ABSTRACT
Aim: The economic burden of schizophrenia in the United States (US) was estimated at $155.7 billion in 2013. Since 2013, the US experienced significant health care reforms and treatment advances. This study analyzed recent data and literature to update the US economic burden estimate for schizophrenia.
Methods: Direct and indirect costs associated with schizophrenia were estimated using a prevalence-based approach. Direct health care costs were assessed retrospectively using an exact matched cohort design in the IBM Watson Health MarketScan databases from October 1, 2015, through December 31, 2019. Patients with schizophrenia (identified using ICD-10-CM codes F20 and F25) were exactly matched to controls on demographics, insurance type, and index year. Direct non–health care costs were estimated using published literature and government data. Indirect costs were estimated using a human capital approach and the value of quality-adjusted life-years lost. Cost offsets were estimated to account for basic living costs avoided. Excess costs, comparing costs for individuals with and without schizophrenia, were reported in 2019 USD.
Results: The estimated excess economic burden of schizophrenia in the US in 2019 was $343.2 billion, including $251.9 billion in indirect costs (73.4%), $62.3 billion in direct health care costs (18.2%), and $35.0 billion in direct non–health care costs (10.2%). The largest drivers of indirect costs were caregiving ($112.3 billion), premature mortality ($77.9 billion), and unemployment ($54.2 billion). Cost offsets, representing $6.0 billion (1.7%), were subtracted from direct non–health care costs.
Conclusions: The estimated burden of schizophrenia in the US doubled between 2013 and 2019 and was $343.2 billion in 2019, highlighting the importance of effective strategies and treatment options to improve the management of this difficult-to-treat patient population.
J Clin Psychiatry 2022;83(6):22m14458
To cite: Kadakia A, Catillon M, Fan Q, et al. The economic burden of schizophrenia in the United States. J Clin Psychiatry. 2022;83(6):22m14458.
To share: https://doi.org/10.4088/JCP.22m14458
© 2022 Physicians Postgraduate Press, Inc.
aSunovion Pharmaceuticals, Marlborough, Massachusetts
bAnalysis Group, Inc., New York, New York
cAnalysis Group, Inc., Boston, Massachusetts
*Corresponding author: Carole Dembek, MS, Sunovion Pharmaceuticals, 84 Waterford Dr, Marlborough, MA 01752 ([email protected]).
Schizophrenia is a chronic, severe, and disabling mental health disorder affecting 1.19% of the US population and is characterized by deficits in thought processes, perceptions, and emotional responsiveness, leading to loss of function and autonomy.1–4 Adults with schizophrenia in the US are more than 3.5 times as likely to die compared to adults in the general population, with cardiovascular risk factors, tobacco use, and substance abuse contributing to this excess mortality burden.5
Schizophrenia is associated with significant economic burden, not only for patients but also for families, other caregivers, and the wider society. In the US, the annual cost of schizophrenia was estimated to be greater than the annual costs of all cancers combined.6 The costs of schizophrenia can be characterized as direct health care, direct non–health care, and indirect costs. Direct health care costs include inpatient, outpatient, emergency department, long-term care, pharmacy costs, and costs related to other medical care (eg, community-based, nursing-home, and rehabilitation).7 Direct non–health care costs typically include costs associated with law enforcement, homeless shelters, other social services, and research and training costs.7,8 The indirect costs of schizophrenia are frequently defined as costs related to unemployment, lost productivity, caregiving, and premature mortality.7
A recent estimate of the overall cost burden of schizophrenia was published in 2016.8 Cloutier et al estimated the annual US societal cost of schizophrenia in 2013 at approximately $155.7 billion (excess direct health care costs: $37.7 billion; direct non–health care costs: $9.3 billion; indirect costs: $117.3 billion; cost offsets: $8.6 billion). Using a prevalence-based approach, Cloutier et al estimated incremental health care costs by insurance type (ie, Medicare, Medicaid, commercially insured, and uninsured) compared to matched control patients without schizophrenia. In addition, direct non–health care costs of law enforcement, homeless shelters, and research and training as well as indirect costs of unemployment, reduced work productivity, premature mortality, and caregiving were estimated.
The 2013 estimate of the US cost burden of schizophrenia does not reflect recent health care system reforms and treatment advances in schizophrenia. The Patient Protection and Affordable Care Act, enacted in 2010, reduced the proportion of uninsured adults from 18% in 2013 to 8% in 20199,10 and an estimated 15 million US residents gained Medicaid coverage over the same period.11 Furthermore, the transition to the International Classification of Diseases, 10th Revision (ICD-10), on October 1, 2015, resulted in new billing codes that may affect the coding of diagnoses of schizophrenia. Antipsychotic treatment options for patients with schizophrenia also changed since 2013, with new antipsychotics approved (eg, brexpiprazole, cariprazine, lumateperone, and aripiprazole long-acting injectable) and others going off patent (eg, quetiapine, olanzapine, and oral aripiprazole), thus affecting direct pharmacy costs.
Updated estimates of the societal economic burden of schizophrenia may increase awareness of the current burden of schizophrenia and inform future health care spending decisions. This study updated the prior 2013 analysis to estimate the total societal economic burden of schizophrenia in the US in 2019.
METHODS
This study updated and refined the methodology described by Cloutier et al8 to estimate the economic burden of schizophrenia in the US using a prevalence-based approach. A lifetime prevalence of 1.19% was used as the base case.3 Sensitivity analyses were conducted using a lifetime prevalence of 0.72%.3
Excess costs represent the difference in costs between the population with schizophrenia and a similar population without schizophrenia. The total economic burden was estimated as the sum of excess direct health care costs, excess direct non–health care costs, and excess indirect costs, after subtracting the direct cost offsets.
Direct health care costs (pharmacy, outpatient care, inpatient care, emergency department visits, long-term care, and other medical services), direct non–health care costs (law enforcement, research and training, homeless shelters, and Supplemental Security Income [SSI] and Social Security Disability Insurance [SSDI]), direct cost offsets (basic living costs avoided by institutionalized individuals who would otherwise resort to the social safety net), indirect costs (unemployment, productivity loss, premature mortality, and caregiving), and overall costs were estimated using the most recent data available prior to the COVID-19 pandemic (to reflect a typical year of care), with all costs expressed in 2019 US dollars (USD).
Specific methods for the calculation of direct health care costs, and each dimension of direct non–health care and indirect costs, are described in the following section and in Table 1.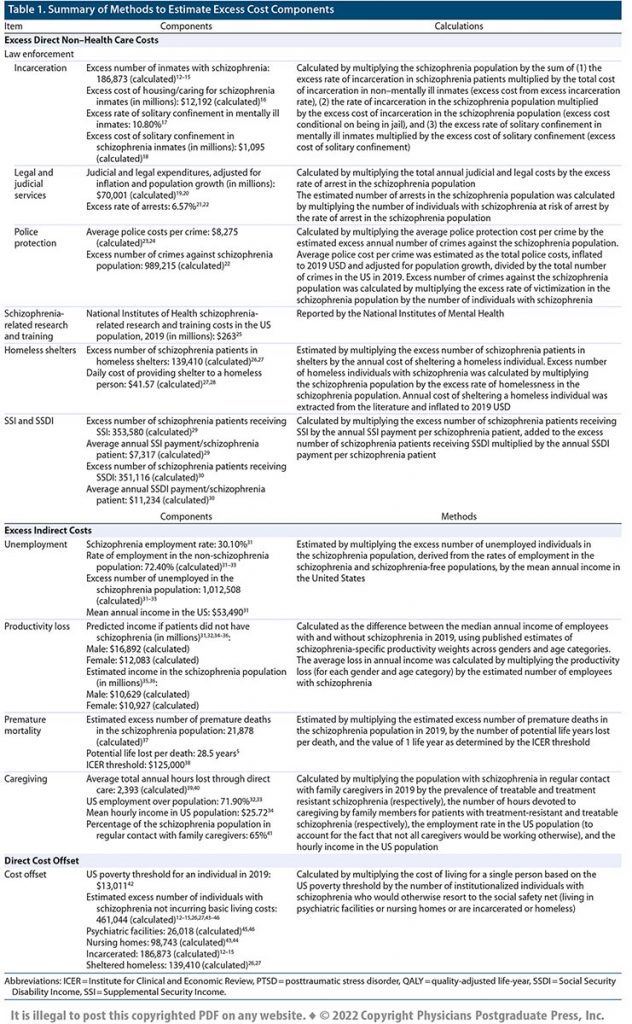
Direct Health Care Costs
Direct health care costs for insured patients were estimated retrospectively using an exact matched cohort design, comparing patients with (case cohort) and without schizophrenia (control cohort). Insurance claims data from the IBM Watson Health MarketScan databases (October 1, 2015, through December 31, 2019) were used to group patients into 3 samples: Medicaid-insured patients from the Multi-State Medicaid Database, commercially insured patients from the Commercial Claims and Encounters Database, and Medicare-insured patients from the Medicare Supplemental Database. This study was exempt from review by an institutional review board because the data were deidentified and compliant with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act.
Patients were required to have continuous health plan enrollment for ≥ 12 months. The study period was defined as the last 12-month period available in the data, while the index date was defined as the last calendar date followed by 12 months of continuous enrollment in a health plan (ie, the last calendar date before the study period). Medicaid-insured and commercially insured patients were required to be ≥ 18 years old and < 65 years old at the index date, while Medicare patients were required to be ≥ 65 years at the index date. In addition, patients included in the schizophrenia cohorts were required to have ≥ 2 diagnoses of schizophrenia (ICD-10-CM code: F20) or a schizoaffective disorder (ICD-10-CM code: F25) and were exactly matched to patients without schizophrenia on a ratio of up to 1:3 on age, sex, region of residence (commercial and Medicare only), race (Medicaid only), health plan type, and year of index date.
Patient characteristics were summarized descriptively for each payer population and included age, race, sex, insurance type, region, and index year, when available. Total direct health care costs for insured patients were estimated over the study period. Excess direct health care costs were based on the costs incurred by schizophrenia patients compared to non-schizophrenia patients in each payer population. Total excess health care costs for uninsured patients were calculated assuming a mean annual cost of $909 per uninsured patient ($800 in 2011 USD inflated to 2019 dollars)47 and a cost ratio between patients with and without schizophrenia similar to the cost ratio observed in the Medicaid-insured population. Frequencies and proportions were reported for categorical variables, while means, standard deviations (SDs), medians, and interquartile ranges (IQRs) were reported for continuous variables.
RESULTS
Total Economic Burden
Given a prevalence estimate of 1.19%, the schizophrenia population in the US in 2019 was estimated to be 3,906,050, contributing to an excess economic burden of $343.2 billion (Figure 1, Table 2), which corresponded to an annual excess cost per person with schizophrenia of $87,856. The excess direct health care costs were $62.3 billion ($15,957 per person with schizophrenia), the excess direct non–health care costs were $35.0 billion ($8,956 per person with schizophrenia), and the excess indirect costs were $251.9 billion ($64,479 per person with schizophrenia) (Figure 1). Costs associated with caregiving were the greatest contributor to excess indirect costs at $112.3 billion ($28,761 per person with schizophrenia), accounting for about a third of the total excess costs (Figure 1). Cost offsets, representing $6.0 billion ($1,536 per person with schizophrenia), were subtracted from direct non–health care costs.
Excess Direct Health Care Costs
Direct health care costs were estimated based on a sample of 131,125 patients with schizophrenia. Among these patients, 24,881 (19.0%) were commercially insured, 2,779 (2.1%) were Medicare-insured, and 103,465 (78.9%) were Medicaid-insured (Table 3). On average (mean values), patients were 37.3, 76.2, and 41.7 years old at index across the commercially insured, Medicare-insured, and Medicaid-insured populations, respectively; most of the commercial and Medicaid population were male (56.0% and 53.3%, respectively) while most of the Medicare population (64.9%) were female (Table 3).
Excess direct health care costs were estimated to be $62.3 billion and included costs associated with pharmacy ($12.1 billion), outpatient care ($12.9 billion), inpatient care ($30.2 billion), emergency department visits ($5.6 billion), long-term care ($1.5 billion), and other medical services ($120.6 million) (Table 2). Mean total health care costs were similar across the commercially insured and Medicaid-insured cohorts but were higher for Medicare-insured patients ($26,904, $26,095, and $34,391, respectively) (Table 4). Mean excess health care costs varied across cohorts, with the greatest excess among commercially insured patients ($19,293), followed by Medicaid- and Medicare-insured patients at $15,347 and $11,963, respectively. The estimated excess cost per uninsured patient with schizophrenia was $1,289, representing a total excess cost of $411.9 million.
Excess Direct Non–Health Care Costs
Excess direct non–health care costs were estimated to be $35.0 billion, accounting for approximately 10.2% of the total economic burden of schizophrenia in 2019 (Figure 1, Table 2). Excess law enforcement costs were estimated to be $26.1 billion, including $8.2 billion in police protection, $4.6 billion in judicial and legal services, and $13.3 billion in incarceration costs. Excess homeless shelter costs were estimated to be $2.1 billion, corresponding to homeless shelter costs for 139,410 excess sheltered homeless individuals with schizophrenia. Annual schizophrenia-related research and training costs were $263.0 million, as reported by the National Institutes of Health.25 Excess costs related to SSI and SSDI were estimated to be $6.5 billion, accounting for mean annual SSI and SSDI payments of, respectively, $7,317 and $11,234 per schizophrenia patient.
Excess Direct Cost Offsets
Based on an estimated 461,044 excess individuals with schizophrenia not incurring basic living costs in 2019, direct cost offsets of $6.0 billion were deducted from the excess direct non–health care costs based on the US Census Bureau Poverty Threshold for an individual in 2019,42 which was $13,011 (Figure 1, Table 2).
Excess Indirect Costs
Excess indirect costs accounted for 73.4% ($251.9 billion) of the total economic burden of schizophrenia (Figure 1, Table 2). Costs associated with caregiving were the greatest contributor to excess indirect costs at an estimated $112.3 billion, accounting for 32.7% of the total economic burden. Costs due to premature mortality, unemployment, and productivity loss totaled $77.9 billion, $54.2 billion, and $7.4 billion, respectively.
Sensitivity Analysis
Using a lifetime prevalence rate of 0.72%,3 the schizophrenia population in the US in 2019 was estimated to be 2,363,325, contributing to an excess economic burden of $215.1 billion (Table 2). Using this prevalence estimate, excess direct health care, direct non–health care, and indirect costs represented $37.7 billion (17.5%), $30.8 billion (14.3%), and $152.8 billion (71.1%), respectively.
DISCUSSION
The economic burden of schizophrenia in the US in 2019 was estimated at $343.2 billion. Indirect costs accounted for over 73% of total costs and were largely driven by caregiving costs ($112.3 billion), which accounted for about one-third (32.7%) of the total excess economic burden. These findings suggest that the total estimated burden of schizophrenia doubled (+100.9%) between 2013 and 2019 (after adjusting for inflation). On a per-patient basis, the burden increased by 78.8% (after adjusting for inflation), consistent with an overall increase in schizophrenia burden. A sensitivity analysis using a lower prevalence estimate of 0.72% estimated that the total burden increased by 25.9% between 2013 and 2019.
Compared to Cloutier et al8 and after adjusting for inflation, direct health care costs were 50.7% higher ($62.3 billion in 2019 vs $41.4 billion in 2013). The increase in direct health care costs (+50.7%) was primarily driven by a $13.5 billion increase in inpatient costs (+80.9%) and a $4.8 billion increase in outpatient costs (+58.8%). Although other direct health care costs represented a smaller proportion of the overall increase, long-term care costs (+$0.8 billion) and emergency department costs (+$2.8 billion) doubled in 6 years (respectively, +124.5% and +97.8%), suggesting a potentially concerning trend. Over the same period, pharmacy (drug) costs increased by 19.2% (+$1.9 billion).
The difference in direct health care costs between Cloutier et al8 and the current study can be attributed to several factors: the increase in the schizophrenia population (+12%), influenced by the increase in the US population and the difference in prevalence between the two studies (1.19% vs 1.10%); the change in per-patient excess costs among commercially insured patients (+41.1%), Medicaid patients (+12.4%), and Medicare patients (−12.1%); a decrease in the size of the uninsured US population between 2013 and 2019 and the assumed health care costs among uninsured patients (annual excess costs related to uncompensated care estimated at $1,289 per patient versus assumed to be $0).
Direct non–health care costs and indirect costs were, respectively, 290.4% higher ($39.8 billion in 2019 vs $10.2 billion in 2013), and 95.7% higher ($251.9 billion vs $128.7 billion in 2013) than in Cloutier et al,8 partially due to a change in methodology to estimate these excess costs more comprehensively. The increase in law enforcement costs (+293.1%) was driven by a higher victimization rate in the schizophrenia population from the literature (25.33% in current study vs 5.25% in Cloutier et al8), leading to a 6-fold increase in police protection costs. The calculation of incarceration costs in this study considered the excess rate of incarceration in the schizophrenia population as in Cloutier et al,8 but also the excess cost of incarceration conditional on being in jail and the excess cost of solitary confinement. Direct non–health care costs also included SSI and SSDI, which constitute important sources of income for people living with schizophrenia but were not included in the 2013 estimate.48
The increase in indirect costs was driven by a 20-fold increase in the estimate of premature mortality costs (+$74.3 billion) and by the doubling of caregiving costs (+$54.7 billion). Cloutier et al8 included only suicide-related premature mortality costs using a human capital approach. In contrast, the current study considered all premature mortality costs and valued life years lost at $125,000 per life-year, the midpoint between $100,000 and $150,000 per quality-adjusted life-year gained, which is used by several value assessment organizations n the US.16 As suicide-related costs constitute only a small proportion of the premature mortality costs of schizophrenia, the current methods accounted for the burden of schizophrenia on premature mortality more comprehensively regardless of the direct cause of death. Concerning caregiving costs, the current study used a direct valuation approach (as in Cloutier et al8) along with updated estimates accounting for heterogeneity in caregiving time between patients with treatable and treatment-resistant schizophrenia. This is an important distinction, as these two subgroups of patients require very different caregiver involvement.17 The updated estimate of caregiving time was based on peer-reviewed publications39,40 (versus a news survey in Cloutier et al8).
In 2021, The Schizophrenia & Psychosis Action Alliance (SPAA) published a report48 estimating the cost of schizophrenia in the US at $281.6 billion in 2020 (versus $343.2 billion in 2019 in this study), including $27.2 billion in direct health care costs (versus $62.3 billion), $46.6 billion in direct non–health care costs (versus $35.0 billion), and $219.6 billion in indirect costs (versus $251.9 billion; including caregiving [$104.5 billion vs $112.3 billion]).
The difference in costs between this study and the SPAA report is due to the use of a different prevalence estimate (0.8% versus 1.19% in this study) as well as different data sources and methodologies to estimate direct and indirect cost components. Much lower direct health care costs in the SPAA report ($27.2 billion vs $62.3 billion in this study) are due to the use of Medical Expenditure Panel Survey data (versus claims data), which rely on patient self-report and may underreport health care use as well as underrepresent patients with high expenditures.18 The large difference in costs for supportive housing and homelessness ($24.7 billion vs $2.1 billion in this study) is due to the incorporation of total costs for supportive housing in the SPAA report because excess costs could not be calculated. In the absence of the data necessary to calculate excess costs, this study did not include supportive housing costs (thus providing a conservative estimate). Indirect cost estimates, which included some of the largest contributors to the overall burden, including caregiving, premature mortality, and productivity loss, were generally consistent between the two studies despite the use of different data sources and methodologies.
Limitations
This study utilized a prevalence-based approach. According to the National Institute of Mental Health (NIMH), precise estimates of schizophrenia prevalence are difficult to achieve due to its overlap with other disorders in presentation, clinical complexity, and inconsistent diagnostic methods.2 The estimation of direct health care costs included both schizophrenia (ICD-10-CM code F20) and schizoaffective disorders (ICD-10-CM code F25). However, the estimation of direct non–health care costs and indirect costs is based on the literature, where the definition used for schizophrenia (including or excluding schizoaffective disorders) was not consistently available. Therefore, this estimate of the total excess burden of schizophrenia may under or overestimate the true burden of disease. To mitigate this concern, this study includes a sensitivity analysis using a 0.72% prevalence estimate in addition to the base case of 1.19%.
There may be wide variation in costs across patients with schizophrenia depending on severity of schizophrenia and the presence and severity of comorbidities. This study uses average costs as inputs to calculate excess costs, which accounts for the distribution of severity in the population in the calculation of total costs. In addition, the study accounts for heterogeneity in costs within the schizophrenia population whenever possible; for example, caregiving costs consider the heterogeneity in caregiving time between patients with treatable and treatment-resistant schizophrenia.
This study estimates excess costs among individuals diagnosed with schizophrenia. Consequently, the direct health care costs among people with undiagnosed schizophrenia were not captured, thereby likely underestimating the excess burden of schizophrenia. Similarly, patients eligible for multiple insurance types (eg, Medicare and Medicaid) and those covered by military health insurance were not represented in this sample. Our analysis assumed that these individuals were similar to individuals included in our sample, which may limit the generalizability of the findings to these populations. Further, to estimate the direct health care costs in the uninsured population, it was assumed that the cost ratio observed in the Medicaid population between the schizophrenia and schizophrenia-free populations also applied to the uninsured population, which may not be the case. Finally, premature mortality was estimated using a life-year valuation approach and would change if different life-year valuations were used.
CONCLUSION
The estimated societal burden of schizophrenia in the US in 2019 was $343.2 billion, representing a 100.9% increase in the estimated burden from 2013 to 2019 (inflation adjusted). Indirect costs contributed the most to the overall economic burden of disease, driven largely by costs associated with caregiving ($112.3 billion), which accounted for about a third of the total economic burden. The large societal burden of schizophrenia in the US highlights the importance of effective strategies and treatment options to improve the management of this difficult-to-treat patient population.
Submitted: March 16, 2022; accepted July 26, 2022.
Published online: October 10, 2022.
Author contributions: Ms Kadakia, Ms Dembek, Ms Fan, and Dr Williams made substantial contributions to the design of the study and the interpretation of the data and have substantially revised the work. Dr Catillon, Dr Marden, Ms Anderson, and Dr Kirson made substantial contributions to the design of the study, the data analysis, and the interpretation of the data and have substantially revised the work. All authors have approved the final submitted version of the manuscript and agree both to be personally accountable for their contributions and to ensure that questions related to the accuracy or integrity of any part of the work will be appropriately investigated, resolved, and documented in the literature.
Relevant financial relationships: Ms Kadakia, Ms Dembek, Ms Fan, and Dr Williams are employed by Sunovion. Dr Catillon, Dr Marden, Ms Anderson, and Dr Kirson are employed by Analysis Group, Inc., which received funding from Sunovion to conduct this study.
Funding/support: This study was sponsored by Sunovion Pharmaceuticals.
Role of the sponsor: The funding agency contributed to and approved the study design and received regular updates on the progress of the study. The funding agency also contributed to data analysis, data interpretation, and development of the manuscript. The funding agency was not involved in data collection.
Previous presentations: The results from this study have been presented at the Psych Congress; October 29–November 1, 2021; San Antonio, Texas and at the Neuroscience Education Institute Congress (NEI); November 4–7, 2021; Colorado Springs, Colorado
IRB: This study was exempt from review by an institutional review board because the data were de-identified and compliant with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act.
Additional information: The data used for the present study were licensed by Analysis Group, Inc., from IBM Watson and are not publicly available. Further information on the IBM MarketScan databases can be found at https://www.ibm.com/products/marketscan-research-databases.
CLINICAL POINTS
- Estimating the burden of schizophrenia is complex, and past assessments of the burden of schizophrenia have not been updated to account for recent health care system reforms and treatment advances in schizophrenia.
- There is a need for effective treatment options and strategies to improve the management of schizophrenia.
References (48)

- Schizophrenia (NIH Publication No. 19-MH-8082). National Institute of Mental Health. US Department of Health and Human Services, National Institutes of Health. NIH website. https://www.nimh.nih.gov/sites/default/files/documents/health/publications/schizophrenia/21-mh-8082_schizophrenia.pdf. 2021. Accessed February 1, 2022.
- Schizophrenia National Institute of Mental Health. National Institute of Health website. https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml. 2018. Accessed February 1, 2022.
- McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30(1):67–76. PubMed CrossRef
- Brain Facts - A Primer on Brain and Nervous System. Society for Neuroscience. Brain Facts website. https://tdlc.ucsd.edu/tdlc2/events/Brain%20Facts_A%20primer.pdf. 2018. Accessed February 1, 2022.
- Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with Schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172–1181. PubMed CrossRef
- Thaker GK, Carpenter WT Jr. Advances in schizophrenia. Nat Med. 2001;7(6):667–671. PubMed CrossRef
- Chong HY, Teoh SL, Wu DB, et al. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. PubMed
- Cloutier M, Aigbogun MS, Guerin A, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–771. PubMed CrossRef
- Borelli MC, Bujanda M, Maier K. The Affordable Care Act Insurance Reforms: where are we now, and what’s next? Clin Diabetes. 2016;34(1):58–64. PubMed CrossRef
- Table H-01. Health Insurance Coverage Status and Type of Coverage by Selected Characteristics: 2019. United States Census Bureau website. https://www.census.gov/data/tables/time-series/demo/income-poverty/cps-hi/hi.2019.html. 2019. Accessed February 1, 2022.
- Total Monthly Medicaid/CHIP Enrollment and Pre-ACA Enrollment. Kaiser Family Foundation website. https://www.kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. 2019. Accessed February 1, 2022.
- Zeng Z, Menton T. Jail Inmates in 2019. US Department of Justice. US Bureau of Justice Statistics website. https://bjs.ojp.gov/library/publications/jail-inmates-2019. 2021. Accessed February 1, 2022.
- Carson EA. Prisoners in 2019. US Department of Justice. US Bureau of Justice Statistics website. https://bjs.ojp.gov/library/publications/prisoners-2019. 2021. Accessed February 1, 2022.
- Bronson J, Berzofsky M. Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011–2012. NCJ 250612. US Department of Justice website. https://bjs.ojp.gov/content/pub/pdf/imhprpji1112.pdf. 2017. Accessed February 1, 2022.
- Bipolar Disorder National Institute of Mental Health. National Institute of Health website. https://www.nimh.nih.gov/health/statistics/bipolar-disorder. 2017. Accessed February 1, 2022.
- Swanson JW, Frisman LK, Robertson AG, et al. Costs of criminal justice involvement among persons with serious mental illness in connecticut. Psychiatr Serv. 2013;64(7):630–637. PubMed CrossRef
- Beck A. Use of Restrictive Housing in the US Prisons and Jails, 2011–2012. US Bureau of Justice Statistics website. https://bjs.ojp.gov/content/pub/pdf/urhuspj1112.pdf. 2015.
- Johnson C, Chapell B. Solitary Confinement Costs $78K Per Inmate and Should Be Curbed, Critics Say. NPR website. https://www.npr.org/sections/thetwo-way/2014/02/25/282672593/solitary-confinement-costs-78k-per-inmate-and-should-be-curbed-critics-say%20$78k%20per%20year. 2014. Accessed February 1, 2022.
- Buehler E. Justice Expenditure and Employment Extracts Series. Bureau of Justice Statistics website. https://bjs.ojp.gov/data-collection/justice-expenditure-and-employment-extracts-series. 2016. Accessed February 1, 2022.
- US and World Population Clock. US Census Bureau website. https://www.census.gov/popclock/. 2022. Accessed February 1, 2022.
- 2019 Crime in the United States–Persons Arrested. US Department of Justice, Investigation FBI website. https://ucr.fbi.gov/crime-in-the-u.s/2019/crime-in-the-u.s.-2019/topic-pages/persons-arrested.pdf. 2019. Accessed February 1, 2022.
- Ascher-Svanum H, Nyhuis AW, Faries DE, et al. Involvement in the US criminal justice system and cost implications for persons treated for schizophrenia. BMC Psychiatry. 2010;10(1):11. PubMed CrossRef
- Morgan RE, Truman JL. Criminal Victimization, 2019. US Department of Justice. NCJ 255113. Bureau of Justice Statistics website https://bjs.ojp.gov/library/publications/criminal-victimization-2019. Accessed February 1, 2022.
- Buehler ED. Justice Expenditure and Employment Extracts, 2016-Final. US Department of Justice. NCJ 300061. Bureau of Justice Statistics website. https://bjs.ojp.gov/library/publications/justice-expenditure-and-employment-extracts-2016-final. 2016. Accessed February 1, 2022.
- Estimates of Funding for Various Research, Condition, and Disease Categories. National Institutes of Health website. https://report.nih.gov/funding/categorical-spending#/. 2020. Accessed February 1, 2022.
- Ayano G, Tesfaw G, Shumet S. The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):370. PubMed CrossRef
- Henry M, Watt R, Mahathey A, et al. The 2019 Annual Homeless Assessment Report (AHAR) to Congress. The US Department of Housing and Urban Development website. https://www.huduser.gov/portal/sites/default/files/pdf/2019-AHAR-Part-1.pdf. 2020. Accessed February 1, 2022.
- Spellman B, Khadduri J, Sokol B, et al. Costs Associated with First Time Homelessness for Families and Individuals. US Department of Housing and Urban Development website. https://www.huduser.gov/portal/publications/povsoc/cost_homelessness.html. 2010. Accessed February 1, 2022.
- Report SSAS. 2019. Social Security Administration website. https://www.ssa.gov/policy/docs/statcomps/ssi_asr/2019/index.html. 2020. Accessed February 1, 2022.
- Annual Statistical Report on the Social Security Disability Insurance Program, 2019. Social Security Administration website. https://www.ssa.gov/policy/docs/statcomps/di_asr/2019/index.html. 2020. Accessed February 1, 2022.
- 2019 Uniform Reporting System (URS) Output Tables. Substance Abuse and Mental Health Services Administration: US Department of Health & Human Services. SAMHSA website. https://www.samhsa.gov/data/report/2019-uniform-reporting-system-urs-output-tables. 2020. Accessed February 1, 2022.
- Annual Estimates of the Resident Population for Selected Age Groups by Sex for the Unites States. US Census Bureau. CDC website. https://chronicdata.cdc.gov/w/b2jx-uyck/x389-wqiw?cur=i-SvSpCKOSL&from=-HszoLWj0gc. 2019. Accessed February 1, 2022.
- Labor Force Survey by Sex and Age. Organisation for Economic Cooperation and Development website. https://stats.oecd.org/Index.aspx?DataSetCode=lfs_sexage_i_r. 2019. Accessed February 1, 2022.
- May 2019 National Occupational Employment and Wage Estimates United States. US Bureau of Labor Statistics website. https://www.bls.gov/oes/current/oes_nat.htm. 2022. Accessed February 1, 2022.
- Historical Income Tables—People. US Census Bureau website. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-income-people.html. 2022. Accessed February 1, 2022.
- Goeree R, O’Brien BJ, Blackhouse G, et al. The valuation of productivity costs due to premature mortality: a comparison of the human-capital and friction-cost methods for schizophrenia. Can J Psychiatry. 1999;44(5):455–463. PubMed CrossRef
- Underlying Cause of Death 1999–2019. Center for Disease Control and Prevention WONDER. CDC website. https://wonder.cdc.gov/ucd-icd10.html. 2022. Accessed February 1, 2022.
- Dubois RW. Cost-effectiveness thresholds in the USA: are they coming? are they already here? J Comp Eff Res. 2016;5(1):9–11. PubMed CrossRef
- Correll CU, Brevig T, Brain C. Patient characteristics, burden and pharmacotherapy of treatment-resistant schizophrenia: results from a survey of 204 US psychiatrists. BMC Psychiatry. 2019;19(1):362. PubMed CrossRef
- Velligan DI, Brain C, Bouérat Duvold L, et al. Caregiver burdens associated with treatment-resistant schizophrenia: a quantitative caregiver survey of experiences, attitudes, and perceptions. Front Psychiatry. 2019;10:584. PubMed CrossRef
- McDonell MG, Short RA, Berry CM, et al. Burden in schizophrenia caregivers: impact of family psychoeducation and awareness of patient suicidality. Fam Process. 2003;42(1):91–103. PubMed CrossRef
- Poverty Thresholds for 2019 by Size of Family and Number of Related Children Under 18 Years. US Census Bureau website. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html. 2019. Accessed February 1, 2022.
- Distribution of Certified Nursing Facilities by Certification Type, 2019. National Center for Health Statistics; Contract No: 43; 2019. https://www.kff.org/be48f7e/. Accessed February 1, 2022.
- Tori K, Kalligeros M, Nanda A, et al. Association between dementia and psychiatric disorders in long-term care residents: an observational clinical study. Medicine (Baltimore). 2020;99(31):e21412. PubMed CrossRef
- Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS): Data on Mental Health Treatment Facilities. https://www.samhsa.gov/data/data-we-collect/n-mhss-national-mental-health-services-survey. 2021. Accessed February 1, 2022.
- Mental Health, United States, 2002. Rockville, MD: Substance Abuse and Mental Health Services Administration. Office of Justice Programs website. https://www.ojp.gov/ncjrs/virtual-library/abstracts/mental-health-united-states-2002. 2004. Accessed February 1, 2022.
- Garthwaite C, Gross T, Notowidigdo M. Hospitals as Insurers of Last Resort. Am Econ J Appl Econ. 2018;10(1):1–39. CrossRef
- Societal Costs of Schizophrenia & Related Disorders. Schizophrenia & Psychosis Action Alliance website. Alexandria, VA. https://sczaction.org/wp-content/uploads/2021/11/571-012_WhitePaper_Report_FINAL_updated_11.09.21.pdf. 2021. Accessed February 1, 2022.
This PDF is free for all visitors!