Abstract
Objective: To review the effects of the ketogenic diet on epilepsy in children and adolescents.
Data Sources: A literature search was conducted in PubMed with no publication date or language restrictions based on the Preferred Reporting Items for Systematic Reviews and Meta Analyses guidelines. Keywords used included children, adolescent, ketogenic diet, epilepsy, and seizure.
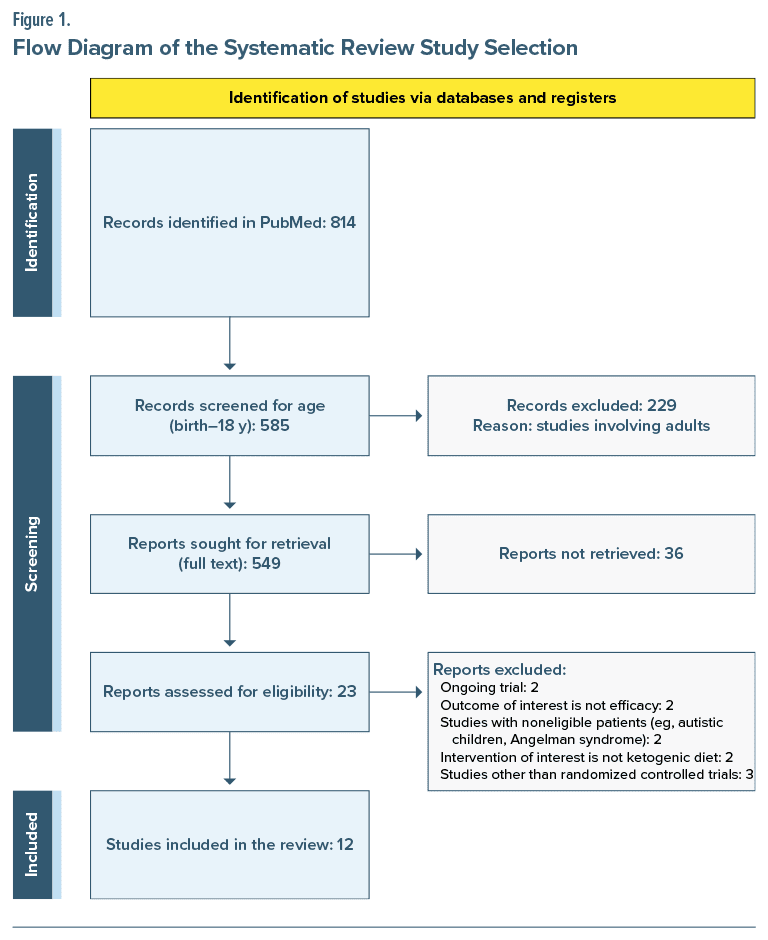
Study Selection: After excluding articles that did not meet the inclusion criteria, such as missing variables of study, adult population, and nonrandomized clinical trials, a total of 12 studies were included in the final review.
Data Extraction: Data on study design, duration, sample size, population, and type of intervention were collected using a standard template.
Results: The ketogenic diet and its modified versions were noted to have beneficial effects in reduction of seizure frequency and severity, with manageable adverse effects such as gastrointestinal disturbances, dehydration, dyslipidemia, hyperuricemia, infection, and metabolic acidosis.
Conclusions: Depending on patient compliance and comorbidities, all variations of the ketogenic diet were found to be helpful for seizure treatment, whether as an additive or an alternative treatment option, for children and adolescents with epilepsy.
Prim Care Companion CNS Disord 2024;26(3):23r03661
Author affiliations are listed at the end of this article.
Epilepsy is a common neurological disorder affecting children and adolescents worldwide, with an annual incidence rate of 5–7 cases per 100,000 and a prevalence rate of 20–60 cases per 100,000.1 Epilepsy is recurrent seizures with brief episodes of involuntary movements involving part of the body (partial) or all of the body (generalized) with or without loss of consciousness, bowel, and bladder function.2 The major causes that lead to epilepsy are inherited disorders, congenital anomalies, fever, central nervous system infection, hydrocephalus, and brain tumors.3 Approximately 20%–40% of epilepsy cases are refractory or drug-resistant to standard antiepileptic drugs and require alternative treatment modalities including ketogenic diet therapy, surgical treatment, and vagal nerve stimulation.4,5
The ketogenic diet refers to a dietary composition of high fat, low carbohydrate, and adequate protein, which results in a ketogenic state of human metabolism and is considered to reduce seizure frequency.5–7 There are 4 major types of ketogenic diet therapy: the classic ketogenic diet (cKD), modified Atkins diet (MAD), medium-chain triglyceride ketogenic diet (MCTKD), and low-glycemic index treatment (LGIT).8 Reduced excitability of neurons as a result of multiple mechanisms in the brain and alteration of gut microflora plays a role in the positive effects of the ketogenic diet on epilepsy.9 The type of diet should be considered based on the patient’s age, family conditions, and severity and type of epilepsy.10
Evidence for the ketogenic diet in epilepsy in previous studies is limited by small sample size, high attrition rates, lack of evidence in adults, and limited number of studies.6,7 Adverse effects associated with ketogenic diets such as gastrointestinal problems, weight loss, and cardiovascular complications also remain a limiting factor in studies.6,7 In this review article, we aim to present the effects of the ketogenic diet on epilepsy in children and adolescents to provide a better understanding for clinicians and patients.
METHODS
A systematic search was conducted in PubMed with no publication date or language restrictions based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)11 and followed a predefined protocol. The primary aim of the review was to evaluate the efficacy of the ketogenic diet in children and adolescents with epilepsy. Epilepsy was defined as recurrent seizures with brief episodes of involuntary movements of the whole body or body parts with or without loss of consciousness, bowel, and bladder function. We included all 4 major types of ketogenic diets (cKD, MAD, MCTKD, and LGIT) and defined ketogenic diet as a dietary composition of high fat, low carbohydrate, and adequate protein. Articles on various types of ketogenic diet as intervention and efficacy were selected. The secondary aim of the study was to highlight the possible adverse effects of various types of ketogenic diet.
Inclusion and Exclusion Criteria
Articles were included if (1) the study population included children and adolescents with epilepsy, (2) they implemented a ketogenic diet, and (3) they were randomized controlled trials (RCTs) exploring the efficacy of a ketogenic diet. Articles were excluded if (1) they included adults or noneligible patients (eg, autistic children and Angelman syndrome) as the study population, (2) they were not RCTs or were ongoing trials or non–full-text articles, (3) the intervention of interest was not a ketogenic diet, and (4) the outcome of interest was not efficacy.
Search Strategy and Selection
We followed PRISMA guidelines in conducting the systematic review exploring the efficacy of a ketogenic diet. Articles in PubMed were searched using the search terms ((“children’’[Title/Abstract] OR “adolescent”[Title/Abstract] OR “toddler”[Title/Abstract] OR “newborn”[Title/Abstract] OR “infant”[Title/ Abstract]) AND ([“ketogenic diet”[Title/Abstract] OR “keto diet”[Title/Abstract] OR “atkins diet”[Title/ Abstract] OR “low glycemic index treatment”[Title/ Abstract] OR “classic ketogenic diet”[Title/Abstract] OR “medium chain triglyceride ketogenic diet”[Title/ Abstract]) AND (“epilepsy”[Title/Abstract] OR “seizure”[Title/Abstract])) AND ((randomized controlled trial[Filter]) AND (fft[Filter]) AND (allchild[Filter])).
The title and abstract of articles retrieved from the initial search were evaluated. Full texts of included articles were assessed, and those that did not meet the inclusion criteria were discarded. Any disagreements were discussed and resolved by consensus and consultation with an expert. Data on study name (first author), study design, duration, sample size, population characteristics (country, mean/median age in years, and sex [%]), type of intervention (various types of ketogenic diet), and outcomes (efficacy and adverse effects) were collected using a standard template, and any disagreement was resolved by the authors (Y-C.H. and D.P.). Figure 1 describes the data collection process.
RESULTS
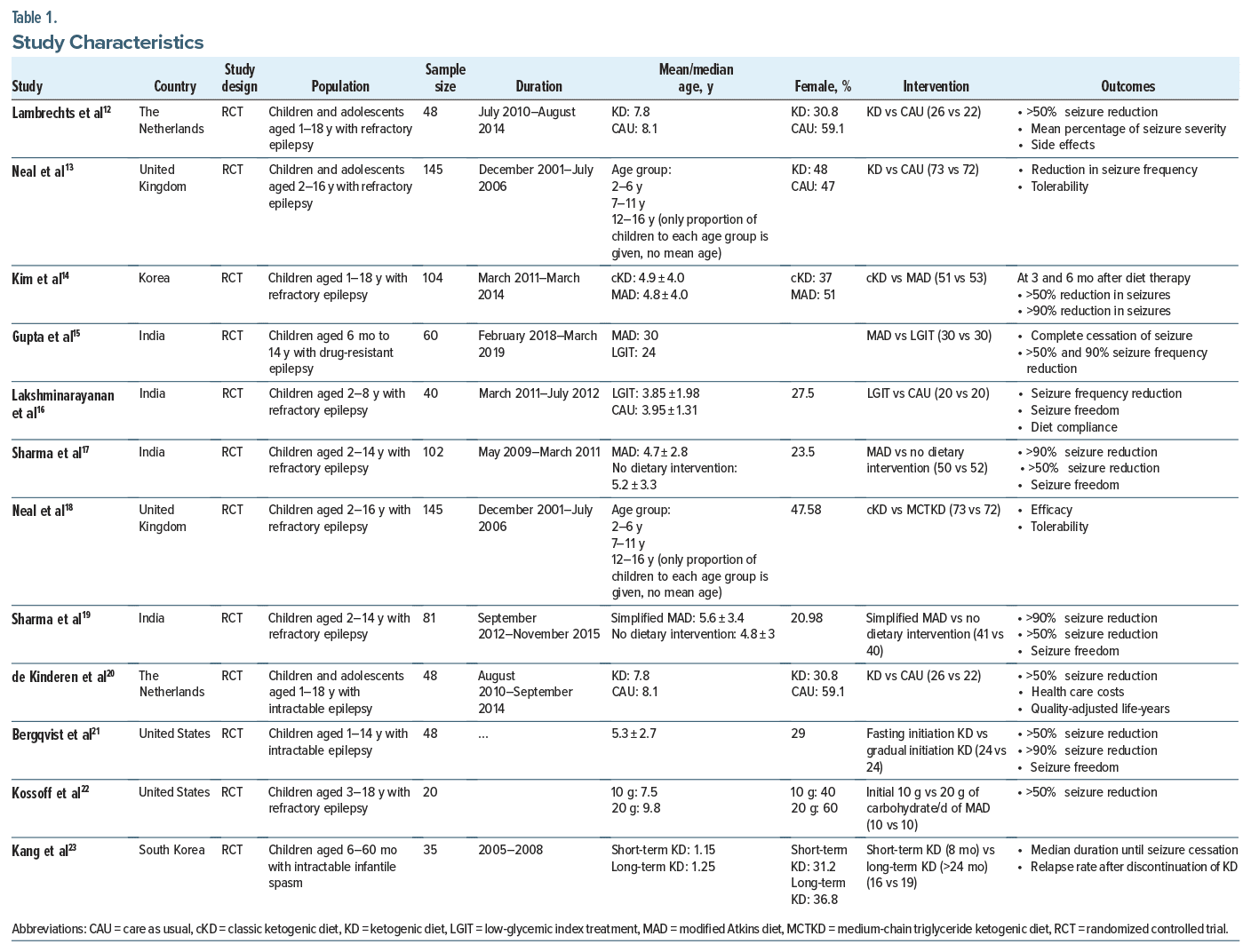
The search strategy resulted in 814 articles. A total of 12 articles were included in the final review. The RCTs were conducted in various countries including the United States, the Netherlands, the United Kingdom, Korea, and India. Table 1 provides the characteristics of the studies, and Table 2 describes the findings.
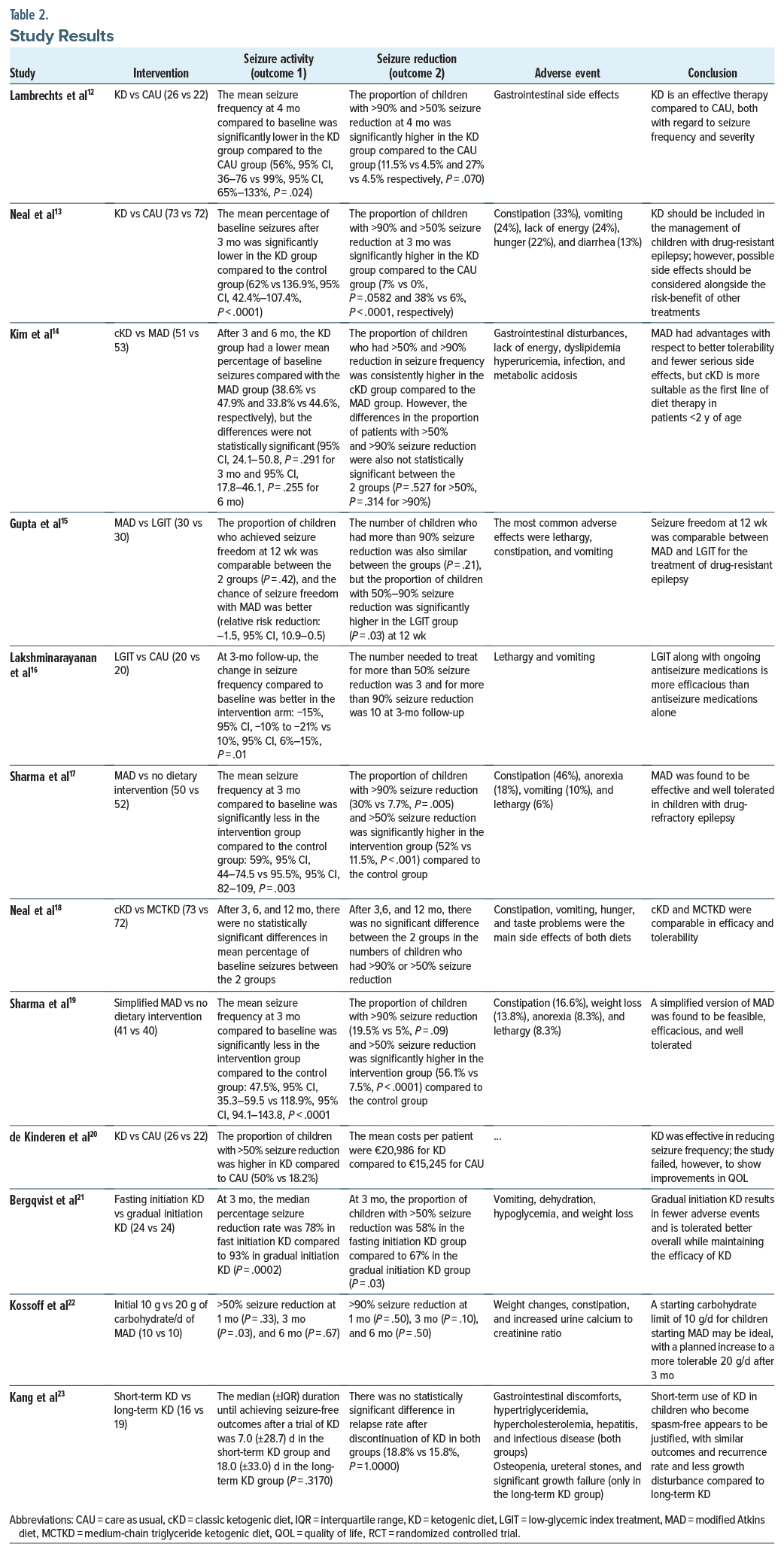
Several studies, including Lambrechts et al,12 Neal et al,13 and de Kinderen et al,20 compared the efficacy of the ketogenic diet with no dietary intervention for treating drug-resistant epilepsy in children and adolescents. Lambrechts et al12 found that, at 4 months, the proportion of children with >90% and >50% seizure reduction was significantly higher in the ketogenic diet group compared to the no dietary intervention group (11.5% vs 4.5% and 27% vs 4.5%, respectively; P = .070). Similarly, Neal et al13 found that, at 3 months, the proportion of children with >90% and >50% seizure reduction was significantly higher in the ketogenic diet group compared to the no dietary intervention group (7% vs 0%, P = .0582 and 38% vs 6%, P < .0001, respectively). The study conducted by de Kinderen et al20 also found that the proportion of children with >50% seizure reduction was higher in the ketogenic diet group compared to the no dietary intervention group (50% vs 18.2%). These studies indicate that the ketogenic diet is an effective therapy for reducing seizure frequency and severity when compared to no dietary intervention.
Lakshminarayanan et al,16 Sharma et al,17 and Sharma et al19 conducted studies comparing modified versions of the ketogenic diet with no dietary intervention for treating drug-resistant epilepsy in children and adolescents. These studies indicate that modified versions of the ketogenic diet are more effective in treating epilepsy in children and adolescents than no dietary intervention. Lakshminarayanan et al16 compared LGIT with no dietary intervention and found that at 3-month follow-up, the change in seizure frequency as compared to baseline was better in the LGIT group compared to the no intervention group (–15% [95% CI, –10% to –21%] vs 10% [95% CI, 6% to 15%], P = .01). Similarly, Sharma et al17 compared MAD with no dietary intervention, while Sharma and colleagues19 compared simplified MAD with no intervention. Both studies demonstrate that the proportion of children with >90% seizure reduction (30% vs 7.7%, P = .005 and 9.5% vs 5%, P = .09, respectively) and >50% seizure reduction (52% vs 11.5%, P < .001 and 56.1% vs 7.5%, P < .0001, respectively) was significantly higher in the dietary intervention group compared to the control group.
Moreover, studies, such as that of Kim et al,14 Gupta et al,15 and Neal et al,18 compared 2 distinct types of ketogenic diet (cKD vs MAD, MAD vs LGIT, and cKD vs MCTKD, respectively) for treating drug-resistant epilepsy in children. These studies revealed comparable efficacy and tolerability of these dietary interventions.
Bergqvist et al21 found that gradual initiation of the ketogenic diet leads to greater seizure reduction and fewer adverse events compared to fasting initiation (at 3 months, >50% seizure reduction: 67% vs 58%, P = .03). On the other hand, Kossoff et al22 found no significant difference in seizure reduction between initial 10 g vs 20 g of carbohydrate/day for MAD. Similarly, Kang et al23 compared short-term versus long-term ketogenic diet and observed comparable outcomes in both groups.
Adverse events were documented in various studies, and nonadherence to the ketogenic diet frequently arises due to challenges related to the diet’s tolerability and feasibility. The most prevalent side effects associated with all forms of the ketogenic diet include gastrointestinal disturbances (such as constipation, vomiting, and diarrhea), lethargy, and weight loss. Other adverse effects encompass anorexia, taste abnormalities, dehydration, dyslipidemia, hyperuricemia, infection, and metabolic acidosis. In terms of tolerability, cKD and MCTKD exhibited similar outcomes.18 However, MAD displayed advantages by being better tolerated and presenting fewer severe side effects compared to cKD.14 Additionally, a study conducted by Bergqvist et al21 illustrated that gradually initiating the ketogenic diet resulted in fewer adverse events and overall better tolerability compared to initiating the diet through fasting, while still maintaining the diet’s efficacy.
DISCUSSION
In comparison with conventional antiepileptic drug therapy with no dietary interventions, the ketogenic diet has demonstrated favorable effects in the treatment of children and adolescents with epilepsy, particularly those with refractory epilepsy. In this population, the ketogenic diet appears to be capable of effectively controlling seizures. As a result of dietary interventions for 3–4 months, patients achieved significant decreases in baseline seizures, as well as notable reductions in seizures by >50% and >90%, and even seizure freedom. Often, achieving a seizure reduction of >50% is considered a clinically meaningful outcome, whereas achieving a reduction of >90% represents a substantial improvement in quality of life. The findings of this study indicate the potential for the ketogenic diet to improve the lives of individuals with epilepsy. The ketogenic diet and its modified versions appear to have comparable efficacy. Patients’ overall well-being and quality of life can greatly improve when they are seizure-free.
The current seizure management plan takes a multifaceted approach. Accurate diagnosis and evaluation, the use of appropriate antiepileptic drugs, implementation of lifestyle changes to reduce triggers and maintain overall health, and, for some people, consideration of alternative treatments like the ketogenic diet are all part of seizure management. The objective is to manage seizures while reducing adverse effects and increasing quality of life. The treatment plan is periodically assessed and modified as necessary.
Lambrechts et al12 found that ketogenic diet therapy was an effective therapy compared to no dietary intervention regarding seizure frequency and severity. Neal et al13 suggested that ketogenic diet therapy should be considered as part of the management plan for children with drug-resistant epilepsy. However, the potential side effects of ketogenic diet therapy such as constipation (33%), vomiting (24%), lack of energy (24%), hunger (22%), and diarrhea (13%) should be carefully considered alongside the risk-benefit of other treatments. A variety of ketogenic diets are available to manage epilepsy, including Atkins, keto, classic, LGIT, and MCT. Keto emphasizes high fats, moderate proteins, and low carbs, while Atkins allows higher protein and carb intake. Traditional ketogenic diets are high in fat and low in carbohydrates and have adequate protein levels. LGIT restricts carbs with low-glycemic index. MCT incorporates MCT oil for higher carbohydrate and protein intake. Kim et al14 concluded that MAD had advantages with respect to better tolerability and fewer serious side effects, but cKD is more suitable as the first line of diet therapy in patients under 2 years of age. Additionally, Gupta et al15 found that the proportion of children achieving seizure freedom at 12 weeks was similar between the MAD and LGIT groups.
Lakshminarayanan et al16 demonstrated the superior efficacy of LGIT when used in conjunction with ongoing antiseizure medications, compared to antiseizure medication alone. LGIT versus no dietary intervention showed that the number needed to treat for more than 50% seizure reduction was 3 and for more than 90% seizure reduction was 10 at 3-month follow-up. In another study, Sharma et al17 found that MAD was effective and well tolerated in children with drug-refractory epilepsy, surpassing the outcomes of conventional antiepileptic drug therapy. The study demonstrated that the proportion of children with >90% seizure reduction (30% vs 7.7%, P=.005) and >50% seizure reduction (52% vs 11.5%, P <.001) was significantly higher in the intervention group compared to the control group. Neal et al18 found that cKD and MCTKD exhibited comparable efficacy and tolerability, and there were no statistically significant differences in mean percentage of baseline seizures between the 2 groups or in seizure frequency reduction. Furthermore, Sharma et al18 demonstrated the feasibility, efficacy, and good tolerability of a simplified version of MAD and found that the proportion of children with >90% seizure reduction (9.5% vs 5%, P=.09, respectively) and >50% seizure reduction (56.1% vs 7.5%, P<.0001, respectively) was significantly higher in the intervention group compared to the control group.
de Kinderen et al20 conducted a study that revealed the effectiveness of the ketogenic diet in reducing seizure frequency; however, there were no significant improvements in the quality of life of the participants. On the other hand, Bergqvist et al21 found that gradually initiating (starting ketogenic diet protocol with 1:1 ratio of fat: carbohydrate+protein by weight, full-calorie-goal meals, and then daily advanced to a 2:1, 3:1, and finally to a 4:1 ratio) the ketogenic diet resulted in fewer adverse events and better overall tolerability, while maintaining the diet’s efficacy. Kossoff et al22 found that for children starting MAD, beginning with a carbohydrate limit of 10 g/day and gradually increasing it to a more tolerable 20 g/day after 3 months may be an optimal approach. Kang et al23 demonstrated that short-term use of the ketogenic diet in children who become spasm-free appears to be justified, with similar outcomes, recurrence rate, and less growth disturbance compared to long-term use.
Overall, the ketogenic diet stands as a viable and efficacious alternative treatment option for children and adolescents with epilepsy. Moreover, the ketogenic diet has displayed favorable safety profiles, with adverse events being generally manageable and outweighed by the potential benefits.
Strengths and Limitations
The strengths of the current review include the comprehensive integration of evidence from 5 countries across 3 continents, alongside the meticulous adherence to the PRISMA protocol to evaluate evidence quality. Only RCTs were included, which adds to the strength in the level of evidence.
This review possesses certain limitations that should be acknowledged. First, the inclusion of only RCTs may have limited its comprehensiveness. Second, the available evidence regarding the efficacy of ketogenic dietary therapy for epilepsy is constrained by small sample sizes, high attrition rates, lack of evidence in adults, and the presence of adverse effects associated with ketogenic diet therapy, including gastrointestinal issues, weight loss, and lethargy.
CONCLUSION
In conclusion, the ketogenic diet represents a compelling and effective alternative treatment modality for children and adolescents suffering from epilepsy. Its ability to significantly alleviate seizures, coupled with its generally acceptable safety profile, positions it as a valuable supplemental part of the treatment regimen in the management of pediatric epilepsy. Nonadherence to the ketogenic diet is a common issue, often stemming from challenges associated with the tolerability and feasibility, but continued research and improvements in the implementation and monitoring of the diet hold the potential for even greater success in the future.
Article Information
Published Online: June 25, 2024. https://doi.org/10.4088/PCC.23r03661
© 2024 Physicians Postgraduate Press, Inc.
Submitted: October 24, 2023; accepted February 27, 2024.
To Cite: Parveen D, Jain V, Kannan D, et al. Advances in ketogenic diet therapies in pediatric epilepsy: a systematic review. Prim Care Companion CNS Disord. 2024;26(3):23r03661.
Author Affiliations: Ganesh Shankar Vidyarthi Memorial Medical College, Kanpur, India (Parveen); Department of Pediatrics, Jawaharlal Nehru Medical College, Ajmer, India (Jain); Government Villupuram Medical College and Hospital, Mundiyampakkam, India (Kannan); Department of Medicine, University of Washington, Seattle, Washington (Mandava); GI Medicine and Pediatrics, Baylor College of Medicine, Houston, Texas (Urazbayeva); Neonatal Special Care Unit, Port of Spain General Hospital, Port of Spain, Trinidad and Tobago (Che-Marie); Department of Neonatology, Port of Spain General Hospital, Port of Spain, Trinidad and Tobago (Jogie); RCSM Government Medical College, Kolhapur, India (Patel); Consultation Liaison Psychiatry, Mount Sinai Beth Israel, New York, New York (McCarthy); Department of Psychiatry, Child and Adolescent Division, Bronxcare Hospital, Bronx, New York (Wilson); Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, New York (Patel); Department of Public Health, Icahn School of Medicine at Mount Sinai, New York, New York (Hsieh); Department of Pediatrics Neurology, Sunrise Children’s Hospital, HCA Far West, Las Vegas, Nevada (Chavda); Department of Pediatrics, Bassett Healthcare Network, Cooperstown, New York (Thakker).
Corresponding Author: Ya-Ching Hsieh, MD, MPH, MBA, Department of Public Health, Icahn School of Medicine at Mount Sinai, 1 Gustave L. Levy Pl, New York, NY 10029 ([email protected]).
Drs Parveen and Jain contributed equally to this work.
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Compared to conventional antiepileptic drug therapy with no dietary interventions, the ketogenic diet demonstrated favorable effects in the treatment of children and adolescents with epilepsy, particularly those with refractory epilepsy.
- The ketogenic diet displayed favorable safety profiles, with adverse events being generally manageable and outweighed by the potential benefits.
- Nonadherence to the ketogenic diet is a common issue, often stemming from challenges associated with tolerability and feasibility.
References (23)

- Rezaei S, Abdurahman AA, Saghazadeh A, et al. Short-term and long-term efficacy of classical ketogenic diet and modified Atkins diet in children and adolescents with epilepsy: a systematic review and meta-analysis. Nutr Neurosci. 2019;22(5):317–334. PubMed CrossRef
- World Health Organization, Epilepsy. Accessed February 9, 2023. https://www.who.int/news-room/fact-sheets/detail/epilepsy
- Epilepsy Foundation, Causes of Epilepsy in Childhood. Accessed August 27, 2013. https://www.epilepsy.com/parents-and-caregivers/kids/causes-epilepsy-childhood
- UpToDate. Evaluation and Management of Drug-Resistant Epilepsy. Accessed December 19, 2023. https://www.uptodate.com/contents/evaluation-andmanagement-of-drug-resistant-epilepsy
- Roehl K, Sewak SL. Practice paper of the academy of nutrition and dietetics: classic and modified ketogenic diets for treatment of epilepsy. J Acad Nutr Diet. 2017;117(8):1279–1292. PubMed CrossRef
- Martin K, Jackson CF, Levy RG, et al. Ketogenic diet and other dietary treatments for epilepsy. Cochrane Database Syst Rev. 2016;2:CD001903. PubMed CrossRef
- Martin-McGill KJ, Bresnahan R, Levy RG, et al. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2020;6(6):CD001903. PubMed CrossRef
- Kossoff EH, Zupec-Kania BA, Auvin S, et al. Optimal clinical management of children receiving dietary therapies for epilepsy: updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open. 2018;3(2):175–192. PubMed CrossRef
- Ułamek-Kozioł M, Czuczwar SJ, Januszewski S, et al. Ketogenic diet and epilepsy. Nutrients. 2019;11(10):2510. PubMed
- de Brito Sampaio LP. Ketogenic diet for epilepsy treatment. Arq Neuropsiquiatr. 2016;74(10):842–848. PubMed CrossRef
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. PubMed CrossRef
- Lambrechts DAJE, de Kinderen RJA, Vles JSH, et al. A randomized controlled trial of the ketogenic diet in refractory childhood epilepsy. Acta Neurol Scand. 2017;135(2):231–239. PubMed
- Neal EG, Chaffe H, Schwartz RH, et al. The ketogenic diet for the treatment of childhood epilepsy: a randomised controlled trial. Lancet Neurol. 2008;7(6):500–506. PubMed CrossRef
- Kim JA, Yoon JR, Lee EJ, et al. Efficacy of the classic ketogenic and the modified atkins diets in refractory childhood epilepsy. Epilepsia. 2016;57(1):51–58. PubMed CrossRef
- Gupta S, Dabla S, Kaushik JS. Modified Atkins diet vs low glycemic index treatment for drug-resistant epilepsy in children: an open label, randomized controlled trial. Indian Pediatr. 2021;58(9):815–819. PubMed
- Lakshminarayanan K, Agarawal A, Panda PK, et al. Efficacy of low glycemic index diet therapy (LGIT) in children aged 2–8 years with drug-resistant epilepsy: a randomized controlled trial. Epilepsy Res. 2021;171:106574. PubMed CrossRef
- Sharma S, Sankhyan N, Gulati S, et al. Use of the modified Atkins diet for treatment of refractory childhood epilepsy: a randomized controlled trial. Epilepsia. 2013;54(3):481–486. PubMed CrossRef
- Neal EG, Chaffe H, Schwartz RH, et al. A randomized trial of classical and medium-chain triglyceride ketogenic diets in the treatment of childhood epilepsy. Epilepsia. 2009;50(5):1109–1117. PubMed CrossRef
- Sharma S, Goel S, Jain P, et al. Evaluation of a simplified modified Atkins diet for use by parents with low levels of literacy in children with refractory epilepsy: a randomized controlled trial. Epilepsy Res. 2016;127:152–159. PubMed CrossRef
- de Kinderen RJA, Lambrechts DAJE, Postulart D, et al. Research into the (Cost-) effectiveness of the ketogenic diet among children and adolescents with intractable epilepsy: design of a randomized controlled trial. BMC Neurol. 2011;11:10. PubMed
- Bergqvist AGC, Schall JI, Gallagher PR, et al. Fasting versus gradual initiation of the ketogenic diet: a prospective, randomized clinical trial of efficacy. Epilepsia. 2005;46(11):1810–1819. PubMed CrossRef
- Kossoff EH, Turner Z, Bluml RM, et al. A randomized, crossover comparison of daily carbohydrate limits using the modified Atkins diet. Epilepsy Behav. 2007;10(3):432–436. PubMed CrossRef
- Kang HC, Lee YJ, Lee JS, et al. Comparison of short- versus long-term ketogenic diet for intractable infantile spasms. Epilepsia. 2011;52(4):781–787. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!