Abstract
Cannabis use during pregnancy is increasing; the study of adverse outcomes in cannabis-exposed pregnancies is therefore important. Previous articles in this series described increased risks of maternal adverse outcomes, fetal adverse outcomes, birth defects in newborns, and autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) in childhood. This article examines neuropsychiatric adverse outcomes in offspring gestationally exposed to cannabis. Currently available research suggests that prenatal cannabis exposure is associated with increased risks of ASD, ADHD, psychosis proneness, psychotic like experiences, internalizing problems, externalizing problems, attention problems, thought-related problems, social problems, impaired executive function, and observed aggression. There is insufficient study of prenatal cannabis exposure and offspring IQ. Shortcomings in the existing literature are discussed; as examples, many outcomes were determined by screening rather than by formal assessment, prenatal cannabis exposure was ascertained retrospectively in some studies, childhood adverse experiences and exposures were seldom included as covariates, and details about cannabis use (source, potency, frequency, reasons) were unavailable. Curiously, the findings of adverse outcomes were inconsistent, and the effect sizes were small. Possible explanations are that women who use cannabis during pregnancy may not admit it and their pregnancy outcomes may then be misclassified into the control group, assessment of outcomes at too young an age or with insufficient accuracy may blur differences between exposed and unexposed groups, and adjustment for covariates may mask the full effects of cannabis. A last observation is that the studies reviewed were based on exposures that occurred decades ago. Given the increasing potency of currently available cannabis and the limitations of the existing research, it is possible that the available findings underestimate the breadth and severity of the risks. Cannabis is not a necessary substance for use during pregnancy, and so women who consider it safe might do well to guard against complacency and unnecessary exposure.
With liberalization in regulations regarding cannabis and in attitudes towards its use, the use of cannabidiol, medicinal cannabis, cannabis extracts, and cannabis, itself, has increased across the world, including by women of childbearing age and during critical periods such as pregnancy. Earlier articles in this series examined the epidemiology of cannabis use in different populations, possible actions of cannabis constituents on the placenta and on the developing fetus, and the associated risks of different adverse outcomes associated with gestational exposure to cannabis. The outcomes considered included maternal adverse outcomes, fetal adverse outcomes, birth defects in newborns, and autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) in childhood.1–3 The present article summarizes the findings of a recent meta-analysis, as well as findings from a sample of articles not included in the meta-analysis, on gestational exposure to cannabis and the risk of adverse outcomes during childhood and early adult life. The present article also provides a critical perspective of the field as a whole.
Meta-Analysis: Gestational Exposure to Cannabis and Neuropsychiatric Disorders in Offspring
Bassalov et al4 described a systematic review and meta-analysis of the risk of neuropsychiatric disorders in children and young adults who had been gestationally exposed to cannabis. These authors searched 3 electronic databases and reference lists and identified 17 relevant observational studies (pooled N =534,445) representing 14 cohorts. In almost all studies, cannabis use during pregnancy had been based on maternal self-report (only 3 studies had included maternal urine screens).
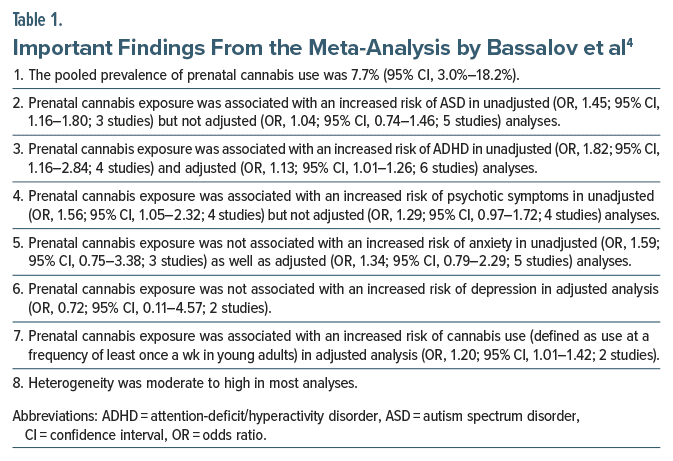
Important findings from the meta-analysis are presented in Table 1. In summary, the pooled prevalence of prenatal cannabis use was 7.7%. Prenatal cannabis exposure was associated with an increased risk of ADHD (unadjusted as well as adjusted analyses) as well as ASD and psychotic symptoms (unadjusted analyses, only). Prenatal cannabis exposure was also associated with an increased risk of cannabis use in offspring who had reached young adult life. Prenatal cannabis exposure was not associated with an increased risk of anxiety or depression in children.
The meta-analysis had many unavoidable limitations. In 10 of the studies the number of exposed pregnancies was <100 and only in 1 study was the number of exposed pregnancies >300. Most of the forest plots pooled just 3–4 studies; 2 forest plots pooled only 2 studies; and the largest forest plot had just 6 studies. Most studies assessed outcomes through self-report or screening rather than through formal diagnostic procedures. In most studies, assessments may have been conducted at too young an age; this was perhaps particularly relevant in the analysis of psychotic symptoms. Finally, most studies did not adjust for influential postnatal covariates and confounds, including childhood adversities.
An avoidable limitation was that in one forest plot (the ASD analysis), data from cohort and case-control studies were combined; this practice is discouraged.2
Prenatal Cannabis Exposure and Psychosis Proneness in Children
Cannabis exposure may be causally associated with an increased risk of schizophrenia spectrum disorders in young adults.5 In their meta-analysis of 4 studies, Bassalov et al4 found that, in an unadjusted analysis, prenatal cannabis exposure was associated with an increased risk of psychotic symptoms in children; the finding narrowly missed statistical significance in the adjusted analysis (Table 1). Given that psychosis more usually arises during young adult life, might psychosis proneness be a more appropriate target for study in children? In this context, Fine et al6 examined whether prenatal exposure to cannabis was associated with an increased risk of psychosis proneness in children.
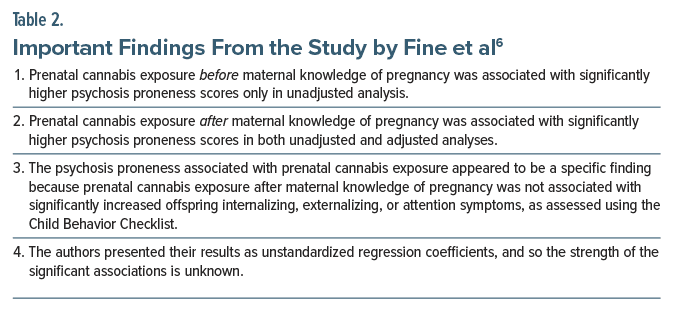
These authors6 studied 4,361 children from the ongoing Adolescent Brain Cognitive Development (ABCD) longitudinal study in the US. The mean age of the sample was 10.0 years. The sample was 52.7% male. Among these children, retrospectively ascertained maternal self report identified 201 (4.6%) to have been gestationally exposed to cannabis. There were 138 children with exposure only before maternal knowledge of pregnancy, 2 with exposure only after maternal knowledge of pregnancy, and 61 with exposure both before and after the mothers knew that they were pregnant. Psychosis proneness was assessed using the Prodromal Questionnaire–Brief Child Version.
Important findings from the study are presented in Table 2. These findings can be interpreted in different ways. One possibility is that women who use cannabis even after they know that they are pregnant may carry risk factors that predispose them to have children with psychosis proneness; that is, cannabis use after discovery of pregnancy may merely be a behavioral marker for the presence of such risk factors. Another possibility is that cannabis use after discovery of pregnancy may occur at a time when the endocannabinoid system is developing in the fetal brain, and when the fetal brain is therefore vulnerable to perturbation by exposure to exogenous cannabinoids. In the absence of clarity, women might prefer to avoid cannabis use especially after discovery of pregnancy.
Prenatal Cannabis Exposure and Neuropsychiatric Outcomes in Children
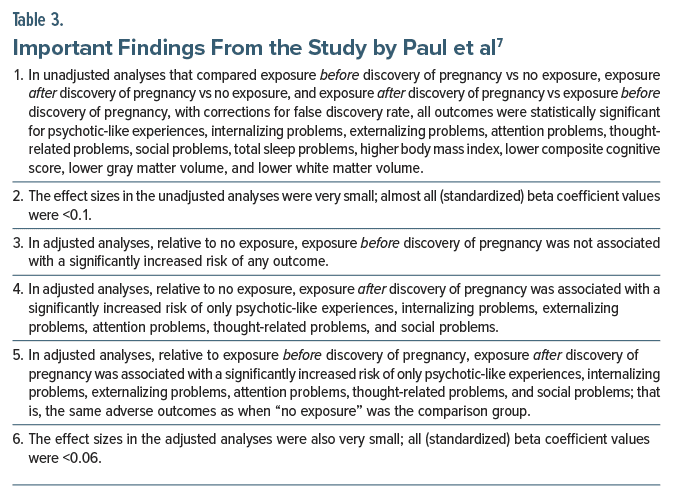
Paul et al7 examined gestational exposure to cannabis and its association with a range of neuropsychiatric outcomes in children. The sample comprised 11,489 children from the ABCD study referred to in the previous section. The mean age of the sample was 9.9 years. The sample was 52.2% male. Among these children, parental self-report identified 655 (5.7%) to have been gestationally exposed to cannabis; 413 children had been exposed only before discovery of pregnancy, and 242 had been exposed after discovery of pregnancy (and possibly before discovery of pregnancy, as well). There were 10,834 children with no exposure. Discovery of pregnancy occurred at a mean of 6.9 weeks. Analyses were adjusted for a range of maternal and pregnancy variables, recorded at baseline.
Important findings from the study7 are presented in Table 3. In summary, gestational exposure to cannabis after discovery of pregnancy was associated with higher risks of many adverse neuropsychiatric findings in children, relative to no gestational exposure as well as relative to gestational exposure before discovery of pregnancy; effect sizes, however, were very small. The implications are similar to those discussed with regard to the study by Fine et al,6 presented in the previous section.
A note in passing: Paul et al7 examined a larger sample of children from the ABCD study than that examined by Fine et al.6 The specificity for psychosis proneness reported by Fine et al6 was not paralleled by specificity for psychotic-like experiences in the study by Paul et al7 although the mean age of the samples in the 2 studies was almost exactly the same.
Baranger et al8 followed children in this cohort to a mean age of 12.0 years. The findings remained much the same, suggesting that gestational exposure to cannabis after discovery of pregnancy is associated with persistent psychopathological effects.
Prenatal Exposure to Cannabis and Other Childhood Outcomes
In a small prospective cohort study of 250 children of whom as many as 80 (32%) had been exposed to cannabis during pregnancy, Keim et al9 found that, at age approximately 5 years, cannabis exposure was associated with poorer attention, poorer inhibitory control, poorer task-based planning ability, and greater observed aggression. No differences were found between exposed and unexposed children for other caregiver and laboratory assessments of executive functioning and behavior. Most of the children in this cohort were non-White and belonged to impoverished families, and 22%–39% of the mothers had used tobacco, alcohol, and other substances during the index pregnancy. In this sample, therefore, it is unknown to what extent the cannabis-related findings were driven by adversities as confounds.
In a retrospectively ascertained cohort of 119,976 children among whom 6,778 (5.6%) had been gestationally exposed to cannabis, exposure was not associated with an increased risk of motor delay, global delay, or speech and language disorders.10 An important limitation of this study is that outcomes were ascertained from healthcare records and at too early an age (medians, 29 months in the exposed sample and 39 months in the unexposed sample) for delays to be reliably identified.
General Summary
Gestational exposure to cannabis is associated with an increased risk of many neuropsychiatric adverse outcomes in childhood. These outcomes include ASD, ADHD, psychosis proneness, psychotic-like experiences, internalizing problems, externalizing problems, attention problems, thought-related problems, social problems, impaired executive function, and observed aggression. However, the findings are inconsistent and the effect sizes are small. There is a paucity of research on prenatal cannabis exposure and IQ in offspring.
Common Limitations of Studies in the Field
Many studies in the Bassalov et al4 meta-analysis established diagnoses by screening rather than by formal assessment of children. In the ABCD cohort studies,6–8 the classification of cannabis exposure was based on an approximately 10-year retrospective recall. Such recall is prima facie unreliable, and is also vulnerable to a retrospective falsification bias arising from lived experiences with the child.
Only a few studies included data on the frequency of use of cannabis during pregnancy. Almost no study included data on the nature and source of the cannabis, the potency of the preparation, the route of administration, the reason for use, and related covariates and confounds, all of which could influence outcomes.
Childhood psychopathology is not driven only by genetic characteristics and gestational exposures. It is also driven by a wide range of postnatal adverse experiences and exposures. Very few studies considered such postnatal experiences and exposures. This is problematic but is hardly surprising, given that postrandomization biases in randomized controlled trials are also seldom addressed in analyses.
The Effect Size Puzzle
Cannabis is not a food to which humans might have adapted during evolution despite exposure during pregnancy. Cannabis is a substance with >550 constituents, many of which act on the placenta or cross the placental barrier.1 Gestational exposure to cannabis could therefore be expected to be associated with many maternal, fetal, neonatal, and early childhood adverse outcomes, as, indeed, have been observed in literature.1–3 Curiously, many findings, such as those examined in the present article, are inconsistent or lose statistical significance in adjusted analyses. Also puzzling is that most of the statistically significant associations are weak; that is, effect sizes are small. There are several possible explanations, considered below, and these need to be addressed in future studies.
First, many women who use cannabis during pregnancy may be reluctant to admit it; if so, their pregnancies will be classified as unexposed, adverse outcomes associated with their pregnancies will be included in control groups, and exposed and unexposed (control) groups may not differ or will differ to smaller extents.
Next, many women who use cannabis may also use tobacco and other substances, and these substances, and their covariates, may share variance with cannabis for the occurrence of adverse gestational outcomes. As a result, when these substances are adjusted for, cannabis may appear to play a diminished “unique” role when its true role may actually be larger. This appeared to be the case, for example, in a study that found that cannabis use disorder during pregnancy was associated with a substantially higher risk of ASD in nonsmokers than in smokers.11
Third, for at least the childhood outcomes, the findings can be biased towards the null when outcomes are ascertained too early. As an example, developmental delays were ascertained at a mean age of 29 months in one study.10
Fourth, if outcome ascertainment is imprecise, the imprecision may introduce statistical noise that makes differences between groups hard to determine. As an example, in one study of cannabis-exposed pregnancies,12 the overall prevalence of ASD was found to be surprisingly high at 3.6% at the early age of approximately 3 years. One wonders how accurate the diagnoses of ASD might have been.
Parting Notes
Much of the currently available research is based on exposures that occurred decades ago, and the absolute numbers of exposed pregnancies (for different adverse outcomes) are not large. Given the increasing prevalence of use of cannabis during pregnancy, the increasing potency of street cannabis, and the study limitations discussed in earlier sections of this article, it is likely that the available findings underestimate the magnitude and breadth of the current problem and the severity of the current risks. Cannabis is not a necessary substance for use during pregnancy, and so women who believe that it is a natural product, and therefore safe, might do well to guard against complacency and unnecessary exposure.
Finally, if cannabis use is also a marker for adversities, these adversities need to be identified and addressed in order to improve pregnancy and offspring outcomes.
Article Information
Published Online: January 6, 2025. https://doi.org/10.4088/JCP.24f15753
© 2025 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Maternal cannabis use during pregnancy and neuropsychiatric adverse outcomes during childhood and early adult life. J Clin Psychiatry. 2025;86(1): 24f15753.
Author Affiliations: Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India; Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India ([email protected]).
References (12)

- Andrade C. Maternal cannabis use during pregnancy and maternal and neonatal adverse outcomes. J Clin Psychiatry. 2024;85(4):24f15611. PubMed CrossRef
- Andrade C. Towards a further understanding of meta-analysis using gestational exposure to cannabis and birth defects as a case in point. J Clin Psychiatry. 2024;85(4):24f15673. PubMed CrossRef
- Andrade C. Maternal cannabis use in pregnancy and autism spectrum disorder or attention-deficit/hyperactivity disorder in offspring. J Clin Psychiatry. 2025;86(1):24f15717.
- Bassalov H, Yakirevich-Amir N, Reuveni I, et al. Prenatal cannabis exposure and the risk for neuropsychiatric anomalies in the offspring: a systematic review and meta-analysis. Am J Obstet Gynecol. 2024;231(6):574–588.e8. PubMed CrossRef
- Vaucher J, Keating BJ, Lasserre AM, et al. Cannabis use and risk of schizophrenia: a Mendelian randomization study. Mol Psychiatry. 2018;23(5):1287–1292. PubMed CrossRef
- Fine JD, Moreau AL, Karcher NR, et al. Association of prenatal cannabis exposure with psychosis proneness among children in the Adolescent Brain Cognitive Development (ABCD) study. JAMA Psychiatry. 2019;76(7):762–764. PubMed CrossRef
- Paul SE, Hatoum AS, Fine JD, et al. Associations between prenatal cannabis exposure and childhood outcomes: results from the ABCD study. JAMA Psychiatry. 2021;78(1):64–76. PubMed CrossRef
- Baranger DAA, Paul SE, Colbert SMC, et al. Association of mental health burden with prenatal cannabis exposure from childhood to early adolescence: longitudinal findings from the Adolescent Brain Cognitive Development (ABCD) study. JAMA Pediatr. 2022;176(12):1261–1265. PubMed CrossRef
- Keim SA, Fried P, Yeates KO, et al. Prenatal cannabis exposure and executive function and aggressive behavior at age 5 years. JAMA Pediatr. 2024;178(12):1316–1325. PubMed CrossRef
- Avalos LA, Oberman N, Alexeeff SE, et al. Early maternal prenatal cannabis use and child developmental delays. JAMA Netw Open. 2024;7(10):e2440295. PubMed CrossRef
- Tadesse AW, Ayano G, Dachew BA, et al. Exposure to maternal cannabis use disorder and risk of autism spectrum disorder in offspring: a data linkage cohort study. Psychiatry Res. 2024;337:115971. PubMed CrossRef
- Avalos LA, Shenkute M, Alexeeff SE, et al. Maternal prenatal cannabis use and child autism spectrum disorder. JAMA Netw Open. 2024;7(10):e2440301. PubMed CrossRef
This PDF is free for all visitors!