Abstract
Importance: Amid and following the COVID-19 pandemic, there has been a growing focus on understanding the underlying etiology of the mental health crisis in children and youth. However, there remains a dearth of empirically driven literature to comprehensively explore these issues. This narrative review delves into current mental health challenges among children and youth, examining perspectives from both pre-pandemic and pandemic periods.
Observations: Research highlights reveal concerning statistics, such as 1 in 5 children experience mental health disorders. The pandemic exacerbated these issues, introducing stressors such as job losses and heightened anticipatory anxiety. Race relations have emerged as a significant public health concern, with biases impacting students, particularly affecting Asian, black, and multiracial individuals. Substance use trends indicate a rise in overdose deaths, particularly among adolescents, with cannabis use linked to adverse outcomes. Increased screen time and income disparities further compound mental health challenges.
Conclusions and Relevance: Proposed public health mitigation strategies include improving access to evidence based treatments, implementing legislative measures for early identification and treatment of developmental disorders, and enhancing suicide prevention efforts. School-based interventions and vocational-technical education are crucial, alongside initiatives targeting sleep hygiene, social media usage, nutrition, and physical activity. Educating health care professionals about both physical and mental health is essential to address workforce burnout and effectively manage clinical complexities.
Prim Care Companion CNS Disord 2024;26(5):24nr03747
Author affiliations are listed at the end of this article.
Adolescence is a critical period of transformation, extensively acknowledged across cultures. A transition from childhood to adulthood necessitates a phase of “storm and stress,” a period of inherent volatility typically resolved by the age of 20. It is also observed that many lifelong psychopathologies emerge by the age of 14. Consequently, developmental psychology, child and adolescent psychiatry, and psychiatric epidemiology have focused on adolescent development to investigate the etiopathogenesis of psychiatric disorders.
The field of epigenetics, which examines the patterning of risk and resilience throughout development, offers a comprehensive scientific framework for evaluating the physiological, emotional, social, moral, and cognitive changes that define human maturation. This approach transcends the traditional “nature versus nurture” debate. Although early theorists were incorrect in asserting that all individuals must undergo a period of storm and stress, they correctly highlighted the importance of this developmentally sensitive and highly interactive phase in understanding both typical and atypical development, as well as the onset of psychiatric conditions.
When change proceeds coherently, we think of teens as maturing normally, thereby enabling parents, teachers, and peers to respond reciprocally to emerging shifts in roles and responsibilities. But intricate biological change rarely unfolds evenly, and the phrase “moving parts get broken” aptly and succinctly frames the context in which adolescent psychopathology takes root. This notion is not specific to adolescent brain development. For example, the more common neoplastic syndromes take root in biological systems with high volatility like squamous cells that comprise the mucosa lining the gut. In those systems, complex gene × environment interactions make errors in cell growth, apoptosis, and communication more likely. It follows, therefore, that the volatility of the gene × environment interactions comprising adolescent development constitute a sensitive, informative, and meaningful window into emerging trends in human development and psychiatric epidemiology.
Alarmingly, rates of adolescent psychopathology have been skyrocketing since 2011.1 Because teenage psychopathology is enduring across the lifespan, this trend is particularly worrisome. Today’s teens are the proverbial canaries in the coal mine, and it is our incumbent obligation to learn more about the changes in risk/resilience patterning that seem to be driving this incontrovertible trend. In the absence of greater insights into this phenomenon, the foreboding likelihood of even greater rates of psychopathology cannot be ignored—especially as these teens become parents. In the last few years, the mental health crisis of children and adolescents has been in the national headlines. These developments led the American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry (AACAP), and Children’s Hospital Association to declare a national emergency in October 2021 and the US Surgeon General to issue an advisory on the youth mental health crisis during the COVID-19 pandemic.2 The White House has echoed its focus on the children and adolescent mental health crisis with major policy statement announcements in the 2022 and 2023 State of the Union Address. The overarching premise of these plans is to address imminent short-term issues and strategic planning for the future. For example, in 2023, the US Department of Health and Human Services committed 55 million dollars to youth mental health care including the expansion of school-based mental health services.3 The mental health crisis remains a poorly described term, with multiple interacting variables and factors that affect the mental health of children, adolescents, and transitional-age youth. Therefore, it is critical to examine the nature and extent of these issues, as understanding the context underlying the empirical data is essential for engaging stakeholders and recognizing the insidious and pervasive nature of these disorders throughout the lifespan.
Furthermore, the continual increase in the overall burden of this problem will have significant implications for the current state of health care and society. Addressing the youth mental health crisis is not only a matter of urgency but also one that necessitates a comprehensive and sustained effort from all sectors of society.
METHODS
A comprehensive search of databases was conducted including PubMed, PubMed Central, PsycINFO, Cochrane Library, Google Scholar, Scopus, MEDLINE, and Web of Science. The search was performed from the date of inception of each database to the date of the search (February 1, 2024). Keywords/controlled vocabulary used included cannabis, legal, mental health, bullying, racism, opiates, parenting, emergency, social media, crisis, and school. Filters were applied to identify articles specific to child and adolescent populations between the ages of 0 and 18 years. While the search criteria were broad, we tried to identify articles published after 2014 and especially over the last 5 years. Although the search focused on articles based on mental health emergencies, we also included some broader topics in the narrative review. The search encompassed all languages. The inclusion criterion for the manuscript was any published material focusing on mental health emergencies in the child and adolescent population. We included book chapters and expert opinions along with peer-reviewed articles, given the nature of some topics and the scarcity of evidence. No restrictions were applied based on publication type. We searched for additional data manually through various websites such as the Centers for Disease Control (CDC), Health Resources and Services Administration, and Public Health Data. Reverse citations were also used to update the manuscript.
A total of 11,263 articles were identified upon initial screening after duplicate removal. The titles and abstracts were reviewed, and 167 articles met the initial inclusion criteria, 87 of which were used for the initial draft, while 30 articles were subsequently added through manual search and reverse citations.
RESULTS
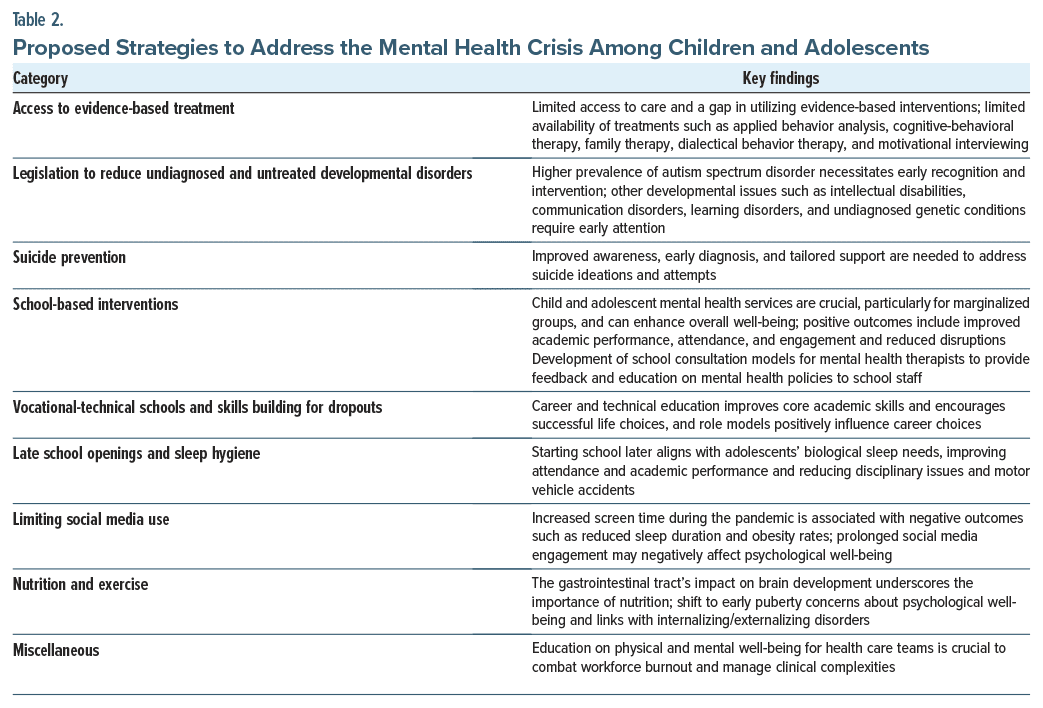
The following sections provide a comprehensive summary of the findings. Participants aged 3–18 years represent a diverse cohort in terms of age, ethnicity, race, geographical location, and gender-related variables. While this review encompasses a broad spectrum of topics, an exhaustive examination of specific areas is beyond the scope of this article. However, we have identified several critical issues and developed frameworks for potential solutions targeted at clinicians, families, policymakers, and stakeholders in the field of child and adolescent mental health. Detailed summaries of these results are presented in Table 1 and Table 2.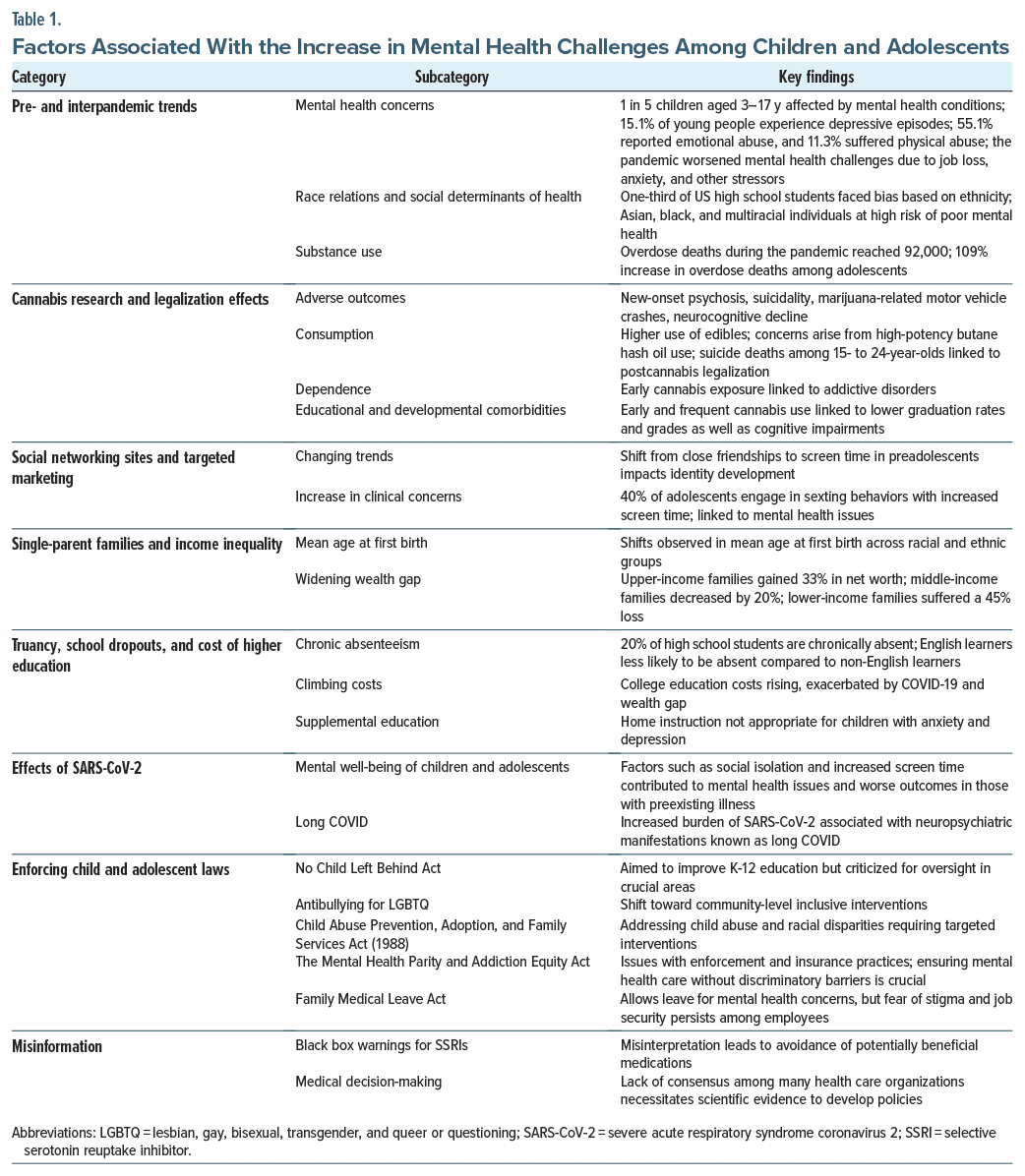
How Do the Pre-Pandemic and Interpandemic Trends Differ?
Interpandemic data about the prevalence of child and adolescent mental health conditions shed light on the scope of the problem. However, practicing clinicians attest to the mounting burden in the last decades. About 20% or approximately 1 in 5 children (aged 3–17 years) in the United States have a mental, emotional, developmental, or behavioral disorder.4 Suicide rates among youth aged 10–24 years in the United States increased by 57% from 2000 to 2018.5 Mental illness has been found to start by age 14 in 50% of cases, and in 75% of cases, symptoms become clearer by the age of 24.6 The CDC 2018–2019 data suggest that 20.1% had major depressive episodes, with a youth prevalence of 1 in 5, and about 36.7% had persistent feelings of sadness or hopelessness, with 75% of youth showing severe impairment.7 The recent statistics reveal that the prevalence of deaths by suicide between 10 and 19 years of age is 7 in 100,000.8 There are striking observations among children living below 100% of the federal poverty level with more than 1 in 5 (22%) having a mental, behavioral, or developmental disorder compared to children not living below the federal poverty level. Likewise, the prevalence of suicide for adolescents and young adults is higher in rural than in urban communities.9 The trends underscore rural-urban, race, poverty, access to education, and gender-linked variability in the prevalence of mental disorders and the resulting health inequity.
According to the CDC, in 2020, emergency department (ED) visits for mental health reasons increased by 24% for ages 5–11 and by 31% for ages 12–17.10 ED visits among female adolescents with eating disorders doubled during the pandemic.11 The Adolescent Behaviors and Experiences Survey (ABES) (January–June 2021) reports about 55.1% of respondents suffered emotional abuse from a parent or another adult in their house in the preceding year, and 11.3% suffered physical abuse.12 The abuse results in traumatic stress and has a positive correlation with increased suicidality.13 One-third of Americans live in designated mental health professional shortage areas.14 The indirect effects on mental health after school closures and lockdowns have been extensively reported globally and cross-culturally. Social isolation remains a key perpetuating factor, and the worsening of untreated mental health without access to treatment leads to the surge. Many providers closed for business during the pandemic; schools where 75% of youth receive mental health treatment also closed, and hospitals functioned at limited capacity. In summary, worsening of an existing crisis would be a more appropriate reframing of these developments. During the pandemic, the destigmatization drives may have contributed to the increase in individuals and families seeking treatment.
Emerging Issues
During the pandemic, there was a continuation of existing issues as well as many new events that further accentuated mental health problems. Parental job loss, financial crisis, overcrowding at home, pandemic-related deaths of caregivers, and increased rates of domestic violence were directly associated with the pandemic and had an impact on the development of children’s psychological problems.15 School closure, increased screen time, lack of physical activity, disruption of the sleep rhythm, and heightened anxiety due to the unpredictable nature of the COVID-19 virus were key determinants for added risks. These factors had an additive and deleterious effect on those who already had an established mental illness.16 The 2021 National Survey on Drug Use and Health revealed that 45.1% of youth aged 12–17 perceived the COVID-19 pandemic to affect their mental health negatively.17 Adolescents who did not receive treatment for their mental health concerns were at risk of substance use, as supported by recent statistics that found an 8.5% comorbid prevalence of substance use disorders.18
Race relations. After George Floyd’s death (2020), there were calls for structural reforms to address systematic racism, bias, and bigotry.19 The unprecedented media coverage and global outrage were followed by actionable measures to address racism as a social determinant of health. Interestingly, in 2019, the AAP policy statement warned about the pernicious effects of racism on the health status of children, adolescents, emerging adults, and their families.20 The ABES data revealed that about one-third of all US high school students experienced bias at school due to race and ethnicity, which is concerning.12 Asian, black, and multiracial students were found to be at the receiving end and at heightened risk for poor mental health.21 There were some links observed, with a 50% surge in suicide rates in girls and young adolescent black and Hispanic youth since 2007.21
The worsening opioid epidemic and mental health impact. The opioid crisis is far from over; in many instances, it is far worse than in previous years. In 2020 during the COVID-19 pandemic, overdose deaths jumped to previously unseen levels of nearly 92,000.22 The overall estimated number of deaths during the first 6 months of 2021 was 53,000, higher than any continuous 6- month period in 2020.22 The CDC’s State Unintentional Drug Overdose Reporting System (SUDORS) found troubling trends among those aged 10–19 years during a 3- year period. Comparing SUDORS data from the last half of 2019 and the last half of 2021, the authors23 found a 109% increase in average monthly overdose deaths among adolescents. This increase in overdose rates is believed to be due to illicitly manufactured fentanyl, which increased deaths by 182% in this age group.24 A parallel research line also suggests that a substance use history or misuse of opiates in parents doubles the risk of suicide attempts in offspring.
Advances in cannabis research and effects postlegalization. In the last decade, postlegalization cannabis use and its mental health effects on youth have become a concern. By 2022, 36 states legalized medical use, and 18 permitted recreational use. It is crucial to study the impact of marijuana policies on adolescents, given risks such as increased substance use, psychosis, suicidality, impaired driving, and cognitive decline, including educational underperformance.25–37 Despite no significant recent data change, longitudinal analyses are lacking. Legalization has led to more potent cannabis products and diverse consumption methods such as vaping and edibles.38,39 From 2008 to 2017, the National Institute on Drug Abuse reported the average Δ9-THC concentration rose from 8.9% to 17.1%. In legal states, adolescents have higher rates of using edibles (51.4% vs 37.2%) and concentrates (22.0% vs 15.4%) than in nonlegal states.40,41 High-potency products, such as butane hash oil (“dab” or “shatter”), raise concerns for adverse effects on adolescents, including acute psychosis and cardiotoxicity.41–44 Vaping cannabis among adolescents is rising rapidly across demographics and faster than occasional use.45
Adolescent cannabis exposure has been shown to increase the risk of developing psychosis and schizophrenia in adulthood by up to twofold.46 This dose-dependent finding is replicated in large cohort studies controlling for various factors, including family history, psychosis preceding cannabis use, and intoxication at final assessment.47 The brain’s dopamine system may be vulnerable to cannabis during adolescence, potentially contributing to psychotic disorders. Regulation is needed to limit youth access.
Another mental health risk for youth across all races and socioeconomic groups is suicide, the second leading cause of death in people aged 10–24.48 Studies show higher rates of suicide attempts and completions among heavy cannabis users.49 After legalization in Washington state, a modest increase in suicide deaths in 15–24-year olds was observed.50 A meta-analysis found adolescent cannabis consumption to be linked to higher odds of depression, suicidal ideations, and attempts in young adulthood, even without premorbid conditions.51 Literature reviews indicate that adolescents using cannabis, even at subclinical levels, face higher risks of suicidal thoughts and behaviors compared to nonusers.50,51 Physicians should screen adolescent cannabis users for suicide risk and provide informed consent about these risks.
Early cannabis use is linked to increased addiction risk and impaired cognitive development. Cross-sectional and longitudinal studies show a significant relationship between adolescent cannabis exposure and higher likelihood of developing substance use disorders later in life.35,52–54 A longitudinal study illustrates that daily use before age 17 increases the likelihood of cannabis dependence and illicit drug use.55 Many adolescents do not view cannabis as addictive, highlighting the need for public health campaigns. Adolescent cannabis use also correlates with lower academic achievement, including reduced odds of high school graduation and degree attainment, suggesting causation.56 Impairments in psychomotor skills, emotional control, learning, memory, and executive function may contribute to higher absenteeism, reported school difficulty, and decreased college degree attainment.57 More research is needed on potential adverse psychosocial outcomes from adolescent cannabis exposure during this critical developmental stage. Cognitive impairment during adolescence can have long-term effects.58
Suspensions for cannabis use may further hinder graduation and academic performance. In Colorado, high school suspensions for cannabis increased from 17% to 23% postlegalization in 2012.59 Even during the COVID 19 pandemic (2019–2021), cannabis remained the top reason for law enforcement contacts in Colorado schools.60 Adopting remedial methods like psychoeducation instead of suspensions has reduced cannabis use.60 School-based health centers providing confidential counseling, screening, brief intervention, and referral to treatment can lower youth cannabis use, highlighting the importance of prevention programs in schools.60
Cannabis use risks should be emphasized in general drug education and mental health programs in schools. Educators must explicitly address the potential mental health dangers of frequent cannabis consumption, focusing on high-risk groups like those with a family history of psychosis or substance use. This messaging should target both cannabis users and their peers, who significantly influence behaviors and habits in this age group.
Social media and targeted marketing. An influential psychiatrist, Dr Harry Stack Sullivan, wrote in his seminal work that preadolescents (aged 10–13 years) enter a period of chumship to find someone and share their innermost thoughts and feelings.61 During this process, he or she can explore and reveal both positive and negative aspects of self without fear of being judged in an environment of total acceptance. This is critical for the development of personality, accepting many negative self-evaluations and others’ points of view. There is a shift in how children and adolescents are spending time. The lack of unstructured play and average screen time of 7 hours during the pandemic underscores the problem. Cross-sectional studies have found a correlation between time spent on the internet and mental health.62–65 Screen time almost doubled during the pandemic, which has serious negative clinical implications. Prospective studies have found cyber victimization, sleep disturbance, gaming addiction, and disruption of protective factors such as in-person social activity and physical mobility.64,65 Sexting has also increased with one study estimating that 40% of adolescents engage in sexting behaviors.66 Given its association with coercion and victimization at a young age, sexting is associated with poor mental health outcomes.67
Single-parent families and income inequality. In 2020, about 15 million children and youth lived with a single mother in the United States, and about 3.27 million children lived with a single father.68 A study reported that the United States has the world’s highest rate of children living in single-parent households.69 Although since 2000, the mean age at first birth has increased for all race and ethnic origin groups, there is significant intergroup variability, as American Indian or Alaska Native mothers had the youngest mean age at first birth in 2014, and Asian or Pacific Islander mothers had the oldest.70 The wealth gap between upper-income and lower- and middle-income families has grown wider. As of 2016, upper-income families had 7.4 times as much wealth as middle-income families and 75 times as much wealth as lower-income families. These ratios were 3.4 and 28, respectively, in 1983.70 These factors emphasize the social determinants of health and are beyond the scope of this article but are included to highlight critical confounding variables that need further examination.
Truancy, school dropouts, and cost of higher education. About 7 million students missed 15 or more days of school in 2015–2016, representing 16% of the student population. More than 20% of high school students are chronically absent compared to over 14% of middle school students.71 English-speaking learners are about 1.2 times less likely to be chronically absent than non-English learners, 14% vs 16%, respectively. Students with disabilities are 1.5 times more likely to be chronically absent than those without disabilities.72 The Individuals with Disabilities Education Act aims to ensure all students with disabilities receive a free, appropriate education, but chronic absenteeism hinders this goal.73 Children from low-income families who start with high test scores often struggle to maintain them. The Elementary and Secondary Education Act seeks to close achievement gaps by providing federal funding to schools with impoverished children.74 A report indicates that 81% of principals use these funds for professional development.75 College costs have increased by 169% since 1980, with significant tuition spikes in many southern states for the lowest-income families.76
Hospital homebound (HHB) programs support students with chronic severe medical illnesses who cannot attend school. HHB criteria and duration vary by state.77 For example, in West Virginia, children can receive HHB education for extended periods if medically necessary.78 However, HHB outcomes are mixed.79,80 For children with mental health conditions, particularly school avoidance, HHB may be counterproductive, as it can foster parental accommodations. Parents sometimes choose HHB to avoid truancy charges. Uniformity in contingency management programs for school avoidance and modifications to truancy laws may help address the mental health burden. Providers need to be educated that HHB is not appropriate for those with social anxiety and school avoidance.
Indirect and direct effects of the COVID-19 pandemic. The extensively studied indirect effects of the COVID-19 pandemic on the mental health of children and adolescents have multiple predisposing and perpetuating factors not limited to social isolation, screen time, lack of physical activity, heightened perceived risks, and parenting stress. These factors are attributed to a surge in mental health emergency visits, self-reports of symptoms of anxiety and depression in adolescents, and externalizing disorders among college aged youths.81 The underlying cellular and molecular mechanisms attributing to the neuroinvasiveness and neurovirulence of SARS-CoV-2 remain poorly understood. Post–COVID-19 neuropsychiatric manifestations or long COVID are widely accepted in adults, and emerging evidence supports its presence in youth.18 With the emergence of new variants and higher rates of infections, there is a gap in the information about the true estimates of long COVID. The trends in the data on overall duration, pathophysiology, risk factors, and impairments in social and academic areas are critical to understanding the burden of long COVID in children and adolescents.
Strengthening systems and laws and addressing violations. In recent decades, there has been strong advocacy for legislation and policy to meet the needs of children and adolescents in the United States. A statute requires critical appraisals to assess enforcement gaps, violations, and the need for amendments. The Family First Prevention Services Act aims to use evidence-based treatments, increase community well-being, and decrease out-of-home care entries and expenditures.82 The No Child Left Behind Act and Every Student Succeeds Act govern K-12 public education policy. However, these reforms have been criticized for focusing on raising test scores while overlooking individualized educational planning and testing requirements.83
There is skepticism about enforcing antibullying laws, including protection for LGBTQ youth. Bullying is a pervasive problem with high prevalence among children and adolescents. Although many antibullying statutes and practices exist, their effectiveness remains unclear.84
Under the Child Abuse Prevention, Adoption, and Family Services Act of 1988, a report of alleged child abuse is made every 10 seconds in the United States.85 In fiscal year 2020, an estimated 1,750 children died from abuse and neglect at a rate of 2.38 per 100,000 children.85 African American child fatalities (5.90 per 100,000) are significantly higher than those of white (1.90 per 100,000) and Hispanic children (1.65 per 100,000). In 2020, about 4.68 children died each day from abuse and neglect in the United States, up from 3.13 in 1998.86 The Stronger Child Abuse Prevention and Treatment Act, which cleared the House in March 2022, aims to address underreporting of child abuse, which was at an all-time high during the pandemic.
The Mental Health Parity and Addiction Equity Act faces scrutiny due to a recent American Medical Association report highlighting insurers’ violations regarding mental health treatment.87 Issues include nonquantitative treatment limitations, such as preauthorization requirements. Notable cases include Wit v. United Behavioral Health (UBH, 2019), wherein a federal judge ruled that UBH had discriminatory policies, and Christine S. v. Blue Cross Blue Shield of N.M. (2021), which highlighted the ongoing challenges. According to the National Alliance on Mental Illness, enforcement remains a significant issue, with recent concerns under review by the Senate HELP Committee and the House Ways and Means Committee.
The Family Medical Leave Act allows employees up to 12 weeks of leave for mental health issues, but data on its usage are limited, and issues of stigma and fear of termination persist. There is also an increase in requests for threat assessments due to increasing concerns about gun violence and threats made by students.88 It is important to note that not every circumstance is related to mental illness.89 Clinicians cannot predict violence,90 but they are often asked to provide documentation for students’ return to school. More research and expert guidelines on threat assessments and treatment options are needed.
Misinformation and messaging. Child and adolescent psychiatry is not an expectation when it comes to widespread misinformation about scientific facts. Like other fields, it evolved with robust dialectical processes, debates, and controversies, which led to many systematic changes and advances. However, many issues continue to exist, such as black box warnings for selective serotonin reuptake inhibitors (SSRIs). The US Food and Drug Administration (FDA) inquiries about reports of increased suicidal ideations during many SSRI randomized clinical trials in 1980 and 1990, using a retrofit statistical model, yielded a statistical risk that has been widely debated. Besides strong evidence of its efficacy in National Institute of Mental Health (NIMH) trials (Treatment for Adolescents with Depression Study and Treatment of Resistant Depression in Adolescents), SSRIs have been declined by many who may benefit due to these warnings.91
Likewise, there is compelling evidence for stimulant medication to treat young children with ADHD, and there is misinformation about its reinforcing effects and the risk for substance abuse in adulthood.92 Parents frequently rely on peer forums and their own experiences to decline its use, which takes away an effective treatment for a serious and highly treatable condition. Another common misperception is that suboxone is just another substance rather than an effective treatment for opioid-addicted youth. This underscores poor messaging from organizations and policy-making health care agencies to counter incorrect facts and replace them with jargon-free scientific evidence.
Potential Solutions to Address Modifiable Risk Factors
Access to evidence-based treatment. For most children and adolescents with mental health conditions, psychological interventions are recommended as the first line of treatment. However, access to treatment is limited, and many who receive care do not benefit from evidence based interventions. This is evident from psychiatric readmission rates within a year, ranging from 31% to 38%.93 Training deficits in professionals, mismatches in prioritizing treatments for co-occurring conditions, and diagnostic ambiguity contribute to this issue. Generic therapies cannot replace evidence-based psychological interventions. Treatment failures can also be attributed to factors such as illness chronicity and poor adherence to treatments.
The availability of applied behavior analysis, cognitive-behavioral therapy, family therapy, and dialectical behavior therapy is inconsistent and needs to be scaled up to meet growing demands. Multisystemic therapies integrated with dialectical behavioral therapy, motivational interviewing, and relapse prevention have been effective for troubled youth with a history of delinquency but are not widely available.94
Psychopharmacologic treatments are also common, with pediatricians and family medicine clinicians often being the first to prescribe these agents. Knowledge of evidence-based medicine principles is crucial to avoid serious negative outcomes. For example, paroxetine is not FDA approved for youth, and there is evidence of increased suicidal ideations, leading to a black box warning in 2003. Follow-up is essential when medications with such warnings are prescribed. The use of SSRIs in individuals with autism spectrum disorder (ASD) requires high caution, given the potential harm when patients and families are not adequately educated and monitored. This is particularly important due to the increasing burden of undiagnosed ASD with affective illnesses, which necessitates meticulous assessments and individualized treatments.
During hospitalization, best practices include a shared planning process with the patient, the school liaison, peer support, the outpatient team, and caregivers. Additional actions such as prompt access to neuropsychological testing, integration of systems for pharmacy medication reconciliation, and timely interdisciplinary discharge summaries to communicate with primary care are also crucial.
Follow-up after hospital discharge is imperative. A study of youth aged 10–18 years with Medicaid insurance who experienced psychiatric hospitalization found that attending a follow-up mental health appointment within 1 week of discharge was associated with a reduced risk of suicide.95 A liaison with case managers, access to crisis helplines, and postdischarge contact information should also be included.
Legislation to address the growing burden of untreated and undiagnosed neurodevelopmental disorders among younger children. In 2023, the CDC changed the prevalence of ASD from 1 in 44 to 1 in 36 (children under age 8). The data correlate to the burden of clinical problems and have been applauded by clinicians, families, and advocacy groups. The 2016 US Preventive Services Task Force recommendations against universal screenings were criticized and given the newer data and serious public health concerns may need to be reconsidered.96
Besides ASD, communication and language disorders, learning disorders, and undiagnosed genetic conditions need early recognition and interventions. The epigenetic risk factors are critical in the emerging data about ASD children and adolescents being at significantly higher risk of suicidal thoughts and behaviors. The lifetime prevalence of suicidal ideation in ASD adults ranges between 19.7% and 66%, and suicide attempts between 1.8% and 36%, with the highest prevalence estimates being in late-diagnosed adults.97
Schools-based interventions. During the COVID-19 pandemic, as pediatric visits decreased and social interactions waned, schools remained crucial for children and adolescents, playing a pivotal role in promoting their mental health and identifying those in crisis. School-based interventions are essential for improving access to mental health care, circumventing traditional barriers faced by families. They are the primary source of such services in the United States, particularly vital for identifying at-risk children.
School-based child and adolescent mental health services address disparities in care faced by low-income, minority, LGBTQ+, and immigrant youth who often encounter health care inequities. Adolescents from marginalized backgrounds are more likely to access services exclusively through educational settings compared to other venues.97,98 Thus, integrating child and adolescent mental health services into schools is critical for advancing health equity and ensuring comprehensive support for all children and adolescents.
In addition to mental health services, schools offer interventions to enhance students’ social and emotional well-being, benefiting all students.99 These interventions range from school-wide prevention efforts to individualized therapies such as on-site counseling and psychiatric services. For instance, recommendations for children with ASD include sensory-friendly environments and structured routines to improve their school performance.
These interventions yield benefits such as enhanced academic performance, attendance, engagement, and a more conducive learning environment.21 Schools are also ideal settings for universal mental health screening, crucial for addressing pandemic-related challenges among youth. However, accurate diagnosis by trained professionals is essential to avoid misinterpretation.100
Initiatives like Colorado’s adoption of the Behavior Assessment System for Children, Third Edition (Behavioral and Emotional Screening System) for universal mental health screening in schools highlight the importance of early detection and timely referrals.4 Collaborative efforts between child psychiatrists, therapists, schools, and pediatric providers are essential to expand mental health access and integrated care within school settings. Expanding school-based health clinics with on-site mental health professionals is critical for improving health equity. Key steps include integrating mental health into the school’s mission, garnering stakeholder consensus, and enabling billing through Medicaid and insurance for school-based services.101,102
Before COVID-19, regulatory barriers hindered the launch or expansion of telehealth services in School Based Health Centers.103 Temporary flexibilities during the pandemic, such as reimbursable remote services and cross-state licensing, proved essential, especially in rural areas.77,104 Maintaining these policy adaptations is crucial to address long-term mental health repercussions among youth.
Furthermore, implementing school consultation models where mental health experts educate staff on policies can enhance mental health support within schools. In summary, schools serve as vital hubs for children and adolescents, providing essential mental health services and interventions that promote overall well-being, address disparities, and support academic success, particularly during disruptive events like the COVID-19 pandemic.
Vocational-technical schools and improving skills building for dropouts. In the 1980s, career and technical education was considered an option for underachieving students who would not attend a 4-year college or university. Career and technical education can motivate students to attend school more frequently and be more engaged and therefore improve core academic skills.105 When adult role models are engaged more directly in encouraging and supporting students’ educational and career choices, students are better able to make these choices.105,106
Late school openings and sleep hygiene. According to a CDC study that analyzed US Department of Education data from the 2011–2012 school year, 42 states reported that most (75%–100%) public middle and high schools started before 8:30 AM. The American Academy of Sleep Medicine recommends that adolescents should regularly sleep 8–10 hours per day. The American Academy of Pediatrics has recommended that middle and high schools start at 8:30 AM or later to allow students to get the amount of sleep they need.107 Adolescents who are sleep deprived are more likely to be overweight; not engage in daily physical activity; suffer from symptoms of depression108; engage in unhealthy risk behaviors such as drinking, smoking tobacco, and using illicit drugs; and experience declines in school performance, which could lead to discipline referrals.109 There has also been a link between poor sleep and a 2-fold increase in suicidal ideation and attempts.110
During puberty, adolescents have shifts in biological circadian rhythms often combined with poor sleep habits (including irregular bedtimes and the presence of electronics in the bedroom). The combination of late bedtimes and early school start results in most adolescents not getting enough sleep.111
Later school start times support the evidence to meet the biological needs of adolescents.112 Other benefits of later start times include improved attendance at school, decreased tardiness, better student grades, fewer occurrences of falling asleep in class, reduced irritability and depressive symptoms, and fewer disciplinary issues. One study also reported a 16.5% decrease in the adolescent motor vehicle accident rate after the school start time was pushed back 1 hour.113,114
Limiting the use of social media. There are reports that younger children between the ages of 8 and 12 spend approximately 4–6 hours per day on-screen while adolescents spend an average of 7–9 hours per day. During the pandemic, screen time has exceeded these limits. Excessive media use in children has been associated with a myriad range of undesirable health outcomes, such as reduced sleep, increased obesity, and language and social emotional delays.113 Social media has been associated with activations in reward-related brain regions and is weakly correlated with negative indicators of psychological well being.115 It is established in the empirical literature that in younger children, higher-order cognitive skills (including attentional and emotional control) are associated with parent-child interactions and unstructured social play.
Nutrition and exercise. Emerging evidence suggests that alterations in the development of the gastrointestinal (GI) tract during the postnatal period have implications for brain development. It is increasingly recognized that the GI tract and brain communication is mainly driven by neural, endocrine, immune, and metabolic mediators, collectively called the gut-brain axis.116,117 There is increasing evidence that the colonization of the GI tract by the microbiota appears to have a parallel developmental trajectory to the brain for up to 3 years of age.
Early puberty is relatively uncommon, affecting nearly 1 in every 5,000–10,000 children, with a female to-male ratio of approximately 10:1. In the last decade, there has been a substantial surge in the incidence of early puberty, with children as young as 5 years developing breasts and those younger than 8 years starting menstruation in some reported cases.118 The condition is associated with affective illness, eating disorders, substance abuse, and antisocial behavior.
The American Heart Association recommends a daily limit of 6 teaspoons of sugar for women and 9 teaspoons for men. To put that into context, a can of Coca-Cola contains 8.25 teaspoons of sugar, while a small banana contains 3 teaspoons. A study provides evidence that sugar intake from sweet food/beverages increases the chance of mood disorders.119 With a link between the high prevalence of mood disorders and sugar intake, the policies promoting the reduction of sugar consumption could additionally support primary and secondary prevention of mental illness.
DISCUSSION
There is an age-old saying that emphasizes the collective effort required to raise a child, and when it comes to addressing serious issues such as mental health and emotional struggles affecting 40% of youth, the need for a coordinated approach is urgent.90 Such an approach involves not only the collaboration of various scientific disciplines but also legislative initiatives, media campaigns, and educational efforts to combat the spread of misinformation.
In today’s complex landscape, factors such as social networking sites, fear of missing out, and perfectionism can hinder both physical and mental development.120 Understanding their long-term consequences remains challenging due to numerous variables.
Addressing workforce shortages through coordinated care has been an evidence-based approach. This not only maintains clinical standards but also promotes ongoing research into childhood and adolescent mental disorders, establishing effective treatments. However, expanding access with minimally trained workers raises concerns about oversimplification and its impact on clinical outcomes, requiring careful evaluation.
Given prevalent workforce burnout and clinical complexities, integrating modules on physical and mental well-being for health care teams is crucial. Advocacy organizations are pushing for swift reforms, influenced by recent DEA policy shifts on opioids, US Preventative Services Task Force anxiety disorder screening recommendations, and Surgeon General advisories on social media, involving diverse stakeholders. Learning from successful strategies in other countries and health care systems, grounded in neurodevelopmental science, also offers promising pathways for improvement.
Strong metrics and data underscore the ongoing child and youth mental health crisis exacerbated by the pandemic. While recent trends show some improvement post-pandemic, the overall burden remains significant, leading to increased health care costs and strained existing systems. Globally, there are varying population based trends and disparities between regions, such as Utah’s higher suicide rates compared to the rest of the United States.121–123
Numerous factors contribute to this complex issue, including workforce challenges, inadequate training, civil unrest, structural racism, and systemic issues.19,124,125 Environmental factors such as social media, artificial intelligence, bullying, and the opioid crisis also play pivotal roles. Today’s teens, or Zoomers, face multiple adversities without proportional increases in resilience factors due to deteriorating familial coherence and social support.
These challenges have led to rising rates of depression, anxiety, self-harm, suicidal ideation, and substance abuse among teens, particularly impacting females, minoritized youth, and gender nonconforming individuals. Parental psychopathology exacerbates these trends across generations.
Research suggests various pathways linking social media, sleep disruption, and psychopathology, highlighting cyberbullying and the quest for external validation as significant risks, especially among vulnerable teens. The pervasive influence of big technology and artificial intelligence further complicates these issues, commodifying teenage behavior with little regard for psychological consequences. In summary, the prevalence of core psychiatric conditions has increased, particularly among at-risk youth, underscoring the urgent need for comprehensive interventions and systemic reforms to support youth mental health.
All these trends predated the pandemic. When the COVID-19 pandemic struck in March 2020, these shifting epidemiologic trends were already manifest. With the imposition of requisite public health mitigation strategies, the further encroachment of risk for teens and families could not be forestalled. Families experienced enormous additive stresses due to seclusion within households, social isolation, increased rates of domestic violence, increased rates of adult substance use, universal concerns about the health of family and friends, disruptions to school and childcare, the need to make new health-related decisions in a context of evolving uncertainty, and financial pressures relating to job insecurity. The result has been catastrophic. For teens and families with preexisting conditions, those with parents who were front-line workers, and those with fewer resources, the rates of persistent psychological distress, adolescent depression and anxiety, adolescent self-harm, and suicidal ideation all doubled. The only metric of teenage mental health that improved was substance abuse—it dropped through the pandemic due to lack of access; however, overdose rates in teens increased during the pandemic. But even that finding has been formulated as a risk: prominent researchers have predicted an epidemic of forthcoming substance use relating to exposure to parental substance abuse in the context of greater family dysfunction relating to social isolation.126–128
Importantly, parental psychopathology has also increased. The old expression “What’s good for the goose is good for the gander” remains vibrantly meaningful in this context. Perhaps unsurprisingly for those of us who navigated the turbulence of the pandemic, rates of adult psychopathology have increased precipitously: 25% of adults reported deteriorations in mental health with a preponderance of anxiety, depression, suicidal ideation, posttraumatic stress disorder, and substance abuse.129 When teen and parent psychopathology rates coincided, the outcomes have been yet worse, with lingering problems in family function. Because the family system is a relevant variable in the study of gene × environment interactions for teens, deteriorating parental mental health is a crucial aspect of this persistent problem. In the circumplex model of family function, stable families manifest a blend of coherence and flexibility that affords the kind of reciprocal, developmentally sensitive communication and interactions required to accommodate adolescent development. Unsurprisingly, the escalating rates of adult psychopathology relating both to the prepandemic demands of parenting vulnerable teens and the unexpected and severe pandemic-related stressors have debilitated family function, pulling metrics of familial coherence and flexibility to all-time lows.
In the absence of resilience factors, it is no surprise that these trends are persisting. As mentioned previously, parenting behavior is a relevant variable for teens. An important parenting finding revealed that the specific task of coparenting—aligning as parents to address emergent problems among the children—was hit hard.130–132 This means the capacity for parents to identify emergent problems among their teens, agree on a response, and implement developmentally sensitive parenting strategies, including seeking and finding professional help for teens, deteriorated. Classically maladroit parenting—the low demanding/low responsive profile—increased, while salutary parenting practices featuring an authoritative approach predicated on greater responsiveness and empathy decreased.
One common risk factor among teens and parents that emerged throughout the pandemic and before is loneliness. Loneliness is a common, universal human experience involving feelings and cognitions that reflect emotionally from perceived deficiencies in social relationships. Loneliness is associated with physical health problems, depression, anxiety, low self-esteem, peer rejection, victimization, aggression and social withdrawal, and problems with attention. Among teens, loneliness increased, paradoxically, with the prepandemic infusion of technological advancements in communication relating to the advent of the smartphone and social media. Among parents, the social isolation pertinent to the pandemic and related disruptions to work and socialization patterning increased. Again, the combination of adolescent and parental problems—in this case, the common denominator of loneliness—predicted greater rates of psychopathology, family dysfunction, and adversity.
One universally accepted resilience factor that has emerged from the pandemic thus far is the universal adoption of tele-mental health. For certain teens and parents, this modality for seeking treatment has improved access to care by lowering the bar for entry.
Catastrophically, the proliferation of risk and decrements in resilience have manifested in biological, morphometric changes in adolescent brain development. A Stanford longitudinal neuroimaging study of MRI data from adolescents aged 10 and older provided refined insights into brain maturation and senescence. While most brain regions exhibited similar trajectories to adult-only data, 7 regions, including the postcentral, temporal, calcarine, and occipital cortices, as well as the thalamus, putamen, and corpus callosum, demonstrated improved model fits with the adolescent data. The findings indicated continued white matter growth in the centrum semiovale and accelerated cortical volume reduction in regions such as the frontal and temporal cortices during adolescence and early adulthood. This white matter expansion, associated with increasing neural connectivity, occurred alongside cortical pruning, reducing neurons with insufficient connectivity. The developmental trajectory suggests white matter continues to expand into early adulthood, with cortical decline becoming more pronounced around age 30 and accelerating near age 60.133 It appears that the pandemic not only adversely affected the mental health of adolescents but also accelerated their brain maturation in a manner consistent with pervasive trauma.
Prior to the pandemic, indeed, before the Zoomer generation, adolescent psychopathology was recognized to be common, persistent, costly, and deadly. With greater risk and diminutions in resilience, adolescent psychopathology is increasing in prevalence, severity, morbidity, and mortality.
Before the pandemic, adolescent mental health care delivery faced systemic challenges: limited screening for psychopathology, underfunded outpatient services, shortened inpatient stays, and inadequate insurance coverage for higher levels of care. Treatment options were fragmented between medication management and poorly coordinated psychosocial interventions, exacerbated by workforce shortages in mental health professions. These systemic deficiencies contributed to increased risk factors exacerbated by social media, leading to widespread psychiatric conditions among teens and families during the pandemic. Addressing these issues requires a focused effort to understand and mitigate the specific links between risk factors, family dynamics, and adolescent psychopathology.
Effective strategies must include robust investments in prevention, clinical care, research, and advocacy. This entails enhancing systems integration across family, educational, medical, and judicial contexts; expanding the mental health workforce; and prioritizing human connection in interventions. Without these measures, the prospect of a dystopian future marked by widespread family dysfunction, loneliness, and mental health crises looms large.
CONCLUSION AND FUTURE DIRECTIONS
The complexities of psychiatric phenomenology, the diversity of conditions, comorbidities, interacting variables, and the concept of resilience continue to challenge and inspire further empirical and scientific research. Genetics, polygenic inheritance, and epigenetic phenomena, which were traditionally poorly understood, have seen significant advancements through genome-wide association studies. As the field of child and adolescent psychiatry progresses with cutting-edge science, it remains crucial to integrate human subjectivity, psychosocial aspects, and multimodal interventions. Collaborations between communities and clinicians working with vulnerable populations to design studies that align with NIMH grants can lead to meaningful changes. These changes can subsequently inform the development of policies grounded in research, ultimately addressing the complex mental health challenges faced by children and youth.
Article Information
Published Online: October 24, 2024. https://doi.org/10.4088/PCC.24nr03747
© 2024 Physicians Postgraduate Press, Inc.
Submitted: March 24, 2024; accepted July 30, 2024.
To Cite: Gupta M, Ladegard K, Gupta N, et al. Antecedents and trajectories of the child and adolescent mental health crisis: assimilating empirically guided pathways for stakeholders. Prim Care Companion CNS Disord. 2024;26(5):24nr03747.
Author Affiliations: Southwood Children’s Behavioral Healthcare, Pittsburgh, Pennsylvania (M. Gupta); Department of Behavioral Health Services, Denver Health Medical Center, Denver, Colorado (Ladegard); Department of Psychiatry, Dayton’s Children Hospital, Dayton, Ohio (N. Gupta); Department of Psychology, Christ University, Delhi, India (Khurana); Yale School of Medicine, New Haven, Connecticut (Krasner).
Corresponding Author: Mayank Gupta, MD, Southwood Children’s Behavioral Healthcare, 2575 Boyce Plaza Rd, Pittsburgh, PA 15241 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
ORCID: Mayank Gupta: https://orcid.org/0000-0002-0521-1419
Clinical Points
- Approximately 1 in 5 children (aged 3–17 years) in the United States have a mental, emotional, developmental, or behavioral disorder.
- Public health mitigation strategies include improved access to evidence-based treatments, implementation of legislative measures for early identification and treatment of developmental disorders, and enhanced suicide prevention efforts.
- School-based interventions and vocational-technical education are crucial, as are initiatives targeting sleep hygiene, social media usage, nutrition, and physical activity.
References (133)

- Wilson S, Dumornay NM. Rising rates of adolescent depression in the United States: challenges and opportunities in the 2020s. J Adolesc Health. 2022;70(3):354–355. PubMed CrossRef
- Dreyer BP. Stepping up to the plate-the role of pediatricians in addressing the child and adolescent mental health crisis. JAMA Netw Open. 2023;6(1):e2249578. PubMed CrossRef
- The Biden-Harris Administration Invests $55 Million in Expanding Access to Youth Mental Health Care. Health Resources and Services Administration. Accessed February 21, 2024. https://www.hrsa.gov/about/news/pressreleases/fy-2023-youth-mental-health-care
- Data and Statistics on Children’s Mental Health. CDC. Accessed January 8, 2024. https://www.cdc.gov/childrensmentalhealth/data.html
- State suicide rates among adolescents and young adults aged 10–24: United States, 2000–2018. Accessed January 9, 2024. https://stacks.cdc.gov/view/cdc/93667
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. PubMed CrossRef
- Jones SE, Ethier KA, Hertz M, et al. Mental health, suicidality, and connectedness among high school students during the COVID-19 pandemic—adolescent behaviors and experiences Survey, United States, January–June 2021. MMWR Suppl. 2022;71(suppl 3):16–21. PubMed CrossRef
- Bitsko RH, Claussen AH, Lichstein J, et al. Mental health surveillance among children – United States, 2013–2019. MMWR Suppl. 2022;71(2):1–42.
- Liu J, Yang L, Zheng Y, et al. Rural-urban differences in prevalence and correlates of suicidal ideation in adolescent patients with depression in a large sample of Chinese. J Affect Disord. 2023;322:118–124. PubMed CrossRef
- Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health-related emergency department visits among children aged <18 Years during the COVID-19 pandemic – United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675–1680. PubMed CrossRef
- Radhakrishnan L, Leeb RT, Bitsko RH, et al. Pediatric emergency department visits associated with mental health conditions before and during the COVID-19 pandemic – United States, January 2019–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(8):319–324. PubMed CrossRef
- Krause KH, Verlenden JV, Szucs LE, et al. Disruptions to school and home life among high school students during the COVID-19 pandemic – adolescent behaviors and experiences Survey, United States, January–June 2021. MMWR Suppl. 2022;71(3):28–34. PubMed
- Martin MS, Dykxhoorn J, Afifi TO, et al. Child abuse and the prevalence of suicide attempts among those reporting suicide ideation. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1477–1484. PubMed CrossRef
- Over one-third of Americans live in areas lacking mental health professionals. USAFacts. Accessed January 9, 2024. https://usafacts.org/articles/over-one-third-of-americans-live-in-areas-lacking-mentalhealth-professionals/
- Golberstein E, Kolvenbach S, Carruthers H, et al. Effects of electronic psychiatric consultations on primary care provider perceptions of mental health care: survey results from a randomized evaluation. Healthc. 2018;6(1):17–22. PubMed CrossRef
- Fegert JM, Vitiello B, Plener PL. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;20:14. PubMed CrossRef
- 2021 National Survey on drug use and health (NSDUH) releases. Accessed September 9, 2024. https://www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases#annualnational-report
- Gupta M. Mental health effects of the COVID-19 pandemic on children and young adults: empirical analysis of the past, present and the way forward. BJPsych Open. 2023;10(1):e7. PubMed CrossRef
- Alvarez K, Cervantes PE, Nelson KL, et al. Review: structural racism, Children’s mental health service systems, and recommendations for policy and practice change. J Am Acad Child Adolesc Psychiatry. 2022;61(9):1087–1105. PubMed CrossRef
- National Substance Use and Mental Health Services Survey (N-SUMHSS): 2022 Data on Substance Use and Mental Health Treatment Facilities | CBHSQ Data. Accessed January 9, 2024. https://www.samhsa.gov/data/report/2022-nsumhss-annual-report
- Trent M, Dooley DG, Dougé J, et al. The impact of racism on child and adolescent health. Pediatrics. 2019;144(2):e20191765. PubMed CrossRef
- Mpofu JJ, Cooper AC, Ashley C, et al. Perceived racism and demographic, mental health, and behavioral characteristics among high school students during the COVID-19 pandemic — adolescent behaviors and experiences survey, United States, January–June 2021. MMWR Suppl. 2022;71(suppl 3):22–27. PubMed
- Patel I, Walter LA, Li L. Opioid overdose crises during the COVID-19 pandemic: implication of health disparities. Harm Reduct J. 2021;18(1):89. PubMed
- Kuehn BM. Fentanyl drives startling increases in adolescent overdose deaths. JAMA. 2023;329(4):280–281.
- Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98(11):1493–1504. PubMed CrossRef
- Hanna RC, Perez JM, Ghose S. Cannabis and development of dual diagnoses: a literature review. Am J Drug Alcohol Abuse. 2017;43(4):442–455. PubMed CrossRef
- Kim HS, Hall KE, Genco EK, et al. Marijuana tourism and emergency department visits in Colorado. N Engl J Med. 2016;374(8):797–798. PubMed CrossRef
- Ksir C, Hart CL. Cannabis and psychosis: a critical overview of the relationship. Curr Psychiatry Rep. 2016;18(2):12. PubMed
- Lynskey MT, Glowinski AL, Todorov AA, et al. Major depressive disorder, suicidal ideation, and suicide attempt inTwins discordant for cannabis dependence and early-onset cannabis use. Arch Gen Psychiatry. 2004;61(10):1026–1032. PubMed CrossRef
- Nussbaum A, Thurstone C, Binswanger I. Medical marijuana use and suicide attempt in a patient with major depressive disorder. Am J Psychiatry. 2011;168(8):778–781. PubMed CrossRef
- Pedersen W. Does cannabis use lead to depression and suicidal behaviours? A population-based longitudinal study. Acta Psychiatr Scand. 2008;118(5):395–403. PubMed CrossRef
- Price C, Hemmingsson T, Lewis G, et al. Cannabis and suicide: longitudinal study. Br J Psychiatry. 2009;195(6):492–497. PubMed CrossRef
- Rasic D, Weerasinghe S, Asbridge M, et al. Longitudinal associations of cannabis and illicit drug use with depression, suicidal ideation and suicidal attempts among Nova Scotia high school students. Drug Alcohol Depend. 2013;129(1–2):49–53. PubMed CrossRef
- Schimmelmann BG, Conus P, Cotton S, et al. Prevalence and impact of cannabis use disorders in adolescents with early onset first episode psychosis. Eur Psychiatry. 2012;27(6):463–469. PubMed CrossRef
- Sharma P, Murthy P, Bharath MMS. Chemistry, metabolism, and toxicology of cannabis: clinical implications. Iran J Psychiatry. 2012;7(4):149–156. PubMed
- Silins E, Swift W, Slade T, et al. A prospective study of the substance use and mental health outcomes of young adult former and current cannabis users. Drug Alcohol Rev. 2017;36(5):618–625. PubMed CrossRef
- Tanz LJ, Dinwiddie AT, Mattson CL, et al. Drug overdose deaths among persons aged 10–19 Years – United States, July 2019–December 2021. MMWR Morb Mortal Wkly Rep. 2022;71:1576–1582. PubMed CrossRef
- Hall W, Lynskey M. Assessing the public health impacts of legalizing recreational cannabis use: the US experience. World Psychiatry. 2020;19(2):179–186. PubMed CrossRef
- van Ours JC, Williams J, Fergusson D, et al. Cannabis use and suicidal ideation. J Health Econ. 2013;32(3):524–537. PubMed CrossRef
- Chandra S, Radwan MM, Majumdar CG, et al. New trends in cannabis potency in USA and Europe during the last decade (2008–2017). Eur Arch Psychiatry Clin Neurosci. 2019;269(1):5–15. PubMed CrossRef
- Smart R, Caulkins JP, Kilmer B, et al. Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. Addiction. 2017;112(12):2167–2177. PubMed CrossRef
- Bell C, Slim J, Flaten HK, et al. Butane hash oil burns associated with marijuana liberalization in Colorado. J Med Toxicol. 2015;11(4):422–425. PubMed CrossRef
- Keller CJ, Chen EC, Brodsky K, et al. A case of butane hash oil (marijuana wax)–induced psychosis. Subst Abus. 2016;37(3):384–386. PubMed CrossRef
- Rickner SS, Cao D, Kleinschmidt K, et al. A little “dab” will do ya’ in: a case report of neuro-and cardiotoxicity following use of cannabis concentrates. Clin Toxicol. 2017;55(9):1011–1013.
- Major Uptick Reported in Cannabis Vaping for All Adolescents. Columbia University Mailman School of Public Health. 2022. Accessed October 8, 2023. https://www.publichealth.columbia.edu/news/major-uptick-reported-cannabisvaping-all-adolescents
- Arseneault L, Cannon M, Poulton R, et al. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ. 2002;325(7374):1212–1213. PubMed CrossRef
- Levine A, Clemenza K, Rynn M, et al. Evidence for the risks and consequences of adolescent cannabis exposure. J Am Acad Child Adolesc Psychiatry. 2017;56(3):214–225. PubMed CrossRef
- Heron T, Gibson R, Abel W. Gender and suicidal behaviour among adolescents who use alcohol. Int J Public Health. 2017;9(1):51.
- Borges G, Bagge CL, Orozco R. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 2016;195:63–74. PubMed CrossRef
- Doucette ML, Borrup KT, Lapidus G, et al. Effect of Washington State and Colorado’s cannabis legalization on death by suicides. Prev Med. 2021;148:106548. PubMed CrossRef
- Gobbi G, Atkin T, Zytynski T, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–434. PubMed
- Coffey C, Patton GC. Cannabis use in adolescence and young adulthood: a review of findings from the victorian adolescent health cohort study. Can J Psychiatry. 2016;61(6):318–327. PubMed CrossRef
- Fergusson DM, Boden JM, Horwood LJ. Psychosocial sequelae of cannabis use and implications for policy: findings from the Christchurch Health and Development Study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1317–1326. PubMed CrossRef
- Nocon A, Wittchen HU, Pfister H, et al. Dependence symptoms in young cannabis users? A prospective epidemiological study. J Psychiatr Res. 2006;40(5):394–403. PubMed CrossRef
- Silins E, Horwood LJ, Patton GC, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1(4):286–293. PubMed CrossRef
- Mashhoon Y, Sagar KA, Gruber SA. Cannabis use and consequences. Pediatr Clin North Am. 2019;66(6):1075–1086. PubMed CrossRef
- Lisdahl KM, Gilbart ER, Wright NE, et al. Dare to delay? The impacts of adolescent alcohol and marijuana use onset on cognition, brain structure, and function. Front Psychiatry. 2013;4:53. PubMed CrossRef
- Home. Smart approaches to marijuana. Accessed October 8, 2023. https://learnaboutsam.org/
- Healthy kids Colorado Survey data tables and reports | department of public health & environment. Accessed October 8, 2023. https://cdphe.colorado.gov/healthy-kids-colorado-survey-data-tables-and-reports?utm_medium=email&utm_source=transaction
- Evans-Whipp TJ, Plenty SM, Catalano RF, et al. Longitudinal effects of school drug policies on student marijuana use in Washington state and victoria, Australia. Am J Public Health. 2015;105(5):994–1000. PubMed CrossRef
- Gupta M, Chedrawy E. An ontological, anthropological, and psychoanalytic perspective on physician burnout. Cureus. 2023;15(1):e34282. PubMed CrossRef
- Barthorpe A, Winstone L, Mars B, et al. Is social media screen time really associated with poor adolescent mental health? A time use diary study. J Affect Disord. 2020;274:864–870. PubMed CrossRef
- Nunes AF, Monteiro PML, Ferreira FBP, et al. Convergence insufficiency and accommodative insufficiency in children. BMC Ophthalmol. 2019;19(1):58. PubMed CrossRef
- Twenge JM. Increases in depression, self-harm, and suicide among U.S. Adolescents after 2012 and links to technology use: possible mechanisms. Psychiatr Res Clin Pract. 2020;2(1):19–25. PubMed
- Valkenburg PM. Social media use and well-being: what we know and what we need to know. Curr Opin Psychol. 2022;45:101294. PubMed CrossRef
- Maes C, Vandenbosch L. Physically distant, virtually close: adolescents’ sexting behaviors during a strict lockdown period of the COVID-19 pandemic. Comput Human Behav. 2022;126:107033. PubMed CrossRef
- Doyle C, Douglas E, O’Reilly G. The outcomes of sexting for children and adolescents: a systematic review of the literature. J Adolesc. 2021;92(1):86–113. PubMed
- U.S. Children Living in a Single Parent Family 1970-2023. Statista. Accessed January 9, 2024. https://www.statista.com/statistics/252847/number-of-childrenliving-with-a-single-mother-or-single-father/
- Hogg AS. IF health is wealth, America’s working mothers are living in extreme poverty.
- Mathews TJ, Hamilton BE. Mean Age of Mothers Is on the Rise: United States, 2000–2014. NCHS Data Brief, No 232. National Center for Health Statistics; 2019. Accessed January 9, 2024. https://www.cdc.gov/nchs/products/databriefs/db232.htm
- Understanding chronic absenteeism. 2023. Accessed March 6, 2024. https://www.aft.org/ae/winter2019-2020/marsh
- Pew Research Center. Trends in Income and Wealth Inequality. Pew Research Center’s Social & Demographic Trends Project; 2020. Accessed January 9, 2024. https://www.pewresearch.org/social-trends/2020/01/09/trends-in-incomeand-wealth-inequality/
- Chronic absenteeism in the nation’s schools. Accessed January 9, 2024. https://www2.ed.gov/datastory/chronicabsenteeism.html
- Beginning - Elementary and Secondary Education Act (ESEA). Office of elementary and secondary education. Accessed January 9, 2024. https://oese.ed.gov/beginning-elementary-and-secondary-education-act-esea/
- Why Federal Spending on Disadvantaged Students (Title I) Doesn’t Work. Brookings. Accessed January 9, 2024. https://www.brookings.edu/articles/why-federal-spending-on-disadvantaged-students-title-idoesnt-work/
- Hess AJ. College costs have increased by 169% since 1980—but pay for young workers is up by just 19%: georgetown report. CNBC. 2021. Accessed January 9, 2024. https://www.cnbc.com/2021/11/02/the-gap-in-college-costs-andearnings-for-young-workers-since-1980.html
- Legal rights. Accessed October 8, 2023. https://projectpencil.com/legal-rights/?utm_medium=email&utm_source=transaction
- WV code § 18-20-1. Accessed October 8, 2023. https://www.wvlegislature.gov/wvcode/ChapterEntire.cfm?art=20&chap=18§ion=1&utm_medium=email&utm_source=transaction
- Black EW, Ferdig RE, Fleetwood A, et al. Hospital homebound students and K-12 online schooling. PLoS One. 2022;17(3):e0264841. PubMed CrossRef
- Searle NS, Askins M, Bleyer WA. Homebound schooling is the least favorable option for continued education of adolescent cancer patients: a preliminary report. Med Pediatr Oncol. 2003;40(6):380–384. PubMed CrossRef
- Williams NJ, Scott L, Aarons GA. Prevalence of serious emotional disturbance among U.S. Children: a meta-analysis. Psychiatr Serv. 2018;69(1):32–40. PubMed
- Family first prevention services Act (FFPSA) – advancing the Children’s bureau’s vision – child welfare capacity building collaborative. Accessed January 1, 2024. https://capacity.childwelfare.gov/about/cb-priorities/family-first-prevention
- No child Left behind: an overview. Accessed January 9, 2024. https://www.edweek.org/policy-politics/no-child-left-behind-an-overview/2015/04
- Gupta M, Gupta N, D’souza V. Do antibullying laws in the United States have an impact? CNS Spectr. 2023;28(1):1–3. PubMed
- The child abuse prevention center – preventing child abuse. Accessed January 9, 2024. https://www.thecapcenter.org/help/prevent-or-report-abuse/preventing-child-abuse
- National Child Abuse Statistics from NCA. National Children’s alliance. Accessed January 9, 2024. https://www.nationalchildrensalliance.org/media-room/national-statistics-on-child-abuse/
- Insurer Accountability on Mental Health Parity is Long Overdue. American Medical Association; 2022. Accessed January 9, 2024. https://www.ama-assn.org/delivering-care/patient-support-advocacy/insurer-accountability-mentalhealth-parity-long-overdue
- School shootings over time: incidents, injuries, and deaths. Accessed January 9, 2024. https://www.edweek.org/leadership/school-shootings-over-timeincidents-injuries-and-deaths
- Gold LH. Gun violence: psychiatry, risk assessment, and social policy. J Am Acad Psychiatry Law. 2013;41(3):337–343. PubMed
- Gupta M, Gupta N, Robinson M. A panorama of the medicolegal aspects of suicide assessments: integrating multiple vantage points in improving quality, safety, and risk management. CNS Spectr. 2023;28(3):282–287. PubMed CrossRef
- Brent DA. The treatment of ssri-resistant depression in adolescents (TORDIA): in search of the best next step. Depress Anxiety. 2009;26(10):871–874. PubMed CrossRef
- Humphreys KL, Eng T, Lee SS. Stimulant medication and substance use outcomes: a meta-analysis. JAMA Psychiatry. 2013;70(7):740–749. PubMed CrossRef
- Han X, Jiang F, Tang Y, et al. Factors associated with 30-day and 1-year readmission among psychiatric inpatients in Beijing China: a retrospective, medical record-based analysis. BMC Psychiatry. 2020;20(1):113. PubMed CrossRef
- Rowland MD, Halliday-Boykins CA, Henggeler SW, et al. A randomized trial of multisystemic therapy with Hawaii’s felix class youths. J Emot Behav Disord:13(1):13–23.
- Brent DA, Goldstein TR, Benton TD. Bridging gaps in follow-up appointments after hospitalization and youth suicide: mental health care disparities matter. JAMA Netw Open. 2020;3(8):e2013100. PubMed CrossRef
- Gupta N, Gupta M. Diagnostic overshadowing in high-functioning autism: mirtazapine, buspirone, and modified cognitive behavioral therapy (CBT) as treatment options. Cureus. 2023;15(5):e39446. PubMed CrossRef
- Dow D, Morgan L, Hooker JL, et al. Anxiety, depression, and the interpersonal theory of suicide in a community sample of adults with autism spectrum disorder. Arch Suicide Res. 2021;25(2):297–314. PubMed CrossRef
- Ali MM, West K, Teich JL, et al. Utilization of mental health services in educational setting by adolescents in the United States. J Sch Health. 2019;89(5):393–401. PubMed CrossRef
- Curtin SC. National vital statistics reports volume 69, number 11 September 11, 2020 state suicide rates among adolescents and young adults aged 10–24: United States, 2000–2018.
- Connors EH, Moffa K, Carter T, et al. Advancing mental health screening in schools: innovative, field-tested practices and observed trends during a 15-month learning collaborative. Psychol Sch. 2022;59(6):1135–1157. PubMed CrossRef
- Elias MJ. Academic and social-emotional learning. In: Educational Practices Series. International Bureau of Education. Publications Unit; 2003. Accessed October 10, 2023. https://eric.ed.gov/?id=ED473695
- Want to improve school mental health interventions? Ask young people what they actually think - Foulkes - 2022 - Journal of Philosophy of Education - Wiley Online Library. Accessed October 10, 2023. https://onlinelibrary.wiley.com/doi/full/10.1111/1467-9752.12649
- Sullivan E, Goddard A, Fields P, et al. Health technology in school-based health centers: supporting continuous care during COVID-19. Health Technol. 2021;5(0). doi: 10.21037/ht-20-30 CrossRef
- Affairs (ASPA) AS for P. HHS fact sheet: telehealth flexibilities and resources and the COVID-19 public health emergency. Health and Human Services. 10/hhs-fact sheet-telehealth-flexibilities-resources-covid-19-public-health-emergency. html.
- State laws. Accessed October 8, 2023. https://projectpencil.com/legal-rights/state-laws/?utm_medium=email&utm_source=transaction
- Gottfried MA, Bozick R, Rose E, et al. Does career and technical education strengthen the STEM pipeline? Comparing students with and without disabilities. J Disabil Pol Stud. 2016;26(4):232–244.
- Wagner MM, Newman LA, Javitz HS. The benefits of high school career and technical education (CTE) for youth with learning disabilities. J Learn Disabil. 2016;49(6):658–670. PubMed CrossRef
- School start times for adolescents - PubMed. Accessed October 10, 2023. https://pubmed.ncbi.nlm.nih.gov/25156998/
- Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85. PubMed CrossRef
- Owens JA, Dearth-Wesley T, Lewin D, et al. Self-regulation and sleep duration, sleepiness, and chronotype in adolescents. Pediatrics. 2016;138(6):e20161406. PubMed CrossRef
- Baiden P, Tadeo SK, Tonui BC, et al. Association between insufficient sleep and suicidal ideation among adolescents. Psychiatry Res. 2020;287:112579. PubMed CrossRef
- Dunster GP, de la Iglesia L, Ben-Hamo M, et al. Sleepmore in Seattle: Later school start times are associated with more sleep and better performance in high school students. Sci Adv. 2018;4(12):eaau6200. PubMed CrossRef
- Bin-Hasan S, Kapur K, Rakesh K, et al. School start time change and motor vehicle crashes in adolescent drivers. J Clin Sleep Med. 2020;16(3):371–376. PubMed CrossRef
- Wahlstrom KL, Plog AE, McNally J, et al. Impact of changing school start times on teacher sleep health and daytime functioning. J Sch Health. 2023; 93(2):128–134. PubMed
- Villani S. Impact of media on children and adolescents: a 10-year review of the research. J Am Acad Child Adolesc Psychiatry. 2001;40(4):392–401. PubMed CrossRef
- Herman DR, Rhoades N, Mercado J, et al. Dietary habits of 2- to 9-year-old American children are associated with gut microbiome composition. J Acad Nutr Diet. 2020;120(4):517–534. PubMed CrossRef
- Hur JL, Gupta M. Growing up in the Web of social networking: adolescent development and social media. Adolesc Psychiatry:3(3):233–244.
- Kraaij R, Schuurmans IK, Radjabzadeh D, et al. The gut microbiome and child mental health: a population-based study. Brain Behav Immun. 2023;108:188–196. PubMed CrossRef
- Tenedero CB, Oei K, Palmert MR. An approach to the evaluation and management of the obese child with early puberty. J Endocr Soc. 2022;6(1):bvab173. PubMed CrossRef
- Freije SL, Senter CC, Avery AD, et al. Association between consumption of sugar sweetened beverages and 100% fruit juice with poor mental health among US adults in 11 US states and the District of Columbia. Prev Chronic Dis. 2021;18:E51. PubMed CrossRef
- Annor FB, Zwald ML, Wilkinson A, et al. characteristics of and precipitating circumstances surrounding suicide among persons aged 10–17 Years - Utah, 2011–2015. Morb Mortal Wkly Rep. 2018;67(11):329–332.
- Marcotte DE, Hansen B. The re-emerging suicide crisis in the U.S.: patterns, causes and solutions. J Pol Anal Manage. 2024;43(2):582–612.
- McGraw JS, Peer SO, McManimen S, et al. Comparison of lifetime suicide attempts and recent suicidal/self-harming thoughts among sexual minority and heterosexual utahns: results from a population-based Survey. Arch Suicide Res. 2022;26(2):961–967. PubMed CrossRef
- Clark EC, Cranston E, Polin T, et al. Structural interventions that affect racial inequities and their impact on population health outcomes: a systematic review. BMC Public Health. 2022;22(1):2162. PubMed CrossRef
- Gupta M, Sharma A. Fear of missing out: a brief overview of origin, theoretical underpinnings and relationship with mental health. World J Clin Cases. 2021;9(19):4881–4889. PubMed CrossRef
- Amaro H, Sanchez M, Bautista T, et al. Social vulnerabilities for substance use: stressors, socially toxic environments, and discrimination and racism. Neuropharmacology. 2021;188:108518. PubMed CrossRef
- Johnson D, Browne DT, Prime H, et al. Parental mental health trajectories over the COVID-19 pandemic and links with childhood adversity and pandemic stress. Child Abuse Negl. 2023;2023:106554. PubMed CrossRef
- Parolin M, Simonelli A, Mapelli D, et al. Parental substance abuse as an early traumatic event. Preliminary findings on neuropsychological and personality functioning in young drug addicts exposed to drugs early. Front Psychol. 2016;7:887. PubMed CrossRef
- McLaughlin KA, Rosen ML, Kasparek SW, et al. Stress-related psychopathology during the COVID-19 pandemic. Behav Res Ther. 2022;154:104121. PubMed CrossRef
- Basu D, Nagpal S, Mutiso V, et al. Enhancing resilience and mental health of children and adolescents by integrated school- and family-based approaches, with a special focus on developing countries: a narrative review and call for action. World Soc Psychiatry. 2020;2(1):7.
- Mongelli F, Georgakopoulos P, Pato MT. Challenges and opportunities to meet the mental health needs of underserved and disenfranchised populations in the United States. Focus (Am Psychiatr Publ). 2020;18(1):16–24. PubMed CrossRef
- Yang C, Gao H, Li Y, et al. Analyzing the role of family support, coping strategies and social support in improving the mental health of students: evidence from post COVID-19. Front Psychol. 2022;13:1064898. PubMed CrossRef
- Pfefferbaum A, Rohlfing T, Rosenbloom MJ, et al. Variation in longitudinal trajectories of regional brain volumes of healthy men and women (ages 10 to 85 years) measured with atlas-based parcellation of MRI. NeuroImage. 2013;65:176–193. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!



