Abstract
Objective: Irritability is a debilitating, transdiagnostic symptom in adolescents spanning internalizing and externalizing disorders, and early reduction in irritability with antidepressant treatments has been seen as a positive prognostic sign in depression recovery. There are substantial knowledge gaps regarding how transcranial magnetic stimulation (TMS) treatments impact irritability.
Methods: This exploratory study sought to investigate the relationship between irritability and depressive symptoms in adolescents with a DSM-5 diagnosis of major depressive disorder (MDD) undergoing treatment with 2 different doses of TMS. Participants aged 12–18 years (N = 41) underwent 6 weeks of treatment (30 sessions) in a double-blind, randomized trial of 1 Hz vs. 10 Hz TMS for the treatment of MDD. The clinical trial was conducted from September 24, 2018, through March 3, 2023. A linear mixed model was used to assess the change in irritability (assessed with item 8 on the Children’s Depression Rating Scale Revised) throughout the treatment course, and a logistic regression was implemented to examine the relationship between early (week 4) irritability improvements and a posttreatment Clinical Global Impressions-Improvement (CGI-I) score.
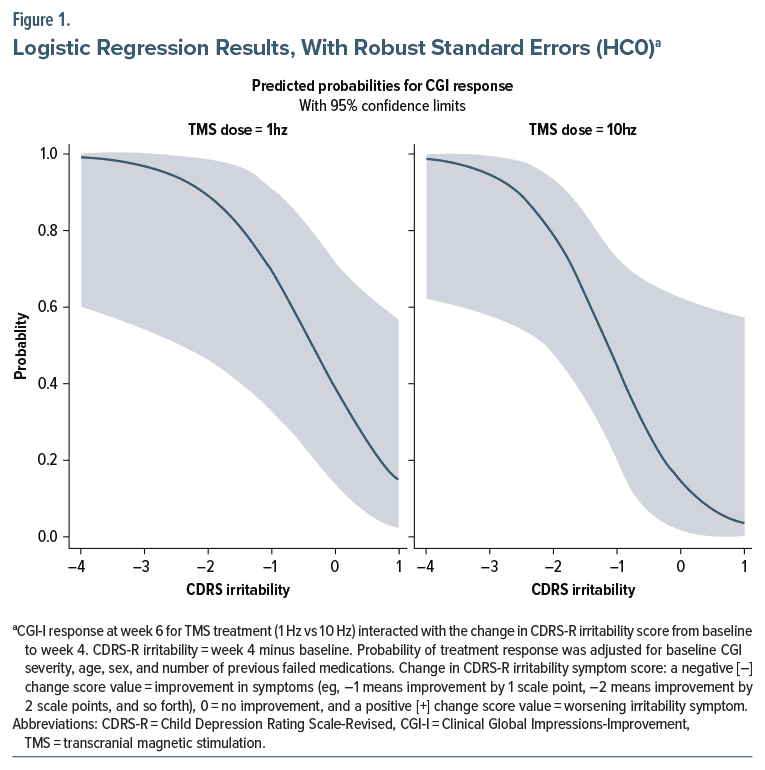
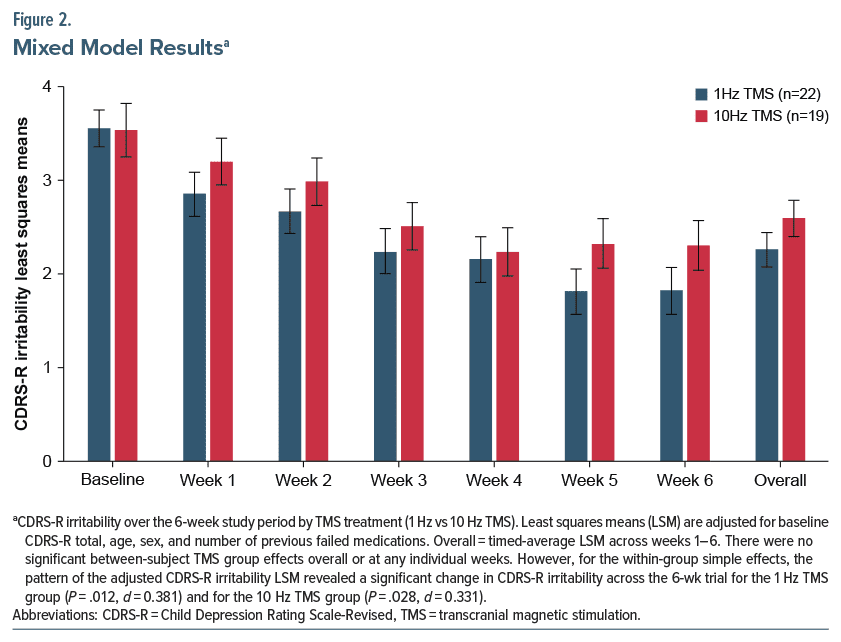
Results: Irritability significantly improved during the course of TMS treatments in conjunction with overall depression improvement across the 6 week trial for the 1 Hz TMS group (P = .0120, d =0.381) and for the 10 Hz TMS group (P = .0288, d = 0.331). There was a significant negative (inverse) relationship between the change in irritability symptoms and CGI-I response for the 10 Hz TMS group (δ log odds = −1.5474, SE = 0.7343, P = .0351) and for the 1 Hz TMS group (δ log odds = −1.2852, SE = 0.5656, P = .0231).
Conclusion: These results suggest that irritability is an important correlate of disease severity and predictor of treatment response for MDD in adolescents, replicating similar results found in trials using antidepressant medications. Future research should focus on incorporating assessments of irritability into clinical decision-making and intervention discovery for transdiagnostic symptoms of irritability in youth and adolescents.
Clinical Trial Registration: Data used in this secondary analysis came from ClinicalTrials.gov identifier: NCT03363919.
J Clin Psychiatry 2025;86(2):24m15684
Author affiliations are listed at the end of this article.
Irritability in youth is a transdiagnostic symptom defined as a low threshold for experiencing anger in response to frustration,1 and it is among the most common reasons why families seek treatment for youth.2 Along with depressed mood and anhedonia, irritability is a cardinal mood symptom for depression in adolescents and is a criterion for the diagnosis of major depressive disorder (MDD) in the DSM-5.3 Irritability is a potential bridge symptom between depressive and anxious symptoms in adolescent psychiatry that is present in many other DSM-5 diagnoses and likely is a central symptom related to functional impairment across diagnoses.4 Research on the treatment of irritability as a standalone construct is in its infancy in adolescent samples,5 but irritability can respond to a variety of pharmacologic and nonpharmacologic treatments within specific diagnostic samples.6 Transcranial magnetic stimulation (TMS) is a noninvasive neuromodulation therapy which has received US Food and Drug Administration clearance for the adjunctive treatment of depression in adolescents aged 15–21 years. Prior work suggests that TMS interventions can reduce irritability co-occurring with depression in adults,7 but no studies have been published in depressed adolescents, and the most effective TMS protocol for reducing irritability is unknown.
Irritability appears to have a predictive relationship with clinical outcomes in the context of both adolescent and adult depression. Early reductions in irritability are strongly associated with better outcomes in youths with depression, regardless of baseline depression severity, across a variety of medications.8 Baseline-to-week-four changes in irritability predicted antidepressant treatment outcomes in a large sample of adults with major depression.9 However, since the majority of the literature comes from trials using selective serotonin reuptake inhibitors (SSRIs), it is unclear whether early changes in irritability serve as a prognostic indicator for a subtype of adolescent mood disorder responsive to a specific medication, or whether irritability can demonstrate a broader association with disease severity and ultimate response.10 A replication of this relationship in patients treated with TMS would provide additional support for the role of irritability as a predictor of symptom response in the treatment of MDD in adolescents.
Given the importance of irritability within adolescent depression, it is essential to better understand both its own response to treatment and its connection to later depression outcomes in adolescent samples. To our knowledge, this is the first study that examines the trajectory of irritability symptoms in adolescents with depression undergoing TMS. The aim of this study was to analyze whether an early change in irritability is predictive of TMS antidepressant response. The secondary aim was to determine whether TMS impacted irritability significantly throughout the treatment course. We hypothesized that an early improvement in irritability would predict treatment response, similar to the relationship seen in pharmacologic studies, and that TMS would significantly impact irritability independent of depression symptom changes.
METHODS
Procedures and Measures
Participants. This study is a secondary analysis of a double blind, randomized trial of 1 Hz and 10 Hz repetitive TMS for adolescents with depression.11 The clinical trial was conducted from September 24, 2018, through March 3, 2023. Participants in this analysis were 41 children and adolescents (ages 12–18 years) with depressive symptom severity corresponding to a score of 40 or greater on the Children’s Depression Rating Scale-Revised (CDRS-R).12 Participants were not taking antidepressants or other psychotropic medications during the study and were excluded if comorbid psychiatric or neurological disorders were present in the past year. Full inclusion and exclusion criteria have been published elsewhere.11 Participants were randomized to either 1 Hz TMS with 2,400 continuous pulses per session at 120% motor threshold or 10 Hz TMS with 4 seconds on and 36 seconds off for 2,400 pulses each session at 120% of resting motor threshold over left dorsolateral prefrontal cortex (LDLPFC). TMS protocols were delivered using the NeuroStar Advanced Therapy System. Treatment was given 5 days per week for 6 weeks, for a total of 30 sessions. Participants who completed less than 1 week of treatment were excluded from all analyses as there were no follow-up clinical assessments. This study was approved by the Mayo Clinic Institutional Review Board, and both participants and parents/guardians provided informed assent and consent before any study activities, and the study was registered at ClinicalTrials.gov (identifier: NCT03363919).13
Assessments. The details of all measurements collected can be found in the original manuscript.11 In the present study, the primary assessments used were the 17-item CDRS-R scale which was administered at baseline and weekly for the 6 weeks of treatment and the Clinical Global Impressions-Improvement (CGI-I) which was administered at baseline, week 4, and posttreatment. The primary outcome of treatment response was defined as a score of 1 or 2 on the CGI-I scale at week 6.13 Irritability was defined using item 8 of the CDRS-R scale, in which the clinician rates “irritability” based on both adolescent and parent reports by indicating one of the following: 1=rarely irritable; 3=easily irritable, periods of irritability occur several times a week but do not last long; 5=frequently irritable, extended periods of irritability occur several times a week and are difficult to break out of; 7=constant experience of irritability, nothing changes this mood. Total CDRS-R scores minus the irritability item were used to estimate the severity of all other depression dimensions.
Statistical analysis. A logistic regression was implemented to examine the relationship between CGI-I treatment response at week 6 (as the binary outcome) and the change in CDRS-R irritability symptoms from baseline to week 4. The model contained fixed effects terms for TMS treatment, change in irritability symptoms, and TMS treatment×change in irritability symptoms interaction. Baseline CGI severity, age, sex at birth, and number of previously failed medication trials (a measure of treatment resistance) were included as covariates in the model. In addition, the change in CDRS-R irritability over the 6-week study period was compared between the TMS treatment groups using a linear mixed model analysis of repeated measures. The mixed model contained fixed effects terms for TMS treatment, time, and TMS treatment×time interaction. Baseline CDRS-R total, time-varying CDRS-R total minus irritability item, age, sex, and number of previously failed medication trials were included as covariates in the model. Restricted maximum likelihood estimation along with Type 3 tests of fixed effects were used with the Kenward-Roger correction applied to the autoregressive (AR1) covariance structure. Least squares (LS) means were estimated as part of the mixed model in order to interpret the TMS group effect (LS mean difference between groups). Simple TMS group effects at each time period as well as within-group change over the 6 weeks were also assessed. Cohen d was calculated and interpreted as the effect size estimator. Statistical analyses were carried out using SAS software, Version 9.4.14 The level of significance was set at α=0.05 (2-tailed).
RESULTS
Summary of Participant Characteristics
A full description of the study participants’ characteristics can be found elsewhere.11 Of the 41 youth, 60.98% were female, 82.92% were white, and the mean age was 15.78 years (range 12–18 years). The 10 Hz and 1 Hz treatment groups did not significantly differ on any demographic or clinical characteristics. Of the 36 youth that completed all 6 weeks of treatment, 61.11% showed CGI-I rated response. In the 10 Hz group, 9 of 17 (52.94%) responded, and in the 1 Hz group, 13 of 19 (68.42%) responded.
Prediction of Response
The results from the logistic regression revealed a significant negative (inverse) relationship between the change in irritability symptoms and CGI-I response for the 10 Hz TMS group (δ log odds = −1.5474, SE = 0.7343, P = .0351) and for the 1 Hz TMS group (δ log odds = −1.2852, SE = 0.5656, P = .0231). In other words, as CDRS-R irritability symptoms improved over the first 4 weeks, the probability of CGI-I response at week 6 increased for both the 1 Hz and 10 Hz TMS groups. However, there was no significant interaction between the TMS treatment group and change in irritability symptoms on CGI-I response (P = .7323). Thus, TMS stimulus frequency (1 Hz vs 10 Hz) did not moderate the relationship between the change in irritability symptoms and CGI-I response. Although this suggests that an improvement in irritability symptoms by week 4 predicts subsequent response to TMS treatment irrespective of TMS frequency, examination of Figure 1 shows that a greater probability of treatment response was observed at lower levels of change in irritability symptoms (eg −1 to 1) for the 1 Hz TMS frequency vs the 10 Hz TMS frequency.
Improvement in Irritability
The mixed model repeated measures analysis revealed that there was no significant TMS treatment group by period interaction effect (P = .8356) as well as no significant main effects of TMS group (P = .3350) and period (P = .5165) on CDRS-R irritability. Although not significant, the pattern of the overall LS TMS treatment group means over the 6-week trial showed that adjusted CDRS-R irritability was lower for the 1 Hz TMS group versus the 10 Hz TMS group (2.295 [SE= 0.175] vs 2.549 [SE = 0.187], P = .3350; d = 0.293). Moreover, for the within-group simple effects, the pattern of the adjusted CDRS-R irritability LS means revealed no significant change (or improvement) in CDRS-R irritability across the 6 week trial for the 1 Hz TMS group (P = .6263, d = 0.073) and for the 10 Hz TMS group (P = .6515, d = 0.068) when change in CDRS-R total minus irritability was accounted for. The simple TMS treatment group effects at the individual weeks also revealed no significant TMS group differences (Ps < 0.7671). However, if the time-varying CDRS-R total minus irritability item is removed from the model, the pattern of adjusted CDRS-R irritability LS means now revealed a significant change in CDRS-R irritability across the 6 week trial for the 1 Hz TMS group (P = .0120, d = 0.381) and for the 10 Hz TMS group (P = .0288, d = 0.331, Figure 2).
DISCUSSION
The goal of this study was to examine the trajectories of irritability symptoms in adolescents undergoing 1 Hz and 10 Hz TMS for the treatment of depression. Through this secondary analysis, we found that an early (week 4) improvement in irritability symptoms was predictive of treatment response at week 6, irrespective of TMS treatment group (frequency) or initial depression severity. These results align with current evidence that early improvements in irritability are predictive of antidepressant treatment response.8,9 However, by replicating this relationship using TMS instead of antidepressant medications such as in previous research, we were able to show that changes in irritability are associated with later treatment response broadly within adolescent depression, instead of solely within a phenotype responsive to SSRIs.15 These results may be valuable for clinician decision-making in treatment courses for adolescent depression because irritability changes appear to be a robust early predictor of treatment success. Depression in adolescents is associated with adverse outcomes in adulthood and causes more disability for young people than any other disease.16,17 Therefore, early identification and intervention for depression in youth and adolescents should be a priority, and analyzing irritability as a treatment prognostic indicator could be an invaluable tool.
In addition, we found that treatment significantly improved irritability symptoms in both 1 Hz and 10 Hz groups. This extends the findings from a previous study, which found that 10 Hz TMS reduces irritability co occurring with depression in adults.18 However, this relationship found in the current study is attenuated when controlling for changes in other depression symptom dimensions. This suggests that while TMS has a positive impact on irritability in adolescents, the relationship cannot be separated from the impact of TMS on overall illness severity. As irritability is a core dimension of depression in adolescents, it is unclear whether irritability improves as an indicator of resolved underlying psychopathology, or whether it is impacted through a separate process. However, functional neuroimaging studies in adolescents have demonstrated that irritability is associated with both altered activation and connectivity in regions associated with reward processing and threat processing (eg, amygdala, anterior cingulate cortex [ACC], and prefrontal cortex [PFC]),10 and TMS delivered to the DLPFC has been previously shown to induce directional functional connectivity changes between the DLPFC, ACC, and other salience network regions.19 Therefore, it is possible, but speculative, that TMS-induced changes to these neural networks could benefit adolescent patients with irritability, even in the absence of depressive symptoms. The lack of distinct association may have been related to the sample size, sample homogeneity, and related statistical power for this exploratory study. It is also possible that the relationship could not be separated because TMS impacts both depression and irritability, and while improvements in irritability are a promising signal of antidepressant effect, it may also improve in the absence of depressive symptoms.
We found that 1 Hz TMS demonstrated numerically higher changes in irritability than 10 Hz, but this difference was not statistically significant. This presents providers with multiple options for the treatment of adolescent irritability and depression, although prospective studies with larger sample sizes may be beneficial to corroborate that both treatments are equivalent in their relationship to irritability. Notably, 1 Hz TMS may be more tolerable and safer compared to 10 Hz, while providing similar results.11,20,21 In addition, low frequency TMS has been found to effectively decrease irritability in other samples, especially children with autism spectrum disorder (ASD).22–24 While these studies were in younger ages than our sample, it is promising to see a similar pattern in the response of irritability to 1 Hz TMS. This study provides preliminary evidence that it may be a suitable treatment for irritability in a broader range of adolescents, and future studies should continue to explore the utility of 1 Hz TMS in other pediatric and adolescent samples with irritability.
Irritability is a dimensional symptom present in adolescent diagnoses of depression, bipolar disorder, disruptive mood dysregulation disorder (DMDD), disruptive behavior disorder, and others.25,26 Elevated irritability in childhood and adolescence often will presage adverse outcomes such as psychiatric diagnoses or suicidal ideation.27–29 As the trajectory of irritability plays a crucial role in other psychiatric presentations, it will be important to develop better interventions for childhood irritability. In mood disorders, medications with various mechanisms of action have been applied with equally heterogeneous methods, with some effects found on measures of irritability.30 Studies in both children and adults have demonstrated positive effects of antidepressant pharmacotherapies of multiple mechanisms on irritability,31–33 and these current results add that TMS antidepressant therapy also shares a similar relationship. As DMDD, of which irritability is the main construct, is classified as a depressive disorder in the DSM-5, further research should examine the utility of antidepressant treatments in addressing irritability.10,30,34 A survey of psychiatrists revealed that SSRIs are a common treatment for DMDD, especially in the absence of comorbid ADHD.35 As TMS is considered a safe add on therapy for adolescents with MDD and is an emerging treatment for other conditions such as ADHD and ASD, it may be valuable to consider TMS especially in cases of treatment resistant irritability.36,37 Our results demonstrate preliminary evidence that both 1Hz and 10Hz TMS may provide clinical benefit in these situations.
There are limitations of this report. As the findings of this report are based on an unplanned secondary analysis, they should be considered preliminary and require confirmation in other samples of patients with depression. The small size and homogeneous nature of Jthe sample also limited statistical power in this analysis and generalizability. In addition, while irritability was measured using a validated item, the future use of a multidimensional scale, such as the Affective Reactivity Index questionnaire, would provide more detailed irritability ratings in future research.38
CONCLUSION
This analysis found that treatment with either 1 Hz or 10 Hz TMS improved irritability in conjunction with improvement in adolescent depressive symptoms, and improvement in irritability at 4 weeks predicted antidepressant response after 6 weeks of TMS. These results suggest that early improvements in irritability could be an indicator of clinical response to TMS, and the potential of TMS to treat transdiagnostic adolescent irritability could be a useful avenue for future research.
Article Information
Published Online: April 9, 2025. https://doi.org/10.4088/JCP.24m15684
© 2025 Physicians Postgraduate Press, Inc.
Submitted: October 25, 2024; accepted January 23, 2025.
To Cite: Delaney K, Nakonezny PA, Buyuktaskin D, et al. Trajectories of irritability improvement in depressed adolescents treated with 1 Hz and 10 Hz transcranial magnetic stimulation. J Clin Psychiatry 2025;86(2):24m15684.
Author Affiliations: Department of Molecular Pharmacology and Therapeutics, Mayo Clinic, Rochester, Minnesota (Delaney, Athreya and Croarkin); Department of Biostatistics, Peter O’Donnell Jr. School of Public Health, and Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, Texas (Nakonezny); Department of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota (Buyuktaskin, Sangster Carrasco, Athreya, Romanowicz, Shekunov, Vande Voort, and Croarkin).
Corresponding Author: Paul E. Croarkin, DO, MS, 200 First St SW, Rochester, MN 55905 ([email protected]).
Relevant Financial Relationships: Dr Croarkin has received research support from the National Institutes of Health (NIH), National Science Foundation (NSF), Agency for Healthcare Research and Quality (AHRQ), Brain and Behavior Research Foundation, the Mayo Clinic Foundation, and Pfizer, Inc; has received grant-in-kind equipment support from Neuronetics, Inc and MagVenture, Inc. for investigator-initiated studies; received grant-in-kind supplies and genotyping from Assurex Health, Inc. for an investigator-initiated study; served as the principal investigator for a multicenter study funded by Neuronetics Inc, a site principal investigator for a study funded by NeoSync, Inc, and site principal investigator for a study funded by Innosphere; served as a paid consultant for Engrail Therapeutics, Meta Platforms, Inc, MindMed, Myriad Neuroscience, Procter & Gamble Company, and Sunovion; is employed by Mayo Clinic; and receives compensation as the Editor-in-Chief for the Journal of Child and Adolescent Psychopharmacology. Dr Vande Voort has received grant-in-kind supplies and genotyping from Assurex Health for an investigator-initiated study. Dr Buyuktaskin is supported by the Scientific and Technological Research Council of Türkiye. The other authors have no disclosures to report.
Funding/Support: This project was funded by the National Institute of Mental Health (NIMH) under Award Number R01MH113700, Bethesda, Maryland. Neuronetics, Inc., Malvern, Pennsylvania, provided device and equipment support through a grant-in kind. The NIMH and Neuronetics had no role in the design, analysis, interpretation, or publication of this study.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or NIMH.
Previous Presentation: Presented at the American College of Neuropsychopharmacology annual meeting; December 8–11, 2024; Phoenix, Arizona.
ORCID: Karina Delaney: https://orcid.org/0009-0004-5052-167X; Dicle Buyuktaskin: https://orcid.org/0000-0003-4679-3846; Lucero Sangster Carrasco: https://orcid.org/0000-0002-4073-0521; Arjun P. Athreya: https://orcid.org/0000-0001-9764-1768; Magdalena Romanowicz: https://orcid.org/0000-0002-4916-0625; Julia Shekunov: https://orcid.org/0000-0002-9685-3539; Jennifer L. Vande Voort: https://orcid.org/0000-0002-3630-4773; Paul E. Croarkin: https://orcid.org/0000-0001-6843-6503
Clinical Points
- While irritability is a core element of adolescent depression, the effect of transcranial magnetic stimulation (TMS) treatment on irritability in this population is unknown.
- Both 1 Hz and 10 Hz TMS appeared to improve irritability in conjunction with improvement in depressive symptoms in a sample of adolescents with depression.
- Early improvements in irritability are predictive of later depression treatment response with TMS in adolescents with depression.
Editor’s Note: We encourage authors to submit papers for consideration as a part of our Focus on Childhood and Adolescent Mental Health section. Please contact Karen D. Wagner, MD, PhD, at psychiatrist.com/contact/wagner.
References (38)

- Brotman MA, Kircanski K, Leibenluft E. Irritability in children and adolescents. Annu Rev Clin Psychol. 2017;13:317–341. CrossRef
- Evans SC, Corteselli KA, Edelman A, et al. Is irritability a top problem in youth mental Health care? A multi-informant, multi-method investigation. Child Psychiatry Hum Dev. 2023;54(4):1027–1041. CrossRef
- Stringaris A, Maughan B, Copeland WS, et al. Irritable mood as a symptom of depression in youth: prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2013;52(8):831–840. PubMed CrossRef
- Li P, Huang N, Yang X, et al. A simulation-based network analysis of intervention targets for adolescent depressive and anxiety symptoms. Asian J Psychiatr. 2024;99:104152. CrossRef
- Brotman MA, Kircanski K, Stringaris A, et al. Irritability in youths: a translational model. Am J Psychiatry. 2017;174(6):520–532. CrossRef
- Breaux R, Baweja R, Eadeh HM, et al. Systematic review and meta-analysis: pharmacological and nonpharmacological interventions for persistent nonepisodic irritability. J Am Acad Child Adolesc Psychiatry. 2023;62(3):318–334. CrossRef
- Pridmore S, Rybak M, Morey R, et al. The impact of transcranial magnetic stimulation (TMS) on irritability occurring with acute major depressive disorder (MDD). Australas Psychiatry. 2021;29(2):218–221. CrossRef
- Mohamed AK, Croarkin PE, Jha MK, et al. Early reduction in irritability is associated with improved outcomes among youth with depression: findings from the AMOD study. J Affect Disord. 2023;324:77–81. CrossRef
- Jha MK, Minhajuddin A, South C, et al. Irritability and its clinical utility in major depressive disorder: prediction of individual-level acute-phase outcomes using early changes in irritability and depression severity. Am J Psychiatry. 2019;176(5):358–366. CrossRef
- Bell E, Boyce P, Porter RJ, et al. Irritability in mood disorders: neurobiological underpinnings and implications for pharmacological intervention. CNS Drugs. 2021;35(6):619–641. CrossRef
- Lewis CP, Nakonezny PA, Sonmez AI, et al. A dose-finding, biomarker validation, and effectiveness study of transcranial magnetic stimulation for adolescents with depression. J Am Acad Child Adolesc Psychiatry. 2024:S0890-8567(24)01839- 2. doi:10.1016/j.jaac.2024.08.487. CrossRef
- Poznanski EO, Mokros HB; Western Psychological Services (Firm). Children’s Depression Rating Scale–Revised (CDRS-R). WPS; 1996.
- Croarkin PE. Glutamatergic and GABAergic Biomarkers in rTMS for Adolescent Depression. Accessed October 5, 2023. https://reporter.nih.gov/project-details/10169516
- SAS software, version 9.4. SAS Institute Inc; 2016.
- Bell E, Malhi GS. Irritability: an inability, or an ability? Aust N Z J Psychiatry. 2020;54(12):1232–1233. PubMed CrossRef
- Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102. PubMed CrossRef
- Hetrick SE, McKenzie JE, Bailey AP, et al. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. 2021;5(5):CD013674.
- Pridmore S, Turnier-Shea Y, Erger S, et al. The impact of “cluster maintenance TMS” on irritability occurring in major depressive disorder. Australas Psychiatry. 2021;29(2):222–225. CrossRef
- Downar J, Siddiqi SH, Mitra A, et al. Mechanisms of action of TMS in the treatment of depression. Curr Top Behav Neurosci. 2024;66:233–277.
- Chen J, Zhou C, Wu B, et al. Left versus right repetitive transcranial magnetic stimulation in treating major depression: a meta-analysis of randomised controlled trials. Psychiatry Res. 2013;210(3):1260–1264. PubMed CrossRef
- Miron JP, Sheen J, Mansouri F, et al. The role of low-frequency repetitive transcranial magnetic stimulation in major depression: a call to increase the evidence base. Brain Stimul. 2020;13(5):1296–1297. PubMed CrossRef
- Sokhadze EM, El-Baz A, Baruth J, et al. Effects of low frequency repetitive transcranial magnetic stimulation (rTMS) on gamma frequency oscillations and event-related potentials during processing of illusory figures in autism. J Autism Dev Disord. 2009;39(4):619–634. PubMed CrossRef
- Wang Y, Hensley MK, Tasman A, et al. Heart rate variability and skin conductance during repetitive TMS course in children with autism. Appl Psychophysiol Biofeedback. 2016;41(1):47–60. CrossRef
- Casanova MF, Baruth JM, El-Baz A, et al. Repetitive transcranial magnetic stimulation (rTMS) modulates event-related potential (ERP) indices of attention in autism. Transl Neurosci. 2012;3(2):170–180.
- Breda M, Ardizzone I. Irritability in developmental age: a narrative review of a dimension crossing paediatric psychopathology. Aust N Z J Psychiatry. 2021;55(11):1039–1048. CrossRef
- Guzick AG, Geller DA, Small BJ, et al. Irritability in children and adolescents with OCD. Behav Ther. 2021;52(4):883–896. CrossRef
- Silver J, Sorcher L, Carlson GA, et al. Irritability across adolescence: examining longitudinal trajectory, stability, and associations with psychopathology and functioning at age 18. J Affect Disord. 2024;354:611–618. CrossRef
- Sorcher LK, Goldstein BL, Finsaas MC, et al. Preschool irritability predicts adolescent psychopathology and functional impairment: a 12-year prospective study. J Am Acad Child Adolesc Psychiatry. 2022;61(4):554–564 e1. CrossRef
- Srinivasan R, Flouri E, Lewis G, et al. Changes in early childhood irritability and its association with depressive symptoms and self-harm during adolescence in a nationally representative United Kingdom birth cohort. J Am Acad Child Adolesc Psychiatry. 2024;63(1):39–51. CrossRef
- Yager J. Irritability disorders in adults: diagnostic categories missing in plain sight? J Nerv Ment Dis. 2020;208(6):459–465.
- Kim S, Boylan K. Effectiveness of antidepressant medications for symptoms of irritability and disruptive behaviors in children and adolescents. J Child Adolesc Psychopharmacol. 2016;26(8):694–704. CrossRef
- Jha MK, Minhajuddin A, Chin Fatt C, et al. Improvements in irritability with sertraline versus placebo: findings from the EMBARC study. J Affect Disord. 2020;275:44–47. PubMed CrossRef
- Peters EMBR. Irritability in a mixed sample of patients with unipolar and bipolar II depression predicts responsiveness to lamotrigine. Person Med Psychiatry. 2018;2018(7–8):27–30.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association Publishing; 2013.
- Boudjerida A, Guile JM, Breton JJ, et al. A Delphi consensus among experts on assessment and treatment of disruptive mood dysregulation disorder. Front Psychiatry. 2023;14:1166228.
- Cao P, Li Y, An B, et al. Efficacy and safety of repetitive transcranial magnetic stimulation combined with antidepressants in children and adolescents with depression: a systematic review and meta-analysis. J Affect Disord. 2023;336:25–34. CrossRef
- Doruk Camsari D, Kirkovski M, Croarkin PE. Therapeutic applications of noninvasive neuromodulation in children and adolescents. Psychiatr Clin North Am. 2018;41(3):465–477. CrossRef
- Evans SC, Abel MR, Doyle RL, et al. Measurement and correlates of irritability in clinically referred youth: further examination of the Affective Reactivity Index. J Affect Disord. 2021;283:420–429. CrossRef
This PDF is free for all visitors!