Abstract
Objective: To assess the viewpoints of psychedelic practitioners in research settings on approaches to psychological support for psychedelic treatments.
Methods: An anonymous survey was distributed via email to contacts listed on ClinicalTrials.gov for clinical trials of psilocybin and LSD, personal contacts of authors, and through snowball sampling. The survey included Likert type, multiple choice, free response, and demographic items. Responses to survey items were coded to represent either emotive (emphasizing human and spiritual elements) or neuromodulatory (emphasizing biological drug effects) approaches to psychedelic treatment. Summative scores (“E-Scores”) were determined to quantitatively represent preferences. Data were collected from March 2023 to July 2023.
Results: Forty qualified respondents completed the survey. Respondents came from varying educational backgrounds (42.5% MD/DO and 57.5% other) and practiced in at least 4 countries, 11 U.S. states, and 16 institutions. Respondents had overseen a total of 1,656 psychedelic sessions (average = 41.4). There was a substantial range of response for many items (average range = 84.2% of maximum). Exploratory factor analysis identified 4 latent factors: The Importance of Trust, The Role of Spirituality, Creating an Emotional Setting, and Conceptualizing Negative Experiences. The average respondent held a slight preference for an emotive approach. Respondents who received training at the Multidisciplinary Association for Psychedelic Studies (MAPS) or the California Institute of Integral Studies (CIIS) had significantly greater emotive preference compared to other respondents (P < .05).
Conclusions: Among psychedelic researchers, there is no consensus on certain psychological support strategies for psychedelic treatments. There is an aggregate preference for an emotive approach to psychological support, which is higher among individuals receiving training at certain institutions.
J Clin Psychiatry 2025;86(1):24m15521
Author affiliations are listed at the end of this article.
Though most psychedelics have been Schedule I substances for over 50 years, limiting clinical research until the past two decades,1–4 multiple classical psychedelics—understood as chemical compounds causing psychoactive effects predominantly through 5-hydroxytryptamine 2A receptor agonism5–7—may be approved for general clinical use within years. Four organizations have received breakthrough therapy designations from the U.S. Food and Drug Administration (FDA) for classical psychedelic compounds to date.8–10 It is commonly believed that offering substantial psychological support and psychotherapy alongside the administration of these potent psychoactive compounds is crucial to the safety and efficacy of treatment,11 but the specifics of what this support should entail is an area of debate.12–19
During the first wave of research into psychedelics in the mid-20th century, lysergic acid diethylamide (LSD) was often characterized as a chemical agent with psychoactive properties that facilitated the process of psychotherapy.20–22 Within a psychoanalytic framework, LSD was deemed helpful for reducing ego defenses, allowing repressed memories to reach consciousness, and catalyzing the formation of psychological insight.20,21 Some providers administered low moderate doses and engaged in active discussion with long-term psychotherapy patients, described as psycholytic therapy.23 By contrast, others administered high doses with music or other environmental factors intended to promote transformative internal experiences in recipients, characterized as psychedelic therapy.22
Recent research has generally employed the psychedelic therapy model. Though specific approaches to psychological support or psychotherapy have varied across studies,1–3 certain core elements are commonly utilized, including monitoring by facilitators—typically including a licensed psychotherapist—who support participants before, during, and after dosing.1,24 More recently, approaches to psychological support have been manualized, especially for large-scale clinical trials.2,3,25 However, few studies have evaluated the relative risks and benefits of particular psychological support models, so the evidence base to confidently support certain practices over others is limited.1,26 Major phase 2 trials of psilocybin have not publicized manuals or detailed information about their psychological support methodologies.2,3
Numerous questions exist surrounding best practices for the provisioning of psychedelic compounds in medical settings. These include best practices for accompanying psychological support or psychotherapy,12,16,18,24,27 the role of the therapist or facilitator and their appropriate training,12,14,18,28 the use of physical touch in treatment,25,29 the incorporation of spiritual or religious ideas into the treatment model,17,19 the importance of the subjective experience and its characterization to recipients of treatment,30–34 and how use within secular medical settings should relate to ceremonial practices in other cultures, such as administration in group settings.35 The norms adopted surrounding administration of psychedelics will likely affect public perception of these drugs and their wider application in medical settings.
Despite an inherited tradition of the use of psychedelics in psychotherapy18 and evidence that supports the role of therapeutic relationships in treatment response,36 some commentators hypothesize that intrinsic neurobiological effects of psychedelics may be most relevant to the improvements observed in clinical trials13,37,38 or suspect that some form of core psychological support—but not psychotherapy, per se—is what is needed for treatment response.12 Conversely, other commentators suggest that insufficient psychotherapy may have contributed to worsened safety outcomes in a phase 2 trial of psilocybin for treatment resistant depression2,14 and that an overestimation of the importance of drug effects relative to psychosocial factors is a problem within the field generally.18,39 The outcome of this debate is important for any scaling up of the use of psychedelics as therapeutics, since accompanying psychosocial interventions may be crucial to the safety and efficacy of the treatment approach.14,15,18,40 Requirements about which providers may facilitate psychedelic treatment, and how many are needed, may impact treatment cost and accessibility.
Psychedelic compounds often induce highly meaningful psychological experiences,30,41 and increasing evidence supports that these contribute to therapeutic outcomes.30,41–44 Because subjective experiences elicited are affected by the psychosocial context of administration,40,45 it is likely to be challenging, if not impossible to isolate any intrinsic psychological effects of psychedelic drugs. Despite this, regulators have encouraged efforts to isolate the standalone effects of the drugs in clinical trials and have also recommended researchers justify the inclusion of psychotherapy in clinical trial design, with the rationale that this may contribute to undesired expectancy effects.46
One method of conceptualizing current tensions in the field of psychedelic psychiatry involves a novel conceptual axis created for this study, which ranges from emotive to neuromodulatory. Many current debates in the field of psychedelic psychiatry—such as the proper role of psychotherapy,12–15,18 spirituality,17,19,37,43 and physical touch in treatment29—could be understood through this broader conceptual framework.
An emotive approach aims to maximize the emotional salience of the psychedelic experience. Human and spiritual components of psychedelic treatments are highlighted, with the accompanying belief that these play key roles in therapeutic outcomes. Providers favoring an emotive approach may endorse various psychosocial methods for increasing the emotional salience of treatment, such as incorporating it within intensive psychotherapy,14,18,36 harnessing setting elements to promote the occurrence of mystical-type experiences,41,43 or employing physical touch to enhance feelings of connection during treatment.11,25
A neuromodulatory approach instead emphasizes the role of drug effects, in which the drug treatment is considered to be largely distinct and separable from accompanying psychosocial intervention, and the treatment functions predominantly through a biological rather than a psychological mechanism.12,13,37,47 Providers adopting components of this perspective may favor limiting the psychosocial involvement of providers to core elements of support needed for the safety of drug administration,12 place lesser emphasis on the relevance of the subjective experience to therapeutic effects,37 or have greater aversion to the promotion of spiritual experiences during treatment.17,19
This survey study characterizes the views of psychedelic practitioners in academic settings on topics pertaining to the therapeutic rationale for and clinical approach to treatment with classical psychedelics, using a quantitative analysis to identify the degree to which practitioners prefer emotive or neuromodulatory approaches to treatment. This is the first study to use these concepts to quantify the viewpoints of psychedelic practitioners on psychedelic treatments. In the setting of ongoing cultural and scientific dialogue surrounding how to evaluate and use these compounds, the perspectives of those with practical experience serve to further inform this discussion.
METHODS
Survey Design
Physician-researchers from Washington University and Johns Hopkins University developed the survey. Quantitative data collected included 28 6-point Likert-type items and 2 multiple-choice questions. The survey was divided into 3 subsections: demographic information, quantitative response, and qualitative/free response.
Response patterns were coded prior to data collection to represent emotive or neuromodulatory perspectives. Emotive and neuromodulatory poles were assigned to positions of agreement or disagreement on Likert-type survey items on the basis of consensus among survey designers. One Likert-type item (Supplementary Materials Appendix 1—Item 16) was not given these designations. Two multiple choice items with quantitative answers were also assigned emotive-neuromodulatory poles (Data Analysis). The existence of these poles was not conveyed on the survey.
Instructions were provided at the beginning of the survey. Respondents were instructed to answer survey items on the basis of individuals receiving psychedelic treatments in research or professional settings (Supplementary Materials Appendix 1). Demographics were limited to categories most relevant to characterizing the study population without compromising the anonymity of respondents. Participants had the option to provide their academic institution, location of residence, and information about prior training in psychedelic therapy. The survey was conducted anonymously to maximize response rates and minimize conformity bias.
The survey was created and distributed using REDCap database software.48,49
Participant Recruitment and Data Collection
Study staff recruited participants via email (Supplementary Materials Appendix 2). Potential participants were identified via 3 methods:ClinicalTrials.gov search, personal contacts of study authors, and snowball sampling. Email recipients were identified via ClinicalTrials.gov search from November 2022 to February 2023, and data were collected from March 2023 to July 2023 (Supplementary Methods). Though the determination of response rate is imprecise given the anonymous nature of the study and method of data collection, the estimated response rate range is 41.4%–100% (Supplementary Methods).
Since the survey was anonymous, no formal consent document was used. The Washington University in St. Louis Institutional Review Board approved this study.
Data Analysis
Data were converted from Likert-type responses to values 1–6. For the determination of reliability, calculation of E-Scores (see below), and exploratory factor analysis (EFA), responses in which agreement corresponded to the neuromodulatory pole were inverted, such that high values represented an emotive preference. For 2 multiple-choice items (Supplementary Appendix 1—29–30), responses were assigned a value of 1–6 such that higher recommended psychotherapy hours corresponded to emotive preference.
“E-Scores” are a normalized quantitative representation of the degree to which respondents prefer an emotive vs. neuromodulatory approach. Scores ranged from −1.0 to 1.0, with 1.0 representative of fully emotive preference and −1.0 fully neuromodulatory (Supplementary Methods). Measurements of reliability and EFA were used to further analyze the emotive/neuromodulatory constructs (Supplementary Methods). E-Scores were calculated for all items and latent factors.
Demographic questions and optional free-response items were used to determine academic degrees and prior psychedelic training (Supplementary Methods).
RESULTS
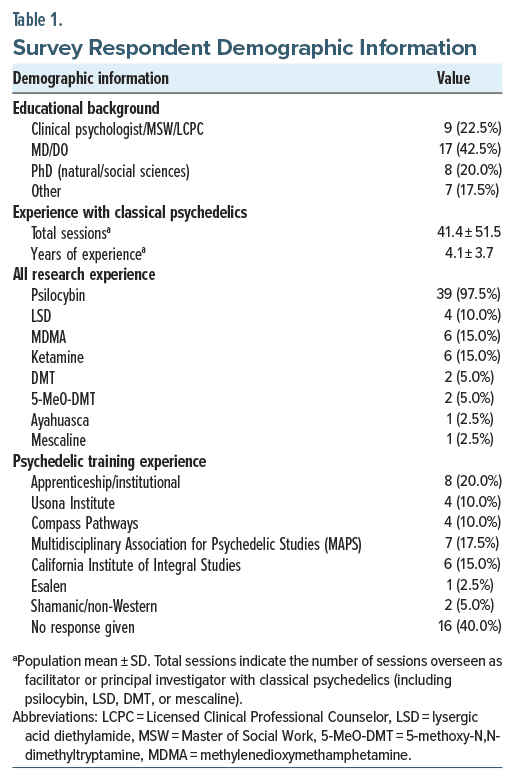
40 qualified respondents completed the survey. Almost all (39/40) respondents had worked with psilocybin, while fewer had worked with LSD (4/40) or methylenedioxymethamphetamine (MDMA) (6/40). Respondents were from at least 16 institutions, 4 countries, and 11 U.S. states (Supplementary Appendix 3) and had overseen an average of 41.4 psychedelic sessions in research settings (median 16 and range 2–200). 42.5% of respondents were physicians, while 57.5% of the population had other degrees (Table 1).
Responses to all Likert-type items are displayed in Figure 1. There was notable disagreement among the respondent population for many survey items, with an average range of response=4.21 (maximum possible=5). Half of the items had an average response between somewhat disagree and somewhat agree. These items had comparatively high response ranges (mean response range=4.50 vs. 3.93 for other items) and standard deviations (mean standard deviation=1.29 vs. 1.05 for other items), suggesting that the lack of strong opinion observed at the population level results largely from a lack of consensus, rather than uniform ambivalence. There was a strong overall opinion (average score of agree/disagree or greater) for only 2 items: item 1, in which respondents collectively asserted that it is unprofessional for facilitators to cuddle or have sustained full-body contact with recipients of treatment, and item 2, in which respondents emphasized the importance of trust in determining treatment outcomes.
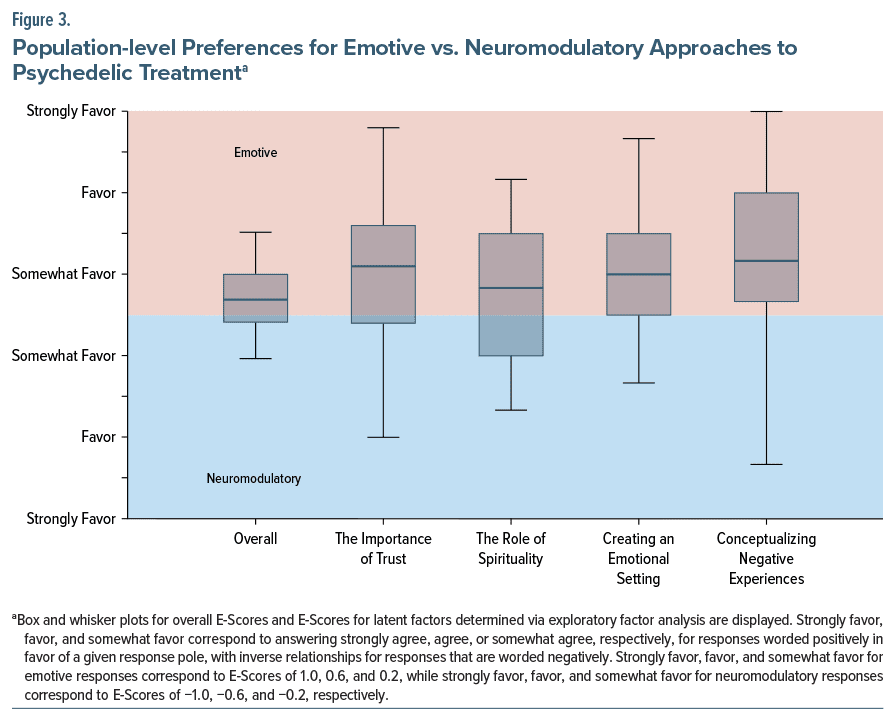
E-Scores represent the degree to which a given respondent prefers an emotive or a neuromodulatory approach to treatment. Data gathered from all items using this conceptual dichotomization, based on categories assigned by the study team before data collection, had Cronbach α = 0.59.
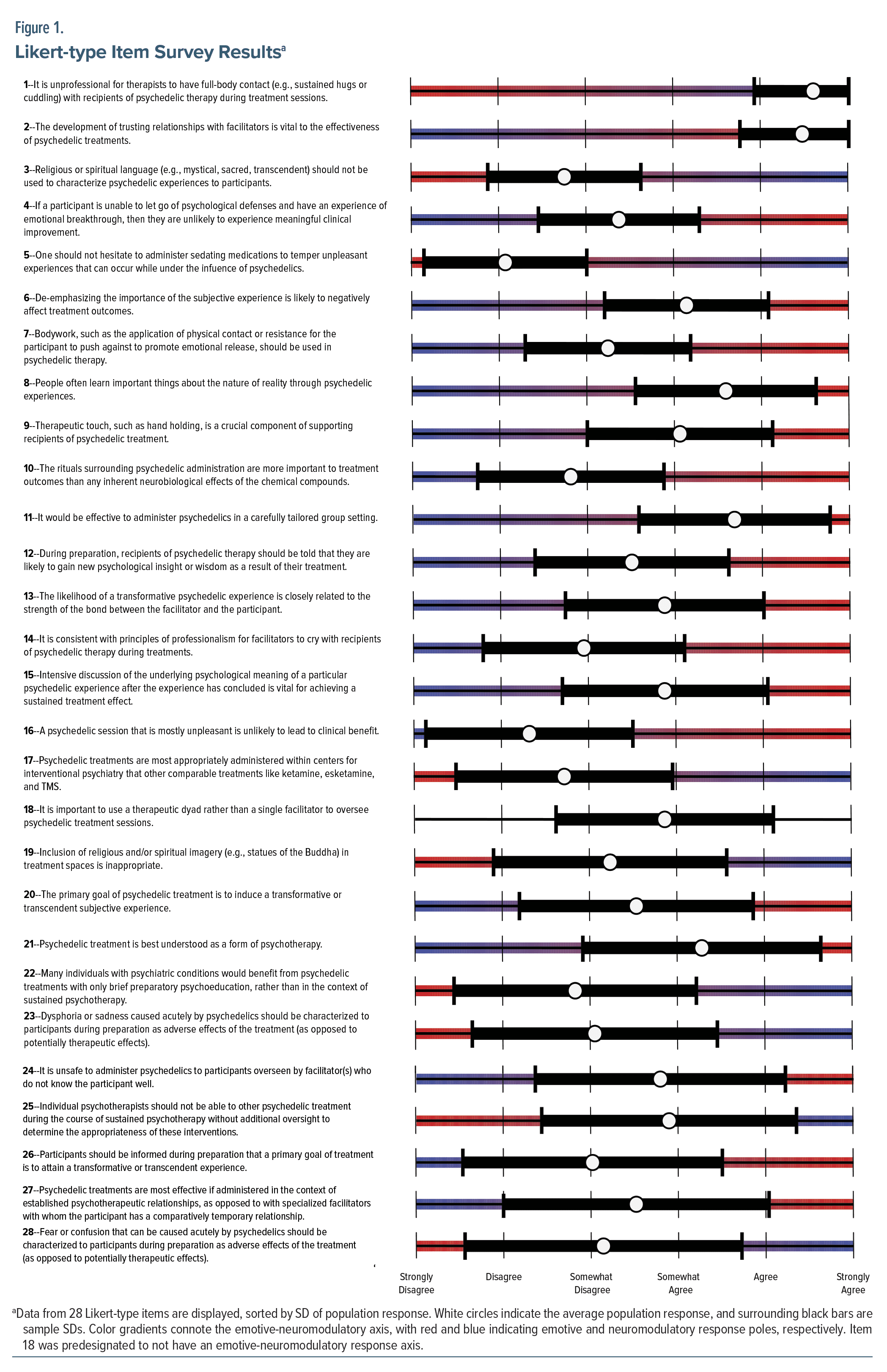
An EFA was performed to assess latent structure in the dataset, which determined subgroups of items that were most highly correlated along the predetermined emotive neuromodulatory axis. Resultant subcategories included The Importance of Trust (α=0.80), The Role of Spirituality (α=0.76), Creating an Emotional Setting (α=0.66), and Conceptualizing Negative Experiences (α=0.74).
Figure 2 displays the survey items within each factor. The Importance of Trust items pertain to the importance of the relationship between participant and facilitator, as well as to the hours of psychotherapy outside treatment sessions that should be included. The Role of Spirituality items relate to the psychological effects of the treatment experience and the incorporation of spiritual/religious concepts. Creating an Emotional Setting items discuss ways in which the emotionality of the treatment setting might be increased. Conceptualizing Negative Experiences items focus on whether dysphoric and disorienting experiences should be described to recipients as adverse effects of treatment, and how to manage such experiences.
Results of the E-Score analyses are displayed in Figure 3. Respondents had a slight preference for an emotive approach to psychedelic treatment (average E-Score = 0.08), and these responses were consistent with a normal distribution (Jarque-Bera test, P > .05). Latent factors trended further in the direction of an emotive preference, though with wider response variability, with average subscores ranging from 0.11 (The Role of Spirituality) to 0.29 (Conceptualizing Negative Experiences).
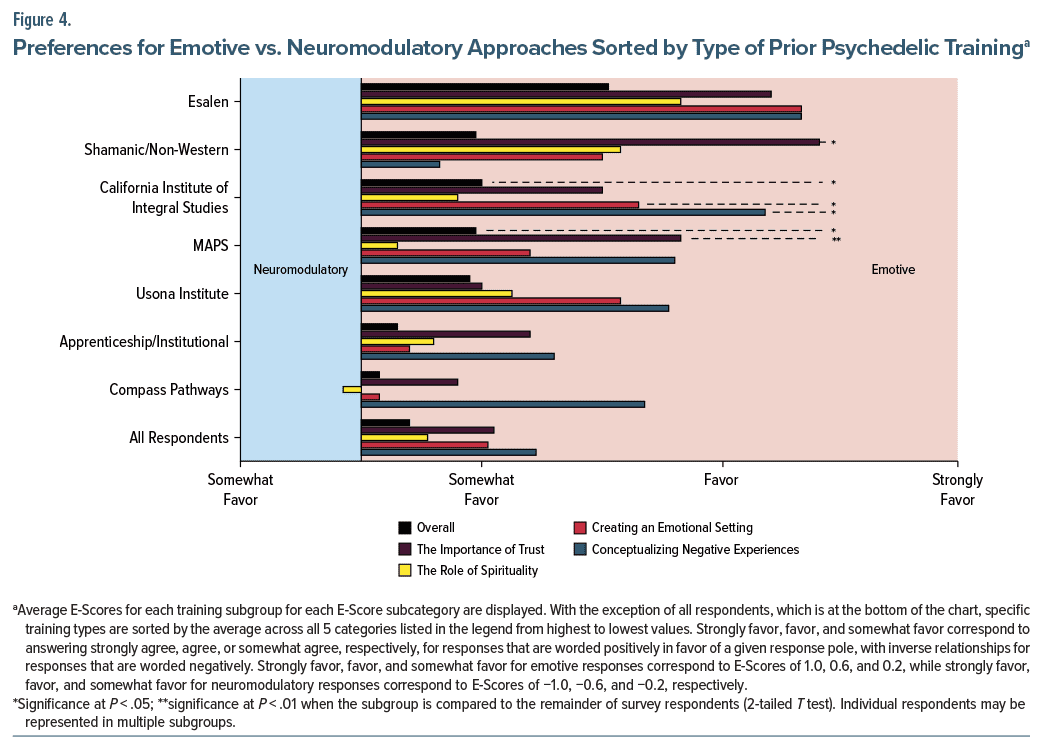
E-Scores varied by type of psychedelic training (Figure 4). Survey respondents who reported psychedelic training at the Multidisciplinary Association for Psychedelic Studies (MAPS) and the California Institute of Integral Studies (CIIS) had significantly higher E-Scores when compared to the remainder of respondents (2-tailed t-test, MAPS=0.19 vs. remainder of population=0.06, P=.018; CIIS=0.20 vs. remainder of population=0.06, P =.016). E-Scores for respondents reporting training at Esalen and in non-Western/shamanic settings had mostly insignificant but notable trends toward emotive preference, as these groups had especially small sample sizes in our respondent population (Table 1). No significant difference in E-Score was found between physician and nonphysician respondents.
DISCUSSION
In a future where psychedelic drugs may be approved medications for evidence-based psychiatric care, it will be important to establish guidelines surrounding best practices for delivering treatment safely and effectively outside research settings.50 This study offers insight into the views of psychedelic practitioners regarding the administration of classical psychedelics in professional settings. Many survey items elicited substantial disagreement among respondents, suggesting a variety of topics where additional research and discussion may contribute to greater consensus.
Our results indicate a slight preference toward an emotive approach to treatment among psychedelic practitioners. EFA found several subcategories which demonstrate a slightly more pronounced trend in favor of an emotive approach (Figure 3).
Notably, preferences vary among different subgroups with distinct psychedelic training backgrounds. For instance, respondents who trained with MAPS favored an emotive approach, especially in emphasizing the role of the therapeutic relationship and the quantity of psychotherapy needed during treatment (The Importance of Trust), while respondents who trained with Compass Pathways held a comparatively neuromodulatory perspective (Figure 4). Compass Pathways trials have been critiqued for the possibility that they may offer insufficient psychological support,14 study investigators have advanced a conceptualization of psychedelic treatment as pharmacotherapy rather than drug-assistedpsychotherapy,12 and the company has advanced a partnership with an interventional psychiatry company to administer psilocybin within that setting.51 By contrast, several participants in MAPS-sponsored trials—which included extensive psychotherapeutic support52,53—reported substantial emotional challenges when separating from their psychotherapists upon concluding the study, which may be an undesirable consequence of a comparatively emotive approach.54,55 Thus, these results may represent differences in culture within the field and support the construct validity of the metrics.
The survey instructed respondents to answer items on the basis of drug administration in a research or professional environment (Supplementary Appendix 1), though views may differ between these. This is especially pertinent regarding the role of expectation in clinical trials, as the FDA has emphasized the importance of minimizing expectancy effects, and researchers may also.46 It is important to note that any framing of the treatment—regardless of the content or perceived neutrality—should be considered part of the intervention, given the key role of social context in psychedelic experiences.40,56
Recent published research has been confined to relatively few research groups, in part due to the challenges of researching these Schedule I compounds, including limited federal funding to date.57 Through mid-2021, only 269 patients had received psilocybin or LSD in published clinical trials since 1991 (with at least several hundred additional patients receiving psilocybin since this time2–4), with slightly over 2,000 individuals receiving classical psychedelics in research studies generally.1 Because of this, respondents who meet this study’s inclusion criteria were likely a select group at the time of data collection. Respondents to this survey were experienced, having overseen 1,656 total psychedelic sessions. Respondents also came from varying educational backgrounds and locations—including at least 16 institutions, 11 U.S. states, and 4 countries—supportive of generalizability. Compass Pathways–trained respondents accounted for 10% of the population, who may be underrepresented, given that this group conducted the largest psychedelic trial to date by over 100 participants.
The E-Score metric was not validated prior to sending the survey to the target population, and the E-Score included a broad selection of subject matter. Despite this, Cronbach α = 0.59 for the construct, supportive of a moderate degree of construct reliability, in addition to evidence described above supportive of construct validity. The EFA performed in this study identified several latent factors with higher internal reliability, so these groups of items may be most immediately usable for future studies as independent constructs.58
The method of data collection for this study has several strengths. Data were acquired anonymously, useful for minimizing conformity and sampling bias. Because recruitment emails were sent to all study contacts listed in ClinicalTrials.gov, regardless of affiliation, sampling bias that might arise through other methods of recruitment was reduced.
Sampling bias could arise from informal sampling approaches, such as the recruitment of personal contacts of study authors and snowball recruitment. Other limitations of the data collection approach include that it was not possible to verify whether respondents in fact met inclusion criteria, it was unlikely to reach all potential respondents, and it was impossible to determine the precise response rate.
Historically, various cultures that have had socially sanctioned uses for psychedelic plants or fungi have used them in religious settings, considering them sacred.59–62 While such connotations are unlikely to fully persist within secular medical settings, this recurrent pattern carries significance for understanding potential social applications of the fundamental neurobiological effects of psychedelics. Established paradigms in biological psychiatry, as represented by the rationale for treatment and administration practices for esketamine or a regulatory emphasis on isolating pure drug effects without taking social setting into account,18,46 may not be safely or effectively applied to classical psychedelics.
The promise of psychedelic therapies has led to increasing public interest,63 mounting research results,1–4 increasing approval among the psychiatric profession,64,65 legalization or consideration of legalization,66 and movement toward FDA approval for medical use. Scaling these therapies to offer sustainable social benefits will require further dialogue and research on the many fascinating but challenging questions on how these substances best fit into the medical field and the broader culture.
Article Information
Published Online: February 5, 2025. https://doi.org/10.4088/JCP.24m15521
© 2024 Physicians Postgraduate Press, Inc.
Submitted: July 18, 2024; accepted October 21, 2024.
To Cite: Bender DA, Nayak SM, Siegel JS, et al. Psychological support approaches in psychedelic therapy: results from a survey of psychedelic practitioners. J Clin Psychiatry. 2025;86(1):24m15521.
Author Affiliations: Washington University School of Medicine, Saint Louis, Missouri (Bender, Siegel, Ercal, Lenze); The Johns Hopkins University School of Medicine, Baltimore, Maryland (Nayak); NYU Langone Center for Psychedelic Medicine, Department of Psychiatry, New York University Grossman School of Medicine, New York, New York (Siegel); Columbia University Vagelos College of Physicians and Surgeons, New York, New York (Hellerstein); New York State Psychiatric Institute, New York, New York (Hellerstein).
Corresponding Author: David A. Bender, MD, Washington University in St. Louis School of Medicine, 660 S. Euclid Ave, Saint Louis, MO 63110 ([email protected]).
Relevant Financial Relationships: Dr Nayak is an employee at the Johns Hopkins Center for Psychedelic and Consciousness Research, which is funded by philanthropic support from the Steven and Alexandra Cohen Foundation, as well as Tim Ferriss, Matt Mullenweg, Blake Mycoskie, and Craig Nerenberg. The funders had no input on the design, execution, or interpretation of this report. Dr Siegel is a former employee of Sumitomo Pharma America and has received consulting fees from Longitude Capital/Silo Wellness/Forbes & Manhattan and a speakers’ fee from SunCloud Health. Dr Hellerstein reports grant funding (to Research Foundation for Mental Hygiene, NY State) from the following: Compass Pathways, Relmada, Marinus, Intracellular Therapies, Beckley Scientific, NIAMS (M. Walker, PI), Velocity Foundation (Columbia; J. Markowitz, PI); has been on scientific advisory boards for Reset Pharmaceuticals, Mind Medicine Inc; and has received honoraria from Johns Hopkins University Press and Columbia University Press. Dr Ercal is a coinvestigator on a current Compass Pathways clinical trial, with no current or prior financial compensation for this role. Dr Lenze has a patent pending for sigma 1 agonists for COVID-19 and has done consulting for Merck, IngenioRx, Pritilin ICR, and Boehringer-Ingelheim. Dr Bender has no financial conflicts of interest to report.
Funding/Support: The study received funding from National Institutes of Health (R25- MH112473).
Role of the Sponsor: The sponsor had no role in the design or execution of the study.
Previous Presentation: Poster presented at the American Psychiatric Association Annual Meeting; May 5, 2024; New York, New York.
Acknowledgments: Many thanks to Stefan Larsen, B.A, and Amanada Pekau, MPH, BSN, RN-BC (Washington University in St Louis), for their assistance with data collection. These contributors have no pertinent financial conflicts of interest to report.
ORCID: David Bender: https://orcid.org/0000-0001-9842-2110
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- There is ongoing debate within the field of clinical psychedelic research regarding best practices for providing psychological support alongside drug administration.
- Our results quantify the differences of opinion on this topic among psychedelic researchers, demonstrating a slight overall trend toward preference for an emotive approach.
- Further discussion and research will be important for potential future providers of psychedelic treatments.
Editor’s Note: We encourage authors to submit papers for consideration as a part of our Focus on Psychotherapy section. Please contact John C. Markowitz, MD, at Psychiatrist.com/contact/markowitz or Rachel C. Vanderkruik, PhD, at Psychiatrist.com/contact/vanderkruik.
References (66)

- Bender D, Hellerstein DJ. Assessing the risk-benefit profile of classical psychedelics: a clinical review of second-wave psychedelic research. Psychopharmacol (Berl). 2022;239(6):1907–1932. PubMed
- Goodwin GM, Aaronson ST, Alvarez O, et al. Single-dose psilocybin for a treatment resistant episode of major depression. N Engl J Med. 2022;387(18):1637–1648. PubMed
- Raison CL, Sanacora G, Woolley J, et al. Single-dose psilocybin treatment for major depressive disorder: a randomized clinical trial. JAMA. 2023;330(9):843–853. PubMed
- Bogenschutz MP, Ross S, Bhatt S, et al. Percentage of heavy drinking days following psilocybin-assisted psychotherapy vs placebo in the treatment of adult patients with alcohol use disorder: a randomized clinical trial. JAMA Psychiatry. 2022;79(10):953–962. PubMed
- Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Bäbler A, et al. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport. 1998;9(17):3897–3902. PubMed CrossRef
- Becker AM, Klaiber A, Holze F, et al. Ketanserin reverses the acute response to LSD in a randomized, double-blind, placebo-controlled, crossover study in healthy participants. Int J Neuropsychopharmacol. 2023;26(2):97–106.
- Preller KH, Herdener M, Pokorny T, et al. The fabric of meaning and subjective effects in LSD-induced states depend on serotonin 2A receptor activation. Curr Biol. 2017;27(3):451–457.
- MindMed Breakthrough Therapy Article. 2024. Accessed January 07, 2024. https://www.forbes.com/sites/ajherrington/2024/03/11/fda-grants-breakthroughtherapy-status-to-lsd-drug-to-treat-anxiety/?sh=6edcf48e7ccb
- Cybin Gets Breakthrough Therapy Designation For Its Psychedelic-based Therapeutic CYB003. 2024. Accessed January 07, 2024. https://www.nasdaq.com/articles/cybin-gets-breakthrough-therapy-designation-for-its-psychedelic-basedtherapeutic-cyb003
- Heal DJ, Smith SL, Belouin SJ, et al. Psychedelics: threshold of a therapeutic revolution. Neuropharmacology. 2023;236:109610. PubMed
- Johnson M, Richards W, Griffiths R. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22(6):603–620. PubMed CrossRef
- Goodwin GM, Malievskaia E, Fonzo GA, et al. Must psilocybin always “assist psychotherapy”? Am J Psychiatry. 2024;181(1):20–25.
- Goodwin GM. Psilocybin: psychotherapy or drug? J Psychopharmacol. 2016;30(12):1201–1202.
- O’Donnell KC, Anderson BT, Barrett FS, et al. Misinterpretations and omissions: a critical response to Goodwin and colleagues’ commentary on psilocybin-assisted therapy. Am J Psychiatry. 2024;181(1):74–75.
- Schenberg EE, King F 4th, da Fonseca JE, et al. Is poorly assisted psilocybin treatment an increasing risk? Am J Psychiatry. 2024;181(1):75–76.
- Yaden DB, Earp D, Graziosi M, et al. Psychedelics and psychotherapy: cognitive behavioral approaches as default. Front Psychol. 2022;13:873279. PubMed
- Johnson MW. Consciousness, religion, and gurus: pitfalls of psychedelic medicine. ACS Pharmacol Transl Sci. 2021;4(2):578–581.
- Grunder G, Brand M, Mertens LJ, et al. Treatment with psychedelics is psychotherapy: beyond reductionism. Lancet Psychiatry. 2024;11(3):231–236.
- Borrell B. The Psychedelic Evangelist. 2024. Accessed January 07, 2024. https://www.nytimes.com/2024/03/21/health/psychedelics-roland-griffiths-johnshopkins.html
- Grof S. LSD Psychotherapy. 2nd ed. Hunter House;1994:352.
- Chandler AL, Hartman MA. Lysergic acid diethylamide (LSD-25) as a facil agent psychotherapy. AMA Arch Gen Psychiatry. 1960;2(3):286–299. PubMed
- Grinspoon L, Bakalar JB. Psychedelic Drugs Reconsidered. Basic Books; 1979.
- Passie T, Guss J, Krahenmann R. Lower-dose psycholytic therapy - a neglected approach. Front Psychiatry. 2022;13:1020505. PubMed
- Nayak S, Johnson MW. Psychedelics and psychotherapy. Pharmacopsychiatry. 2021;54(4):167–175.
- Mithoefer M, Mithoefer A, Jerome L. A Manual for MDMA-Assisted Psychotherapy in the Treatment of Posttraumatic Stress Disorder. 2017. Accessed January 07, 2024. https://maps.org/mdma/mdma-resources/treatment-manualmdma-assisted-psychotherapy-for-ptsd/.
- Nayak SM, Bradley MK, Kleykamp BA, et al. Control conditions in randomized trials of psychedelics: an ACTTION systematic review. J Clin Psychiatry. 2023;84(3):22r14518.
- Gukasyan N, Nayak SM. Psychedelics, placebo effects, and set and setting: insights from common factors theory of psychotherapy. Transcult Psychiatry. 2022;59(5):652–664.
- Anderson BT, Danforth AL, Grob CS. Psychedelic medicine: safety and ethical concerns. Lancet Psychiatry. 2020;7(10):829–830. PubMed CrossRef
- McNamee S, Devenot N, Buisson M. Studying harms is key to improving psychedelic-assisted therapy-participants call for changes to research landscape. JAMA Psychiatry. 2023;80(5):411–412.
- Yaden DB, Griffiths RR. The subjective effects of psychedelics are necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. 2021;4(2):568–572.
- Nayak SM, Singh M, Yaden DB, et al. Belief changes associated with psychedelic use. J Psychopharmacol. 2023;37(1):80–92.
- Timmermann C, Kettner H, Letheby C, et al. Psychedelics alter metaphysical beliefs. Sci Rep. 2021;11(1):22166. PubMed
- Smith WR, Sisti D. Ethics and ego dissolution: the case of psilocybin. J Med Ethics. 2020:medethics-2020-106070.
- Villiger D. Giving consent to the ineffable. Neuroethics. 2024;17(1):11.
- Gasser P. Psychedelic group therapy. Curr Top Behav Neurosci. 2022;56:23–34.
- Murphy R, Kettner H, Zeifman R, et al. Therapeutic alliance and rapport modulate responses to psilocybin assisted therapy for depression. Front Pharmacol. 2021;12:788155. PubMed
- Olson DE. The subjective effects of psychedelics may not be necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. 2021;4(2):563–567.
- Rosenblat JD, Leon-Carlyle M, Ali S, et al. Antidepressant effects of psilocybin in the absence of psychedelic effects. Am J Psychiatry. 2023;180(5):395–396. PubMed
- National Academies of Sciences, Engineering, and Medicine. Mechanisms of action and key research gaps for psychedelics and entactogens. In: Exploring Psychedelics and Entactogens as Treatments for Psychiatric Disorders: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2022.
- Carhart-Harris RL, Roseman L, Haijen E, et al. Psychedelics and the essential importance of context. J Psychopharmacol. 2018;32(7):725–731. PubMed CrossRef
- Griffiths RR, Richards WA, McCann U, et al. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacol (Berl). 2006;187(3):268–292;discussion 284–292. PubMed
- Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181–1197. PubMed CrossRef
- Ko K, Knight G, Rucker JJ, et al. Psychedelics, mystical experience, and therapeutic efficacy: a systematic review. Front Psychiatry. 2022;13:917199. PubMed
- Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165–1180. PubMed CrossRef
- Hartogsohn I. American Trip: Set, Setting, and the Psychedelic Experience in the Twentieth Century. The MIT Press;2020:418. CrossRef
- FDA Guidance on Psychedelic Trials. 2023. Accessed January 07, 2024. https://www.fda.gov/media/169694/download
- Olson DE. Psychoplastogens: a promising class of plasticity-promoting neurotherapeutics. J Exp Neurosci. 2018;12:1179069518800508. PubMed CrossRef
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–381. PubMed CrossRef
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208. PubMed
- Appelbaum PS. Psychedelic research and the real world. Nature. 2022;609(7929):S95. PubMed
- Compass Pathways and Greenbrook TMS Enter into Three-Year Research Collaboration Agreement. 2024. Accessed February 10, 2024. https://www.globenewswire.com/news-release/2024/01/05/2804617/0/en/CompassPathways-and-Greenbrook-TMS-enter-into-three-year-research-collaborationagreement.html
- Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Focus (Am Psychiatr Publ). 2023;21(3):315–328.
- Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021;27(6):1025–1033.
- Cover Story Podcast: Open-Heart Surg. 2022. Accessed February 10, 2024. https://www.thecut.com/2022/03/cover-story-podcast-open-heart-surgery.html
- Ross DNLK. Introducing Cover Story: Power Trip. New York Magazine; 2021.
- Hartogsohn I. Set and setting, psychedelics and the placebo response: an extra pharmacological perspective on psychopharmacology. J Psychopharmacol. 2016;30(12):1259–1267. PubMed CrossRef
- Barnett BS, Parker SE, Weleff J. United States National Institutes of Health grant funding for psychedelic-assisted therapy clinical trials from 2006–2020. Int J Drug Pol. 2022;99:103473. PubMed
- Nunnally JC. Psychometric Theory. 2nd ed. McGraw-Hill Series in Psychology. New York: McGraw-Hill; 1978:xv, 701.
- Fernandez, JW, Bwiti: An Ethnography of the Religious Imagination in Africa. Princeton University Press; 1982:xxiv, 731, 16 of plates.
- Myerhoff BG. Peyote Hunt; The Sacred Journey of the Huichol Indians. Symbol, Myth, and Ritual Series. Ithaca NY: Cornell University Press;1974:285.
- Wasson RG. The Wondrous Mushroom: Mycolatry in Mesoamerica. McGraw-Hill; 1980:xxv, 209.
- Pollan M. How to Change Your Mind: What the New Science of Psychedelics Teaches us About Consciousness, Dying, Addiction, Depression, and Transcendence. Penguin Press; 2018:1 online resource.
- Danias G, Appel J. Public interest in psilocybin and psychedelic therapy in the context of the COVID-19 pandemic: google trends analysis. JMIR Form Res. 2023;7:e43850. PubMed
- Barnett BS, Siu WO, Pope HG Jr. A survey of American psychiatrists’ attitudes toward classic hallucinogens. J Nerv Ment Dis. 2018;206(6):476–480. PubMed CrossRef
- Barnett BS, Arekalian M, Beebe D, et al. American psychiatrists’ opinions about classic hallucinogens and their potential therapeutic applications: a 7-year follow up survey. Psychedelic Med. 2023;2(1):1–9.
- Siegel JS, Daily JE, Perry DA, et al. Psychedelic drug legislative reform and legalization in the US. JAMA Psychiatry. 2023;80(1):77–83.
This PDF is free for all visitors!