Abstract
Objective: Pharmacotherapy plays a crucial role in treating attention-deficit/ hyperactivity disorder (ADHD). However, current medications for ADHD have limitations and potential adverse effects. Glutamate, a neurotransmitter that directly and indirectly modulates dopamine neurotransmission, is considered a new therapeutic target for ADHD. We conducted a systematic review to determine the efficacy and safety of memantine, an uncompetitive N-methyl D-aspartate (NMDA) receptor antagonist, in both pediatric and adult patients with ADHD.
Data Sources: We searched PubMed, EMBASE, PsycINFO, and Cochrane Library for articles on memantine use in ADHD patients published up to August 31, 2023, using terms related to ADHD and memantine.
Study Selection: Studies selected according to PRISMA guidelines. We included both randomized and nonrandomized trials for a comprehensive review. We excluded non-English publications, review articles, and studies without full text.
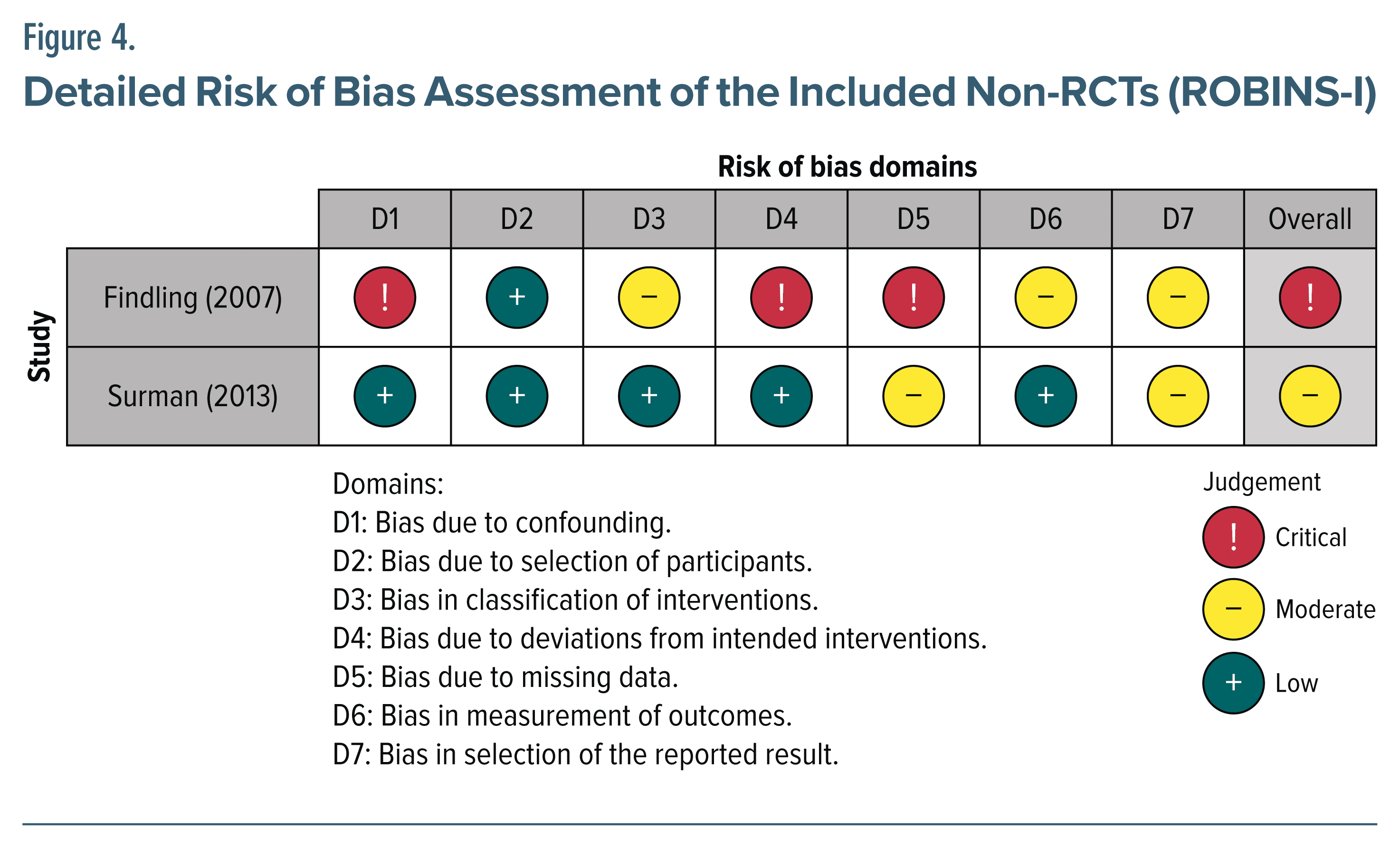
Data Extraction: Two authors extracted data using the data extraction form designed for this review. Independent authors conducted a risk of bias assessment using risk of bias 2 (RoB 2) and Risk of Bias in Nonrandomized Studies of Interventions (ROBINS-I).
Results: Six studies met the inclusion criteria, 3 on pediatric populations, and 3 on adults. Three studies were conducted in the United States (2 in adults) and 3 in Iran (1 in adults). Memantine showed potential benefits in managing ADHD symptoms and had a favorable safety profile. However, most studies involved small patient groups at single institutions, and their quality was low.
Conclusions: Memantine has the potential to be a relatively safe alternative or adjunctive treatment for ADHD, but more refined studies with larger populations are needed.
J Clin Psychiatry 2025;86(1):24r15507
Author affiliations are listed at the end of this article.
Attention-deficit/hyperactivity disorder (ADHD) is a widely acknowledged psychiatric disorder characterized by long-lasting symptoms of inattention or hyperactivity/impulsivity.1 ADHD was previously recognized as a disorder exclusively present in children and adolescents, but recent research has investigated it in the adult population. It is now considered to be a chronic “lifespan” disorder,2 with evidence indicating personal, social, and occupational impairments that extend into adulthood.3
ADHD is currently thought to be a multifactorial neurodevelopmental disorder involving alterations in the dopamine, norepinephrine, and serotonin systems.4–6 Recent pharmacologic interventions to treat ADHD regulate the dopaminergic and noradrenergic systems by blocking the reuptake of those neurotransmitters. Pharmacologic treatments for ADHD are classified as stimulants (eg, methylphenidate and amphetamine) and nonstimulants (eg, atomoxetine, atomoxetine, guanfacine, clonidine, and viloxazine, recently approved for ADHD).7–10 Both classes of medications have received approval for use in children, adolescents, and adults. Especially, stimulants are used as first-line treatment in both children and adults with reasonable treatment efficacy and tolerability.11 However, they have limitations such as a short duration of action9 and concerns about misuse.12 Furthermore, evidence suggests that long-term treatment with those drugs might have a negative effect on growth, leading to decreases in the weights and body mass indexes of children with ADHD9,13 and increasing the risk of cardiovascular disease in both adolescents14 and adults.15 Furthermore, the occurrence of those adverse effects can lead to nonadherence to the treatment of ADHD across all age groups, with reported nonadherence rates ranging from 15% to 85%.16 In adults with ADHD, common adverse effects that increase proportionally with stimulant dosage include decreased appetite, dry mouth, sleep problems, headaches, and nausea, which often lead to reduced medication adherence.17 For these reasons, various nonstimulant drugs are now being used to treat ADHD. Additionally, approximately 40% of patients exhibit an inadequate response to stimulant medications, necessitating a medication change to nonstimulant medication.18 However, the effects of nonstimulant medications tend to occur more slowly than those of stimulants, and they exhibit limited efficacy and produce side effects similar to those of stimulant medications.19,20
The Potential Role of Glutamate in ADHD
In this context, glutamate is a noteworthy target neurotransmitter for treatment of ADHD. Glutamate is an important neurotransmitter in disease models for disorders such as schizophrenia21 and Alzheimer disease,22 and it is thought to regulate dopamine release through a neuronal interaction between the prefrontal cortex and the striatum, an important brain region in ADHD.23 The glutamatergic system extends throughout various brain regions and influences the development and function of the brain from embryonic stages to adulthood.24 Disruption of glutamatergic function has been shown to be associated with symptoms of ADHD in both animal models25 and human studies, as evidenced by in vivo studies, magnetic resonance spectroscopy studies,26,27 and a biomarker study.28 Although the brain regions affected by ADHD differ between children and adults, recent meta-analyses have found that an increase in glutamatergic tone in the right medial frontal area in children and adolescents is significant and meaningful in ADHD.26 In adults with ADHD, glutamate levels in the anterior cingulate cortex correlate positively with symptoms related to impulsivity and excessively inappropriate behavior.29 Furthermore, in human studies, normalization of glutamatergic activity has been observed following drug treatment with both these types of medications to treat ADHD.24,30,31 These findings suggest that glutamate alterations in humans might be involved in the pathophysiology of ADHD.
Glutamate-Dopamine Neurotransmission Interaction in ADHD
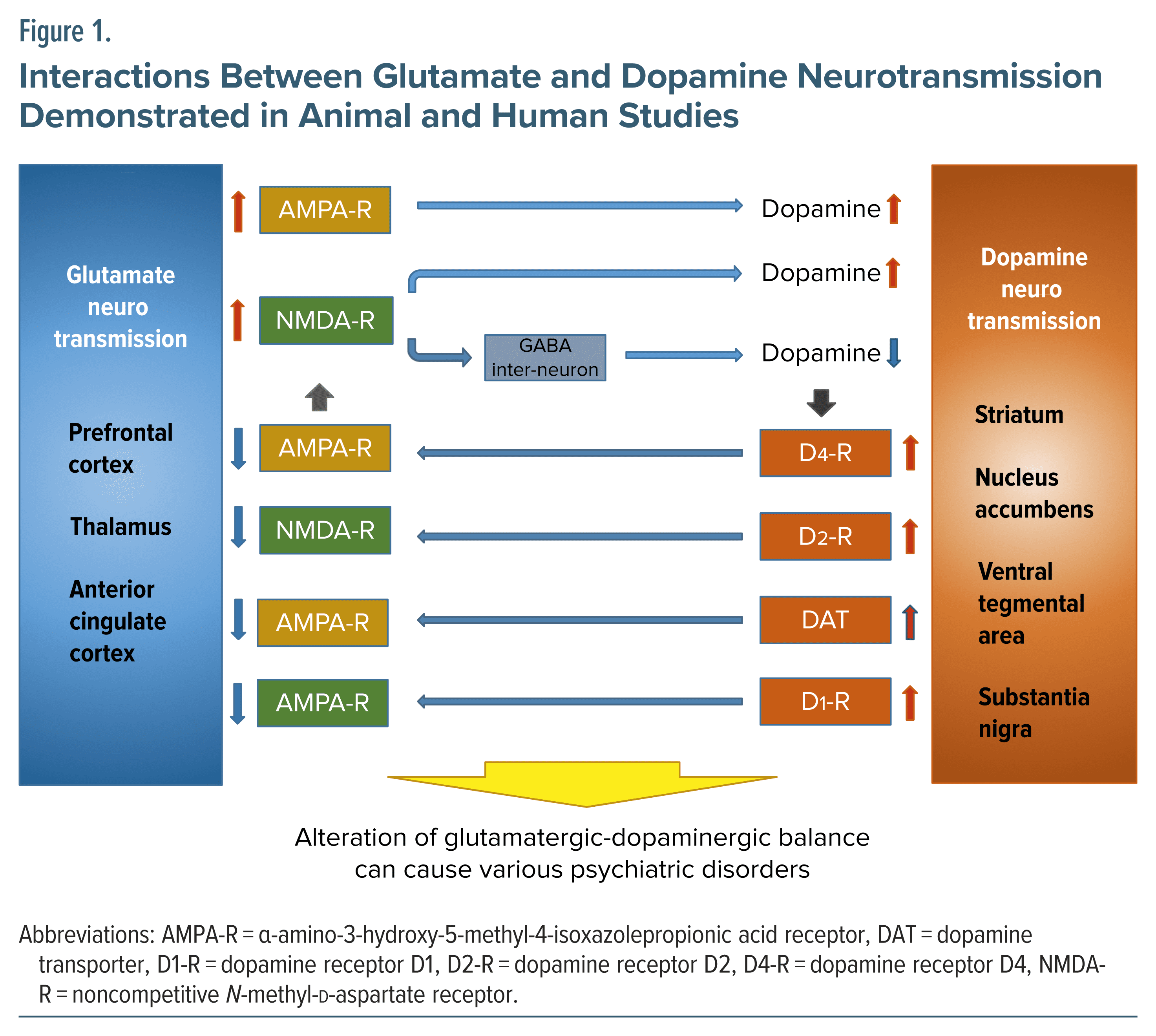
Considering the complex interactions identified between dopaminergic neurons and glutamatergic neurons in various brain regions defined in human and animal studies,21,23,25,32–39 glutamate holds potential as a crucial neurotransmitter in the pathophysiology of various psychiatric disorders, including ADHD (Figure 1). Furthermore, integrated findings from genomic studies of glutamate receptors in individuals with ADHD37,40–43 support their role in the pathophysiology of ADHD.
Previous in vivo studies have verified the involvement of glutamate in ADHD symptoms.37 The results of those studies indicate that noncompetitive N-methyl-D aspartate (NMDA) receptor blockers44 or glutamate allosteric modulators45 improve hyperactivity and attention, which are the core symptoms of ADHD. It has also been shown that spontaneously hypertensive rats, an animal model of ADHD, have increased glutamate induced dopamine release in the substantia nigra.34 However, another animal study46 reported that activating NMDA receptors triggers dopamine release in the striatum. Results about the association between NMDA receptors and dopamine are mixed.
The Glutamate-Modulating Effects of Memantine and Its Therapeutic Potential in ADHD
Memantine, an uncompetitive and reversible antagonist of the NMDA receptor, has been approved by the US Food and Drug Administration to treat Alzheimer disease.47 Its pharmacologic kinetics involve rapid blocking and unblocking of the NMDA receptor that is mediated by membrane depolarization.48,49 Consequently, memantine is deemed to regulate glutamatergic neurotransmission through its low affinity to the NMDA receptor.50,51 It also has a unique characteristic termed partial trapping to indicate that its occupancy of the receptor fluctuates depending on the concentration of glutamate, a neurotransmitter that activates the NMDA receptor.51–53
According to previous human research, memantine controls both prefrontal glutamate and dopamine activity and the overall activity level in prefrontal regions.50,54–57 Furthermore, memantine exhibits neuroprotective effects by modulating excessive NMDA receptor activity, which prevents an influx of neurotoxic calcium ions and increases the release of neurotrophic factor from astroglia in the brain.58
In this context, memantine might ameliorate the symptoms of ADHD by regulating dopamine neurotransmission and can exert neuroprotective effects by modulating glutamatergic neurotransmission. Lately, interest has been growing in the use of memantine not only to treat Alzheimer disease but also to manage other psychiatric disorders, including cognitive function in schizophrenia59 and aggression and behavioral problems associated with autism spectrum disorder.60
Recently, Abdi Dezfouli et al61 conducted a systematic review of the efficacy of antidementia drugs such as donepezil and memantine in ADHD; however, that study focused on the association between Alzheimer disease and ADHD, and it did not differentiate treatment efficacy or safety between pediatric and adult ADHD patients.
Given the therapeutic potential of memantine in ADHD, there is a need to establish its therapeutic efficacy and safety, as well as the associated glutamate modulation mechanism and its correlation with ADHD. Thus, our systematic review of relevant studies aims to elucidate the efficacy and safety of memantine among pediatric and adult patients with ADHD.
METHOD
Study Search Strategy and Data Sources
The present review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.62 We searched the PubMed, EMBASE, Scopus, PsycINFO, and Cochrane Central Register of Controlled Trials electronic libraries to find studies published before August 31, 2023. Following previous systematic reviews of memantine,63,64 we combined the search terms “adhd” OR “add” OR “attention deficit” with a list of search terms related to memantine: memantine OR memantin OR memantine hydrochloride OR 1,3-dimethyl-5-aminoadamantane OR 1-amino-3,5-dimethyladamantane OR namenda OR ebixa OR axura. Two authors (W.-S.C. and Y.S.W.) independently conducted the initial search. This study was registered with PROSPERO (CRD42023460516).
Inclusion and Exclusion Criteria
We included randomized clinical trials (RCTs) with double-blind, parallel group, and placebo- or active controlled designs in our review. In addition, to comprehensively evaluate the safety and efficacy of memantine by examining adverse effects across various studies, we also included non-RCTs.
To accommodate the heterogeneity of diagnostic tools used for ADHD, we included studies of patients diagnosed by any set of ADHD diagnostic criteria (eg, Diagnostic and Statistical Manual of Mental Disorders [DSM] or International Classification of Diseases) or a standardized screening/diagnostic tool (eg, Adult ADHD Self-report Scale [ASRS]65). Our search was not limited based on ADHD subtype or presentation, gender, intelligence quotient, socioeconomic status, or comorbidities. We excluded review articles (including systematic reviews, narrative reviews, and meta analyses), nonrelevant articles, non-English papers, studies without full-text access, and abstract-only papers.
Study Selection and Data Extraction
First, the studies obtained from the initial search were deduplicated by EndNote 20. Then, inclusion/ exclusion screening was performed by 2 reviewers (W.-S.C. and Y.S.W.). The initial evaluation assessed the titles and abstracts for inclusion or exclusion. For articles whose relevance was uncertain, a full-text review was conducted. Subsequently, the complete texts of all included articles were acquired for a comprehensive assessment against our detailed eligibility criteria. All disparities that occurred during study selection were addressed through discussion, with the involvement of other authors as needed.
This review extracted the following data from the full texts of the selected studies: (1) description of study characteristics (country, year of publication, type of study, sample size, age range or mean age/SD, and gender composition); (2) diagnostic tools used for ADHD; (3) intervention method, dosage of memantine, and duration of intervention; (4) study outcome, adverse events, and all-cause dropouts during the trial. All extracted data were logged in a Microsoft Excel spreadsheet.
Study Classification
We classified the selected studies into research targeting pediatric and adult populations, defining pediatric populations as people aged 17 years or younger and adult populations as people aged 18 years or older. We included all types of clinical studies, both RCTs and non-RCTs, and did not categorize them by type.
Assessing the Risk of Bias
Two authors (W.-M.B. and S.M.W.) independently assessed the risk of bias in the included studies. The second version of the Cochrane risk of bias tool (RoB.2) was used to assess RCTs, and non-RCTs were assessed using the Risk of Bias in Nonrandomized Studies of Interventions (ROBINS-I) tool.66 This instrument evaluates potential biases from confounding, participant selection, intervention classification, deviations from intended interventions, missing data, outcome measurement, and reported result selection.
RESULTS
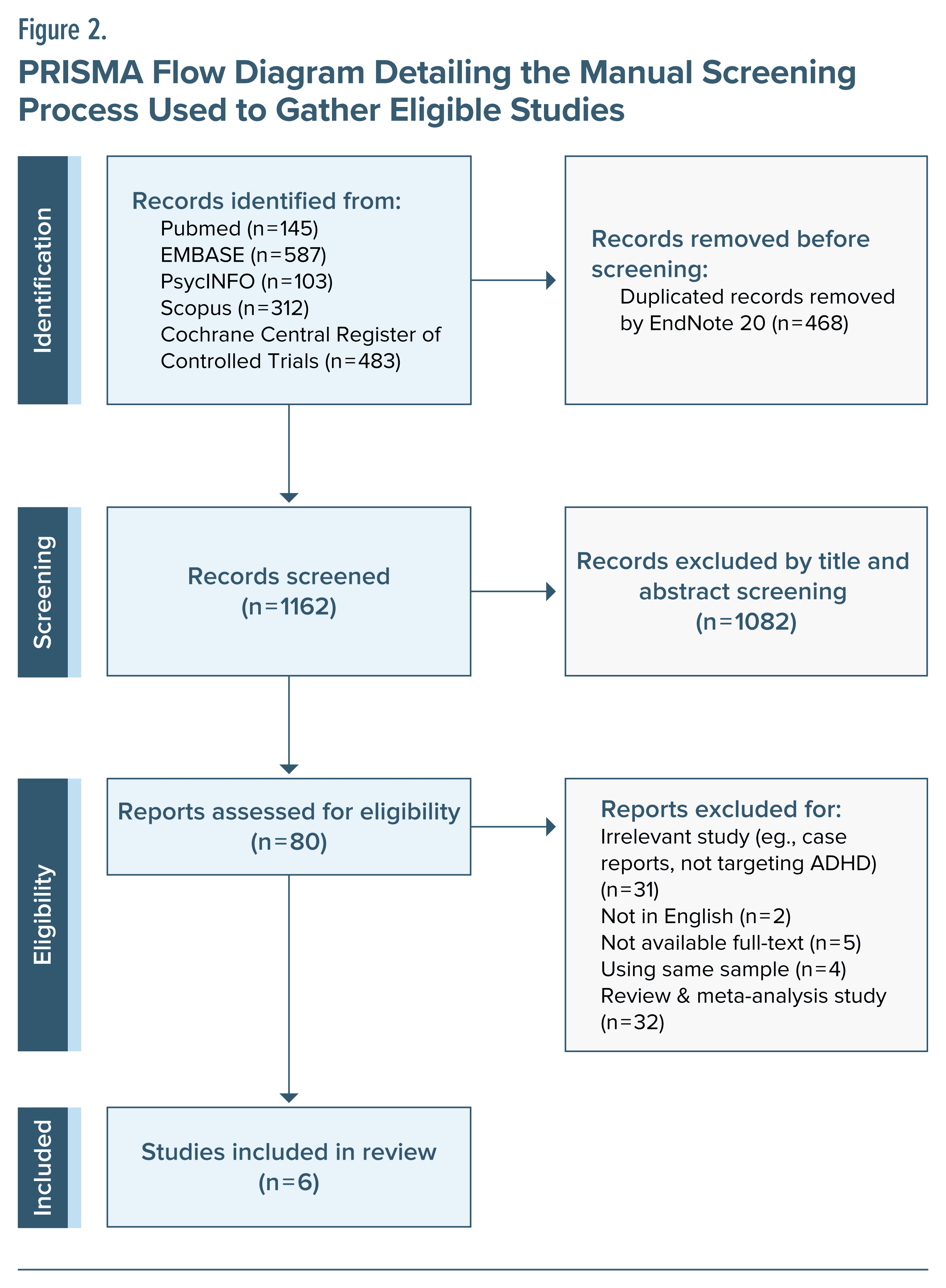
In total, 1,630 articles were identified by the aforementioned method, and 468 duplicates were removed. An additional 1,082 were excluded by screening titles and abstracts. The remaining 80 articles were reviewed in full to identify whether they met the inclusion and exclusion criteria of our study, and 74 articles were excluded. Therefore, 6 articles were included in our systematic review. The PRISMA flow diagram, including the detailed reasons for exclusion, is presented in Figure 2.
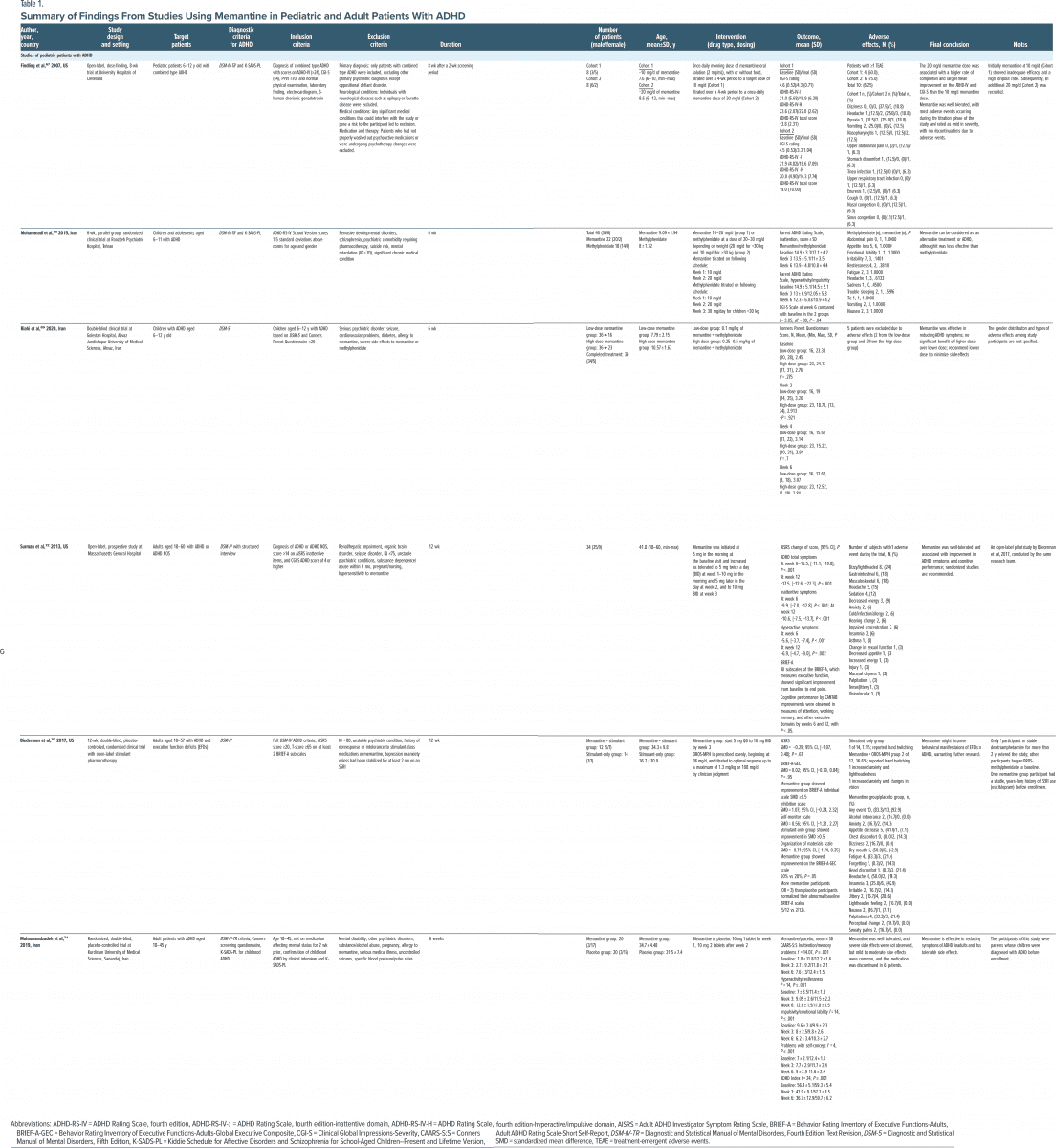
Characteristics of the Included Studies
Of the 6 studies, 3 focused on pediatric populations67–69 and the remaining 3 targeted adults.70–72 Among the studies targeting pediatric populations, 1 was conducted in the United States,67 and 2 were carried out in Iran.68,69 Among the studies targeting adults, 2 were conducted in the United States,70,72 and 1 was carried out in Iran.71 Only 1 study distinguished between subtypes of ADHD and included only the combined type.67 A summary of each included study is presented in Table 1.
Studies About Pediatric Patients With ADHD
Findling et al67 conducted an open-label study of memantine in children aged 6–12 years with ADHD. Their research objective was to determine a dosage of memantine that is both safe and efficacious in children. They included patients with the combined type of ADHD based on the DSM-IV-TR diagnostic criteria (called the combined presentation in DSM-5). The diagnosis of ADHD in the children involved a 2-step process of screening and diagnosis confirmation. The screening used DSM-IV-TR and the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime Version (K-SADS-PL),73 and diagnosis confirmation used the ADHD Rating Scale, Fourth Edition (ADHD-RS-IV),74 the Clinical Global Impressions Severity scale (CGI-S),75 and the Peabody Picture Vocabulary Test, Third Edition (PPVT III),76 to evaluate intellectual function. The investigators initially recruited 8 participants (3 boys and 5 girls). They started with a memantine dose of 10 mg/d, but some patients did not show sufficient symptom improvement, resulting in challenges in patient retention. Therefore, they recruited 8 more participants (6 boys and 2 girls), all receiving a higher dose of 20 mg/ d. As a result, both dosage groups showed positive effects, with the higher dose group (20 mg/d) exhibiting greater improvement in ADHD-RS-IV and CGI-S scores. Furthermore, they estimated the maximum plasma concentration of memantine and reported a dose dependent therapeutic effect when the plasma concentration of memantine reached a certain initial threshold. No severe adverse effects were observed in either group.
One of the 2 pediatric studies conducted in Iran68 was a single-center, parallel group, double-blind clinical trial. The study focused on children aged 6–11 years and used DSM-IV-TR and K-SADS-PL to diagnose ADHD. Each child diagnosed with ADHD was randomized into a group receiving methylphenidate or a group receiving memantine. Patients received medication for 6 weeks, with both drugs titrated up over 3 weeks to a maximum of 30 mg/d for methylphenidate and 20 mg/d for memantine. The ADHD-RS-IV and CGI-S instruments were used for efficacy comparison, and measurements were collected at baseline, 3 weeks, and 6 weeks. Forty patients were enrolled in the study (18 for methylphenidate and 22 for memantine). Neither drug caused serious side effects, and their effectiveness did not differ significantly. However, according to the 6- week ADHD-RS-IV assessment, methylphenidate showed better treatment results. The main limitation of this study is the absence of patients treated with a placebo. The researchers argued that memantine could serve as a safe alternative treatment for patients unable to use methylphenidate.
The second pediatric trial conducted in Iran69 was a 6- week, single-center, double-blind trial to investigate the efficacy and safety of memantine to augment methylphenidate treatment. Children aged 6–12 years participated in the study. The researchers diagnosed ADHD using the DSM-5 and included children with Conners Parent Rating Scale (CPRS)77 scores of 20 or higher. They randomly divided the patients into low-dose memantine (0.1 mg of memantine/kg) and high-dose memantine (0.25–0.5 mg of memantine/kg) groups. In both groups, the children were titrated up to a maximum of 20 mg of methylphenidate per day for 4 weeks. During the remaining 2-week observation period, a fixed dose of methylphenidate and memantine was administered. Throughout the trial, the parents provided CPRS scores at 2-week intervals. The researchers initially recruited 72 patients, but only 39 (16 from the low-dose group and 23 from the high-dose group) completed the study. Among the 33 patients who dropped out, 5 (2 from the low-dose group and 3 from the high-dose group) withdrew due to side effects. However, the authors did not provide details about those side effects. The study reported no significant difference in therapeutic effects (as shown by CPRS scores) between the low-dose and high dose groups. The researchers suggested that adding a low dose of memantine to methylphenidate might be better than adding a high dose. A limitation of their study, as in the other studies, was the absence of a placebo group.
Studies About Adult Patients With ADHD
The memantine studies targeting adult ADHD consisted of 1 open-label trial72 and 2 RCTs.70,71 The 2 studies conducted in the US were carried out by the same research group.70,72
Surman et al72 conducted an open-label trial as a pilot study to assess the treatment effects on executive function and the safety and tolerability of memantine in adults with ADHD. In the study, the target population was individuals aged 18–60 years who were diagnosed with ADHD based on the DSM-IV criteria. Because the DSM IV criteria required that symptoms be present before age 7 years for an ADHD diagnosis,78 the researchers included cases that met the diagnostic criteria for ADHD but exhibited symptoms emerging after age 7, defining them as ADHD-NOS (not otherwise specified). During the 12- week observation period, the participants (n = 34, 74% male) started with a daily memantine dose of 5 mg and titrated up to a daily dose of 20 mg. The Adult ADHD Investigator Symptom Rating Scale (AISRS)79 was used to assess ADHD symptoms, and the Behavior Rating Inventory of Executive Function-Adult Version (BRIEF A)80 and Cambridge Neuropsychological Test Automated Battery (CANTAB)81 were used to evaluate executive function after 3 weeks. In this study, memantine presented therapeutic effects for ADHD symptoms in approximately half of the patients (44%), without significant serious side effects. Patients with initially lower scores on CANTAB and BRIEF-A, indicating lower performance, showed greater improvement in AISRS scores than others after treatment. This implies increased responsiveness to the medication in individuals with lower cognitive functioning. However, this study has limitations, including a small sample size and the absence of a placebo group, and the placebo effect cannot be excluded.
Building upon Surman et al,72 the same research team presented an RCT in 2017 that investigated the use of memantine as an adjunct to methylphenidate in adult ADHD patients aged 18–57 years.70 Similar to the earlier study,72 they diagnosed ADHD using the DSM-IV and AISRS. However, they narrowed the participant window by including only those with AISRS scores of 20 or higher and BRIEF-A subscale scores of 65 or higher in at least 2 areas. All participants had been receiving a stimulant at an appropriate dose for a minimum of 1 month or were newly initiated to methylphenidate upon enrollment. The participants were openly prescribed methylphenidate at a minimum of 36 mg/d, with a maximum dosage of 1.3 mg/kg (low dose) or 108 mg/d (high dose), as determined by clinical judgment. This trial was conducted over a 12-week study period, with patients randomly assigned to either the memantine augmentation or stimulant-only group in a 1:1 ratio. A total of 33 participants were recruited, with 29 randomized. Ultimately, 26 patients (14 for stimulant only and 12 for memantine augmentation) completed the 12-week trial. Overall, the reduction in AISRS scores and improvement in BRIEF-A total scores did not differ significantly between the stimulant-only and memantine-augmentation groups. Differences between the 2 groups were notable in individual BRIEF-A subscales. The memantine-augmentation group showed greater improvement in the Inhibit and Self-Monitor scales, and the Organization of Materials scale demonstrated higher improvement in the stimulant only group. In terms of safety, 3 participants discontinued the trial due to side effects—1 in the stimulant-only group (hand twitching) and 2 in the memantine-augmentation group (anxiety, dizziness, and visual disturbance). The adverse effect frequencies were similar between the memantine-augmentation and stimulant-only groups (83.3% vs 92.9%), with common issues such as dry mouth, headache, and insomnia potentially influenced by the use of concurrent stimulant medications. This study is also limited by its small sample size, which restricts the generalizability of the findings and complicates comparisons of differences in treatment effects using standardized mean differences or odds ratios.
The most recent study conducted on adults is by Mohammadzadeh et al,71 conducted in Iran. They conducted a 6-week, single-center, double-blind RCT targeting adult ADHD patients aged 18–45 years with no history of psychotropic medication for at least 2 weeks before the study. A distinctive feature of this study is that the primary participants were the parents of children diagnosed with ADHD. Participants were initially screened for the presence of childhood ADHD through a psychiatric interview. Subsequently, the K-SADS-PL was conducted to confirm the diagnosis of pediatric ADHD according to the DSM-IV-TR diagnostic criteria. The participants were randomly assigned to either the memantine or placebo group (n = 20 for both groups). The memantine group received 10 mg/d for the first week and then 20 mg/d for the remainder of the trial. The treatment effects between the 2 groups were compared using the Conners Adult ADHD Rating Scale—Short Self-Report (CAARS S:S).82 The memantine group differed significantly from the placebo group in the reduction of all 5 subscales of the CAARS-S:S after 3 and 6 weeks of medication. Although patients in the memantine group did not experience severe adverse effects, 6 of the 20 stopped taking the medication due to mild to moderate side effects such as dizziness, confusion, constipation, back pain, and sleepiness.
Risk of Bias Assessment
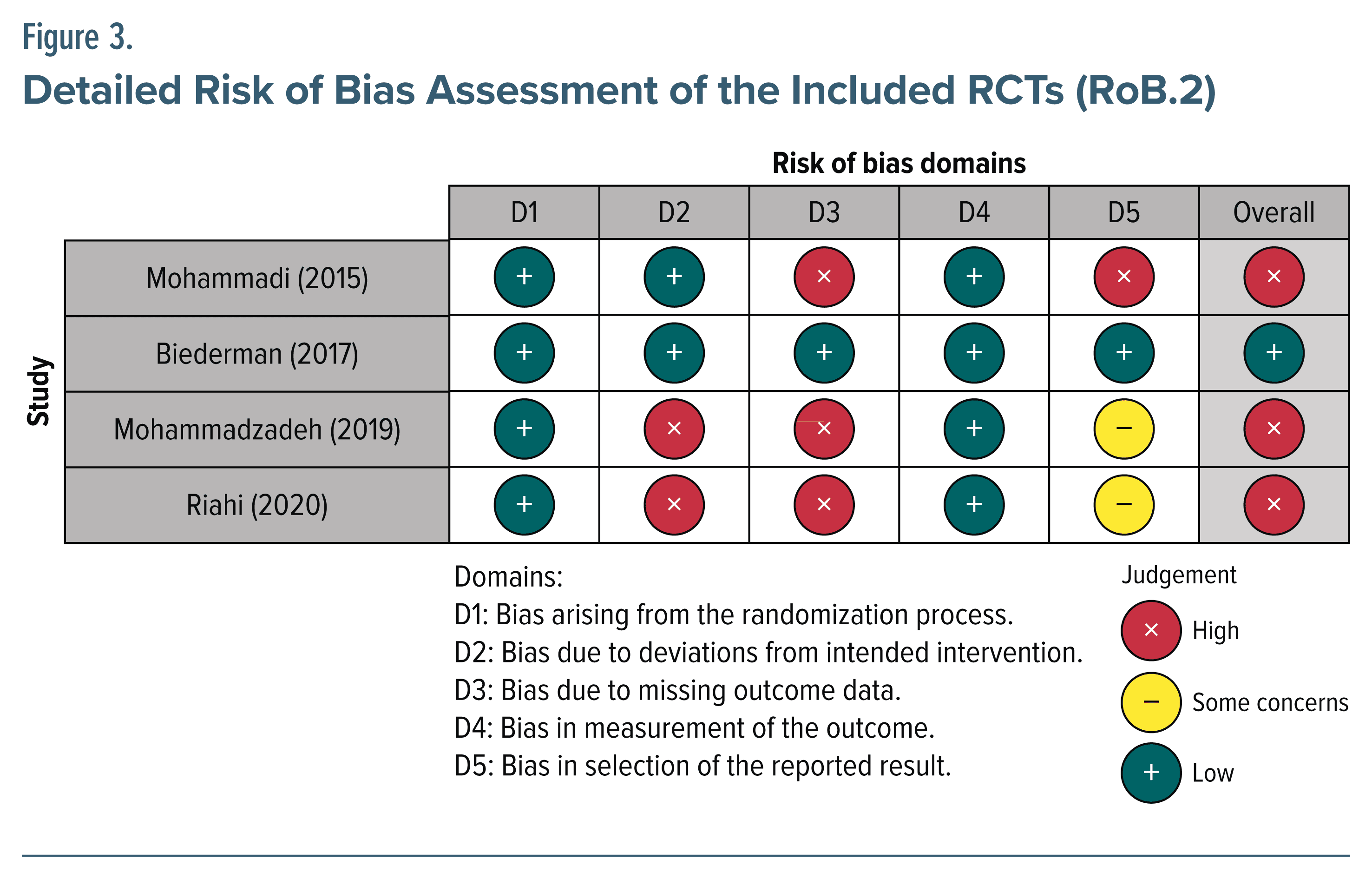
According to the RoB.2 and ROBINS-I tools used to assess the risk of bias in each study, only 1 RCT70 exhibited a low level of bias, and only 1 non-RCT study72 was deemed to have a moderate level of bias. The remaining 4 studies67–69,71 all demonstrated a high degree of bias. The most common reason for the high risk of bias was missing outcome data. The detailed risk of bias assessments for each study are presented in Figures 3 and 4.
DISCUSSION
This systematic review evaluated the potential of memantine as a pharmacologic option for treating ADHD in both pediatric and adult patients. As far as we know, this is the first systematic review to investigate the efficacy and safety of memantine.
The 6 studies included in this review predominantly used the DSM-IV, DSM-IV-TR, or DSM-5 criteria for ADHD diagnosis. In studies of pediatric subjects, the K-SADS-PL was additionally used for diagnosis. Additional diagnostic tools, such as ASRS, CAARS, or the Diagnostic Interview for ADHD in adults,83 were not used for the adult ADHD participants. This is presumed to be a strategic choice to maximize the inclusion of a larger number of patients, given the small final participant number.
In the 3 studies targeting pediatric ADHD, memantine showed ameliorative effects on ADHD symptoms when administered as a monotherapy.67,69 When it was compared with methylphenidate, no significant differences were observed in the treatment efficacy for ADHD.68 A notable characteristic across all 3 studies is the absence of severe adverse events, including psychiatric manifestations such as exacerbation of ADHD symptoms or mood alterations, associated with either low- (10 mg/d) or high-dose (20 mg/d) regimens in the pediatric population. Only a few neurological side effects, such as headaches and dizziness, were observed. Memantine, approved for use in individuals with moderate to severe Alzheimer disease, is considered to have minimal serious adverse effects.84 This safety profile has been well documented in previous studies in pediatric and adolescent neurological patients.85 Although its therapeutic efficacy remains a subject of debate, antecedent studies using memantine in pediatric patients with psychiatric conditions such as autism spectrum disorder,86–88 pervasive developmental disorder,89,90 or other neurological disorders such as epilepsy85 corroborate our findings.
In studies of adult ADHD patients, memantine demonstrated efficacy in addressing ADHD symptoms in both an open-label study72 and an RCT.71 Also, as an adjunct to stimulant therapy, memantine exhibited treatment efficacy superior to stimulant monotherapy in improving executive function and alleviating ADHD symptoms.70 A previous study indicated that memantine could lead to increased glucose metabolism in the frontal lobe of traumatic brain injury patients, accompanied by corresponding improvements in cognitive function.91 That finding might be due to memantine’s indirect agonism for dopamine, which is the primary neurotransmitter for frontal lobe function.24,92 In previous studies, memantine administration has been shown to increase dopamine levels in the frontal cortex and striatum.55,93 Alterations in dopamine transporter density in these brain regions are thought to be an important pathophysiology of ADHD.94,95 In this context, the dopaminergic action of memantine might have contributed to its improvement of executive function and ADHD symptoms.
When memantine was used in adults as an adjunctive therapy with stimulants,70 some psychiatric manifestations were reported, such as an increase in anxiety, and gastrointestinal adverse effects, particularly appetite reduction and nausea, were prevalent. However, the authors suggest that those side effects might have been due to the coadministered methylphenidate rather than the memantine. When memantine was used as a monotherapy, neurological adverse effects, such as lightheadedness, were relatively frequent. These findings are similar to the adverse effects observed in pediatric ADHD patients in this review.
Our review has several limitations that should be acknowledged in the interpretation. First, most of the studies (5 of 6) were from a single center, and all were conducted in either the US or Iran. Thus, there are limitations in extrapolating the suggested therapeutic effects and safety of memantine proposed in this review. Second, most studies targeted only a small number of participants (from 16 to 72), which limits the generalizability of the findings. Third, due to limitations in the data provided in the included studies, we were unable to determine whether memantine was more effective for inattention or impulsivity/hyperactivity in pediatric and adult populations. In the same vein, most studies have not differentiated between subtypes of ADHD, which limits the interpretation of the study results. Fourth, only 161 of the 3 studies using methylphenidate67,68,70 provided information on the drug formulation. Lastly, 567–69,71,72 of the 6 studies in this review were judged to have a high potential for bias in reporting their outcome results. This further weakens the evidence for memantine’s therapeutic benefit in ADHD.
Nevertheless, we consider the potential of memantine as an agent with dopaminergic and norepinephrine actions similar to the stimulant and nonstimulant agents already used to treat ADHD. As an alternative to developing novel drugs, drug repurposing is being supported by both governments and industry due to the high cost of new drug development.96 With recent advances in proteomics and genomics, this repurposing is also being applied to various psychiatric diseases.97,98 Furthermore, given the heterogeneous phenotypes of ADHD and the involvement of multiple neurobiological factors in ADHD symptoms, medications that do not target dopamine or norepinephrine directly, such as memantine, might have therapeutic benefit in patients who are unresponsive to stimulants. To treat ADHD in a broad and varied population, economically favorable off-patent drugs could be targeted for such repurposing, and memantine could be one option with a proven safety profile.
CONCLUSION
Memantine appears to be safe for the treatment of pediatric and adult patients with ADHD. It is also thought to improve overall ADHD symptoms and cognitive functioning in both populations, but the evidence for that is currently weak due to small sample sizes, short observation periods, and limited outcome reporting. To support clinical applications of memantine in children and adults with ADHD, prospective studies with larger sample sizes and structured double-blind designs are needed. Moreover, considering the efficacy and high tolerability of memantine, future studies are needed to classify ADHD subtypes and target patients with comorbid conditions in order to identify populations that may benefit more from memantine as either monotherapy or augmentation therapy for ADHD. Further research is also needed to confirm the complex link between the glutamate system and dopaminergic regulation in the human brain.
Article Information
Published Online: December 25, 2024. https://doi.org/10.4088/JCP.24r15507
© 2024 Physicians Postgraduate Press, Inc.
Submitted: July 12, 2024; accepted September 26, 2024.
To Cite: Choi WS, Wang SM, Woo YS, et al. Therapeutic efficacy and safety of memantine for children and adults with ADHD with a focus on glutamate-dopamine regulation: a systematic review. J Clin Psychiatry. 2025;86(1):24r15507.
Author Affiliations: Department of Psychiatry, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea (Choi, Wang, Woo, Bahk); Woo and Bahk Psychiatry Clinic, Seoul, Republic of Korea (Woo, Bahk).
Corresponding Authors: Won-Myong Bahk, MD, PhD ([email protected]), and Young S. Woo, MD, PhD ([email protected]), Department of Psychiatry, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 10, 63-ro, Yeongdeungpo-gu, Seoul 07345, Republic of Korea.
Relevant Financial Relationships: None.
Funding/Support: None.
ORCID: Won-Seok Choi: https://orcid.org/0000-0003-1774-9504; Sheng-Min Wang: https://orcid.org/0000-0003-2521-1413; Young S. Woo: https://orcid.org/0000-0002-0961-838X; Won-Myong Bahk: https://orcid.org/0000-0002-0156-2510
Clinical Points
- Current pharmacologic treatments for attention-deficit/ hyperactivity disorder (ADHD) face limitations in their use for some patients.
- Glutamate has been implicated in the pathophysiology of ADHD and holds the potential to be a therapeutic target for ADHD.
- Memantine may offer a safe treatment option when current ADHD medications have been ineffective or the patient is unable to tolerate the medications.
References (98)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition: DSM-5. American Psychiatric Association; 2013.
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–165. PubMed CrossRef
- Shaw M, Hodgkins P, Caci H, et al. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med. 2012;10:99. PubMed CrossRef
- Banerjee E, Nandagopal K. Does serotonin deficit mediate susceptibility to ADHD? Neurochem Int. 2015;82:52–68. PubMed CrossRef
- Del Campo N, Chamberlain SR, Sahakian BJ, et al. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69(12):e145–e157. PubMed CrossRef
- Faraone SV, Perlis RH, Doyle AE, et al. Molecular genetics of attention-deficit/ hyperactivity disorder. Biol Psychiatry. 2005;57(11):1313–1323. PubMed CrossRef
- Feldman ME, Charach A, Bélanger SA. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Paediatr Child Health. 2018;23(7):462–472.
- Pozzi M, Bertella S, Gatti E, et al. Emerging drugs for the treatment of attention deficit hyperactivity disorder (ADHD). Expert Opin Emerg Drugs. 2020;25(4): 395–407.
- Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450–462. PubMed CrossRef
- Robinson CL, Parker K, Kataria S, et al. Viloxazine for the treatment of attention deficit hyperactivity disorder. Health Psychol Res. 2022;10(3):38360. PubMed
- Cortese S, Adamo N, Del Giovane C, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5(9):727–738. PubMed CrossRef
- Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med. 2014;126(5):64–81. PubMed CrossRef
- Klein RG, Landa B, Mattes JA, et al. Methylphenidate and growth in hyperactive children. A controlled withdrawal study. Arch Gen Psychiatry. 1988;45(12):1127–1130. PubMed CrossRef
- Uzun N, Akıncı MA, Alp H. Cardiovascular disease risk in children and adolescents with attention deficit/hyperactivity disorder. Clin Psychopharmacol Neurosci. 2023;21(1):77–87.
- Zhang L, Li L, Andell P, et al. Attention-deficit/hyperactivity disorder medications and long-term risk of cardiovascular diseases. JAMA Psychiatry. 2024;81(2):178–187.
- Ahmed R, Aslani P. Attention-deficit/hyperactivity disorder: an update on medication adherence and persistence in children, adolescents and adults. Expert Rev Pharmacoecon Outcomes Res. 2013;13(6):791–815. PubMed CrossRef
- Bieś R, Fojcik J, Warchala A, et al. The risk of methylphenidate pharmacotherapy for adults with ADHD. Pharmaceuticals (Basel). 2023;16(9):1292.
- Schein J, Childress A, Cloutier M, et al. Reasons for treatment changes in adults with attention-deficit/hyperactivity disorder: a chart review study. BMC Psychiatry. 2022;22(1):377.
- Hanwella R, Senanayake M, de Silva V. Comparative efficacy and acceptability of methylphenidate and atomoxetine in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis. BMC Psychiatry. 2011;11:176. PubMed CrossRef
- Childress AC. A critical appraisal of atomoxetine in the management of ADHD. Ther Clin Risk Manag. 2015;12:27–39.
- Buck SA, Quincy Erickson-Oberg M, Logan RW, et al. Relevance of interactions between dopamine and glutamate neurotransmission in schizophrenia. Mol Psychiatry. 2022;27(9):3583–3591.
- Francis PT. The interplay of neurotransmitters in Alzheimer’s disease. CNS Spectr. 2005;10(11 suppl 18):6–9. PubMed CrossRef
- Erin MM, Theresa CT, Greg AG, et al. Dopamine and glutamate interactions in ADHD: implications for the future neuropharmacology of ADHD. In: Somnath B, ed. Attention Deficit Hyperactivity Disorder in Children and Adolescents. Ch 6. IntechOpen; 2013.
- Elia J, Izaki Y, Ambrosini A, et al. Glutamatergic neurotransmission in ADHD: neurodevelopment and pharmacological implications. J Pediatr Neonatol. 2020;2:1006.
- Cheng J, Liu A, Shi MY, et al. Disrupted glutamatergic transmission in prefrontal cortex contributes to behavioral abnormality in an animal model of ADHD. Neuropsychopharmacology. 2017;42(10):2096–2104. PubMed CrossRef
- Vidor MV, Panzenhagen AC, Martins AR, et al. Emerging findings of glutamate–glutamine imbalance in the medial prefrontal cortex in attention deficit/hyperactivity disorder: systematic review and meta-analysis of spectroscopy studies. Eur Arch Psychiatry Clin Neurosci. 2022;272(8):1395–1411. PubMed
- Maltezos S, Horder J, Coghlan S, et al. Glutamate/glutamine and neuronal integrity in adults with ADHD: a proton MRS study. Transl Psychiatry. 2014;4(3):e373. PubMed CrossRef
- Ulu E, Demirci E, Sener EF, et al. Role of glutamate receptor-related biomarkers in the etiopathogenesis of ADHD. Clin Psychopharmacol Neurosci. 2024;22(1):79–86.
- Bauer J, Werner A, Kohl W, et al. Hyperactivity and impulsivity in adult attention-deficit/hyperactivity disorder is related to glutamatergic dysfunction in the anterior cingulate cortex. World J Biol Psychiatry. 2018;19(7):538–546. PubMed CrossRef
- Egger B, Gold KS, Brand AH. Notch regulates the switch from symmetric to asymmetric neural stem cell division in the Drosophila optic lobe. Development. 2010;137(18):2981–2987. PubMed CrossRef
- Lubke GH, Hudziak JJ, Derks EM, et al. Maternal ratings of attention problems in ADHD: evidence for the existence of a continuum. J Am Acad Child Adolesc Psychiatry. 2009;48(11):1085–1093. PubMed CrossRef
- Abdallah CG, Averill LA, Krystal JH, et al. Glutamate and norepinephrine interaction: relevance to higher cognitive operations and psychopathology. Behav Brain Sci. 2016;39:e201. PubMed CrossRef
- Batten S, Gerhardt G, Glaser P. Should we be excited about glutamate dysregulation in the etiology of ADHD? A review of the data. In: Modulators of Glutamatergic Signaling. Nova Science Publishers, Inc; 2015:17–41.
- Warton FL, Howells FM, Russell VA. Increased glutamate-stimulated release of dopamine in substantia nigra of a rat model for attention-deficit/hyperactivity disorder—lack of effect of methylphenidate. Metab Brain Dis. 2009;24(4):599–613. PubMed CrossRef
- Naaijen J, Lythgoe DJ, Zwiers MP, et al. Anterior cingulate cortex glutamate and its association with striatal functioning during cognitive control. Eur Neuropsychopharmacol. 2018;28(3):381–391. PubMed CrossRef
- Sun X, Zhao Y, Wolf ME. Dopamine receptor stimulation modulates AMPA receptor synaptic insertion in prefrontal cortex neurons. J Neurosci. 2005;25(32):7342–7351. PubMed CrossRef
- Huang X, Wang M, Zhang Q, et al. The role of glutamate receptors in attention-deficit/hyperactivity disorder: from physiology to disease. Am J Med Genet B Neuropsychiatr Genet. 2019;180(4):272–286. PubMed CrossRef
- Kotecha SA, Oak JN, Jackson MF, et al. A D2 class dopamine receptor transactivates a receptor tyrosine kinase to inhibit NMDA receptor transmission. Neuron. 2002;35(6):1111–1122. PubMed CrossRef
- Yuen EY, Yan Z. Dopamine D4 receptors regulate AMPA receptor trafficking and glutamatergic transmission in GABAergic interneurons of prefrontal cortex. J Neurosci. 2009;29(2):550–562. PubMed CrossRef
- Hinney A, Scherag A, Jarick I, et al. Genome-wide association study in German patients with attention deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2011;156B(8):888–897. PubMed
- Kim JI, Kim JW, Park S, et al. The GRIN2B and GRIN2A gene variants are associated with continuous performance test variables in ADHD. J Atten Disord. 2020;24(11):1538–1546. PubMed
- Lasky-Su J, Neale BM, Franke B, et al. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B Neuropsychiatr Genet. 2008;147B(8):1345–1354. PubMed CrossRef
- Naaijen J, Bralten J, Poelmans G, et al. Glutamatergic and GABAergic gene sets in attention-deficit/hyperactivity disorder: association to overlapping traits in ADHD and autism. Transl Psychiatry. 2017;7(1):e999. PubMed
- Gainetdinov RR, Mohn AR, Bohn LM, et al. Glutamatergic modulation of hyperactivity in mice lacking the dopamine transporter. Proc Natl Acad Sci U S A. 2001;98(20):11047–11054. PubMed CrossRef
- Griebel G, Pichat P, Boulay D, et al. The mGluR2 positive allosteric modulator, SAR218645, improves memory and attention deficits in translational models of cognitive symptoms associated with schizophrenia. Sci Rep. 2016;6:35320. PubMed CrossRef
- Martínez-Fong D, Rosales MG, Góngora-Alfaro JL, et al. NMDA receptor mediates dopamine release in the striatum of unanesthetized rats as measured by brain microdialysis. Brain Res. 1992;595(2):309–315. PubMed CrossRef
- Robinson DM, Keating GM. Memantine: a review of its use in Alzheimer’s disease. Drugs. 2006;66(11):1515–1534. PubMed CrossRef
- Parsons CG, Gilling KE, Jatzke C. Blocking kinetics of memantine on NR1a/2A receptors recorded in inside-out and outside-out patches from Xenopus oocytes. J Neural Transm (Vienna). 2008;115(10):1367–1373. PubMed CrossRef
- Lipton SA. The molecular basis of memantine action in Alzheimer’s disease and other neurologic disorders: low-affinity, uncompetitive antagonism. Curr Alzheimer Res. 2005;2(2):155–165. PubMed CrossRef
- Rogawski MA, Wenk GL. The neuropharmacological basis for the use of memantine in the treatment of Alzheimer’s disease. CNS Drug Rev. 2003;9(3):275–308. PubMed CrossRef
- Johnson JW, Kotermanski SE. Mechanism of action of memantine. Curr Opin Pharmacol. 2006;6(1):61–67. PubMed CrossRef
- Parsons CG, Stöffler A, Danysz W. Memantine: a NMDA receptor antagonist that improves memory by restoration of homeostasis in the glutamatergic system – too little activation is bad, too much is even worse. Neuropharmacology. 2007;53(6): 699–723. PubMed CrossRef
- Johnson JW, Glasgow NG, Povysheva NV. Recent insights into the mode of action of memantine and ketamine. Curr Opin Pharmacol. 2015;20:54–63. PubMed CrossRef
- Danysz W, Parsons CG. The NMDA receptor antagonist memantine as a symptomatological and neuroprotective treatment for Alzheimer’s disease: preclinical evidence. Int J Geriatr Psychiatry. 2003;18(suppl 1):S23–S32. PubMed CrossRef
- Spanagel R, Eilbacher B, Wilke R. Memantine-induced dopamine release in the prefrontal cortex and striatum of the rat – a pharmacokinetic microdialysis study. Eur J Pharmacol. 1994;262(1–2):21–26. PubMed CrossRef
- van Wageningen H, Jørgensen HA, Specht K, et al. A 1H-MR spectroscopy study of changes in glutamate and glutamine (Glx) concentrations in frontal spectra after administration of memantine. Cereb Cortex. 2010;20(4):798–803. PubMed CrossRef
- Wenk GL, Parsons CG, Danysz W. Potential role of N-methyl-D-aspartate receptors as executors of neurodegeneration resulting from diverse insults: focus on memantine. Behav Pharmacol. 2006;17(5–6):411–424. PubMed CrossRef
- Wu HM, Tzeng NS, Qian L, et al. Novel neuroprotective mechanisms of memantine: increase in neurotrophic factor release from astroglia and anti-inflammation by preventing microglial activation. Neuropsychopharmacology. 2009;34(10):2344–2357. PubMed CrossRef
- Zheng W, Zhu XM, Zhang QE, et al. Adjunctive memantine for major mental disorders: a systematic review and meta-analysis of randomized double-blind controlled trials. Schizophr Res. 2019;209:12–21. PubMed CrossRef
- Hosenbocus S, Chahal R. Memantine: a review of possible uses in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2013;22(2):166–171. PubMed
- Abdi Dezfouli R, Akbariforoud S, Esmaeilidezfouli E. Are there links between Alzheimer’s disease and ADHD? The efficacy of acetylcholinesterase inhibitors and NMDA receptor antagonists in controlling ADHD symptoms: a systematic review. Middle East Curr Psychiatr. 2024;31:13.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
- Kishi T, Matsunaga S, Oya K, et al. Memantine for Alzheimer’s disease: an updated systematic review and meta-analysis. J Alzheimers Dis. 2017;60(2):401–425. PubMed CrossRef
- Turalde CWR, Espiritu AI, Anlacan VMM. Memantine for multiple sclerosis: a systematic review and meta-analysis of randomized trials. Front Neurol. 2021;11:574748. PubMed
- Adler L, Kessler RC, Spencer T. Adult ADHD Self-Report Scale-v1. 1 (ASRS-v1. 1) Symptom Checklist. World Health Organization; 2003.
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. PubMed CrossRef
- Findling RL, McNamara NK, Stansbrey RJ, et al. A pilot evaluation of the safety, tolerability, pharmacokinetics, and effectiveness of memantine in pediatric patients with attention-deficit/hyperactivity disorder combined type. J Child Adolesc Psychopharmacol. 2007;17(1):19–33. PubMed CrossRef
- Mohammadi MR, Mohammadzadeh S, Akhondzadeh S. Memantine versus methylphenidate in children and adolescents with attention deficit hyperactivity disorder: a double-blind, randomized clinical trial. Iran J Psychiatry. 2015;10(2):106–114.
- Riahi F, Tashakori A, Enayatollahi M. Comparison of the effects of different doses of memantine in combination with methylphenidate in children affected by ADHD. Arch Psychiatr Psych. 2020;22(4):32–39.
- Biederman J, Fried R, Tarko L, et al. Memantine in the treatment of executive function deficits in adults with ADHD: a pilot-randomized double-blind controlled clinical trial. J Atten Disord. 2017;21(4):343–352.
- Mohammadzadeh S, Ahangari TK, Yousefi F. The effect of memantine in adult patients with attention deficit hyperactivity disorder. Hum Psychopharmacol. 2019;34(1):e2687. PubMed CrossRef
- Surman CBH, Hammerness PG, Petty C, et al. A pilot open label prospective study of memantine monotherapy in adults with ADHD. World J Biol Psychiatry. 2013;14(4):291–298. PubMed CrossRef
- Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and Lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. PubMed CrossRef
- DuPaul GJ, Power TJ, Anastopoulos AD, et al. ADHD Rating Scale—IV: Checklists, Norms, and Clinical Interpretation. The Guilford Press; 1998.
- Guy W. ECDEU Assessment Manual for Psychopharmacology. US Department of Health, Education, and Welfare, Public Health Service; 1976.
- Dunn LM, Dunn LM. Peabody picture vocabulary test. 1965.
- Conners CK, Sitarenios G, Parker JDA, et al. The revised Conners’ Parent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol. 1998;26:257–268. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association; 1994.
- Spencer TJ, Adler LA, Meihua Q, et al. Validation of the adult ADHD investigator symptom rating scale (AISRS). J Atten Disord. 2009;14(1):57–68.
- Roth RM, Gioia GA, Isquith PK. BRIEF-A: Behavior Rating Inventory of Executive Function—Adult Version. Psychological Assessment Resources; 2005.
- Robbins TW, James M, Owen AM, et al. A study of performance on tests from the CANTAB battery sensitive to frontal lobe dysfunction in a large sample of normal volunteers: implications for theories of executive functioning and cognitive aging. Cambridge Neuropsychological Test Automated Battery. J Int Neuropsychol Soc. 1998;4(5):474–490. PubMed CrossRef
- Conners CK, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales. PsycTESTS Dataset; 2012.
- Kooij J, Francken MH. DIVA 2.0. Diagnostic Interview Voor ADHD in Adults bij volwassenen [DIVA 20 Diagnostic Interview ADHD in Adults]. DIVA Foundation; 2010. http://www.divacenter.eu/DIVA.aspx.
- Thomas SJ, Grossberg GT. Memantine: a review of studies into its safety and efficacy in treating Alzheimer’s disease and other dementias. Clin Interv Aging. 2009;4:367–377. PubMed CrossRef
- Bouhadoun S, Poulin C, Berrahmoune S, et al. A retrospective analysis of memantine use in a pediatric neurology clinic. Brain Dev. 2021;43(10):997–1003.
- Aman MG, Findling RL, Hardan AY, et al. Safety and efficacy of memantine in children with autism: randomized, placebo-controlled study and open-label extension. J Child Adolesc Psychopharmacol. 2017;27(5):403–412.
- Soorya LV, Fogg L, Ocampo E, et al. Neurocognitive outcomes from memantine: a pilot, double-blind, placebo-controlled trial in children with autism spectrum disorder. J Child Adolesc Psychopharmacol. 2021;31(7):475–484.
- Elnaiem W, Benmelouka AY, Elgendy AMN, et al. Evaluation of memantine’s efficacy and safety in the treatment of children with autism spectrum disorder: a systematic review and meta-analysis. Hum Psychopharmacol. 2022;37(5):e2841. PubMed CrossRef
- Erickson CA, Posey DJ, Stigler KA, et al. A retrospective study of memantine in children and adolescents with pervasive developmental disorders. Psychopharmacology (Berl). 2007;191(1):141–147. PubMed CrossRef
- Owley T, Salt J, Guter S, et al. AProspective, open-label trial of memantine in the treatment of cognitive, behavioral, and memory dysfunction in pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2006;16(5):517–524. PubMed CrossRef
- Ma HM, Zafonte RD. Amantadine and memantine: a comprehensive review for acquired brain injury. Brain Inj. 2020;34(3):299–315. PubMed CrossRef
- Karimi Tari P, Parsons CG, Collingridge GL, et al. Memantine: updating a rare success story in pro-cognitive therapeutics. Neuropharmacology. 2024;244:109737. PubMed
- Seeman P, Caruso C, Lasaga M. Memantine agonist action at dopamine D2High receptors. Synapse. 2008;62(2):149–153. PubMed CrossRef
- Fusar-Poli P, Rubia K, Rossi G, et al. Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis. Am J Psychiatry. 2012;169(3):264–272. PubMed CrossRef
- Lou HC, Henriksen L, Bruhn P, et al. Striatal dysfunction in attention deficit and hyperkinetic disorder. Arch Neurol. 1989;46(1):48–52. PubMed CrossRef
- Scannell JW, Blanckley A, Boldon H, et al. Diagnosing the decline in pharmaceutical R&D efficiency. Nat Rev Drug Discov. 2012;11(3):191–200. PubMed CrossRef
- Lüscher Dias T, Schuch V, Beltrão-Braga PCB, et al. Drug repositioning for psychiatric and neurological disorders through a network medicine approach. Transl Psychiatry. 2020;10:141. PubMed CrossRef
- Okuyama R. Advancements in drug repurposing: examples in psychiatric medications. Int J Mol Sci. 2023;24(13):11000. PubMed
This PDF is free for all visitors!