death was defined as a composite of spontaneous abortion, intrauterine death, and stillbirth; separate analyses were not conducted for individual outcomes.
Findings From Meta-Analyses
Earlier studies in the field were summarized in many meta-analyses. By way of example, the findings of 2 recent meta-analyses are presented here.
Baía and Domingues34 described a systematic review and meta-analysis of studies on gestational exposure to cannabis, controlled for smoking and use of illicit drugs. They identified 32 relevant studies (26 cohort studies, 22 studies from the US) that provided data for low birth weight (N = 5,579,127), preterm birth (N = 22,578,522), and small for gestational age (N = 23,432,419) outcomes. Gestational exposure to cannabis was associated with an increased risk of low birth weight (OR, 1.52; 95% CI, 1.18–1.96; 19 studies), preterm birth (OR, 1.39; 95% CI, 1.28–1.51; 27 studies), and small for gestational age (OR, 1.47; 95% CI, 1.38–1.58; 21 studies). Heterogeneity was very high in all analyses. Qualitative assessment suggested that risks were also increased for preterm birth <34 weeks and preterm birth <32 weeks. Heavy cannabis use and continued use during middle and late pregnancy appeared to be associated with higher risks.
Lo et al35 described a systematic review and meta analysis of 53 studies of neonatal outcomes associated with gestational exposure to cannabis. They found that cannabis exposure was associated with an increased risk of preterm birth (OR, 1.42; 95% CI, 1.19–1.69) and small for gestational age (OR, 1.76; 95% CI, 1.52–2.05). Importantly, they also examined perinatal mortality as an outcome and found a significantly increased risk (OR, 1.50; 95% CI, 1.39–1.62). The association between cannabis exposure and absolute birth weight was not statistically significant (mean difference, −40.69 g; 95% CI, −124.22 to 42.83 g). Heterogeneity was high in all analyses except that of perinatal mortality.
Guidelines
Many countries, such as the US36 and Canada,37 have guidelines that strongly discourage the use of cannabis during pregnancy. Trusts in the UK and agencies in Australia and New Zealand have clinical recommendations and patient education materials at their websites that likewise discourage the use of cannabis during pregnancy. There is a need, however, for more concerted efforts to be made, by national bodies, across the world, to develop updated guidelines and to disseminate information about risks so that the general public, and especially women of reproductive age, are more aware of the risks.
The Road Ahead
There are many cannabis use variables that need to be evaluated for association with gestational adverse outcomes. These include the kind of cannabis that is used, the route by which it is used, the dose used per occasion, and the frequency of dosing. Next, the effects of these variables need to be examined after exposure in different trimesters of pregnancy. Importantly, outcomes should be examined in women who continue vs those who stop cannabis use after they discover that they are pregnant. Finally, nausea and vomiting, insomnia, chronic pain, stress, and anxiety and depression are common reasons why women may use or continue cannabis during pregnancy; and some women may use cannabis for reasons related to lifestyle and personality. These are potential confounds that need to be measured and adjusted for in analyses.
Take-Home Message
The use of cannabis is increasing among women of reproductive age and women who are pregnant. This is of concern because, during pregnancy, cannabis use can result in adverse outcomes through its action on cannabinoid receptors in the placenta as well as through its constituents that cross the placenta and act on cannabinoid receptors in the developing fetal brain; other mechanisms are also described. Maternal cannabis use during pregnancy has been associated with small to moderately increased risks of gestational hypertension, gestational weight gain less than as well as greater than guidelines, and placental abruption. Maternal cannabis use during pregnancy has also been associated with small to moderately increased risks of preterm birth (<36 weeks, <34 weeks, and <32 weeks), small for gestational age, low birth weight, neonatal intensive care unit admission, and fetal death. The risk of some of these adverse outcomes is greater with greater frequency of cannabis use. These adverse outcomes have been identified even in women who did not use other substances during pregnancy.
Parting Notes
Gestational exposure to cannabis has been associated with major congenital malformations38,39 and with adverse neurodevelopmental and psychiatric outcomes in offspring.40–42 These will be discussed in later articles.
The literature discussed in this article supports the routine screening of pregnant women for cannabis use in order to better guide pregnancy care. However, routine screening is associated with ethical quandaries in places where cannabis use is criminalized. Finally, Hong et al2 provided a useful discussion on the legal and regulatory aspects of medical cannabis in the US. Although the article is US-centric, it contains much information that could be of interest to readers in other parts of the world.
Article Information
Published Online: October 30, 2024. https://doi.org/10.4088/JCP.24f15611
© 2024 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Maternal cannabis use during pregnancy and maternal and neonatal adverse outcomes. J Clin Psychiatry. 2024;85(4):24f15611.
Author Affiliations: Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India; Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India; Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Financial disclosure and more about Dr Andrade.
References (42)

- Farrelly KN, Wardell JD, Marsden E, et al. The impact of recreational cannabis legalization on cannabis use and associated outcomes: a systematic review. Subst Abuse. 2023;17:11782218231172054. PubMed CrossRef
- Hong G, Sideris A, Waldman S, et al. Legal and regulatory aspects of medical cannabis in the United States. Anesth Analg. 2024;138(1):31–41. PubMed
- Felson J, Adamczyk A, Thomas C. How and why have attitudes about cannabis legalization changed so much? Soc Sci Res. 2019;78:12–27. PubMed CrossRef
- Caulkins JP. Changes in self-reported cannabis use in the United States from 1979 to 2022. Addiction. 2024;119(9):1648–1652. PubMed CrossRef
- Mattingly DT, Richardson MK, Hart JL. Prevalence of and trends in current cannabis use among US youth and adults, 2013-2022. Drug Alcohol Depend Rep. 2024;12:100253. PubMed CrossRef
- Brown QL, Sarvet AL, Shmulewitz D, et al. Trends in marijuana use among pregnant and nonpregnant reproductive-aged women, 2002-2014. JAMA. 2017;317(2):207–209. PubMed
- Vanstone M, Taneja S, Popoola A, et al. Reasons for cannabis use during pregnancy and lactation: a qualitative study. CMAJ. 2021;193(50):E1906–E1914. PubMed CrossRef
- Vanstone M, Panday J, Popoola A, et al. Pregnant people’s perspectives on cannabis use during pregnancy: a systematic review and integrative mixed methods research synthesis. J Midwifery Womens Health. 2022;67(3):354–372. PubMed CrossRef
- Bayrampour H, Zahradnik M, Lisonkova S, et al. Women’s perspectives about cannabis use during pregnancy and the postpartum period: an integrative review. Prev Med. 2019;119:17–23. PubMed CrossRef
- Brown QL, Shmulewitz D, Sarvet AL, et al. Cannabis use, cannabis use disorder and mental health disorders among pregnant and postpartum women in the US: a nationally representative study. Drug Alcohol Depend. 2023;248:109940. PubMed CrossRef
- Ewing AC, Schauer GL, Grant-Lenzy AM, et al. Current marijuana use among women of reproductive age. Drug Alcohol Depend. 2020;214:108161. PubMed CrossRef
- Mumford SL, Flannagan KS, Radoc JG, et al. Cannabis use while trying to conceive: a prospective cohort study evaluating associations with fecundability, live birth and pregnancy loss. Hum Reprod. 2021;36(5):1405–1415. PubMed CrossRef
- Skelton KR, Hecht AA, Benjamin-Neelon SE. Women’s cannabis use before, during, and after pregnancy in New Hampshire. Prev Med Rep. 2020;20:101262. PubMed CrossRef
- Alshaarawy O, Anthony JC. Cannabis use among women of reproductive age in the United States: 2002-2017. Addict Behav. 2019;99:106082. PubMed CrossRef
- Volkow ND, Han B, Compton WM, et al. Self-reported medical and nonmedical cannabis use among pregnant women in the United States. JAMA. 2019;322(2):167–169. PubMed
- Kitsantas P, Aljoudi SM, Sacca L. Perception of risk of harm from cannabis use among women of reproductive age with disabilities. Cannabis Cannabinoid Res. 2024. 10.1089/can.2023.0199 CrossRef
- Kitsantas P, Aljoudi SM, Booth EJ, et al. Marijuana use among women of reproductive age with disabilities. Am J Prev Med. 2021;61(4):554–562. PubMed CrossRef
- Meinhofer A, Witman A, Murphy SM, et al. Medical marijuana laws are associated with increases in substance use treatment admissions by pregnant women. Addiction. 2019;114(9):1593–1601. PubMed CrossRef
- Meinhofer A, Hinde JM, Keyes KM, et al. Association of comorbid behavioral and medical conditions with cannabis use disorder in pregnancy. JAMA Psychiatry. 2022;79(1):50–58. PubMed
- Rock EM, Parker LA. Constituents of Cannabis sativa. Adv Exp Med Biol. 2021;1264:1–13. PubMed
- Mato S, Del Olmo E, Pazos A. Ontogenetic development of cannabinoid receptor expression and signal transduction functionality in the human brain. Eur J Neurosci. 2003;17(9):1747–1754. PubMed CrossRef
- Rokeby ACE, Natale BV, Natale DRC. Cannabinoids and the placenta: receptors, signaling and outcomes. Placenta. 2023;135:51–61. PubMed CrossRef
- Rompala G, Nomura Y, Hurd YL. Maternal cannabis use is associated with suppression of immune gene networks in placenta and increased anxiety phenotypes in offspring. Proc Natl Acad Sci U S A. 2021;118(47):e2106115118. PubMed CrossRef
- Natale BV, Gustin KN, Lee K, et al. Δ9-tetrahydrocannabinol exposure during rat pregnancy leads to symmetrical fetal growth restriction and labyrinth-specific vascular defects in the placenta. Sci Rep. 2020;10(1):544. PubMed CrossRef
- Roberts VHJ, Schabel MC, Boniface ER, et al. Chronic prenatal delta-9- tetrahydrocannabinol exposure adversely impacts placental function and development in a rhesus macaque model. Sci Rep. 2022;12(1):20260. PubMed CrossRef
- Ko JY, Farr SL, Tong VT, et al. Prevalence and patterns of marijuana use among pregnant and nonpregnant women of reproductive age. Am J Obstet Gynecol. 2015;213(2):201.e1–201.e10. PubMed CrossRef
- Young-Wolff KC, Chi FW, Campbell CI, et al. Association of psychiatric and substance use disorders with cannabis use and cannabis use disorder during early pregnancy in northern California. Addiction. 2024. 10.1111/add.16622 CrossRef
- Young-Wolff KC, Adams SR, Alexeeff SE, et al. Prenatal cannabis use and maternal pregnancy outcomes. JAMA Intern Med. 2024;184(9):1083–1093. PubMed CrossRef
- Avalos LA, Adams SR, Alexeeff SE, et al. Neonatal outcomes associated with in utero cannabis exposure: a population-based retrospective cohort study. Am J Obstet Gynecol. 2024;231(1):132.e1–132.e13. PubMed CrossRef
- Metz TD, Allshouse AA, McMillin GA, et al. Cannabis exposure and adverse pregnancy outcomes related to placental function. JAMA. 2023;330(22):2191–2199. PubMed CrossRef
- Brik M, Sandonis M, Hernández-Fleury A, et al. Cannabis exposure during pregnancy and perinatal outcomes: a cohort study. Acta Obstet Gynecol Scand. 2024;103(6):1083–1091. PubMed CrossRef
- Crosland BA, Garg B, Bandoli GE, et al. Risk of adverse neonatal outcomes after combined prenatal cannabis and nicotine exposure. JAMA Netw Open. 2024;7(5):e2410151. PubMed CrossRef
- Habersham LL, Hurd YL, Nomura Y. The longitudinal assessment of prenatal cannabis use on neonatal outcomes. J Perinatol. 2024;44(8):1152–1156. PubMed CrossRef
- Baía I, Domingues RMSM. The effects of cannabis use during pregnancy on low birth weight and preterm birth: a systematic review and meta-analysis. Am J Perinatol. 2024;41(1):17–30. PubMed
- Lo JO, Shaw B, Robalino S, et al. Cannabis use in pregnancy and neonatal outcomes: a systematic review and meta-analysis. Cannabis Cannabinoid Res. 2024;9(2):470–485. PubMed CrossRef
- Committee Opinion No. 722: marijuana use during pregnancy and lactation. Obstet Gynecol. 2017;130(4):e205–e209. PubMed CrossRef
- Graves LE, Robert M, Allen VM, et al. Guideline No. 425b: cannabis use throughout women’s lifespans - Part 2: pregnancy, the postnatal period, and breastfeeding. J Obstet Gynaecol Can. 2022;44(4):436–444.e1. PubMed CrossRef
- Delker E, Hayes S, Kelly AE, et al. Prenatal exposure to cannabis and risk of major structural birth defects: a systematic review and meta-analysis. Obstet Gynecol. 2023;142(2):269–283. PubMed
- Tadesse AW, Ayano G, Dachew BA, et al. The association between prenatal cannabis use and congenital birth defects in offspring: a cumulative meta-analysis. Neurotoxicol Teratol. 2024;102:107340. PubMed CrossRef
- Tadesse AW, Dachew BA, Ayano G, et al. Prenatal cannabis use and the risk of attention deficit hyperactivity disorder and autism spectrum disorder in offspring: a systematic review and meta-analysis. J Psychiatr Res. 2024;171:142–151. PubMed CrossRef
- Sorkhou M, Singla DR, Castle DJ, et al. Birth, cognitive and behavioral effects of intrauterine cannabis exposure in infants and children: a systematic review and meta-analysis. Addiction. 2024;119(3):411–437. PubMed
- Bassalov H, Yakirevich-Amir N, Reuveni I, et al. Prenatal cannabis exposure and the risk for neuropsychiatric anomalies in the offspring: a systematic review and meta analysis. Am J Obstet Gynecol. 2024:S0002-9378–3. 10.1016/j.ajog.2024.06.014 CrossRef
This PDF is free for all visitors!