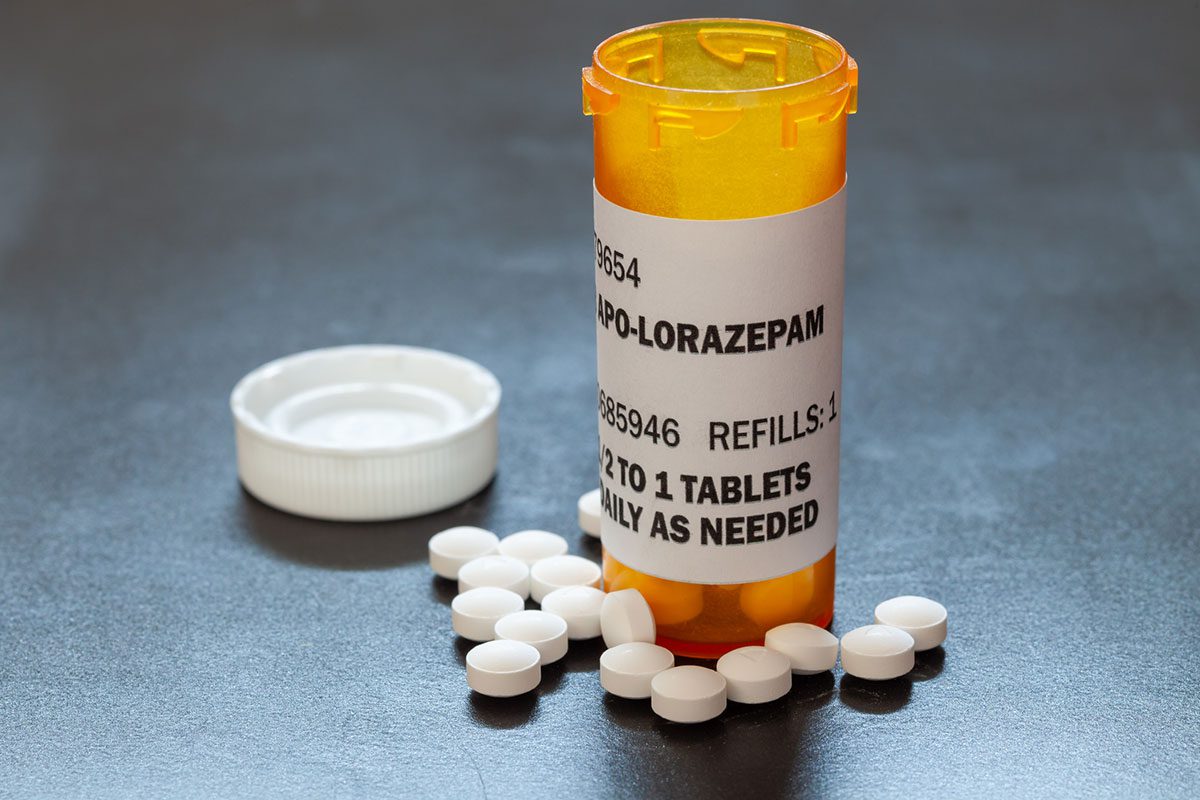
Catatonia, a state of unresponsiveness characterized by motoric immobility or excessive activity, can be a symptom of various psychiatric disorders. Understanding its causes, manifestations, and treatments is crucial. The Journal of Clinical Psychiatry provides comprehensive insights into catatonia, emphasizing evidence-based diagnostic and therapeutic approaches. Our expert editors ensure that content is clinically relevant and actionable, equipping psychiatrists to recognize and address catatonia effectively.
Catatonia
Recently published articles about Catatonia
Brief Report
Treatment with (Es)ketamine in Catatonia: A Systematic Review of Case Reports
October 13, 2025
Recent evidence suggests that NMDA receptor antagonists, such as ketamine, may offer benefit in catatonia. This systematic review was conducted to evaluate the efficacy and safety of ketamine and...