Abstract
Objective: To further characterize the efficacy of oral xanomeline and trospium chloride in the treatment of agitation associated with schizophrenia.
Methods: Analyses were performed on the change from baseline of the Positive and Negative Syndrome Scale-Excited Component (PANSS-EC; composed of excitement, tension, hostility, uncooperativeness, and poor impulse control items) data from the 5-week, randomized, double-blind, placebo controlled, inpatient EMERGENT-1, EMERGENT-2, and EMERGENT-3 trials of xanomeline/trospium in adults with schizophrenia with a recent worsening of psychosis requiring hospitalization. The 3 trials met the primary endpoint of reduction from baseline to week 5 in PANSS total score. Data were analyzed from individual studies and were also pooled.
Results: The population comprised 640 participants from the pivotal trials which were conducted from September 2018 to December 2022. PANSS-EC scores were significantly reduced with xanomeline/trospium vs placebo at week 5 across all 3 EMERGENT trials. In EMERGENT-1, xanomeline/trospium (n = 83) was statistically significantly superior (Cohen’s d =0.62, P = .0002) to placebo (n = 87) in improvement (decrease) of PANSS-EC score at week 5. In EMERGENT-2, xanomeline/trospium (n = 117) was significantly superior (d = 0.43, P = .0026) to placebo (n = 119) at week 5. In EMERGENT-3, xanomeline/ trospium (n = 114) was significantly superior (d = 0.62, P < .0001) to placebo (n = 120) at week 5. Pooled results were consistent with the individual trials.
Conclusion: Xanomeline/trospium showed improvement in agitation as measured by PANSS-EC in participants with acute exacerbations of schizophrenia. Xanomeline/trospium is the first in a new class of treatments for schizophrenia based on muscarinic receptor agonism.
Trial Registration: ClinicalTrials.gov identifiers: NCT03697252, NCT04659161, NCT04738123
J Clin Psychiatry 2025;86(2):24m15668
Author affiliations are listed at the end of this article.
See commentary by Citrome
Agitation is defined in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders as “excessive motor activity associated with a feeling of inner tension. The activity is usually non-productive and repetitious and consists of behaviors such as pacing, fidgeting, wringing of the hands, pulling of clothes, and inability to sit still.”1 Psychomotor agitation is associated with many psychiatric disorders, especially schizophrenia, with the potential for escalation to aggression and violence.2 Patients with schizophrenia can demonstrate agitated, aggressive, or violent behavior that is mostly related to psychotic symptoms. Prompt evaluation and immediate management of agitation are essential to treat potentially dangerous behavior that could escalate to violence.3
In some cases, agitation can be managed with nonpharmacologic approaches, such as verbal interventions and de-escalation, but for many individuals, pharmacologic treatment is necessary, especially in emergency settings.4 Oral medications are preferred over more coercive, intramuscular formulations if patients are able to cooperate with taking the noninvasive, oral treatments.5 Management of acute agitation has traditionally involved antipsychotics (eg, haloperidol) or benzodiazepines (eg, lorazepam). For people with agitation associated with schizophrenia, antipsychotics are preferred over benzodiazepines, because they address the underlying psychosis, and benzodiazepines use should be short term due to risks, such as dependence, psychomotor impairment, and accidents. If agitation does not respond to an antipsychotic alone, then short-term concomitant benzodiazepine and antipsychotic could be used.4,5
Oral and intramuscular formulations of antipsychotics and benzodiazepines are commonly used, and alternative inhaled and sublingual routes of administration are available, but all treatments have potential side effects.6 Antipsychotics are associated with extrapyramidal symptoms, and benzodiazepines could result in oversedation or paradoxical behavioral disinhibition that could exacerbate the distress experienced by agitated patients. Extrapyramidal symptoms due to antipsychotic treatment include akathisia, dyskinesia, dystonia, and parkinsonism.7 Akathisia is especially concerning, because it is often difficult to differentiate between akathisia due to antipsychotic medication versus agitation due to underlying illness. Treating an agitated person with antipsychotics or benzodiazepines that could cause akathisia or oversedation could worsen agitation and compromise compliance.
Antipsychotics have other problematic side effects, including neuroleptic malignant syndrome, tardive dyskinesia, prolactin changes, orthostatic hypotension, leukopenia, seizures, oversedation, QTc prolongation, and metabolic changes, especially weight gain, hyperglycemia, and dyslipidemia.8,9 Furthermore, antipsychotics are associated with cerebrovascular adverse reactions, including stroke and death in studies of psychosis in Alzheimer’s disease. Although dopamine partial agonists have lower rates of parkinsonism and dystonia than other atypical antipsychotics, akathisia has been a common adverse event with dopamine partial agonists.10 These side effects as well as inadequate response are the primary reasons for discontinuation of antipsychotics, so there is a need for a different approach to treat schizophrenia and agitation associated with schizophrenia.11
Xanomeline is a preferential M1 and M4 muscarinic receptor agonist that has demonstrated efficacy in schizophrenia.12,13 Along with improving psychosis in schizophrenia, a placebo-controlled trial of xanomeline in Alzheimer’s disease showed improvement in psychosis and agitation; however, development of xanomeline was discontinued due to procholinergic side effects, such as nausea, vomiting, and orthostasis, that resulted in high discontinuation rates.14 Oral xanomeline and trospium chloride, formerly known as KarXT, combines the muscarinic receptor agonist xanomeline with the peripherally restricted pan-muscarinic receptor antagonist trospium, which reduced the peripheral side effects of xanomeline and decreased discontinuation rates.15,16 Xanomeline/trospium has been developed for the treatment of schizophrenia and has demonstrated improved tolerability compared with xanomeline alone.
The US Food and Drug Administration recently approved xanomeline/trospium as the first in a new class of medications based on muscarinic receptor agonism to treat schizophrenia. Xanomeline/trospium efficacy and safety have been demonstrated in acutely symptomatic adults with schizophrenia in the pivotal EMERGENT-1 (NCT03697252),17 EMERGENT-2 (NCT04659161),18 and EMERGENT-3 (NCT04738123)19 trials. These 5- week, randomized, placebo-controlled, double-blind, flexible-dose trials were nearly identical in design. The nearly identical designs of the pivotal EMERGENT trials provided an opportunity to pool data and assess xanomeline/trospium efficacy and safety with the increased statistical power afforded by a larger population.20
METHODS
Trial Design
The pivotal EMERGENT-1, EMERGENT-2, and EMERGENT-3 trials were 5-week, randomized, double blind, placebo-controlled inpatient trials of xanomeline/ trospium in adults with schizophrenia.17–19 Participants were randomized 1:1 to receive xanomeline/trospium or placebo twice daily for 5 weeks following a 7- to 14-day screening period. The flexible dosing schedule for xanomeline/trospium started at a dose of twice-daily 50- mg xanomeline/20-mg trospium and increased to a maximum of twice-daily 125-mg xanomeline/30-mg trospium by the end of the first week based on tolerability at the investigator’s discretion. Trials ran from September 2018 to December 2022 and enrolled participants at 42 sites in the United States and Ukraine (EMERGENT-3 only).17–19
Trial Population
Enrolled adults (aged 18–60 years, EMERGENT-1; 18–65 years, EMERGENT-2 and EMERGENT-3) were required to have a primary diagnosis of schizophrenia as established by comprehensive evaluation. Additional criteria included exacerbation of psychotic symptoms requiring hospitalization within 2 months of screening, baseline Positive and Negative Syndrome Scale (PANSS) total score between 80 and 120, inclusive,21 a score of ≥4 on at least 2 out of 4 PANSS positive scale items, and a Clinical Global Impression-Severity score of ≥4. Exclusion criteria included a primary diagnosis other than schizophrenia in the year prior to screening, a history of resistance to antipsychotic treatment, improvement of ≥20% in PANSS total score between screening and baseline visit, and risk of violent or destructive behavior. Concomitant benzodiazepines (up to 6 mg lorazepam/ day or equivalent) were permitted for anxiety, agitation, and insomnia as needed during the studies.
Efficacy Assessments
The primary endpoint was change from baseline to week 5 in PANSS total score. PANSS is a validated, clinician-administered, 30-item scale widely used to assess treatment efficacy in clinical trials of schizophrenia.21 Each item is scored on a 7-point scale for a total range of 30–210 points (higher scores indicate greater symptom severity). The PANSS-EC is composed of 5 items of the PANSS: excitement, tension, hostility, uncooperativeness, and poor impulse control. The change from baseline of the PANSS-EC has been used as the primary endpoint in prior studies of antipsychotics for the treatment of agitation associated with schizophrenia.22–25
Safety Assessments
Safety was assessed by monitoring for treatment emergent adverse events (TEAEs), treatment-related adverse events (defined as adverse events that the investigator considered possibly, probably, or definitely related to trial medication), weight, vital signs, clinical laboratory values, electrocardiograms, Simpson-Angus Scale (SAS) to measure extrapyramidal symptoms,26 Barnes Akathisia Rating Scale (BARS) to assess akathisia,27 Abnormal Involuntary Movement Scale (AIMS) to assess tardive dyskinesia,28 and Columbia Suicide Severity Rating Scale to assess suicide risk.
Statistical Analyses
Post hoc analyses included analysis of the 5 PANSS items (excitement, tension, hostility, uncooperativeness, and poor impulse control) that compose the PANSS-EC. Data from each individual trial were analyzed separately and pooled. The modified intent-to treat (mITT) population was defined as all randomized participants who received ≥1 dose of trial medication and had a baseline and ≥1 postbaseline PANSS assessment. Change from baseline in PANSS-EC total score was analyzed using mixed model for repeated measures with terms for treatment, visit, treatment-by-visit interaction, age, sex, and site (for individual studies) or trial (for 3 trials pooled). Baseline was defined as the most recent measurement prior to the first administration of trial medication.
PANSS-EC response was defined as achieving ≥40% improvement over baseline scores at week 5, because this has been considered a clinically relevant reduction in similar studies of antipsychotics.29–31 Response rates with xanomeline/trospium were compared with placebo in the mITT population as well as in a subgroup of participants with baseline PANSS-EC score ≥14 and with at least 1 of the 5 items rated ≥4. Safety analyses were performed in the safety population, defined as all participants who received ≥1 dose of trial medication. Data listings, summaries, and statistical analyses were generated using SAS software version 9.4 (Cary, NC).
RESULTS
Participants
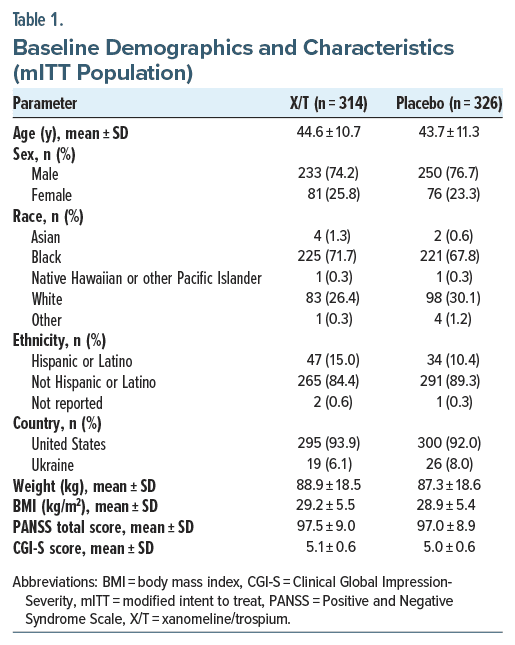
Across the pivotal EMERGENT trials, a total of 1,088 participants were screened, and 690 individuals were randomized to receive xanomeline/trospium (n = 341) or placebo (n = 349). The mITT population included 314 participants in the xanomeline/trospium arm and 326 participants in the placebo arm, and the safety population included 340 participants in the xanomeline/trospium arm and 343 participants in the placebo arm. There were no meaningful differences in baseline demographics and characteristics between treatment groups (Table 1). Mean participant age was 44.6 years and 43.7 years in the xanomeline/trospium and placebo groups, respectively. Most participants were male (xanomeline/trospium, 74.2%; placebo, 76.7%) and Black (xanomeline/trospium, 71.7%; placebo, 67.8%) or White (xanomeline/trospium, 26.4%; placebo, 30.1%). A majority of each treatment arm comprised individuals from the United States (xanomeline/trospium, 93.9%; placebo, 92.0%). Mean weight and body mass index were similar between the treatment groups. Medical history included agitation in 22.4% and 20.4% of the xanomeline/trospium and placebo groups, respectively. During the study, concomitant benzodiazepines (lorazepam, diazepam, alprazolam, and clonazepam) were used with xanomeline/trospium (41.5%) and with placebo (46.1%); 1 placebo-treated participant took both lorazepam and clonazepam.
Efficacy Results
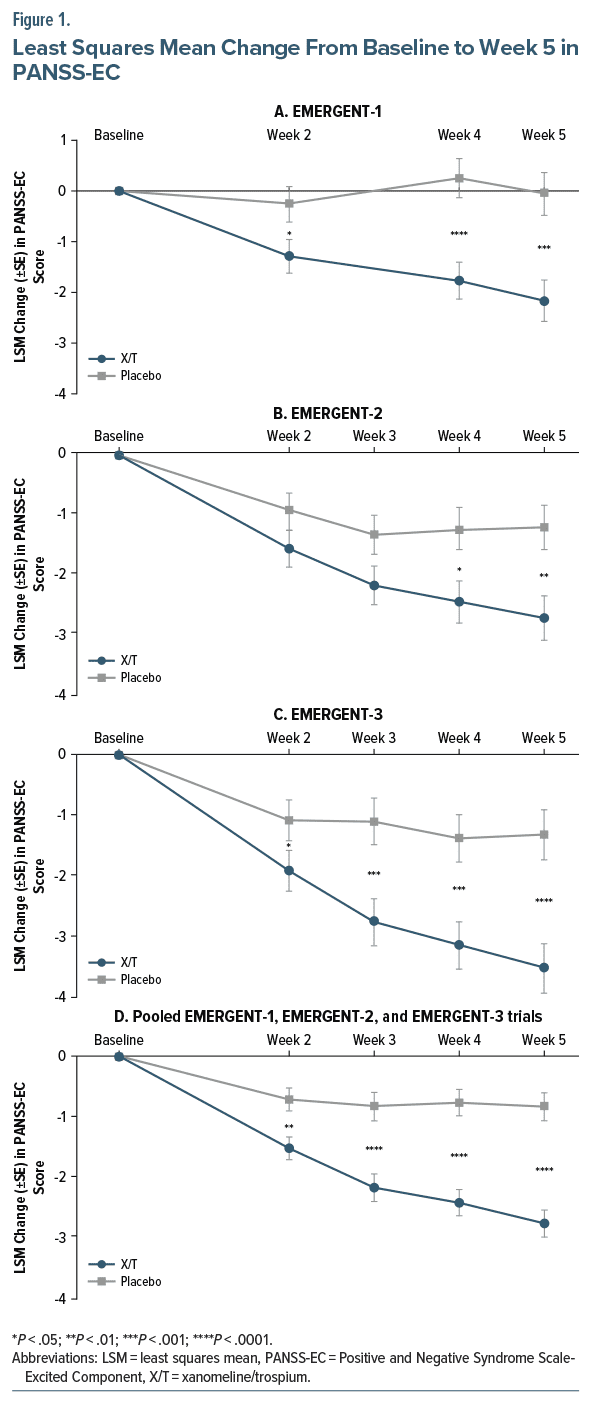
Xanomeline/trospium was associated with significantly greater improvement from baseline to week 5 in PANSS-EC scores compared with placebo across all 3 EMERGENT trials, along with significantly greater improvement in the PANSS total scores in all 3 trials. In all 3 trials, xanomeline/trospium was associated with a significantly greater improvement from baseline to week 5 in PANSS-EC score compared with placebo (EMERGENT-1, Cohen’s d = 0.62, P = .0002, Figure 1A; EMERGENT-2, Cohen’s d = 0.43, P = .0026, Figure 1B; EMERGENT-3, Cohen’s d = 0.62, P < .0001, Figure 1C). In the pooled analyses, xanomeline/trospium was associated with a significantly greater reduction from baseline to week 5 in PANSS-EC score (Cohen’s d = 0.55, P < .0001); improvement with xanomeline/trospium was significantly greater than placebo starting at week 2 (earliest time point assessed) and maintained through week 5 (Figure 1D).
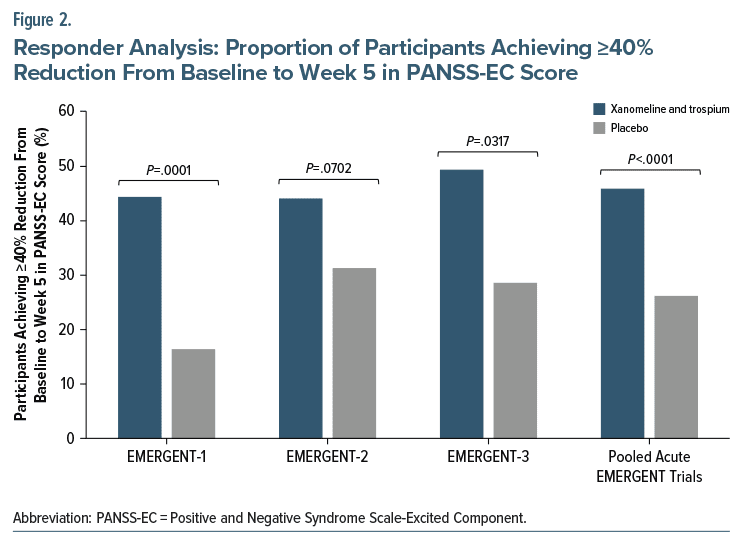
In the mITT population, response (≥40% reduction in PANSS-EC score) rates were 44.4% (32/72) with xanomeline/trospium and 16.4% (12/73) with placebo (P = .0001) in EMERGENT-1, 44.1% (41/93) with xanomeline/trospium and 31.3% (31/99) with placebo (P = .0702) in EMERGENT-2, 49.4% (39/79) with xanomeline/trospium and 28.6% (26/91) with placebo (P = .0317) in EMERGENT-3, and 45.9% (112/244) with xanomeline/trospium and 26.2% (69/263) with placebo (P < .0001) in the pooled analysis (Figure 2). In the subgroup analysis (participants with baseline PANSS-EC score ≥14 and at least 1 of the 5 items rated ≥4), response rates were 52.2% (12/23) with xanomeline/trospium and 21.1% (4/19) with placebo (P=.1178) in EMERGENT-1, 41.9% (13/31) with xanomeline/trospium and 18.8% (6/32) with placebo (P=.0143) in EMERGENT-2, 60.0% (18/30) with xanomeline/trospium and 20.0% (6/30) with placebo (P=.0151) in EMERGENT-3, and 51.2% (43/84) with xanomeline/trospium and 19.8% (16/81) with placebo (P<.0001) in the pooled analysis.
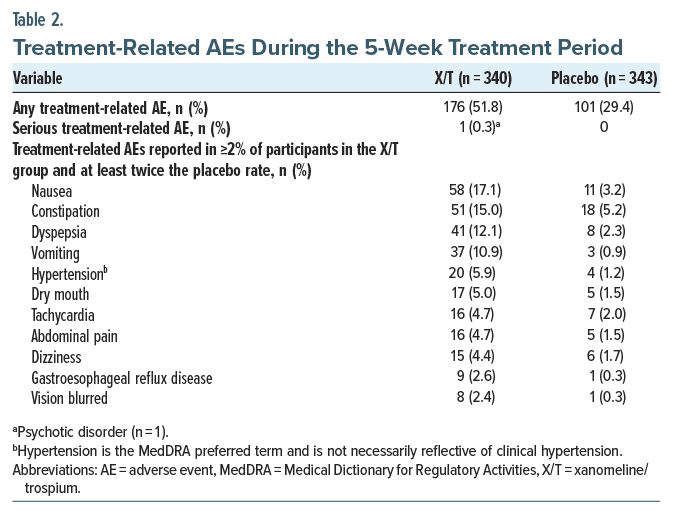
Safety Results
Xanomeline/trospium was generally well tolerated. In the pooled analyses, a total of 51.8% and 29.4% of participants in the xanomeline/trospium and placebo arms, respectively, experienced ≥1 treatment-related adverse event. Two participants who received placebo discontinued the trial due to suicidal or assaultive behavior, but no participant who received xanomeline/ trospium was discontinued from the studies due to suicidal or assaultive behavior. In the safety population, TEAEs included agitation (xanomeline/trospium, 2.1%; placebo, 3.5%) and akathisia (xanomeline/trospium, 2.4%; placebo, 0.9%). The most commonly reported treatment-related adverse events occurring in ≥5% of participants in the xanomeline/trospium versus placebo arm were nausea, constipation, dyspepsia, vomiting, hypertension, and dry mouth (Table 2). All of the most commonly reported TEAEs were mild or moderate in intensity. Xanomeline/trospium was not associated with changes in weight compared with placebo. Mean change from baseline to week 5 in body weight was 1.41 ± 3.18 kg in the xanomeline/trospium group compared with 1.94 ± 5.00 kg in the placebo group. Fewer participants in the xanomeline/trospium group (5.3%) experienced clinically meaningful increase in body weight (defined as an increase of ≥7%) compared with placebo (11.4%).
Mean (±SD) change from baseline to week 5 in systolic blood pressure was +0.7 ± 12.96 mm Hg in the xanomeline/trospium group compared with 0.0 ± 12.01 mm Hg in the placebo group, and mean change in diastolic blood pressure was 1.9 ± 9.14 mm Hg (xanomeline/trospium) and 0.4 ± 9.35 mm Hg (placebo). Mean change from baseline to week 5 in heart rate was 10.4 ± 14.4 beats per minute (bpm) in the xanomeline/ trospium group and 4.5 ± 13.4 bpm in the placebo group. No increases in QTc interval were observed with xanomeline/trospium. Rates of extrapyramidal symptom TEAEs were low in the xanomeline/trospium (3.2%) and placebo (0.9%) groups; extrapyramidal symptom TEAEs were considered treatment related in 1.5% of participants in the xanomeline/trospium group compared with 0.3% of participants in the placebo group, but there were no reports of tardive dyskinesia. All extrapyramidal symptom TEAEs were mild or moderate, and most resolved with continued treatment. Xanomeline/trospium was not associated with clinically meaningful changes from baseline to week 5 in SAS, BARS, or AIMS scores compared with placebo.
DISCUSSION
Antipsychotics and benzodiazepines are cornerstones for the treatment of agitation associated with schizophrenia, but they have significant tolerability limitations. Side effects include extrapyramidal symptoms (especially akathisia) and oversedation, which contribute to an increased risk of nonadherence and complications.4,5 For people experiencing side effects of antipsychotic treatment, other currently available antipsychotics have similar safety and efficacy limitations. Overlap in antipsychotic side effect profiles is not surprising, because all existing antipsychotics have a D2 dopamine receptor mechanism of action. Xanomeline/trospium is the first muscarinic receptor agonist and represents an alternative mechanism to treat schizophrenia. Xanomeline/trospium acts preferentially via M1 and M4 muscarinic receptor agonism without direct action at D2 dopamine receptors, which may avoid some of the traditional adverse effects of currently available antipsychotics.13,16
In pooled analyses of safety data from the 3 short term EMERGENT trials of xanomeline/trospium in adults with schizophrenia, xanomeline/trospium was generally well tolerated, and xanomeline/trospium exhibited few of the side effects often observed with antipsychotic use. For example, a small proportion of participants treated with xanomeline/trospium experienced treatment related extrapyramidal symptom TEAEs (xanomeline/ trospium, 1.5%; placebo, 0.3%), and no clinically meaningful changes from baseline to week 5 were observed in any of the extrapyramidal symptom scales.32 Additionally, rates of somnolence were low and similar among treatment groups (xanomeline/trospium, 5.0%; placebo, 4.1%). The most common side effects observed with xanomeline/trospium were primarily gastrointestinal TEAEs, mild or moderate in intensity, and transient in nature. Adverse events, such as somnolence or parkinsonism, that are commonly observed with other antipsychotics were not associated with xanomeline/trospium use.
Individual trial and pooled analyses provide preliminary results regarding the effect of xanomeline/ trospium on the treatment of agitation in schizophrenia as assessed by the PANSS-EC. All 3 pivotal trials showed significantly greater improvement from baseline to week 5 in PANSS-EC scores compared with placebo (Figure 1). Statistically significant improvements were seen in the PANSS-EC scores by the first postbaseline assessment at week 2, and these improvements continued at every assessment until the completion of the 5-week trials. Response rates were consistent with the PANSS-EC results (Figure 2). The pooled PANSS-EC score and PANSS-EC response rates were highly statistically significant (P<.0001) when the data from the 3 studies were pooled in this post hoc analysis. Therefore, this muscarinic agonist for the treatment of schizophrenia appears to have potential for the treatment of agitation associated with schizophrenia, but additional trials specifically designed to assess agitation are needed.
Limitations of this analysis reflect those of the individual trials. First, these were post hoc analyses of 3 trials that were designed to assess xanomeline/ trospium for the treatment of psychotic symptoms in voluntary participants with schizophrenia as assessed by the PANSS total score and excluded risk of violent or destructive behavior, so the trials were not specifically designed to assess agitation, which may impact generalizability to agitation in nonpsychotic patients at high risk for violent or destructive behavior. The inpatient studies mitigated issues of nonadherence and concomitant use of prescribed or recreational drugs, limiting generalizability to the outpatient setting. The high proportion of Black participants may also affect generalizability to other groups. Another limitation of this analysis is that these studies allowed concomitant benzodiazepines, which were used with xanomeline/ trospium (41.5%) and with placebo (46.1%) and could have affected these results. Design of the 5-week EMERGENT trials lacked a positive control (active comparator) arm, which prevents direct comparisons of xanomeline/trospium with other antipsychotics. Moreover, PANSS-EC assessments were only conducted at baseline and at weeks 2, 3, 4, and 5, so earlier postbaseline assessments were not available. In comparison, pivotal trials of intramuscular antipsychotics for the treatment of agitation associated with schizophrenia had assessments every 15 or 30 minutes for the first 2 hours and at 4, 6, 12, and 24 hours after initial dose.22–24
In conclusion, xanomeline/trospium demonstrated statistically significantly greater improvements compared with placebo across efficacy measures in the treatment of agitation associated with schizophrenia in individual EMERGENT-1, EMERGENT-2, and EMERGENT-3 trials, as well as in the pooled analyses of all 3 trials. In these post hoc analyses, xanomeline/ trospium demonstrated significantly greater improvement in agitation compared with placebo as measured by the PANSS-EC. Muscarinic acetylcholine receptors are implicated in the pathophysiology of schizophrenia, and the mechanism of action of xanomeline appears to be selectivity for the M1 and M4 muscarinic receptor subtypes, which previously demonstrated improvement in agitation associated with Alzheimer’s disease.14–16 Xanomeline/trospium is the first in a new class of medications approved by the US Food and Drug Administration to treat schizophrenia based on muscarinic receptor agonism and without direct D2 dopamine receptor activity. The present findings lend further support for the efficacy of xanomeline/trospium in the treatment of schizophrenia with potential effect on agitation associated with schizophrenia.
Article Information
Published Online: March 24, 2025. https://doi.org/10.4088/JCP.24m15668
© 2025 Physicians Postgraduate Press, Inc.
Submitted: October 16, 2024; accepted December 27, 2024.
To Cite: Yeung PP, Breier A, Zhu H, et al. Xanomeline and trospium chloride for the treatment of agitation associated with schizophrenia: PANSS-Excited Component results from 3 randomized, double-blind, placebo-controlled EMERGENT trials. J Clin Psychiatry 2025;86(2):24m15668
Author Affiliations: Bristol Myers Squibb, Princeton, New Jersey (Yeung, Zhu, Kaul, Marcus); Psychiatry Department, Indiana University School of Medicine, Indianapolis, Indiana (Breier).
Corresponding Author: Paul P. Yeung, MD, MPH, Bristol Myers Squibb, 3401 Princeton Pike, Lawrenceville, NJ 08648 ([email protected]).
Relevant Financial Relationships: Drs Yeung, Kaul, and Marcus are employees of Bristol Myers Squibb. Dr Breier is a consultant to Bristol Myers Squibb. Dr Zhu was an employee of Bristol Myers Squibb at the time the research was performed.
Funding/Support: The EMERGENT trials were funded by Karuna Therapeutics, a Bristol Myers Squibb company, Princeton, NJ.
Role of the Sponsor: Karuna Therapeutics, a Bristol Myers Squibb company, had a role in the design and conduct of the trial; collection, management, and analysis of the data; and review of the manuscript.
Previous Presentation: Poster presented at the American College of Neuropsychopharmacology Meeting; December 3–6, 2023; Tampa, Florida.
Acknowledgments: The authors thank the trial participants and investigators for their roles in this research.
ORCID: Paul Yeung: https://orcid.org/0000-0001-5132-3043
Clinical Points
- Agitation requires nonpharmacologic and sometimes pharmacologic treatment that minimizes side effects.
- Xanomeline/trospium is the first muscarinic treatment for schizophrenia with potential effect on agitation.
References (32)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association; 2013.
- Correll CU, Yu X, Xiang Y, et al. Biological treatment of acute agitation or aggression with schizophrenia or bipolar disorder in the inpatient setting. Ann Clin Psychiatry. 2017;29(2):92–107. PubMed
- Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatry. 2016;17(2):86–128.
- Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165–172.
- Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the American Association for Emergency Psychiatry Project Beta Psychopharmacology Workgroup. West J Emerg Med. 2012;13(1):26–34.
- Citrome L, Correll CU, San L, et al. Alternative approaches for addressing acute agitation in schizophrenia and bipolar disorder. Prim Care Companion CNS Disord. 2024;26(1):23nr03596.
- Tarsy D, Baldessarini RJ, Tarazi FI. Effects of newer antipsychotics on extrapyramidal function. CNS Drugs. 2002;16(1):23–45.
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. PubMed CrossRef
- Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician. 2010;81(5):617–622.
- Citrome L, Volavka J. Specific anti-hostility effects of atypical antipsychotics in persons with schizophrenia: from clozapine to cariprazine. Harv Rev Psychiatry. 2021;29(1):20–34.
- Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223.
- Shekhar A, Potter WZ, Lightfoot J, et al. Selective muscarinic receptor agonist xanomeline as a novel treatment approach for schizophrenia. Am J Psychiatry. 2008;165(8):1033–1039. PubMed CrossRef
- Thorn CA, Moon J, Bourbonais CA, et al. Striatal, hippocampal, and cortical networks are differentially responsive to the M4- and M1-muscarinic acetylcholine receptor mediated effects of xanomeline. ACS Chem Neurosci. 2019;10(8):3910.
- Bodick NC, Offen WW, Levey AI, et al. Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol. 1997;54(4):465–473. PubMed CrossRef
- Breier A, Brannan SK, Paul SM, et al. Evidence of trospium’s ability to mitigate cholinergic adverse events related to xanomeline: phase 1 study results. Psychopharmacology. 2023;240(5):1191–1198.
- Paul SM, Yohn SE, Popiolek M, et al. Muscarinic acetylcholine receptor agonists as novel treatments for schizophrenia. Am J Psychiatry. 2022;179(9):611–627.
- Brannan SK, Sawchak S, Miller AC, et al. Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia. N Engl J Med. 2021;384(8):717–726.
- Kaul I, Sawchak S, Correll CU, et al. Efficacy and safety of the muscarinic receptor agonist KarXT (xanomeline-trospium) in schizophrenia (EMERGENT-2) in the USA: results from a randomised, double-blind, placebo-controlled, flexible-dose phase 3 trial. Lancet. 2024;403(10422):160–170.
- Kaul I, Sawchak S, Walling DP, et al. Efficacy and safety of xanomeline-trospium chloride in schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2024;81(8):749–756.
- Correll CU. Unleashing the power of pooled and subgroup analyses in psychiatry. Int Clin Psychopharmacol. 2022;37(5):223–224.
- Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276.
- Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry. 2002;59(5):441–448. PubMed CrossRef
- Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology. 2006;188(3):281–292. PubMed CrossRef
- Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo controlled trial. J Clin Psychiatry. 2007;68(1):111–119. PubMed CrossRef
- Lesem MD, Tran-Johnson TK, Riesenberg RA, et al. Rapid acute treatment of agitation in individuals with schizophrenia: multicentre, randomised, placebo controlled study of inhaled loxapine. Br J Psychiatry. 2011;198(1):51–58. PubMed CrossRef
- Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19.
- Barnes TR. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989;154:672–676.
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Revised. In: U.S. Department of Health Education, and Welfare. National Institute of Mental Health; 1976.
- Pratts M, Citrome L, Grant W, et al. A single-dose, randomized, double-blind, placebo-controlled trial of sublingual asenapine for acute agitation. Acta Psychiatr Scand. 2014;130(1):61–68. PubMed CrossRef
- Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876–1885. PubMed CrossRef
- Zeller S, Zun L, Cassella JV, et al. Response to inhaled loxapine in patients with schizophrenia or bipolar I disorder: PANSS-EC responder analyses. BJPsych Open. 2017;3(6):285–290. PubMed CrossRef
- Kaul I, Claxton A, Sawchak S, et al. Safety and tolerability of xanomeline and trospium chloride in schizophrenia: pooled results from the 5-week, randomized, double-blind, placebo-controlled EMERGENT trials. J Clin Psychiatry. 2025;86(1):24m15497.
This PDF is free for all visitors!