ABSTRACT
Objective: Aiming at revising the therapeutic reference range for olanzapine, the present study highlights the association between blood olanzapine levels, clinical effects, and dopamine D2–receptor occupancy for oral and long-acting injectable (LAI) formulations.
Data Sources: Databases were systematically searched for randomized controlled trials (RCTs) and uncontrolled trials concerning blood olanzapine levels in relation to clinical outcomes or D2-receptor occupancy using MEDLINE (PubMed), Web of Science, PsycINFO, and Cochrane Library (March 2021, updated in December 2021). We excluded articles not written in English or German and non-human data. Search terms included olanzapine, blood level, drug monitoring, PET, and SPECT.
Study Selection: The process of study selection followed a previously published protocol and PRISMA guidelines. A total of 2,824 articles were identified through database search and 1 article via reference list check. Thirty-four studies were suitable for qualitative synthesis, and 13 studies were included in the quantitative analysis.
Data Extraction: Reviewers performed data extraction and quality assessment of the included studies independently following the review protocol.
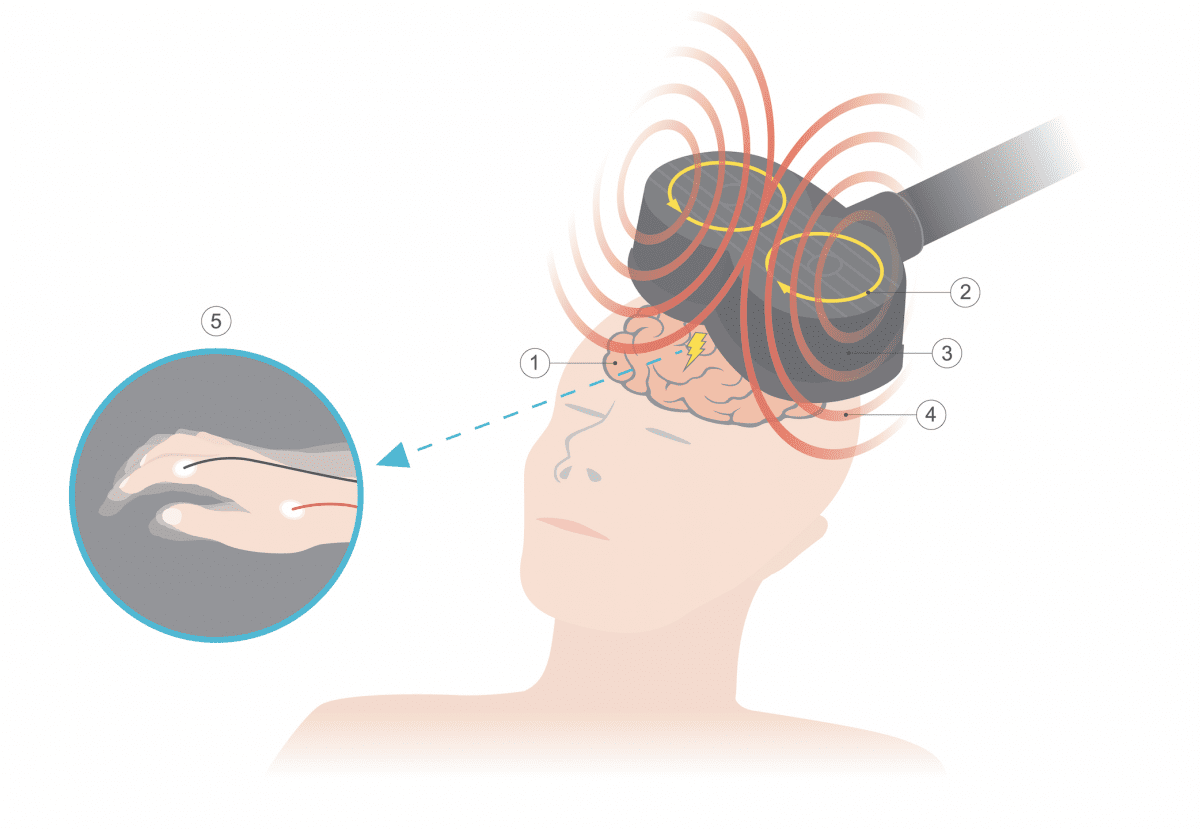
Results: Evidence for a relationship between blood olanzapine level and efficacy/side effects (constipation) is considered low (Level C). In total, 3 studies of moderate quality consistently showed therapeutic thresholds of around 20 ng/mL for olanzapine 12 hours post-dose. This threshold is in line with findings from positron emission tomography (PET) studies that suggest optimal drug efficacy (65%–80% D2-receptor occupancy) between 17 and 44 ng/mL.
Conclusions: We suggest a therapeutic reference range of 20–40 ng/mL for olanzapine oral and LAI formulations. In this range, optimal treatment response is expected in patients with schizophrenia and schizophrenia spectrum disorders. Side effects, especially weight gain, may already occur at therapeutic levels. However, higher plasma concentrations are in general well tolerated and should not necessarily require a dose reduction in case of good response and tolerance.
J Clin Psychiatry 2023;84(5):22r14626
Author affiliations are listed at the end of this article.
Members Only Content
This full article is available exclusively to Professional tier members. Subscribe now to unlock the HTML version and gain unlimited access to our entire library plus all PDFs. If you're already a subscriber, please log in below to continue reading.
References (71)

- Hart XM, Eichentopf L, Lense X, et al. Therapeutic reference ranges for psychotropic drugs: a protocol for systematic reviews. Front Psychiatry. 2021;12:787043. PubMed CrossRef
- Citrome L, McEvoy JP, Todtenkopf MS, et al. A commentary on the efficacy of olanzapine for the treatment of schizophrenia: the past, present, and future. Neuropsychiatr Dis Treat. 2019;15:2559–2569. PubMed CrossRef
- Eli Lilly and Company. ZYYPREXA (olanzapine). Highlights of prescribing information. https://pi.lilly.com/us/zyprexa-pi.pdf. Accessed January 23, 2022.
- Biedermann F, Fleischhacker WW. Psychotic disorders in DSM-5 and ICD-11. CNS Spectr. 2016;21(4):349–354. PubMed CrossRef
- Hilbert A, Hoek HW, Schmidt R. Evidence-based clinical guidelines for eating disorders: international comparison. Curr Opin Psychiatry. 2017;30(6):423–437. PubMed CrossRef
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed CrossRef
- De Hert M, Detraux J, van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8(2):114–126. PubMed CrossRef
- Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225–233. PubMed CrossRef
- Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(01-02):9–62. PubMed CrossRef
- Citrome L, Kantrowitz JT. Olanzapine dosing above the licensed range is more efficacious than lower doses: fact or fiction? Expert Rev Neurother. 2009;9(7):1045–1058. PubMed CrossRef
- Bishara D, Olofinjana O, Sparshatt A, et al. Olanzapine: a systematic review and meta-regression of the relationships between dose, plasma concentration, receptor occupancy, and response. J Clin Psychopharmacol. 2013;33(3):329–335. PubMed CrossRef
- Kapur S, Zipursky R, Jones C, et al. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157(4):514–520. PubMed CrossRef
- Farde L, Wiesel FA, Halldin C, et al. Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry. 1988;45(1):71–76. PubMed CrossRef
- Farde L, Nordström AL, Wiesel FA, et al. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49(7):538–544. PubMed CrossRef
- Detke HC, McDonnell DP, Brunner E, et al. Post-injection delirium/sedation syndrome in patients with schizophrenia treated with olanzapine long-acting injection, I: analysis of cases. BMC Psychiatry. 2010;10(1):43. PubMed CrossRef
- Bushe CJ, Falk D, Anand E, et al. Olanzapine long-acting injection: a review of first experiences of post-injection delirium/sedation syndrome in routine clinical practice. BMC Psychiatry. 2015;15(1):65. PubMed CrossRef
- Alphs L, Gopal S, Karcher K, et al. Are the long-acting intramuscular formulations of risperidone or paliperidone palmitate associated with post-injection delirium/sedation syndrome? an assessment of safety databases. Curr Drug Saf. 2011;6(1):43–45. PubMed CrossRef
- Perry PJ, Sanger T, Beasley C. Olanzapine plasma concentrations and clinical response in acutely ill schizophrenic patients. J Clin Psychopharmacol. 1997;17(6):472–477. PubMed CrossRef
- Mauri MC, Steinhilber CP, Marino R, et al. Clinical outcome and olanzapine plasma levels in acute schizophrenia. Eur Psychiatry. 2005;20(1):55–60. PubMed CrossRef
- Schoretsanitis G, Kane JM, Correll CU, et al; American Society of Clinical Psychopharmacology. Blood levels to optimize antipsychotic treatment in clinical practice: a joint consensus statement of the American Society of Clinical Psychopharmacology and the Therapeutic Drug Monitoring Task Force of the Arbeitsgemeinschaft für Neuropsychopharmakologie und Pharmakopsychiatrie. J Clin Psychiatry. 2020;81(3):19cs13169. PubMed CrossRef
- Taylor DM, Barnes TRE, Young AH. The Maudsley Prescribing Guidelines in Psychiatry. 13th ed. John Wiley & Sons; 2018.
- Schoretsanitis G, Baumann P, Conca A, et al. Therapeutic drug monitoring of long-acting injectable antipsychotic drugs. Ther Drug Monit. 2021;43(1):79–102. PubMed CrossRef
- Junutula SP, Dubasi SK, Reddy Padide SG, et al. Therapeutic drug monitoring of olanzapine: easy and reliable method for clinical correlation. Indian J Pharmacol. 2021;53(1):2–5. PubMed CrossRef
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. PubMed CrossRef
- Hasan A, Bandelow B, Yatham LN, et al; WFSBP Guideline Task Force Chairs. WFSBP guidelines on how to grade treatment evidence for clinical guideline development. World J Biol Psychiatry. 2019;20(1):2–16. PubMed CrossRef
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. PubMed CrossRef
- McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61. PubMed CrossRef
- Lin YC, Ellingrod VL, Bishop JR, et al. The relationship between P-glycoprotein (PGP) polymorphisms and response to olanzapine treatment in schizophrenia. Ther Drug Monit. 2006;28(5):668–672. PubMed CrossRef
- Laika B, Leucht S, Heres S, et al. Pharmacogenetics and olanzapine treatment: CYP1A2*1F and serotonergic polymorphisms influence therapeutic outcome. Pharmacogenomics J. 2010;10(1):20–29. PubMed CrossRef
- Zabala A, Bustillo M, Querejeta I, et al. A pilot study of the usefulness of a single olanzapine plasma concentration as an indicator of early drug effect in a small sample of first-episode psychosis patients. J Clin Psychopharmacol. 2017;37(5):569–577. PubMed CrossRef
- Lu ML, Wu YX, Chen CH, et al. Application of plasma levels of olanzapine and n-desmethyl-olanzapine to monitor clinical efficacy in patients with schizophrenia. PLoS One. 2016;11(2):e0148539. PubMed CrossRef
- Carrillo JA, Herráiz AG, Ramos SI, et al. Role of the smoking-induced cytochrome P450 (CYP)1A2 and polymorphic CYP2D6 in steady-state concentration of olanzapine. J Clin Psychopharmacol. 2003;23(2):119–127. PubMed CrossRef
- Arnaiz JA, Rodrigues-Silva C, Mezquida G, et al; PEPs group. The usefulness of Olanzapine plasma concentrations in monitoring treatment efficacy and metabolic disturbances in first-episode psychosis. Psychopharmacology (Berl). 2021;238(3):665–676. PubMed CrossRef
- Ellingrod VL, Perry PJ, Lund BC, et al. 5HT2A and 5HT2C receptor polymorphisms and predicting clinical response to olanzapine in schizophrenia. J Clin Psychopharmacol. 2002;22(6):622–624. PubMed CrossRef
- Kelly DL, Richardson CM, Yu Y, et al. Plasma concentrations of high-dose olanzapine in a double-blind crossover study. Hum Psychopharmacol. 2006;21(6):393–398. PubMed CrossRef
- Citrome L, Stauffer VL, Chen L, et al. Olanzapine plasma concentrations after treatment with 10, 20, and 40 mg/d in patients with schizophrenia: an analysis of correlations with efficacy, weight gain, and prolactin concentration. J Clin Psychopharmacol. 2009;29(3):278–283. PubMed CrossRef
- Fellows L, Ahmad F, Castle DJ, et al. Investigation of target plasma concentration-effect relationships for olanzapine in schizophrenia. Ther Drug Monit. 2003;25(6):682–689. PubMed CrossRef
- Fekete S, Wewetzer C, Mehler-Wex C, et al. Therapeutic drug monitoring in children and adolescents under pharmacotherapy with olanzapine in daily clinical practice. Ther Drug Monit. 2017;39(3):273–281. PubMed CrossRef
- Nozawa M, Ohnuma T, Matsubara Y, et al. The relationship between the response of clinical symptoms and plasma olanzapine concentration, based on pharmacogenetics: Juntendo University Schizophrenia Projects (JUSP). Ther Drug Monit. 2008;30(1):35–40. PubMed CrossRef
- Raposo NR, Ferreira AS, Gattaz WF. Body mass index increase, serum leptin, adiponectin, neuropeptide Y and lipid levels during treatment with olanzapine and haloperidol. Pharmacopsychiatry. 2011;44(5):169–172. PubMed CrossRef
- Bech P, Gex-Fabry M, Aubry JM, et al. Olanzapine plasma level in relation to antimanic effect in the acute therapy of manic states. Nord J Psychiatry. 2006;60(2):181–182. PubMed CrossRef
- Perry PJ, Lund BC, Sanger T, et al. Olanzapine plasma concentrations and clinical response: acute phase results of the North American Olanzapine Trial. J Clin Psychopharmacol. 2001;21(1):14–20. PubMed CrossRef
- Mauri MC, Maffini M, Di Pace C, et al. “Long-acting” olanzapine in maintenance therapy of schizophrenia: a study with plasma levels. Int J Psychiatry Clin Pract. 2015;19(2):99–105. PubMed CrossRef
- Lane HY, Guo SC, Hwang TJ, et al. Effects of olanzapine plasma concentrations on depressive symptoms in schizophrenia: a pilot study. J Clin Psychopharmacol. 2002;22(5):530–532. PubMed CrossRef
- Italiano D, Bruno A, Santoro V, et al. Generic olanzapine substitution in patients with schizophrenia: assessment of serum concentrations and therapeutic response after switching. Ther Drug Monit. 2015;37(6):827–830. PubMed CrossRef
- Veselinović T, Scharpenberg M, Heinze M, et al; NeSSy Study Group. Dopamine D2 receptor occupancy estimated from plasma concentrations of four different antipsychotics and the subjective experience of physical and mental well-being in schizophrenia: results from the randomized NeSSy Trial. J Clin Psychopharmacol. 2019;39(6):550–560. PubMed CrossRef
- Kapur S, Zipursky RB, Remington G, et al. 5-HT2 and D2 receptor occupancy of olanzapine in schizophrenia: a PET investigation. Am J Psychiatry. 1998;155(7):921–928. PubMed CrossRef
- Kapur S, Zipursky RB, Remington G. Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am J Psychiatry. 1999;156(2):286–293. PubMed CrossRef
- Catafau AM, Penengo MM, Nucci G, et al; Barcelona Clinical Imaging in Psychiatry Group. Pharmacokinetics and time-course of D(2) receptor occupancy induced by atypical antipsychotics in stabilized schizophrenic patients. J Psychopharmacol. 2008;22(8):882–894. PubMed CrossRef
- Attarbaschi T, Sacher J, Geiss-Granadia T, et al. Striatal D(2) receptor occupancy in bipolar patients treated with olanzapine. Eur Neuropsychopharmacol. 2007;17(2):102–107. PubMed CrossRef
- Arakawa R, Ito H, Okumura M, et al. Extrastriatal dopamine D(2) receptor occupancy in olanzapine-treated patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2010;260(4):345–350. PubMed CrossRef
- Graff-Guerrero A, Rajji TK, Mulsant BH, et al. Evaluation of antipsychotic dose reduction in late-life schizophrenia: a prospective dopamine D2/3 receptor occupancy study. JAMA Psychiatry. 2015;72(9):927–934. PubMed CrossRef
- Mamo D, Kapur S, Keshavan M, et al. D2 receptor occupancy of olanzapine pamoate depot using positron emission tomography: an open-label study in patients with schizophrenia. Neuropsychopharmacology. 2008;33(2):298–304. PubMed CrossRef
- McDonnell DP, Landry J, Detke HC. Long-term safety and efficacy of olanzapine long-acting injection in patients with schizophrenia or schizoaffective disorder: a 6-year, multinational, single-arm, open-label study. Int Clin Psychopharmacol. 2014;29(6):322–331. PubMed CrossRef
- Lutz R, Köhnlein O, Schmauss M, et al. [Management of the atypical antipsychotic olanzapine in a clinical environment with particular regard to therapeutic drug monitoring (TDM) in a German State hospital]. (Zum Umgang mit dem modernen atypischen Neuroleptikum Olanzapin im klinischen Alltag unter besonderer Berücksichtigung des Therapeutischen Drug-Monitorings (TDM) (an einer psychiatrischen Versorgungsklinik))Psychiatr Prax. 2004;31(suppl 1):S181–S183. PubMed CrossRef
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems. WHO website. https://icd.who.int/. Accessed October 21, 2021.
- Olesen OV, Linnet K. Olanzapine serum concentrations in psychiatric patients given standard doses: the influence of comedication. Ther Drug Monit. 1999;21(1):87–90. PubMed CrossRef
- Xiao T, Wang Z, Li G, et al. What to do about missed doses? a retrospective study of olanzapine in the elderly. Drug Des Devel Ther. 2021;15:3411–3423. PubMed CrossRef
- Baldelli S, Mauri MC, Di Pace C, et al. Intraindividual and interindividual variability of olanzapine trough concentrations in patients treated with the long-acting injectable formulation. J Clin Psychopharmacol. 2018;38(4):365–369. PubMed CrossRef
- Korell J, Green B, Rae A, et al. Determination of plasma concentration reference ranges for oral aripiprazole, olanzapine, and quetiapine. Eur J Clin Pharmacol. 2018;74(5):593–599. PubMed CrossRef
- Callaghan JT, Bergstrom RF, Ptak LR, et al. Olanzapine: pharmacokinetic and pharmacodynamic profile. Clin Pharmacokinet. 1999;37(3):177–193. PubMed CrossRef
- Batail JM, Langrée B, Robert G, et al. Use of very-high-dose olanzapine in treatment-resistant schizophrenia. Schizophr Res. 2014;159(2-3):411–414. PubMed CrossRef
- Kang D, Lu J, Liu W, et al. Association between olanzapine concentration and metabolic dysfunction in drug-naive and chronic patients: similarities and differences. Schizophrenia (Heidelb). 2022;8(1):9. PubMed CrossRef
- Faden J, Serdenes R, Citrome L. Olanzapine-samidorphan combination tablets for the treatment of schizophrenia and bipolar I disorder - what is it, and will it be used? Expert Rev Neurother. 2022;22(5):365–376. PubMed CrossRef
- Leucht S, Crippa A, Siafis S, et al. Dose-response meta-analysis of antipsychotic drugs for acute schizophrenia. Am J Psychiatry. 2020;177(4):342–353. PubMed CrossRef
- Uchida H, Suzuki T, Takeuchi H, et al. Low dose vs standard dose of antipsychotics for relapse prevention in schizophrenia: meta-analysis. Schizophr Bull. 2011;37(4):788–799. PubMed CrossRef
- Zernig G, Hiemke C. Pharmacokinetic and Pharmacodynamic Principles. In: Riederer P, Laux G,Nagatsu T, et al, eds. NeuroPsychopharmacotherapy, Springer, Cham. 2020:1–19. doi:https://doi.org/10.1007/978-3-319-56015-1_1-1
- Agid O, Kapur S, Arenovich T, et al. Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003;60(12):1228–1235. PubMed CrossRef
- Hiemke C. Concentration-effect relationships of psychoactive drugs and the problem to calculate therapeutic reference ranges. Ther Drug Monit. 2019;41(2):174–179. PubMed CrossRef
- Schoretsanitis G, de Leon J. Best practices for starting clozapine in patients with schizophrenia: how to switch from the prior antipsychotic(s). J Clin Psychiatry. 2022;83(4):22ac14500. PubMed CrossRef
- Bezchlibnyk-Butler KZ, Remington GJ. Antiparkinsonian drugs in the treatment of neuroleptic-induced extrapyramidal symptoms. Can J Psychiatry. 1994;39(2):74–84. PubMed CrossRef