Nearly a decade ago, Jeste and colleagues1 published a review in this journal highlighting the importance of harnessing positive psychosocial characteristics (PPCs) in promoting psychiatric outcomes. Among these, optimism—the expectation that good as opposed to bad things will happen in the future—is the most extensively studied. Although optimism has been linked to subjective well-being and improved physical and mental health,2–5 research on its population level correlates remains limited. Existing studies have identified psychosocial factors such as depression, posttraumatic stress disorder, social support, and resilience as being associated with optimism,6–8 but expanding these findings to populations at greater risk for adverse health outcomes is essential to inform effective interventions to bolster optimism.
Military veterans represent one such group, given their exposures to trauma (eg, combat) and higher prevalence of health conditions relative to nonveterans.9 One study published 14 years ago found that dispositional optimism buffered veterans from the adverse effects of war-associated stress on symptoms of posttraumatic stress disorder and work impairment.10 Despite this promising finding, limited research has since examined optimism in this population. Here, we conducted an exploratory study using data from a nationally representative sample of US veterans to examine the prevalence and correlates of optimism.
Methods
Sample. Data were analyzed from the National Health and Resilience in Veterans Study, which surveyed a nationally representative sample of 4,069 US veterans between 2019–2020 from KnowledgePanel, a probability-based online survey panel of >50,000 US households.
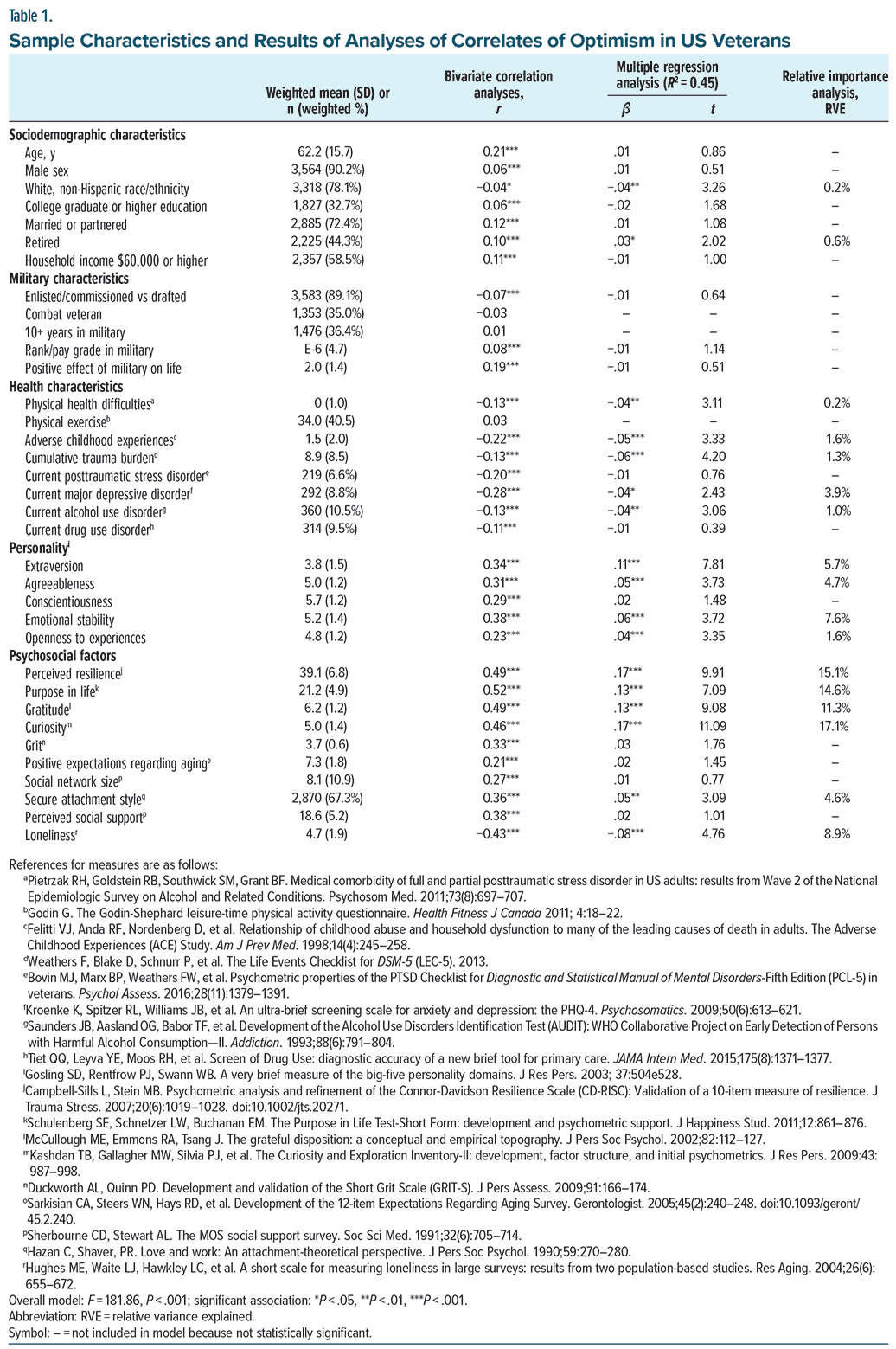
Measures. Optimism was assessed using a single-item measure from the Life Orientation Test-Revised11: “Please indicate how much you agree or disagree with the following statement: In uncertain times, I usually expect the best,” rated on a 7-point scale ranging from Strongly Disagree to Strongly Agree. Table 1 lists other measures.
Data Analysis. Spearman correlation and linear regression analyses were conducted to identify correlates of optimism scores. A relative importance analysis was then conducted to quantify the variance in optimism scores attributable to each significant independent variable after accounting for intercorrelations among these variables.
Results
The majority of the sample (67.1%) endorsed that they Slightly-to-Strongly Agreed that they were optimistic (18.0% endorsed Slightly Agree; 37.0%, Agree; and 12.1%, Strongly Agree).
As shown in Table 1, PPCs such as curiosity, perceived resilience, purpose in life, and gratitude explained the majority (58.1%) of the variance in optimism scores, with loneliness, emotional stability, and extraversion each explaining >5% of the variance in these scores.
Discussion
This exploratory study sought to identify and quantify the level and correlates of optimism in a nationally representative sample of US veterans. While average optimism scores were slightly lower than those in a younger general population (mean age = 57.1 years), the magnitude of this difference was small (Cohen d = 0.05).12
PPCs such as curiosity, perceived resilience, and purpose in life were strongly linked to higher optimism scores. These results suggest that, in addition to interventions directly targeting optimism (eg, Best Possible Self Intervention),13 those that target other PPCs, such as growth mindset interventions to foster curiosity,14 and cognitive-behavioral and mindfulness interventions to strengthen resilience and purpose in life,15–17 may also help increase optimism. Such interventions could also play a critical role in reducing the risk of adverse health outcomes in veterans and other at-risk populations.
Study limitations include the cross sectional design, reliance on self reported data, and a single-item optimism measure. Further research using longitudinal and qualitative designs and interview-based measures is needed to elucidate key correlates and determinants of optimism. Given the association between optimism, positive health outcomes,2–5 and suicide risk in military personnel,18 further research is needed to evaluate whether interventions targeting optimism, related PPCs, and optimism bias19 can effectively reduce risks and improve these outcomes.
Article Information
Published Online: April 21, 2025. https://doi.org/10.4088/JCP.25br15791
© 2025 Physicians Postgraduate Press, Inc.
J Clin Psychiatry 2025;86(2):25br15791
Submitted: January 13, 2025; accepted February 12, 2025.
To Cite: Yang R, Fischer IC, Na PJ, et al. Psychosocial correlates of optimism among US military veterans.
J Clin Psychiatry 2025;86(2):25br15791.
Author Affiliations: Department of Psychology, Harvard University, Cambridge, Massachusetts (Yang); US Department of Veterans Affairs National Center for PTSD, VA Connecticut Healthcare System, West Haven, Connecticut (Fischer, Na, Pietrzak); Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Fischer, Na, Pietrzak); Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, Connecticut (Pietrzak).
Corresponding Author: Robert H. Pietrzak, PhD, MPH, National Center for PTSD, VA Connecticut Healthcare System, 950 Campbell Ave 151E, West Haven, CT 06516 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors thank the veterans who participated in the National Health and Resilience in Veterans Study and the Ipsos staff who coordinated data collection.
ORCID: Rick Yang: https://orcid.org/0009-0003-2894-2796; Robert H. Pietrzak: https://orcid.org/0000-0002-5561-6414
References (19)

- Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76(6):675–683. Abstract CrossRef
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30(7):879–889.
- Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37(3):239–256. Abstract CrossRef
- Conversano C, Rotondo A, Lensi E, et al. Optimism and its impact on mental and physical well-being. Clin Pract Epidemiol Ment Health. 2010;6:25–29. Abstract CrossRef
- Kim ES, Hagan KA, Grodstein F, et al. Optimism and cause-specific mortality: a prospective cohort study. Am J Epidemiol. 2017;185(1):21–29. CrossRef
- Lecomte T, Corbière M, Théroux L. Correlates and predictors of optimism in individuals with early psychosis or severe mental illness. Psychosis. 2010;2(2):122–133.
- Gomez-Molinero R, Zayas A, Ruiz-González P, et al. Optimism and resilience among university students. Int J Dev Educ Psychol. 2018;1:147.
- Beitel M, Savant JD, Cutter CJ, et al. Psychopathology and pain correlates of dispositional optimism in methadone-maintained patients. Am J Addict. 2012;21 suppl 1(0–1):S56–S62. Abstract CrossRef
- Pietrzak RH, Levy BR, Tsai J, et al. Successful aging in older US veterans: results from the 2019–2020 national health and resilience in veterans study. Am J Geriatr Psychiatry. 2021;29(3):251–256. CrossRef
- Thomas JL, Britt TW, Odle-Dusseau H, et al. Dispositional optimism buffers combat veterans from the negative effects of warzone stress on mental health symptoms and work impairment. J Clin Psychol. 2011;67(9):866–880. Abstract CrossRef
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. Abstract CrossRef
- Hinz A, Friedrich M, Glaesmer H, et al. Temporal stability of optimism and pessimism (LOT-R) over 6 years in the general population. Front Psychol. 2024;15:1379651.
- Malouff JM, Schutte NS. Can psychological interventions increase optimism? A meta-analysis. J Posit Psychol. 2016;12(6):594–604. CrossRef
- Schutte NS, Malouff JM. A meta-analytic investigation of the impact of curiosity enhancing interventions. Curr Psychol. 2023;42:20374–20384. CrossRef
- Manco N, Hamby S. A meta-analytic review of interventions that promote meaning in life. Am J Health Promot. 2021;35(6):866–873. CrossRef
- Liu JJW, Ein N, Gervasio J, et al. Comprehensive meta-analysis of resilience interventions. Clin Psychol Rev. 2020;82:101919. Abstract CrossRef
- Schäfer SK, von Boros L, Schaubruch LM, et al. Digital interventions to promote psychological resilience: a systematic review and meta-analysis. NPJ Digit Med. 2024;7(1):30.
- Naifeh JA, Ursano RJ, Stein MB, et al. Optimism, sociability, and the risk of future suicide attempt among U.S. Army soldiers. Mil Med. 2024;189(7–8):e1642–e1652. CrossRef
- Karnick AT, Brick LA. From perception to projection: exploring neuroaffective advances in understanding optimism bias and belief updating. Curr Opin Psychol. 2024;60:101937. CrossRef
This PDF is free for all visitors!