Abstract
Objective: To evaluate weight change with a combination of olanzapine and samidorphan (OLZ/SAM) versus olanzapine by pooling data across clinical studies.
Methods: This study was an individual patient data (IPD) meta-analysis of clinical trial data.
Data Sources and Study Selection: EMBASE, MEDLINE, and PsycInfo were searched for randomized clinical trials (≥12 weeks) in adults with schizophrenia or bipolar I disorder in which weight change from baseline was the primary or secondary end point. Search results were reviewed for eligible studies.
Participants: Patients receiving daily OLZ/SAM (olanzapine 5–20 mg + samidorphan 10 mg) or olanzapine (5–20 mg) who underwent ≥1 postbaseline weight assessment by week 12 were included.
Outcomes: The primary outcome was percent change in body weight at week 12. Secondary outcomes were proportions of patients with ≥7% or ≥10% weight gain from baseline at week 12.
Results: Overall, 1063 patients from 3 studies conducted between June 2013 and December 2021 were analyzed. At week 12, OLZ/SAM treatment was associated with a lower least squares mean (LSM) percent change in body weight from baseline (3.68%) vs olanzapine (5.43%) (LSM [SE] difference=−1.75% [.41]; 95% CI, −2.55 to −0.94). Fewer patients treated with OLZ/SAM gained ≥7% (23.9% vs 34.6%; odds ratio [OR] = 0.58; 95% CI, 0.043–0.79) or ≥10% (13.7% vs 20.4%; OR = 0.60; 95% CI, 0.42–0.88) of their baseline body weight at week 12.
Conclusion: In this IPD meta-analysis, OLZ/SAM treatment was associated with less weight gain and reduced risk of reaching ≥7% or ≥10% gain in body weight versus olanzapine over 12 weeks.
J Clin Psychiatry 2025;86(1):24m15526
Author affiliations are listed at the end of this article.
Schizophrenia and bipolar I disorder (BD-I) are mental health conditions associated with severe symptoms, physical and psychiatric comorbidities, and functional impairments in daily living tasks.1–5 Olanzapine is an antipsychotic medication that has established antipsychotic efficacy for the treatment of schizophrenia and BD-I.6,7 In 2 previously conducted comparative antipsychotic effectiveness trials that enrolled patients with first-episode (12-month randomized open-label trial) or chronic (18-month randomized double-blind trial) schizophrenia, patients treated with olanzapine had the lowest rates of all-cause discontinuation.8,9 In a 5-study meta-analysis10 of patients with BD-I and acute mania, olanzapine treatment significantly reduced symptoms compared with placebo, with the largest effect size for patients with the most severe symptoms at baseline.
Despite its established efficacy in patients with schizophrenia or BD-I, olanzapine’s associated weight gain and potential for causing metabolic abnormalities have thus far limited its clinical use.9,11,12 In clinical studies, a significant proportion of patients treated with olanzapine monotherapy experience clinically significant weight gain (defined as >7% increase from baseline), with rates as high as 86% in those with first-episode psychosis and 30% in those with chronic schizophrenia.8,9 The risk of weight gain with olanzapine is generally dose dependent, with higher doses often associated with a greater likelihood of weight gain.13,14
The combination of olanzapine and samidorphan (OLZ/SAM) is approved in the United States for the treatment of adults with schizophrenia or BD-I.15 This combination product provides the well-known and established antipsychotic efficacy of olanzapine while mitigating olanzapine-associated weight gain with the addition of samidorphan. Samidorphan acts as a µ- opioid receptor antagonist and a partial δ- and κ-opioid receptor agonist.16 In clinical trials, OLZ/SAM has been consistently associated with efficacy similar to that of olanzapine but with less weight gain.17–19 However, previous attempts at estimating the weight-mitigation benefit of OLZ/SAM have been limited by methodological shortcomings.20–22
The objective of this analysis was to evaluate the weight change profile of OLZ/SAM versus olanzapine using individual patient data (IPD) and meta-analytic techniques. The IPD meta-analysis approach has several advantages over aggregate data meta-analysis, such as checking data in detail, standardizing outcomes across studies, and increasing statistical power to detect treatment effects.23,24 The weight change profile of OLZ/SAM versus olanzapine was assessed in patients with schizophrenia or BD-I who participated in clinical trials of ≥12 weeks’ duration in which weight change was measured as a primary or secondary study end point.
METHODS
Protocol and Registration
All procedures for this IPD meta-analysis were in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines for IPD.25 The PRISMA checklist is included as Supplementary Table 1. All analytic methods, study objectives, end points, and patient inclusion criteria were prespecified and documented in a statistical analysis plan for the study. The plan was finalized in November 2022.
Information Sources and Search Strategy
A systematic literature search was conducted through August 23, 2024, in the EMBASE, MEDLINE, and PsycInfo databases. The following search strategy was used for EMBASE and MEDLINE: (olanzapine) AND (samidorphan) AND (random* OR placebo) [all fields + text]. The search string for PsycInfo was (olanzapine AND samidorphan AND (random* OR placebo)).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures, MESH word]. The search was not restricted by language or publication date.
Eligibility Criteria
Eligible studies for this IPD meta-analysis were randomized double-blind studies of OLZ/SAM vs olanzapine ≥12 weeks’ duration in which weight change was measured as a primary or secondary study end point. Inclusion criteria were predetermined in the study plan.
Study Selection
The systematic literature search and initial review for relevance were conducted by medical staff (Omar H. Cabrera and Noud van Helmond). Individual articles were screened by title and abstract for eligibility. M.J.D. and D.M. confirmed the potential eligibility of articles. Full-text articles were reviewed for potentially relevant studies to determine if the report met eligibility criteria.
Risk of Bias in Individual Studies
Included studies were assessed for methodological quality by M.J.D. using the Cochrane Collaboration’s RoB 2 tool for assessing the risk of bias.26
Individual Patient Data
Patients aged ≥18 years and meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, or Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for schizophrenia or BD-I were eligible.27,28 Only patients receiving daily OLZ/SAM (olanzapine 5–20 mg + samidorphan 10 mg, doses approved by the US Food and Drug Administration [FDA]) or olanzapine (5–20 mg) who underwent ≥1 postbaseline weight assessment by week 12 were included. Data from patients taking a non–FDA-approved fixed-dose OLZ/SAM combination containing 5 or 20 mg of samidorphan were excluded.
Assessments
The primary outcome was the percent change from baseline body weight at week 12. Secondary outcomes included the proportions of patients with clinically significant weight gain of ≥7% or ≥10% from baseline at week 12. Percent change from baseline body weight and the clinically significant weight gain thresholds of ≥7% and ≥10% were chosen because they are common end points in studies of weight gain associated with antipsychotic treatment.9,29–31
Additional assessments at week 12 included the overall mean change in weight from baseline. Subgroup analyses assessed percent change from baseline body weight based on various demographic categories (eg, age <30 or ≥30 years, male or female sex, Black or non-Black race, body mass index [BMI] <25 or ≥25 kg/m2, US or non-US region). Adverse event (AE) rates and metabolic parameter changes were evaluated also. Changes in disease severity were assessed by using the Clinical Global Impressions–Severity of Illness (CGI-S) score. All outcomes were prespecified and assessed at the IPD level.
Statistical Analysis
The primary outcome was analyzed using a 1-stage IPD random-effects model and a mixed model for repeated measures (MMRM) approach with percent change from baseline as the dependent variable. Treatment, visit, and treatment-by-visit interaction were categorical fixed effects (considered constant across studies), and study was a random effect. Baseline weight was included as a covariate.
The random-effects model assumes heterogeneity of the treatment effect between studies and that the observed variance is the sum of within-study and between-study components. The 1-stage approach was chosen because it more accurately models the statistical distribution of IPD.23 The analysis was performed on all observed postrandomization, on-treatment weight assessments, without imputation of missing data. Least squares mean (LSM) difference was calculated as the measure of effect size, along with 95% CIs.
The proportions of patients who experienced clinically significant weight gain were analyzed using a generalized linear mixed model using ≥7% or ≥10% weight gain as a dependent variable; treatment, visit, and treatment-by- visit interaction as categorical fixed effects; study as a random effect; and baseline weight as a covariate. Odds ratios (ORs) and 95% CIs were calculated.
For the subgroup analyses by age, sex, race, BMI, and region, treatment effects and 95% CIs were calculated. The numbers and percentages of all randomized patients who received ≥1 dose of study drug in the primary clinical trial and reported an AE during the double-blind treatment period (week 12/week 13), including those for AEs that led to treatment discontinuation, serious AEs, drug- related AEs, and deaths, are provided. Descriptive statistics and changes from baseline values at week 12 (with a ±10-day window) are presented by treatment group (OLZ/SAM or olanzapine) for glycosylated hemoglobin (HbA1c), fasting blood glucose, total, low-density, and high- density lipoprotein cholesterol, and triglyceride levels. CGI-S scores of treated patients who underwent ≥1 postbaseline weight assessment by week 12 were also assessed.
Data analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and R version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Sensitivity Analyses
Prespecified sensitivity analyses were conducted using 1-stage and 2-stage IPD MMRM approaches to evaluate the consistency of the treatment effect. Therefore, study was a variable evaluated as both a random effect (assuming heterogeneity) and a fixed effect (assuming homogeneity). For the 1-stage approach, study was a fixed effect. For the 2-stage approach, 2 analyses were conducted: 1 with study as a random effect and 1 with study as a fixed effect. The 2- stage approach is similar to a standard meta-analysis on aggregate data. Thus, individual study estimates were calculated, plotted, and compared for similarities or differences. The estimates were then weighted and pooled using random or fixed effect methods. Between- study heterogeneity was evaluated in the 2-stage approach with I2, τ2, and Cochran Q P values.
RESULTS
Study Characteristics
A total of 111 records were retrieved across the 3 databases (EMBASE, n=77; MEDLINE, n=25; PsycInfo, n=9; Supplementary Figure 1). After removing 32 duplicates, there were 79 unique articles. Following title and abstract review, 68 articles were excluded for not meeting the eligibility criteria. Eleven articles were potentially eligible and underwent full-text review. Of these publications, 8 were excluded because they reported studies <12 weeks’ duration or were abstracts reporting on the results of a study that were later published in full.
After screening, the following 3 studies were eligible: a phase 2, 12-week efficacy and safety study in patients with schizophrenia (NCT01903837)17; a phase 3, 24- week pivotal weight study in patients with schizophrenia (NCT02694328)17,18; and a phase 3, 12-week study in patients with recent-onset schizophrenia, schizophreniform disorder, or BD-I (NCT03187769)19 (Supplementary Table 2).
All 3 studies were conducted between 2013 and 2021. In each study, eligible patients were required to have a BMI of ≤30 kg/m2. Patient data were maintained in internal databases belonging to Alkermes, Inc., and were checked for completeness.
Population Characteristics
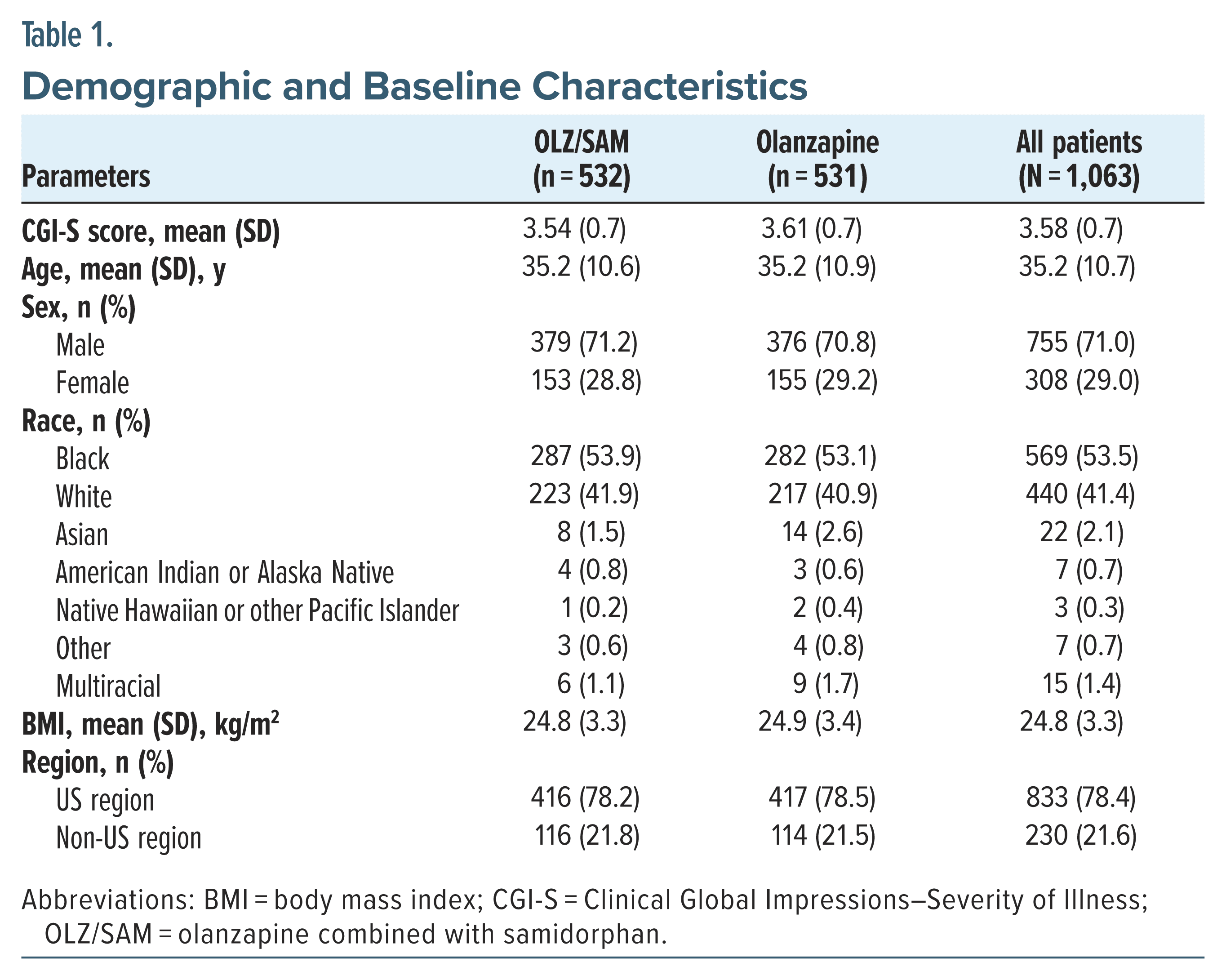
Of the 1336 patients randomized in the 3 studies, 1063 (80%) met inclusion criteria and underwent ≥1 postbaseline weight assessment by week 12 (NCT01903837, n=161; NCT02694328, n=538; NCT03187769, n=364). The baseline mean (SD) age was 35.2 (10.7) years, 755 (71%) patients were male, 569 (54%) patients were Black, and the mean (SD) BMI was 24.8 (3.3) kg/m2. Overall, 833 (78%) patients were from the United States (Table 1).
Patient characteristics were similar between the OLZ/SAM and olanzapine groups, with baseline mean (SD) ages of 35.2 (10.6) and 35.2 (10.9) years, respectively. Most patients in the OLZ/SAM and olanzapine cohorts were male (379 [71%] and 376 [71%], respectively) and Black (287 [54%] and 282 [53%], respectively). The baseline mean (SD) BMIs were 24.8 (3.3) kg/m2 for the OLZ/SAM group and 24.9 (3.4) kg/m2 for the olanzapine group. Overall, 416 (78%) patients in the OLZ/SAM group and 417 (79%) in the olanzapine group were from the United States.
Risk-of-Bias Assessment
The overall risk of bias was low for all studies assessing the weight change profile of OLZ/SAM versus olanzapine. There were some concerns about bias due to missing outcome data for one study17 because multiple imputation was not performed on the weight outcome. However, the overall risk of bias in this study was low, and it was included in the sensitivity analyses. The results of the risk-of-bias assessment are reported in Supplementary Table 3. No data integrity issues were identified in a review of the IPD.
Weight Change From Baseline
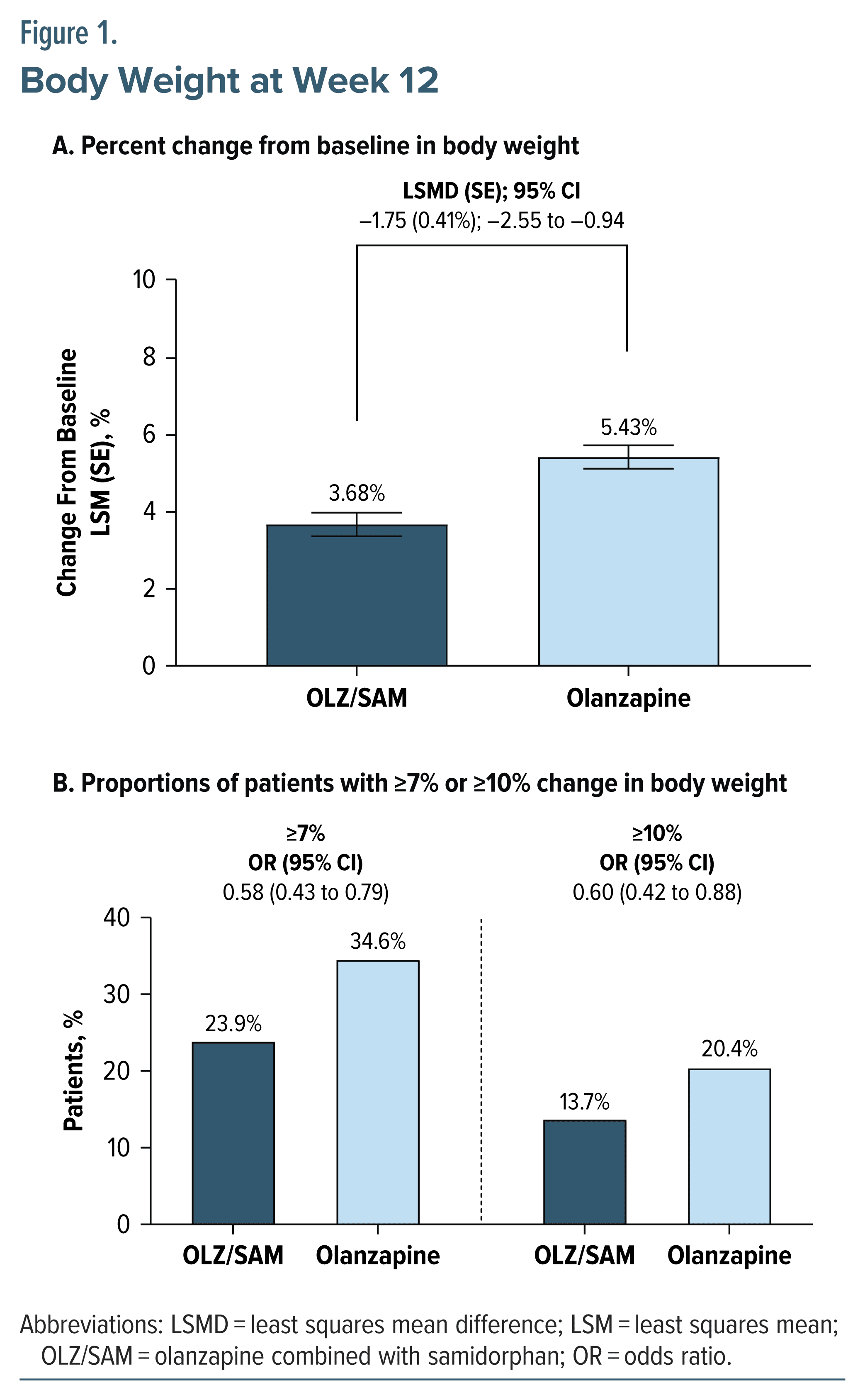
At week 12, treatment with OLZ/SAM was associated with a lower LSM percent change from baseline in body weight (3.68%) compared with olanzapine treatment (5.43%) (LSM [SE] difference = −1.75% [0.41%]; 95% CI, −2.55 to −0.94) (Figure 1). The LSM (SE) change from baseline in weight at week 12 was 2.63 (0.22) kg for the OLZ/SAM group and 3.96 (0.22) kg for the olanzapine group (LSM [SE] difference = −1.33 [0.30] kg; 95% CI, −1.92 to −0.75).
Fewer patients treated with OLZ/SAM (23.9%) than those treated with olanzapine (34.6%) gained ≥7% of their respective baseline body weight at week 12. The OR (95% CI) for attaining a ≥7% increase in body weight from baseline with OLZ/SAM vs olanzapine was 0.58 (0.43–0.79) (Figure 1). Fewer patients treated with OLZ/SAM (13.7%) than those treated with olanzapine (20.4%) had gained ≥10% of their respective baseline body weight at week 12. The OR (95% CI) for attaining a ≥10% increase in body weight from baseline with OLZ/SAM vs olanzapine was 0.60 (0.42–0.88) (Figure 1).
Subgroup Analyses
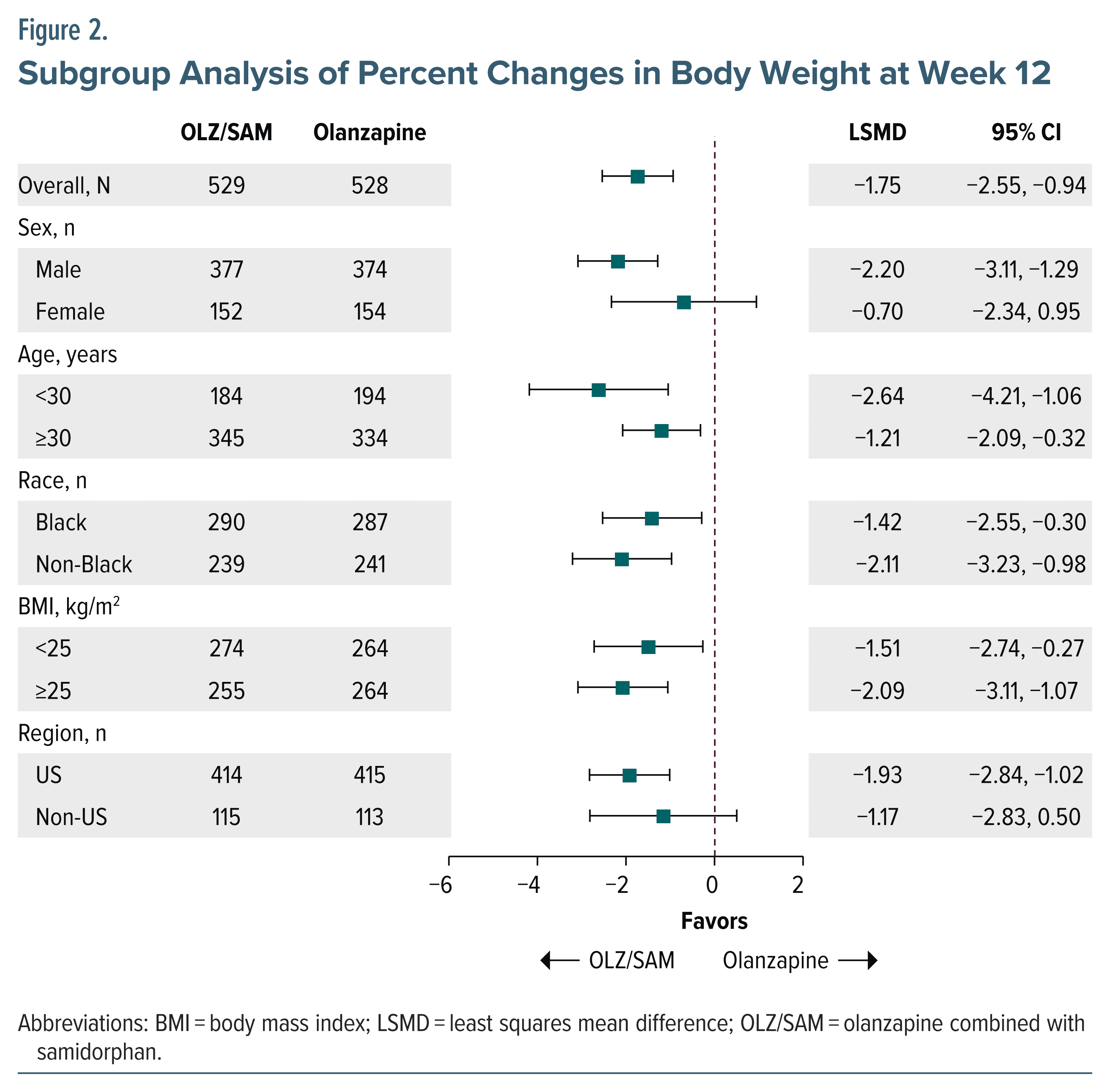
Numerically, OLZ/SAM resulted in a lower percent change in body weight across all subgroups examined, including by age, sex, race, BMI, and region (Figure 2).
Safety
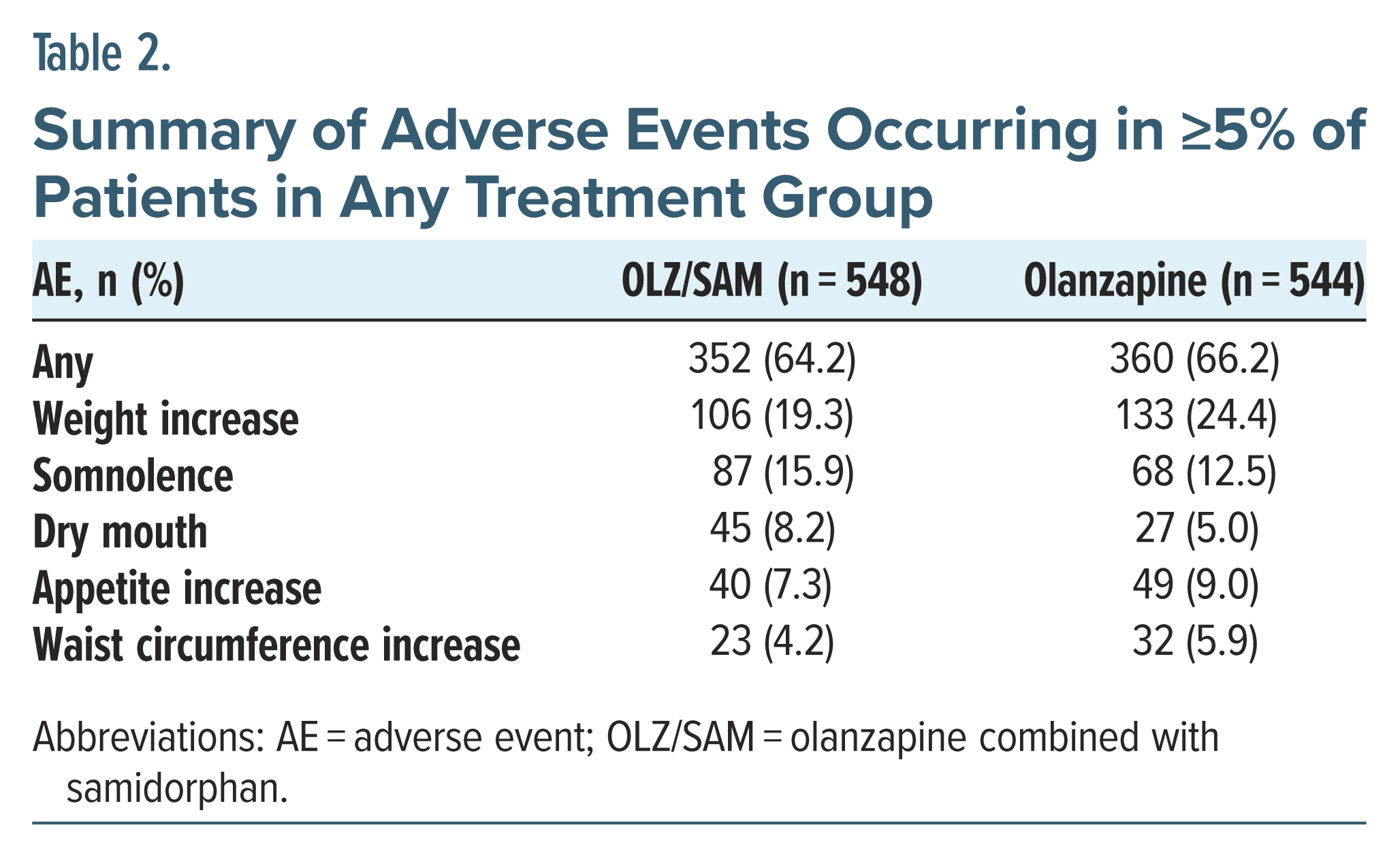
The proportions of patients with any AE(s) were similar between the OLZ/SAM and olanzapine groups, with 64% and 66%, respectively, experiencing at least 1 AE (Table 2). The most common AE was weight increase, which occurred in 19% of the patients receiving OLZ/SAM and 24% of those receiving olanzapine. Other AEs occurring in ≥5% of patients included somnolence, dry mouth, increased appetite, and waist circumference increase, which is consistent with the known AE profiles of olanzapine and OLZ/SAM.
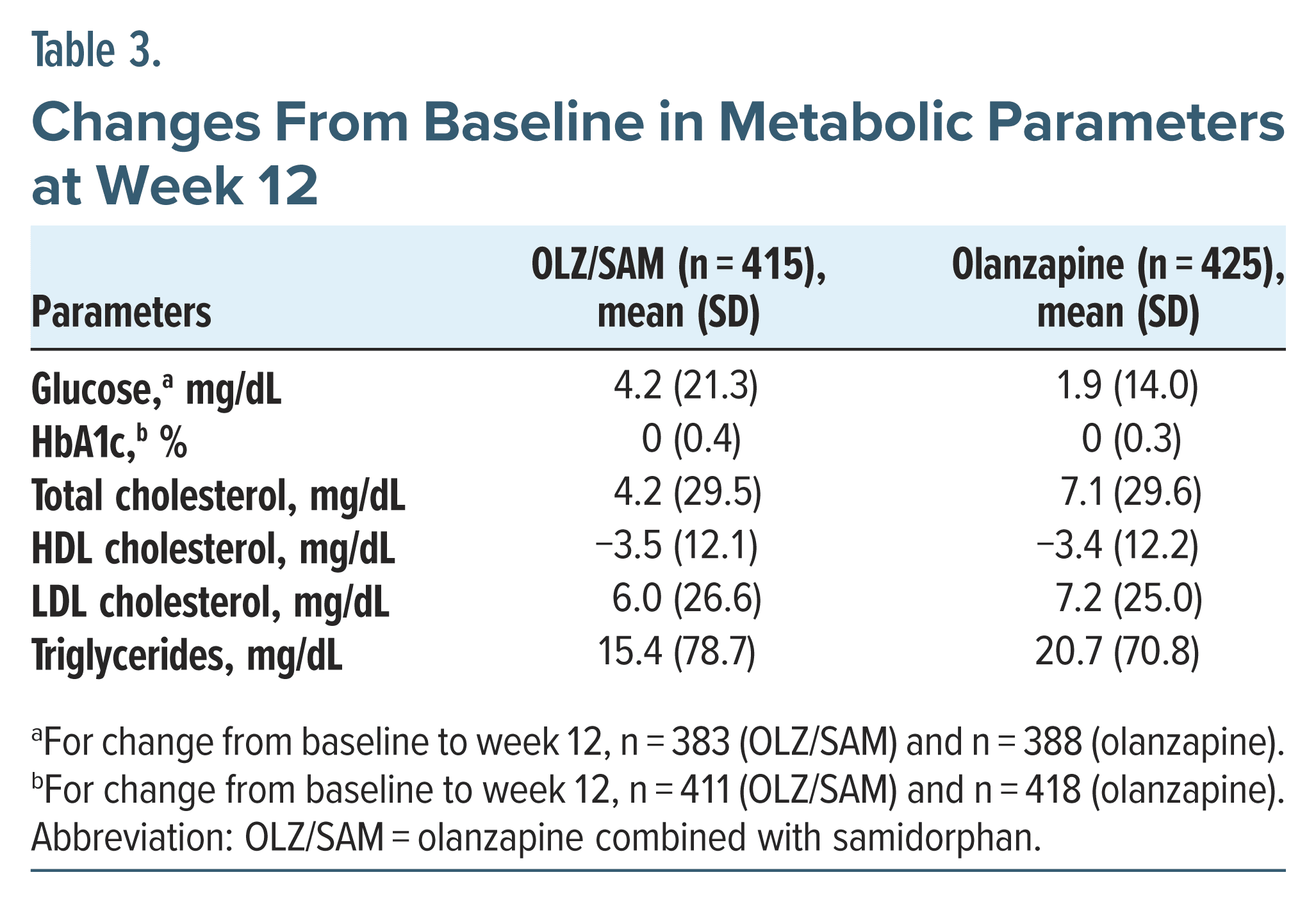
Metabolic Parameters
Changes in metabolic parameters were small and similar between the OLZ/SAM and olanzapine groups at week 12 (Table 3), despite the differential effects on weight that were observed. Mean (SD) blood glucose concentrations increased by 4.17 (21.3) mg/dL in the OLZ/SAM group and 1.93 (14.0) mg/dL in the olanzapine group at week 12. No relevant mean changes in HbA1c levels were observed. A mean (SD) increase in total cholesterol level was noted in both groups at week 12 (OLZ/SAM, 4.23 [29.5] mg/dL; olanzapine, 7.11 [29.6] mg/dL), with similar decreases in high- density lipoprotein cholesterol level and increases in low-density lipoprotein cholesterol level in both groups. Mean (SD) triglyceride levels increased by 15.38 (78.7) mg/dL in the OLZ/SAM group and 20.70 (70.8) mg/dL in the olanzapine group at week 12.
Assessment of Disease Severity
Mean (SD) baseline CGI-S scores were 3.54 (0.7) for OLZ/SAM and 3.61 (0.7) for olanzapine, indicating mild-to-moderate illness severity. Mean (SD) changes from baseline at week 12 in CGI-S score were −0.41 (0.7) for OLZ/SAM and −0.42 (0.7) for olanzapine.
Assessment of Sensitivity Analyses
The results of the sensitivity analysis using the 1- stage approach with study as a fixed effect were similar to those of the primary analysis. Treatment with OLZ/SAM was associated with a lower LSM percent change from baseline in body weight than treatment with olanzapine (LSM [SE] difference=−1.75% [0.41%]; 95% CI, −2.55 to −0.94). Similar results were obtained using the 2-stage approach with study as a random or fixed effect. Treatment with OLZ/SAM was associated with a lower LSM percent change from baseline than was treatment with olanzapine (LSM [SE] difference=−1.52% [0.29%]; 95% CI, −2.08 to −0.95) (Supplementary Figure 2). Measures of between-study heterogeneity suggested that the studies were similar enough in terms of design, population, and treatment effect to pool for meta-analysis.
DISCUSSION
In this IPD meta-analysis of 3 clinical trials, treatment with OLZ/SAM resulted in significantly less weight gain than treatment with olanzapine after 12 weeks. Results consistently favored OLZ/SAM for the outcome of percent change in weight and for the risk of experiencing clinically significant weight gain of ≥7% or ≥10%. In addition, OLZ/SAM resulted in lower mean changes in weight from baseline. On average, patients treated with OLZ/SAM gained about 3 pounds less over 3 months than those treated with olanzapine. Also, OLZ/SAM was associated with lower mean percent changes in body weight across all subgroups examined. These results suggest that OLZ/SAM may consistently mitigate olanzapine-associated weight gain across different patient populations.
This study was the first to generate estimates of the weight-mitigating benefit of OLZ/SAM across similarly designed clinical trials and had several advantages over previous attempts.20–22 Studies included in this analysis were of sufficient duration (≥12 weeks) to detect differences in weight gain between the OLZ/SAM and olanzapine groups.18,19 In each study, the weight trajectories of patients taking OLZ/SAM and those taking olanzapine were similar for the first 4–6 weeks of treatment but diverged thereafter. Weight stabilized for patients on OLZ/SAM, while weight gain continued for patients on olanzapine.18,19 Previous attempts to estimate the weight-mitigating effect of OLZ/SAM included studies that were only 3 or 4 weeks in duration, a time frame too short to determine the differential weight gain effect of OLZ/SAM versus olanzapine accurately.32,33 Indeed, the “real-world” weight-mitigation benefit associated with OLZ/SAM may be even more pronounced over longer treatment durations given that weight gain plateaus within a few weeks after starting OLZ/SAM treatment but continues with olanzapine.17–19 Another advantage of this study is that IPD were used to calculate weight estimates, whereas previous studies have relied on published, aggregated data.20–22 Furthermore, only data from patients receiving an FDA-approved dose of OLZ/SAM (olanzapine 5–20 mg + samidorphan 10 mg) were assessed.34 Other doses of OLZ/SAM are not relevant because they are not available for clinical use.35 The adequacy of the IPD meta- analysis methodology enabled additional assessments of AEs, metabolic parameters, and the antipsychotic efficacy of OLZ/SAM across clinical trials.
The proportions of patients experiencing AEs were similar in the OLZ/SAM and olanzapine groups, and the most common AEs reported were consistent with the known profiles of olanzapine and OLZ/SAM. Both OLZ/SAM and olanzapine were associated with small and similar changes in metabolic parameters across 12 weeks, despite the differences observed in weight gain. However, the 12-week duration of treatment in this analysis may have been too short to detect changes in metabolic risk factors associated with weight gain that develop over longer periods of olanzapine exposure.36,37 Therefore, the observed results do not capture the longer-term health concerns, such as cardiometabolic changes, that may be associated with olanzapine use. In general, treatment with olanzapine has been associated with metabolic worsening and an increased risk of developing metabolic syndrome over time.37,38 In a post hoc analysis of the 24-week pivotal weight study,36 OLZ/SAM resulted in a significant reduction in the risks of metabolic syndrome and hypertension in patients free of those conditions at baseline. In addition, the small metabolic parameter changes observed in the 24-week study18 remained stable over an additional 52 weeks of open-label OLZ/SAM treatment.39 Furthermore, the weight-mitigation benefit observed with OLZ/SAM after 12 weeks of treatment appears to be durable, as changes in weight are small after OLZ/SAM treatment totaling up to 5.5 years.18,39,40
After 12 weeks of treatment, similar improvements in disease severity were observed in both the OLZ/SAM and olanzapine groups based on CGI-S scores. These results are consistent with those of another clinical trial in which OLZ/SAM treatment resulted in antipsychotic efficacy versus placebo that was comparable to that of olanzapine versus placebo.33
Limitations
Several limitations of this post hoc analysis should be considered. This IPD meta-analysis assessed only short- term effects of OLZ/SAM versus those of olanzapine after 12 weeks of treatment. The analysis was not designed to make statistical comparisons between OLZ/SAM and olanzapine regarding AEs, metabolic parameter changes (other than weight gain), or antipsychotic efficacy. Because 2 of the 3 studies included only patients with schizophrenia, relatively few patients with BD-I were available for analysis. Given that patients in the analysis were enrolled in a randomized clinical trial with relevant exclusion criteria, the results may not be generalizable to the larger population of patients with schizophrenia or BD-I. The CGI-S was used to assess changes in disease severity; antipsychotic efficacy was not evaluated. Last, the numbers of patients in some subgroups were relatively small, thus limiting the conclusions that can be drawn from subgroup analyses. Despite these limitations, however, this study was the first IPD meta-analysis of the 3 available clinical trials of sufficient duration to assess the weight-mitigating effect of OLZ/SAM on olanzapine-associated weight gain.
CONCLUSIONS
In this IPD meta-analysis of similarly designed studies that evaluated the effects of OLZ/SAM versus olanzapine on body weight as a primary or secondary study end point, treatment with OLZ/SAM was consistently associated with a lower percent weight gain, lower mean weight gain, and reduced risk of reaching the ≥7% or ≥10% threshold for clinically significant body weight gain versus treatment with olanzapine. In each study, weight mitigation with OLZ/SAM occurred after 4–6 weeks of treatment and body weight stabilized thereafter, whereas patients on olanzapine gained weight throughout the 12-week treatment window.
The reduction in percent weight gain with OLZ/ SAM was observed across all subgroups examined, suggesting that OLZ/SAM provides weight-gain mitigation advantages across different patient populations. Metabolic changes were small and similar between patients taking OLZ/SAM and those taking olanzapine. Similar CGI-S score improvements observed between treatments further support the observation that the weight gain–mitigating effect of OLZ/SAM does not negatively affect the therapeutic efficacy of olanzapine. As a whole, these findings highlight the consistency with which OLZ/SAM mitigates olanzapine-associated weight gain, an effect that has been reported across multiple independent studies. By mitigating olanzapine-associated weight gain, OLZ/SAM provides a treatment option for patients with schizophrenia or BD-I with less weight gain and the established efficacy of olanzapine. Future studies may further explore OLZ/SAM’s long-term benefits with respect to weight mitigation, disease improvement, and metabolic changes.
Article Information
Published Online: January 2, 2025. https://doi.org/10.4088/JCP.24m15526
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 18, 2024; accepted October 21, 2024.
To Cite: Correll CU, Doane MJ, McDonnell D, et al. Olanzapine/samidorphan effects on weight gain: an individual patient data meta-analysis of phase 2 and 3 randomized double-blind studies. J Clin Psychiatry. 2025;86(1):24m15526.
Author Affiliations: Department of Psychiatry, Zucker Hillside Hospital, Glen Oaks, New York (Correll); Department of Psychiatry and Molecular Medicine Hempstead, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York (Correll); Department of Child and Adolescent Psychiatry, Charité Universitätsmedizin, Berlin, Germany (Correll); Department of Health Economics and Outcomes Research, Alkermes, Inc., Waltham, Massachusetts (Doane); Department of Neuroscience, Alkermes Pharma Ireland Ltd., Dublin, Ireland (McDonnell); Department of Medical Strategy, Alkermes, Inc., Waltham, Massachusetts (Akerman); Division of Pharmacotherapy and Translational Science, College of Pharmacy, University of Texas at Austin, San Antonio, Texas (Saklad).
Corresponding Author: Michael J. Doane, PhD, Health Economics and Outcomes Research (HEOR), Alkermes, Inc., 900 Winter Street, Waltham, MA 02451-1420 ([email protected]).
Author Contributions: All authors had full access to the data and contributed to the drafting, critical review, and revision of the manuscript. All authors granted approval of the final manuscript for submission.
Relevant Financial Relationships: Dr Correll has been a consultant and/or advisor to or has received honoraria from AbbVie, Acadia, Adcock Ingram, Alkermes, Allergan, Angelini, Aristo, Biogen, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Denovo, Gedeon Richter, Hikma, Holmusk, Intra-Cellular Therapies, Jamjoom Pharma, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedinCell, Merck, MindPax, Mitsubishi Tanabe Pharma, Mylan, Neurelis, Neurocrine, Newron, Noven, Novo Nordisk, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Sage, Seqirus, SK Life Science, Sumitomo Pharma America, Sunovion, Sun Pharma, Supernus, Takeda, Teva, Tolmar, Vertex, and Viatris; provided expert testimony for Janssen and Otsuka; served on a data safety monitoring board for Compass Pathways, Denovo, Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received grant support from Janssen and Takeda; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Küleon Biosciences, LB Pharma, MindPax, and Quantic. Dr Doane is or was an employee of Alkermes, Inc., and may own stock/options in the company. Dr McDonnell is an employee of Alkermes Pharma Ireland Ltd. and may own stock/ options in the company. Dr Akerman was an employee and shareholder of Alkermes, Inc., at the time this study was conducted. Dr Saklad was an employee of The University of Texas at Austin College of Pharmacy; was appointed to the Texas Health and Human Services Commission, San Antonio State Hospital, and is on the faculty of the UT Health San Antonio Long School of Medicine; has served as consultant for Alkermes, Genomind, Janssen, Karuna, and Otsuka; has participated on the speakers’ bureau for Neurocrine, Otsuka PsychU, Teva, Texas Society of Health-System Pharmacists, and, on occasion, for several professional organizations; served on the Business Development Council for the American Association of Psychiatric Pharmacists; has served as expert witness on both defendant and plaintiff sides; and has no direct stock ownership in any pharmaceutical corporation.
Funding/Support: This study was sponsored by Alkermes, Inc., Waltham, MA.
Role of the Sponsor: This study was conducted by Alkermes, Inc., a pharmaceutical company that developed and markets OLZ/SAM, a combination of olanzapine and samidorphan for the treatment of adults with schizophrenia or bipolar I disorder, in the United States. Employees of Alkermes, Inc., were involved in the study design and data analyses. The authors interpreted the evidence and made the decision to submit the manuscript for publication.
Previous Presentations: Portions of this work were previously presented in a poster at American Society of Clinical Psychopharmacology Annual Meeting; May 30–June 2, 2023; Miami Beach, FL. Psych Congress 2023; September 6–10, 2023; Nashville, TN. 2023 Neuroscience Education Institute Congress; November 9–12, 2023; Colorado Springs, CO. American College of Neuropsychopharmacology Annual Meeting; December 3–6, 2023; Tampa, FL.
Acknowledgments: Medical writing and editorial support were provided by Rebecca Lane, PhD; Omar Cabrera, PhD; John H. Simmons, MD; and Noud van Helmond, MD, PhD, of Peloton Advantage, LLC, an OPEN Health company, and funded by Alkermes, Inc. The authors thank Meihua Wang, PhD, and Martin Dunbar, PhD, for their contributions to this study and data analysis, and Mark S. Todtenkopf, PhD, of Alkermes, Inc., who assisted in the preparation and proofreading of the manuscript.
Data Sharing Statement: The data collected in this study are proprietary to Alkermes, Inc. Alkermes, Inc. is committed to public sharing of data in accordance with applicable regulations and laws, and requests can be submitted to the corresponding author.
ORCID: Christoph U. Correll: https://orcid.org/0000-0002-7254-5646; Michael J. Doane: https://orcid.org/0009-0006-6102-2459; David McDonnell: https://orcid.org/0000-0002-6400-1286; Sarah Akerman: https://orcid.org/0000-0003-0866-5245; Stephen R. Saklad: https://orcid.org/0000-0002-6181-138X
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Previous reports estimating the weight-mitigation effect of a combination of olanzapine and samidorphan (OLZ/SAM) have had methodological shortcomings.
- In this individual patient data meta-analysis, treatment with OLZ/SAM was associated with less weight gain after 12 weeks compared with olanzapine.
- Similar changes in patients’ disease severity were observed between OLZ/SAM and olanzapine; changes in metabolic parameters were small and similar.
References (40)

- Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. 2011;6(9):e24597. PubMed CrossRef
- Goes FS. Diagnosis and management of bipolar disorders. BMJ. 2023;381:e073591. PubMed
- IsHak WW, Brown K, Aye SS, et al. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012;14(1):6–18 PubMed CrossRef
- Michalak EE, Yatham LN, Lam RW. Quality of life in bipolar disorder: a review of the literature. Health Qual Life Outcomes. 2005;3:72. PubMed CrossRef
- Pascual-Sánchez A, Jenaro C, Montes-Rodríguez JM. Quality of life in euthymic bipolar patients: a systematic review and meta-analysis. J Affect Disord. 2019;255:105–115. PubMed CrossRef
- Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–962. PubMed CrossRef
- Yildiz A, Nikodem M, Vieta E, et al. A network meta-analysis on comparative efficacy and all-cause discontinuation of antimanic treatments in acute bipolar mania. Psychol Med. 2015;45(2):299–317. PubMed CrossRef
- Kahn RS, Fleischhacker WW, Boter H, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085–1097. PubMed
- Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. PubMed
- Samara MT, Goldberg Y, Levine SZ, et al. Initial symptom severity of bipolar I disorder and the efficacy of olanzapine: a meta-analysis of individual participant data from five placebo-controlled studies. Lancet Psychiatry. 2017;4(11):859–867. PubMed CrossRef
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi- episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed CrossRef
- Correll CU, Højlund M, Graham C, et al. Weight gain and metabolic changes in patients with first-episode psychosis or early-phase schizophrenia treated with olanzapine: a meta-analysis. Int J Neuropsychopharmacol. 2023;26(7):451–464.
- Sabé M, Pallis K, Solmi M, et al. Comparative effects of 11 antipsychotics on weight gain and metabolic function in patients with acute schizophrenia: a dose- response meta-analysis. J Clin Psychiatry. 2023;84(2):22r14490. PubMed
- Spertus J, Horvitz-Lennon M, Abing H, et al. Risk of weight gain for specific antipsychotic drugs: a meta-analysis. NPJ Schizophr. 2018;4(1):12. PubMed CrossRef
- Zyprexa [Package Insert]. Eli Lilly and Company; 2021.
- Wentland MP, Lou R, Lu Q, et al. Syntheses of novel high affinity ligands for opioid receptors. Bioorg Med Chem Lett. 2009;19(8):2289–2294. PubMed CrossRef
- Martin WF, Correll CU, Weiden PJ, et al. Mitigation of olanzapine-induced weight gain with samidorphan, an opioid antagonist: a randomized double-blind phase 2 study in patients with schizophrenia. Am J Psychiatry. 2019;176(6):457–467. PubMed CrossRef
- Correll CU, Newcomer JW, Silverman B, et al. Effects of olanzapine combined with samidorphan on weight gain in schizophrenia: a 24-week phase 3 study. Am J Psychiatry. 2020;177(12):1168–1178. PubMed CrossRef
- Kahn RS, Kane JM, Correll CU, et al. Olanzapine/samidorphan in young adults with schizophrenia, schizophreniform disorder, or bipolar I disorder who are early in their illness: results of the randomized, controlled ENLIGHTEN-Early study. J Clin Psychiatry. 2023;84(3):22m14674. PubMed
- Srisurapanont M, Suttajit S, Likhitsathian S, et al. A meta-analysis comparing short-term weight and cardiometabolic changes between olanzapine/ samidorphan and olanzapine. Sci Rep. 2021;11(1):7583. PubMed
- Laguado SA, Saklad SR. Opioid antagonists to prevent olanzapine-induced weight gain: a systematic review. Ment Health Clin. 2022;12(4):254–262.
- Peng Z, Jia Q, Mao J, et al. Effects of combined therapy of olanzapine and samidorphan on safety and metabolic parameters in schizophrenia patients: a meta-analysis. Neuropsychiatr Dis Treat. 2023;19:2295–2308. PubMed
- Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36(5):855–875. PubMed CrossRef
- Stewart GB, Altman DG, Askie LM, et al. Statistical analysis of individual participant data meta-analyses: a comparison of methods and recommendations for practice. PLoS One. 2012;7(10):e46042. PubMed CrossRef
- Stewart LA, Clarke M, Rovers M, et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313(16):1657–1665. PubMed
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th ed, Text Revision. American Psychiatric Association; 2000.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. American Psychiatric Publishing; 2013.
- Blin O, Micallef J. Antipsychotic-associated weight gain and clinical outcome parameters. J Clin Psychiatry. 2001;62(Suppl 7):11–21.
- Fitzgerald I, Sahm LJ, Byrne A, et al. Predicting antipsychotic-induced weight gain in first episode psychosis - a field-wide systematic review and meta-analysis of non-genetic prognostic factors. Eur Psychiatry. 2023;66(1):e42.
- Wetterling T. Bodyweight gain with atypical antipsychotics. A comparative review. Drug Saf. 2001;24(1):59–73. PubMed CrossRef
- Silverman BL, Martin W, Memisoglu A, et al. A randomized, double-blind, placebo-controlled proof of concept study to evaluate samidorphan in the prevention of olanzapine-induced weight gain in healthy volunteers. Schizophr Res. 2018;195:245–251. PubMed CrossRef
- Potkin SG, Kunovac J, Silverman BL, et al. Efficacy and safety of a combination of olanzapine and samidorphan in adult patients with an acute exacerbation of schizophrenia: outcomes from the randomized, phase 3 ENLIGHTEN-1 study. J Clin Psychiatry. 2020;81(2):19m12769. PubMed
- Lybalvi [Package Insert]. Alkermes, Inc. 2023.
- Todtenkopf MS, Correll CU, Harris-White ME, et al. Comment on “Opioid antagonists to prevent olanzapine-induced weight gain: a systematic review”. Ment Health Clin. 2023;13(4):196–197.
- Correll CU, Stein E, Graham C, et al. Reduction in multiple cardiometabolic risk factors with combined olanzapine/samidorphan compared with olanzapine: post hoc analyses from a 24-week phase 3 study. Schizophr Bull. 2023;49(2):454–463.
- Pillinger T, McCutcheon RA, Vano L, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7(1):64–77. PubMed CrossRef
- De Hert M, Detraux J, van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2012;8(2):114–126.
- Kahn RS, Silverman BL, DiPetrillo L, et al. A phase 3, multicenter study to assess the 1-year safety and tolerability of a combination of olanzapine and samidorphan in patients with schizophrenia: results from the ENLIGHTEN-2 long-term extension. Schizophr Res. 2021;232:45–53.
- Ballon JS, Kahn RS, Arevalo C, et al. Long-term safety and efficacy of olanzapine/samidorphan: results of a 4-year open-label study [oral presentation]. Annu Schizophrenia International Research Society Conference; Florence, Italy; April 3-7, 2024.
This PDF is free for all visitors!