Mayo Clinic researchers have drafted new criteria for a memory-loss disorder that appears in older adults that looks a lot like Alzheimer’s.
This eerily similar condition – which the Mayo scientists call Amnestic Neurodegenerative Syndrome, or LANS – also attacks the brain’s limbic system.
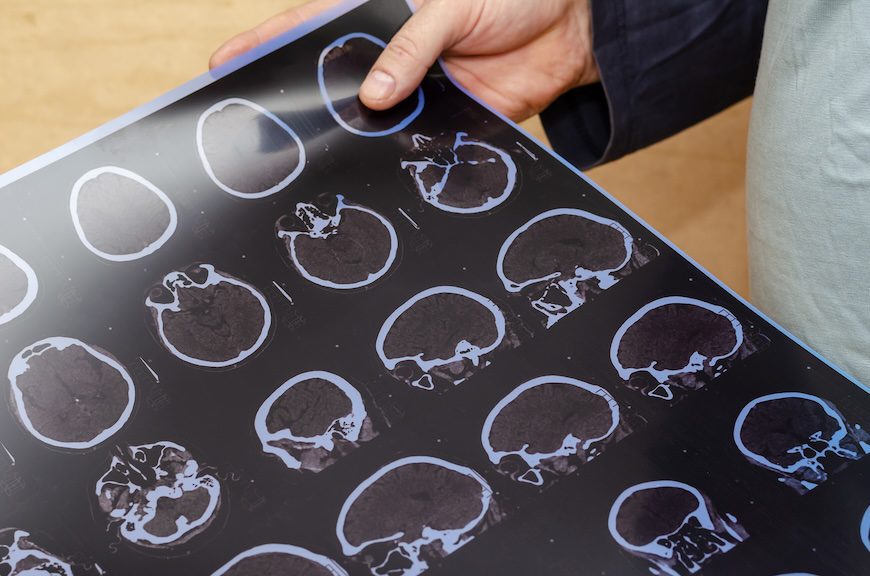
“In our clinical work, we see patients whose memory symptoms appear to mimic Alzheimer’s disease, but when you look at their brain imaging or biomarkers, it’s clear they don’t have Alzheimer’s,” David T. Jones, M.D., a Mayo Clinic neurologist and senior author of the study, explained.
But it’s not all bad news. The researchers found that this disorder appears to advance more slowly and offers a more optimistic prognosis. And this classification should help caregivers better diagnose and treat their memory-loss patients.
Ruling Out Alzheimer’s Offers Diagnostic Hope
Until now, doctors could only confirm the presence of LANS with a post-mortem brain tissue analysis – not unlike chronic traumatic encephalopathy (CTE).
These new criteria, which researchers just published in the journal Brain Communications, offer a way for neurologists and their colleagues to classify the condition in patients struggling with these symptoms. It also offers a way forward in delivering more accurate diagnoses and treatments.
The researchers developed the criteria, which rely on factors such as age, severity of impairment, brain scans, and biomarkers indicating the deposits of specific proteins in the brain, with the help of data from more than 200 participants. The team pulled the numbers from multiple datasets, such as the Mayo Clinic Alzheimer’s Disease Research Center, the Mayo Clinic Study of Aging, and the Alzheimer’s Disease Neuroimaging Initiative.
“Until now, there has not been a specific medical diagnosis to point to, but now we can offer them some answers,” Jones added. “This research creates a precise framework that other medical professionals can use to care for their patients. It has major implications for treatment decisions, including amyloid-lowering drugs and new clinical trials, and counseling on their prognosis, genetics, and other factors.”
Still More Work to Do
But the paper’s first author, Nick Corriveau-Lecavalier, Ph.D., insists that plenty of work remains. These findings simply build upon ongoing efforts to untangle neurological conditions that often look the same or hit at the same time. The problem is that these conditions can demand dramatically different treatments.
“Historically, you might see someone in their 80s with memory problems and think they may have Alzheimer’s disease, and that is often how it’s being thought of today,” Corriveau-Lecavalier said. “With this paper, we are describing a different syndrome that happens much later in life. Often, the symptoms are restricted to memory and will not progress to impact other cognitive domains. So the prognosis is better than with Alzheimer’s disease.”
Without no hint of Alzheimer’s, the researchers looked for another potential culprit – “a buildup of a protein called TDP-43 in the limbic system that scientists have found in the autopsied brain tissue of older adults.” Earlier research classified the build-up of these protein deposits as limbic-predominant age-related TDP-43 encephalopathy, or LATE. And the authors of this new paper suggest that these protein deposits could be linked with the newly classified memory loss syndrome. But there are several other potential causes
With these new clinical criteria, practitioners can soon diagnose LANS in patients more easily and help those with memory loss understand treatment options and disease progression.
Further Reading
FDA Approves New Alzheimer’s Drug
Cognitive Decline Threatens Financial Stability of Older Americans