Brain zaps – sometimes referred to as brain shivers, brain flips, or brain shocks – is a colloquial term used to describe a group of sensory disturbances typically associated with discontinuation or dosage changes of certain medications, most commonly antidepressants.
Most people – even trained professionals – don’t completely understand brain zaps, making it difficult to diagnose because of the different ways patients describe it.
What Causes Brain Zaps?
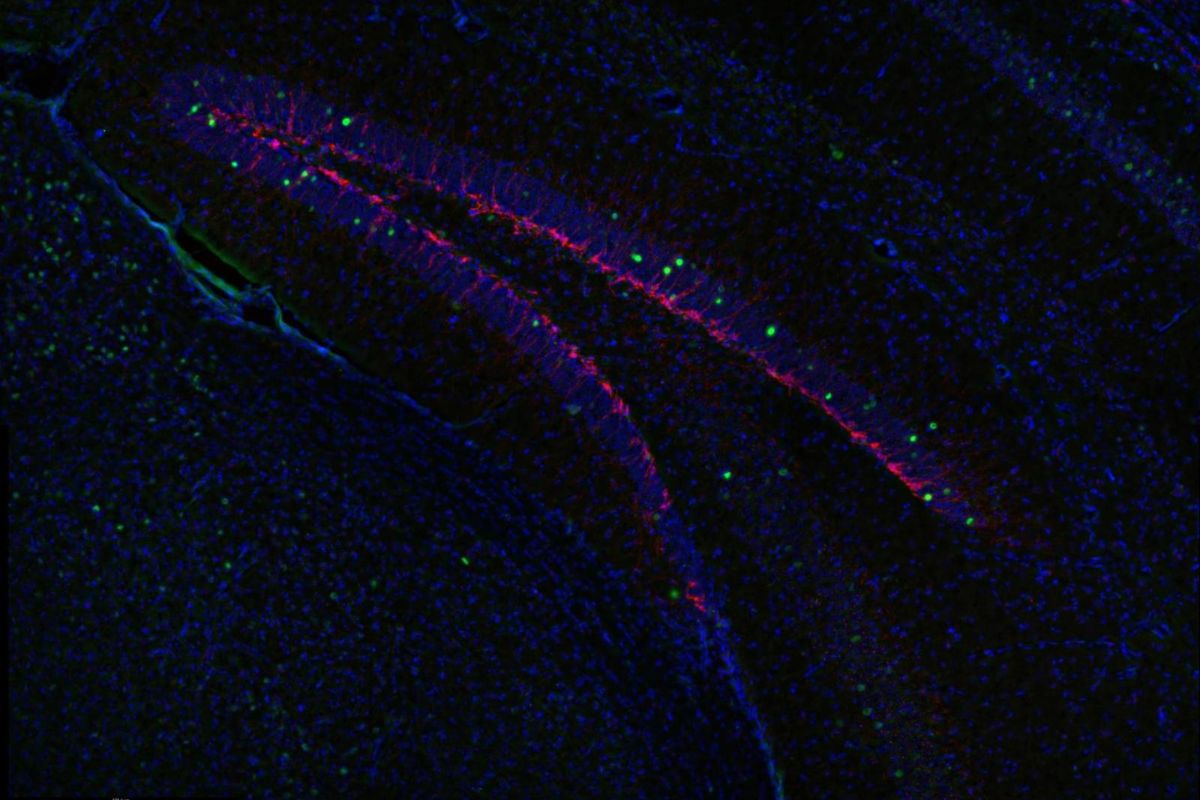
That’s the million-dollar question. The exact mechanism behind the occurrence of these sensory disturbances remains shrouded in mystery. Researchers have suggested that sudden changes to neurotransmitter levels or receptor sensitivity of important neurotransmitters like serotonin and norepinephrine could be responsible.
These changes likely affect electrical signaling within the brain, leading to several symptoms associated with antidepressant withdrawal, collectively referred to as antidepressant discontinuation syndrome (ADS).
Evidence is piling up in support of this theory.
- 39.9% of respondents reported discontinuing their antidepressant medication before the symptoms occurred.
- While other commonly reported triggers included tapering off (25.7%) or skipping a dose (12.5%).
- Longer antidepressant use appears to be more commonly associated with brain zaps (7.8% in people who have been on medications for less than 60 days vs. 36.4% in those who’ve been on it between 60 days and two years). Notably, antidepressant use for more than two years showed a consistently declining prevalence.
- Researchers have noted more frequent episodes in individuals discontinuing serotonin and norepinephrine reuptake inhibitors (SNRIs) than those using selective serotonin reuptake inhibitors (SSRIs). Some suggest it’s because SNRIs interact with a wider range of neurotransmitters, so they’re likely to have more diverse effects on the brain.
- SNRIs also typically have a shorter half-life than SSRIs. This suggests the body eliminates them more quickly, so they’re more prone to sudden changes in neurotransmitter levels and the risk of experiencing brain zaps.
According to the same study, the antidepressants most commonly associated with the condition were venlafaxine (23.3%), sertraline (19.6%), paroxetine (14.7%), citalopram (13.4%), duloxetine (10.7%) and escitalopram (9.2%). Fluoxetine and bupropion ranked near the bottom of the list of offending antidepressants (3.1% and 2.7% respectively).
Other suggested causes include headaches, anxiety, and other medical conditions.
What Do Brain Zaps Feel Like?
One reason these side effects were long overlooked by physicians is the non-specific way they present. Patients have described the sensation in several ways:
- A sudden jolt of electricity in the brain.
- Dizziness.
- Vertigo.
- A buzzing sound.
- Bright flashes of light.
- A brief lapse of consciousness or confusion, commonly described as a “brain blink.”
- The sensation of “hearing” their eyes move.
Interestingly, patients typically describe it along with lateral eye movements. Experts insist that this ocular phenomenon can sometimes trigger these episodes.
How Common Are Brain Zaps?
Several studies on the side effects of antidepressant discontinuation have described a “shock-like” sensation as part of the symptoms.
However, it’s tough for scientists to pin down the prevalence of this condition because of the dearth of dedicated research on the topic and the multiple ways patients describe the symptoms.
Can Anyone Stop Them?
Despite the lack of research, most neurologists agree the condition isn’t necessarily harmful and typically self-limited.
This also probably explains why there’s still no definitive cure for brain zaps. However, there are a few practices that have been tried with varying degrees of success.
- Many patients who experience the symptoms simply continue the medication.
- Some physicians recommend switching to a non-traditional antidepressant, most successfully fluoxetine. However, fluoxetine only halted the symptoms in 50 percent of cases.
- Researchers found that gradually weaning patients off antidepressants helped reduce the occurrence of brain zaps. But it’s not entirely effective.
- Fortunately, the sensory disturbances disappear eventually as the body adjusts to the change in brain chemistry.
Further Reading
Brain Zaps: An Underappreciated Symptom of Antidepressant Discontinuation
In SSRI Withdrawal, Brain Zaps Go from Overlooked Symptom to Center Stage
3 Key Studies on Brain Zaps in Antidepressant Withdrawal
Read the Full Study
Read MoreBrain Zaps: An Underappreciated Symptom of Antidepressant Discontinuation
<div>Brain zaps are a poorly understood symptom of antidepressant discontinuation, which require further study for both better prevention and treatment. This article describes the characteristics of brain zaps and their effect on quality of life.</div>