To the Editor: The perinatal period is a time of increased vulnerability for women to the onset or relapse for psychiatric disorders.1,2 Stressful life events during pregnancy, particularly obstetric complications (OC), are well-known risk factors for perinatal psychiatric disorders,3–5 such as depression and anxiety disorders.6,7 The literature remains incomplete regarding the association between OC and suicide attempts or other disorders, including substance use, posttraumatic stress, or eating disorders.
Our aims were (1) to determine the prevalence of OC in the United States and (2) to examine the associations between OC and psychiatric disorders during the perinatal period in adult US women.
Methods
We used cross-sectional data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) (N = 36,309; 60.1% response rate).8 This face-to-face survey was conducted in 2012–2013 and included a nationally representative sample of civilian, noninstitutionalized US adults aged 18 years and older.8
The analysis focused on women of childbearing age (18–50 years old) who responded affirmatively to the question, “Were you pregnant at any time during the last year?” defining the perinatal period as in previous work.6,9 We used a single question to determine the presence of OC, consistent with previous studies.6,9 Psychiatric disorders in the past 12 months and lifetime were assessed using a structured interview (the Alcohol Use Disorder and Associated Disabilities Interview Schedule-5) to assess all current psychiatric disorders in the perinatal period. Among them, we determined psychiatric disorders with perinatal onset (for women with no previous history).8 Data were reported for mood disorders (including major depressive disorder, bipolar disorder, and dysthymia), anxiety disorders (including panic disorder, social phobia, specific phobia, and generalized anxiety disorder [GAD]), posttraumatic stress disorder (PTSD), eating disorder (including anorexia, bulimia, and binge), history of suicide attempt, and substance use disorders (including alcohol, cannabis, stimulants, opioids, and tobacco).
Results
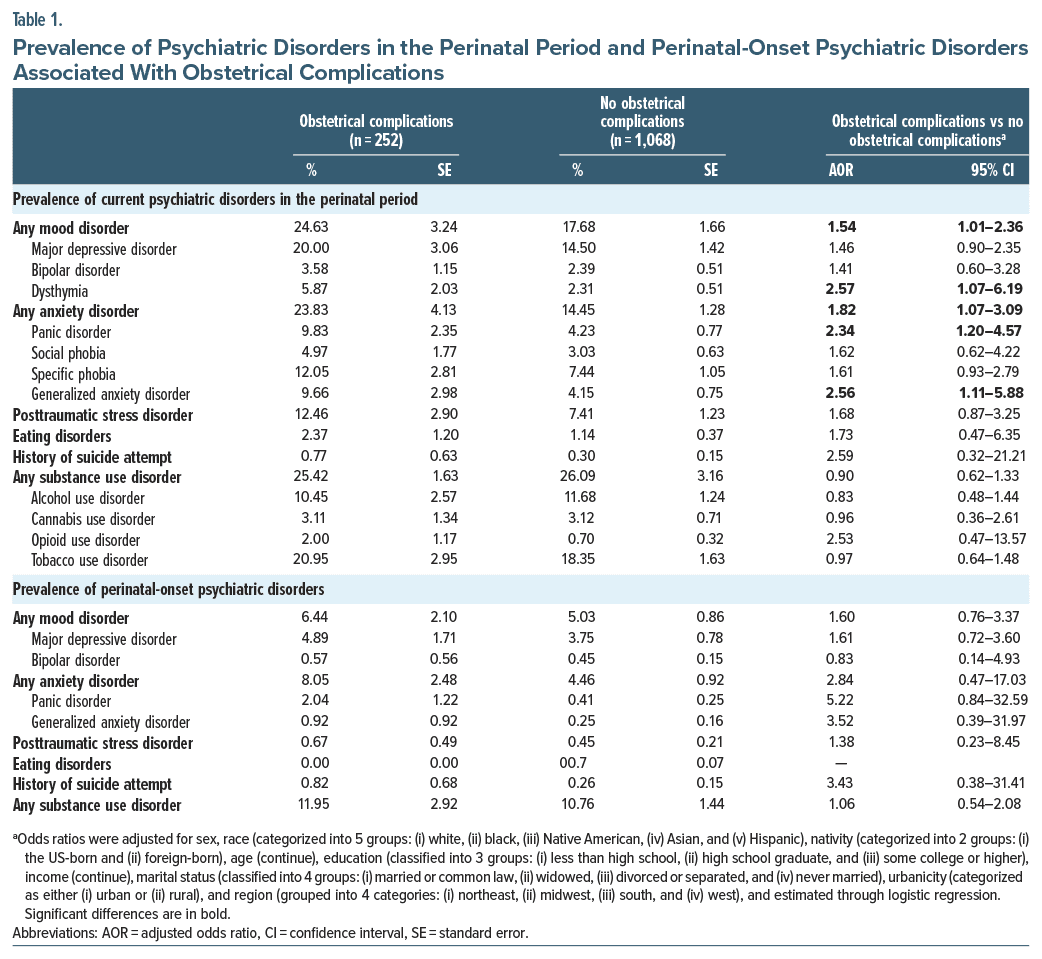
Of the 1,320 women in the perinatal period, 19.1% had OC. The presence of OC was associated with a significantly higher prevalence of current mood disorders (24.63% vs 17.68%, adjusted odds ratio [AOR] = 1.54, 95% CI, 1.01–2.36) and current anxiety disorders (23.83% vs 14.45%, AOR = 1.82, 95% CI, 1.07–3.09) during the perinatal period compared to women without OC, after adjustment for sociodemographic data (Table 1). In particular, OC were significantly associated with a 2-fold increased prevalence of current panic disorder and GAD during the perinatal period. There was no difference in the prevalence of current PTSD, eating and substance use disorders, and history of suicide attempt during the perinatal period between the 2 groups. For all psychiatric disorders, the prevalence of perinatal onset was not significantly different between women with and without OC.
Discussion
In this representative sample of the US population, 19.1% of peripartum women had OC, representing over 700,000 cases annually in the US population. OC are associated with a higher prevalence of mood and anxiety disorders in the perinatal period, consistent with previous research.6,10–12 Interestingly, our study found no significant association between perinatal-onset psychiatric disorders and OC. Women without a psychiatric history did not have a higher prevalence of perinatal psychiatric disorders when they experienced OC compared with women without OC. The risk of perinatal psychiatric disorders is particularly high in women with a history of psychiatric disorders.6 Therefore, women with a history of psychiatric disorders should be followed closely after undergoing OC. Although NESARC is 10 years old and was not designed to answer these questions (the definition of the perinatal period is broad and lacks details concerning OC), and while the cross-sectional design does not allow us to establish a causal relationship between the various psychiatric disorders and OC, these findings highlight the vulnerability of women with a psychiatric history, who need special support in the event of OC.13
Article Information
Published Online: May 27, 2024. https://doi.org/10.4088/JCP.23l15169
© 2024 Physicians Postgraduate Press, Inc.
J Clin Psychiatry 2024;85(2):23l15169
To Cite: Jacquelin M, Dubertret C, Ngameni EG, et al. Prevalence of psychiatric disorders in women with obstetric complications: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Clin Psychiatry. 2024;85(2):23l15169.
Author Affiliations: Université Paris Est Créteil (UPEC), Créteil, France (Jacquelin); Department of Psychiatry, Louis-Mourier Hospital, AP-HP, Colombes, France (Dubertret, Ngameni, Le Strat, Tebeka); Université Paris Cité, Faculty of Medicine, Paris, France (Dubertret, Le Strat, Tebeka); INSERM U1266, Centre for Psychiatry and Neurosciences, Paris, France (Dubertret, Le Strat, Tebeka); Department of Psychiatry, CHU Montpellier, Montpellier, France; IGF, University of Montpellier, CNRS, INSERM, Montpellier, France (Belzeaux).
Corresponding Author: Marine Jacquelin, MD, Université Paris Est Créteil (UPEC), 61 Ave du Général de Gaulle, 94000 Créteil, France ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: This research received no specific grant from any funding agency in the commercial or not for-profit sectors.
Disclaimer: This article does not reflect the opinions or views of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) or the US Government.
Tweetable Statement: Obstetrical complications are associated with a higher prevalence of mood and anxiety disorders during the perinatal period.
Ethical Standard: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Author Contributions: Dr Jacquelin drafted the initial manuscript and approved the final manuscript as submitted. Dr Tebeka carried out the initial analyses, revised the manuscript, and approved the final manuscript as submitted. Drs Dubertret, Ngameni, Belzeaux, and Le Strat significantly revised the manuscript and approved the final manuscript as submitted.
Acknowledgments: The authors are grateful to the NIAAA for providing the necessary data for this research. This article was prepared using a limited access data set obtained from the NIAAA.
References (13)

- Howard LM, Molyneaux E, Dennis CL, et al. Non psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775–1788. PubMed CrossRef
- Tebeka S, Le Strat Y, De Premorel Higgons A, et al. Prevalence and incidence of postpartum depression and environmental factors: the IGEDEPP cohort. J Psychiatr Res. 2021;138:366–374. PubMed CrossRef
- Blom EA, Jansen PW, Verhulst FC, et al. Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG. 2010;117(11):1390–1398. PubMed CrossRef
- Biaggi A, Conroy S, Pawlby S, et al. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. 2016;191:62–77. PubMed CrossRef
- Tebeka S, Le Strat Y, Mandelbrot L, et al. Early and late-onset postpartum depression exhibit distinct associated factors: the IGEDEPP prospective cohort study. BJOG. 2021;128(10):1683–1693. PubMed CrossRef
- Tebeka S, Le Strat Y, Dubertret C. Developmental trajectories of pregnant and postpartum depression in an epidemiologic survey. J Affect Disord. 2016;203:62–68. PubMed CrossRef
- Toscano M, Royzer R, Castillo D, et al. Prevalence of depression or anxiety during antepartum hospitalizations for obstetric complications: a systematic review and meta analysis. Obstet Gynecol. 2021;137(5):881–891. PubMed CrossRef
- Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. 2015;72(8):757–766. PubMed CrossRef
- Shamblaw AL, Sommer JL, Reynolds K, et al. Pregnancy and obstetric complications in women with a history of childhood maltreatment: results from a nationally representative sample. Gen Hosp Psychiatry. 2021;70:109–115. PubMed CrossRef
- Byatt N, Hicks-Courant K, Davidson A, et al. Depression and anxiety among high-risk obstetric inpatients. Gen Hosp Psychiatry. 2014;36(6):644–649. PubMed CrossRef
- Toscano M, Royzer R, Castillo D, et al. Prevalence of depression or anxiety during antepartum hospitalizations for obstetric complications: a systematic review and meta-analysis. Obstet Gynecol. 2021;137(5):881–891. PubMed CrossRef
- Landman A, Ngameni EG, Dubreucq M, et al.; IGEDEPP Group. Postpartum blues: a predictor of postpartum depression, from the IGEDEPP cohort. Eur Psychiatry. 2024;67(1):e30. PubMed CrossRef
- Hompoth EA, Pető Z, Fűrészné Balogh V, et al. Associations between depression symptoms, psychological intervention and perinatal complications. J Clin Psychol Med Settings. 2020;27(1):199–205. PubMed CrossRef
This PDF is free for all visitors!