Abstract
Objective: To assess the relationship of perceived social support and pregnancy related anxiety (PRA) among third trimester pregnant women.
Methods: This was a cross-sectional observational study. The data were collected from July 2021 to March 2022. Study participants included a total of 124 antenatal women who were in their third trimester. PRA was assessed with the Perinatal Anxiety Screening Scale and Pregnancy Anxiety Questionnaire Revised 2. Perceived social support was measured using the Multidimensional Scale for Perceived Social Support (MSPSS). Adequate statistical analysis was done.
Results: Frequency of PRA in the study population was 40.3%. The total MSPSS scores and all its domains were significantly lower in the anxious group (total: P = .002, significant other: P = .006, family: P = .031, and friends: P = .004). PRA was significantly associated with lower perceived social support (P= .002), higher education level (P= .028), and higher number of antenatal visits (P= .031).
Conclusion: Late-pregnancy anxiety is linked to perceived social support, and specific PRA themes (delivery, body shape, and child health) correlate with distinct perceived social support domains.
Prim Care Companion CNS Disord 2025;27(2):24m03833
Author affiliations are listed at the end of this article.
Pregnancy is a unique period in a woman’s life, marked by profound physical, emotional, and psychological changes. While it is often described as a joyous time, pregnancy also brings challenges that can lead to mental health issues such as stress, anxiety, and depression.1 Due to various neurobiological and psychosocial issues, the incidence of mental health problems including stress, anxiety, and depression is more common during pregnancy than in the general population.2 Maternal mental health remains a neglected domain despite the large amount of resources being spent on the care of pregnant women globally and in India.3
Existing literature on mental health disorders during the perinatal period has focused on perinatal depression, and the role of perinatal anxiety disorders remains underrecognized. Across the 3 trimesters of pregnancy, the pooled prevalence of self-reported anxiety symptoms was found to be 18.2% in the first trimester, which increased to 24.6% in the third trimester.4 Among perinatal anxiety disorders, a discrete form of anxiety has been observed, which occurs specifically during pregnancy and revolves only around pregnancy-specific issues. This has been conceptualized as pregnancy specific anxiety or pregnancy-related anxiety (PRA). PRA is a mental state of a pregnant woman whose concerns are specific to the pregnancy itself, such as fears regarding the pregnancy, delivery, and health of the child.1 PRA consists of affective, cognitive, and somatic attributes. The affective attribute consists of the fear of the unknown. The cognitive attribute mainly consists of fetal and maternal well-being, body image, childbirth, parenting, and financial aspects related to having the baby. The somatic attribute mainly includes sleep problems, fatigue tremors, sweating, palpitation, and breathlessness.5
The longitudinal course of PRA has been found to be different from generalized anxiety. PRA occurs more commonly among nulliparous women and is predictive of gestational age at birth and birth weight. The adverse consequences of compromised perinatal mental health affect not only the mother but also the baby, including effects like preterm birth, low birth weight, developmental delay, and poor child mental health.6–9 Women who do not receive treatment may continue to have these symptoms postnatally and potentially through their child’s early years of life.2
Perceived social support is considered a protective factor against anxiety as well as depression.10–12 It is hypothesized that social support may act as a buffer in stressful situations and against the adverse events of the high-stress and life-changing environment of pregnancy and childbirth and being a parent.13,14 Adequate social support and help during pregnancy may contribute to reduced anxiety symptoms and facilitate the transition into safe motherhood.15,16 Social support during pregnancy also helps with recovery during the postpartum period, benefits the parent-child relationship, and improves long-term health consequences for both children and parents.17,18 It has been suggested that social support affects the mental state of women in the third trimester of pregnancy and the levels of anxiety and depression.19 However, there is sparse evidence focusing on such association of social support and PRA. Moreover, most evidence gained in this aspect is from the Western World and might not apply to expectant Indian mothers, as there is a vast difference in the sociocultural practices. Therefore, the present study aims to bridge this gap by exploring the relationship between perceived social support and PRA in Indian third-trimester pregnant women.
METHODS
Study Design and Sampling
This was a cross-sectional observational study. The data were collected from July 2021 to March 2022. Eligibility criteria included antenatal females from the 28th week of pregnancy to full term, who were able to read Hindi or English and willing to participate in the study. Antenatal females who had previous history of psychiatric disorder, who were on any psychotropic medications, or who had profound hearing or vision loss, mental retardation, or significant neurological or chronic illness were excluded from the study. Antenatal females with high-risk pregnancy including severe preeclampsia, fetal growth restriction, and gestational diabetes on insulin or who were in active labor were also excluded. Antenatal females who met the eligibility criteria were recruited from the antenatal clinic of the department of obstetrics and gynecology from a tertiary care center in Western India.
Sample Size
Shafaie et al19 found a negative correlation of r = −0.355 between perceived social support and anxiety. Thus, a sample size of 123 antenatal women was estimated at α value of 0.01, β value of 0.10, and 10% contingency using the formula n = [(Zα+ Zβ)/C]2 + 3.19 Convenience sampling method was used, and study participants were recruited on 2 days in a week.
Study Tools
Perinatal Anxiety Screening Scale. The Perinatal Anxiety Screening Scale (PASS) is 31-item self-rated, acceptable, and psychometrically sound measure that performed well in screening for anxiety disorders in the perinatal period. This tool has screening accuracy of 68% and sensitivity and specificity of 0.7 and 0.3, respectively. The correlation for the PASS global scores was 0.74, indicative of adequate test retest reliability. This tool was used to screen for the presence of anxiety among antenatal females.20,21
Pregnancy Anxiety Questionnaire-Revised 2. The Pregnancy Anxiety Questionnaire-Revised 2 (PRAQ-R2) is a 10-item self-rated Likert scale (1: absolutely not relevant, 2: hardly ever relevant, 3: sometimes relevant, 4: reasonably relevant, and 5: very relevant). It consists of 3 domains: fear of giving birth, worries about bearing a handicapped child, and concern about own appearance. For both nulliparous and parous women, the scale showed an acceptable to good fit to the data (χ234 = 114.28, P < .01, comparative fit index = 0.97, Tucker-Lewis index = 0.96, and root mean square error of approximation = 0.07 for nulliparous and χ234 = 118.39, P < .01, comparative fit index = 0.97, Tucker-Lewis index = 0.96, and root mean square error of approximation = 0.07 for parous women).22
Multidimensional Scale for Perceived Social Support. The Multidimensional Scale for Perceived Social Support (MSPSS) is a self-report measure that contains 12 items designed to measure perceived social support from 3 sources: family, friends, and a significant other. It has been found to have good internal reliability across subject groups, as well as strong factorial validity.23
Statistical Analysis
Fisher exact test was used to test the association between the categorical variables in the anxious and nonanxious groups. Mann-Whitney U test was used to test the difference in the continuous variables between the groups. Spearman correlation was used to identify correlations among the continuous variables.
RESULTS
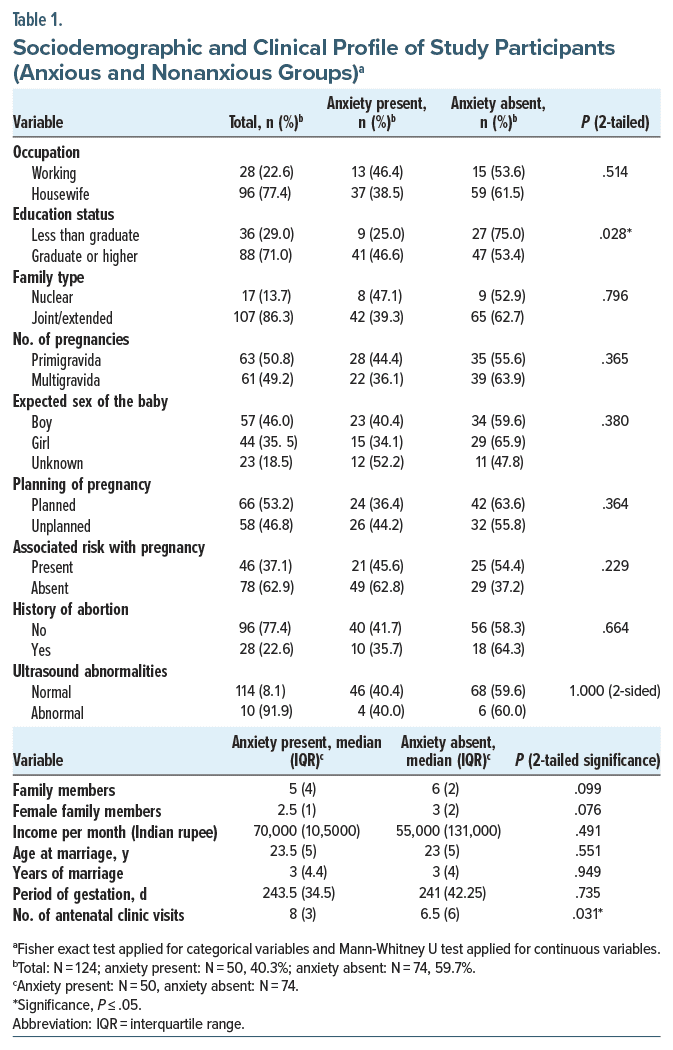
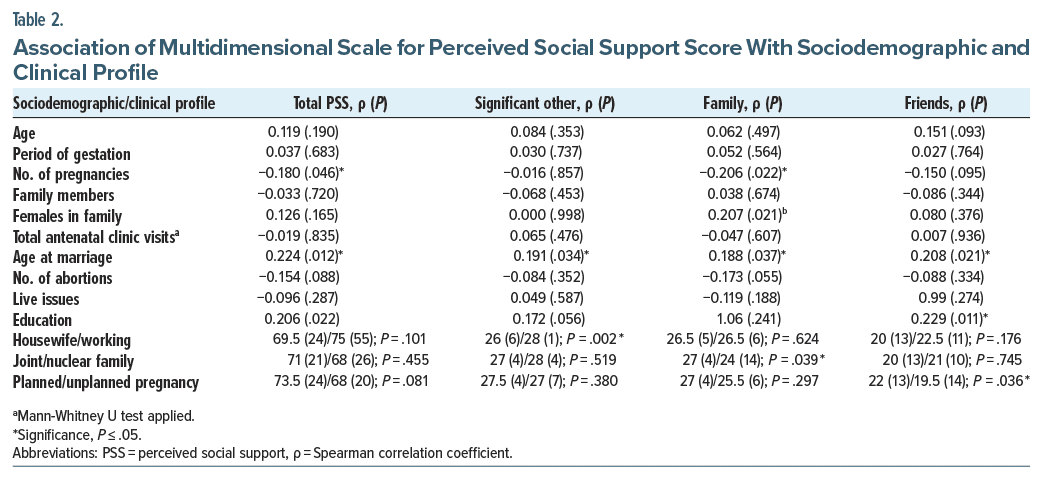
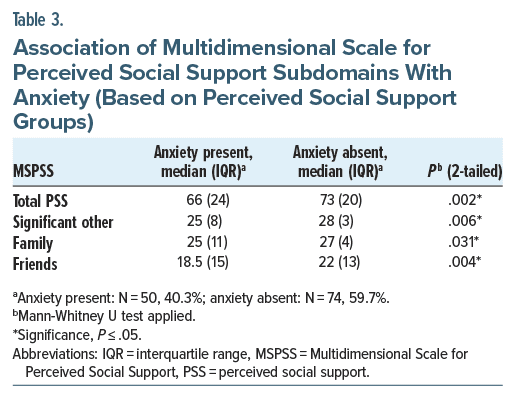
A total of 124 participants were included in the study. The mean ± SD age of the study population was 27.2 ± 4.1 years. The frequency of PRA (PASS score ≥26) among the third-trimester antenatal females in the present study was 40.3%. Table 1 shows the comparison of sociodemographic and clinical profiles of the study participants (anxious and nonanxious groups). The mean ± SD period of gestation was 239.3 ± 24.4 days. Around half of the participants (50.8%) were primigravida, and 32.3% were second gravida. Antenatal females with higher education were significantly more likely to have anxiety. Comparison of MSPSS scores with the sociodemographic and clinical profile of study participants is shown in Table 2. Social support in all domains was found to be significantly lower in the anxious group as shown in Table 3.
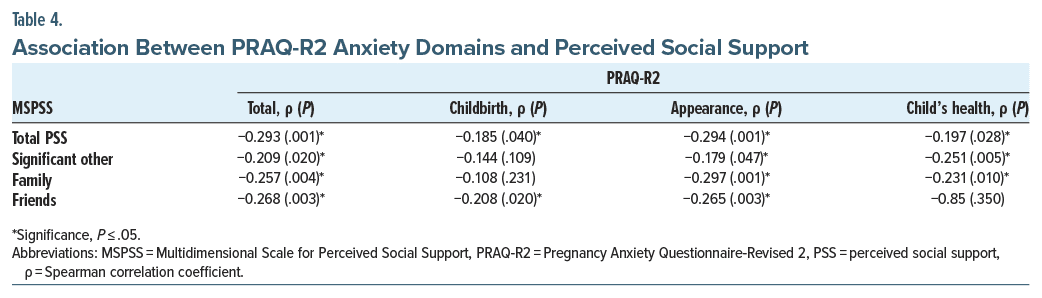
Table 4 shows the correlation between various domains of the PRAQ-R2 and perceived social support among study participants. Significant negative correlations were observed between total MSPSS scores and the overall PRAQ-R2 scores, as well as for all individual domains of the PRAQ-R2. Specifically, the significant other and family domains of the MSPSS were significantly negatively associated with the total PRAQ-R2 score, as well as with scores related to concerns about one’s appearance and the fear of having a handicapped baby. Additionally, the “friends” domain displayed a significant negative correlation with the total PRAQ-R2 scores, along with concerns about appearance and the fear associated with childbirth. Besides negative correlation (P = .052) between the number of females present in the family with worries about the appearance and body changes associated with pregnancy, no other significant association was found between PRAQ-R2 scores and its domains with the sociodemographic profile of the study participants.
DISCUSSION
In the present study, the prevalence of perinatal anxiety was found to be approximately 40% on screening as assessed with the PASS. Higher level of education was found to be associated with higher anxiety. PRA was significantly associated with perceived social support.
The prevalence of anxiety among pregnant women is significantly variable across existing literature. A meta-analysis established the global prevalence of anxiety disorders during pregnancy to be 20.7%.24 Notably, this prevalence rises to 24.5% during the third trimester.24 Furthermore, studies conducted during the COVID-19 pandemic reveal higher prevalence rates, ranging from 30.5% to 34%.25,26 These discrepancies can be directly linked to variations in the sociodemographic characteristics of study participants, the diagnostic criteria utilized, the instruments employed for assessment, and the specific phases of pregnancy investigated.
It is evident from the existing literature that multiple sociodemographic factors play a critical role in influencing anxiety levels in expectant mothers. The present study found that individuals in the anxious group had significantly higher levels of education, with many being graduates or higher (P = .028). This finding is consistent with some earlier studies27,28 but contrasts with others that indicated that respondents with lower education levels exhibited significantly greater anxiety compared to highly educated women.29,30 A systematic review revealed that studies from southeast Asian countries like Bangladesh and Pakistan show anxiety among higher education status women.31 This phenomenon may be attributed to cultural factors in the region, as well as the additional concerns faced by educated women regarding balancing childcare with their careers, which may become challenging in the future. In contrast, previous studies observed that antenatal females belonging to a minority population group30,32 or low socioeconomic status33,34 or who were housewives35,36 were found more often in the anxious group than the nonanxious groups.
The number of female family members was significantly and negatively correlated (P = .052) with worries about body changes associated with pregnancy. This finding may be explained by the observation that females who see other female family members going through similar experiences may feel less anxious about changes in their own bodies. None of the previous studies reported this finding. In the present study, worries about the childbirth process were significantly correlated with the period of gestation. This finding aligns with the study by Silva et al,35 which found that anxiety during pregnancy increased as gestation progressed, with higher levels of anxiety reported in the third trimester compared to the first and second trimesters. As pregnancy progresses and childbirth nears, anxiety can increase due to the anticipation of new responsibilities.
Perceived social support and all its domains were significantly lower in the anxious group compared to the nonanxious group. This finding is consistent with most studies conducted in high-income countries, as well as the low- and middle-income countries, including Canada, Germany, Iran, Pakistan, and China.9,19,34,37,38 Similarly, a study by Nath et al39 in southern India including 380 women found that lower socioeconomic status, low social support, and depression emerged as significant determinants of anxiety. Also, similar conclusions were drawn in previous systematic reviews.12,40 However, a cohort study from Canada including 5,217 pregnant women found that higher anxiety was associated with higher social support.41 The discrepancy may be attributed to the difference in the study population characteristics and sociocultural aspects. It must be borne in mind that perceived social support is deeply seated in the social interaction and culture of a population. In this study, we found that anxiety due to worries regarding childbirth did not significantly correlate with social support from significant others and family; however, it significantly correlated with social support from friends. This can be explained in terms of social conventional norms followed in most Indian settings. The women do not talk about issues of childbirth with their husbands or family members, except possibly the mother or mother in-law, while it is more feasible and unchallenging for women to discuss these matters with their friends and peers. Similarly, the anxiety regarding the birth of a handicapped baby did not significantly correlate with the friend’s domain but did correlate with the significant other and family domain of perceived social support, owing to the fact that significant other and family support may prove useful in the case of the birth of a handicapped baby, while support from friends might not.
In a study from Iran,42 which included 270 nulliparous women, it was found that the total perceived social support correlated significantly with fear of childbirth. In another study in Malawi, however, social support did not differ between women with or without fear of childbirth.43 Similarly, in an African study, anxiety did not correlate significantly with social support of family, however, it did with social support from friends.44 In another study conducted in Icelandic women, it was found that distressed pregnant women had significantly low family and friend support, but not partner support.45 Depending on the country and the sociocultural milieu, social support from different sources is negatively associated with anxiety. In collectivistic cultures like Eastern nations, support from family might be more important. In Western countries, having individualistic cultures, social support from significant others might be more important. More research is needed in this area comparing social support from various sources and anxiety during pregnancy in different regions of the world. This study will add to the existing literature and pave the way for further studies regarding maternal mental health.
Strengths and Limitations
This study highlights PRA among antenatal females and its association with perceived social support in the Indian setting, wherein social support holds great importance owing to the collectivistic Eastern culture and close family bonding. This study provides insight into the Indian social and cultural milieu surrounding pregnant women. The study also sheds light on the various domains of perceived social support and PRA and their relation with each other, which helps to understand the various types of worries women have during pregnancy, the possible areas of social support in India, and their interplay with each other. However, the study has limitations. Small sample size, cross-sectional design, and participants from a clinical setting only limit the generalizability of the findings to community settings. Further studies in the community including large sample size and prospective study design are recommended.
CONCLUSION
This study highlights the critical role of perceived social support in mitigating PRA among Indian women. Screening tools like the PASS and PRAQ-R2 should be integrated into routine antenatal care to identify and support at-risk women. Strengthening social support networks, particularly family and peer groups, is essential for improving maternal mental health outcomes. Furthermore, understanding the various predictive factors for anxiety and depression among pregnant women will not only help in early identification and adequate care for the mothers but also may lead to the birth of healthier babies. Education, awareness, reassurance, and enhancement of social support among women during their critical phase of pregnancy are key to decreasing anxiety and its related complications and improving quality of life as well.
Article Information
Published Online: March 20, 2025. https://doi.org/10.4088/PCC.24m03833
© 2025 Physicians Postgraduate Press, Inc.
Submitted: August 17, 2024; accepted December 20, 2024.
To Cite: Arora IK, Gehlawat P, Gupta T, et al. Association of pregnancy-related anxiety with perceived social support: an observational study among third-trimester antenatal women. Prim Care Companion CNS Disord. 2025;27(2):24m03833.
Author Affiliations: Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bengaluru, India (Arora); Department of Psychiatry, Institute of Human Behaviour and Allied Sciences, New Delhi, India (Gehlawat); Department of Psychiatry, All India Institute of Psychiatry, Jodhpur, India (Gupta, Suthar); Department of Obstetrics and Gynecology, All India Institute of Medical Sciences, Jodhpur, India (Sharma, Singh); Department of Community Medicine and Family Medicine, All India Institute of Medical Sciences, Jodhpur, India (Goel).
Corresponding Author: Pratibha Gehlawat, MD, Department of Psychiatry, Institute of Human Behaviour and Allied Sciences, PO Box 9520, Jhilmil, Dilshad Garden, New Delhi 110095, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: The study was presented in the award poster session at the 75th Annual National Conference of the Indian Psychiatric Society; January 19, 2024; Kochi, Kerala.
Additional Information: Ethical approval was obtained from the Institute’s Ethics Committee via certificate number: AIIMS/IEC/2020/3348.
Clinical Points
- Social support interventions can effectively reduce pregnancy-related anxiety, particularly in collectivistic cultures like India.
- Validated tools such as the Perinatal Anxiety Screening Scale and Pregnancy Anxiety Questionnaire-Revised 2 are essential for comprehensive screening of prenatal anxiety.
- Cultural factors should be considered when designing maternal mental health interventions, ensuring they align with familial and societal norms.
References (45)

- Folliard KJ, Crozier K, Wadnerkar Kamble MM. “Crippling and unfamiliar”: analysing the concept of perinatal anxiety; definition, recognition and implications for psychological care provision for women during pregnancy and early motherhood. J Clin Nurs. 2020;29(23–24):4454–4468.
- Kingston D, Austin M-P, Hegadoren K, et al. Study protocol for a randomized, controlled, superiority trial comparing the clinical and cost- effectiveness of integrated online mental health assessment-referral-care in pregnancy to usual prenatal care on prenatal and postnatal mental health and infant health and development: the Integrated Maternal Psychosocial Assessment to Care Trial (IMPACT). Trials. 2014;15:72.
- Priyadarshini U, Rao AP, Dash S. Recommendations for maternal mental health policy in India. J Public Health Policy. 2023;44(1):90–101.
- Dennis C-L, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. 2017;210(5):315–323.
- Bayrampour H, Ali E, McNeil DA, et al. Pregnancy-related anxiety: a concept analysis. Int J Nurs Stud. 2016;55:115–130.
- Beck CT. Maternal depression and child behaviour problems: a meta-analysis. J Adv Nurs. 1999;29(3):623–629.
- Glasheen C, Richardson GA, Fabio A. A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health. 2010;13(1):61–74.
- Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clin Obstet Gynecol. 2008;51(2):333–348.
- Martini J, Petzoldt J, Einsle F, et al. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective longitudinal study. J Affect Disord. 2015;175:385–395.
- Macalli M, Côté S, Tzourio C. Perceived parental support in childhood and adolescence as a tool for mental health screening in students: a longitudinal study in the i-Share cohort. J Affect Disord. 2020;266:512–519.
- Scardera S, Perret LC, Ouellet-Morin I, et al. Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Netw Open. 2020;3(12):e2027491.
- Wang J, Mann F, Lloyd-Evans B, et al. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156.
- Helgeson VS. Social support and quality of life. Qual Life Res. 2003;12(Suppl 1):25–31.
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11(2):213–218.
- Corrigan CP, Kwasky AN, Groh CJ. Social support, postpartum depression, and professional assistance: a survey of mothers in the Midwestern United States. J Perinat Educ. 2015;24(1):48–60.
- Stapleton LRT, Schetter CD, Westling E, et al. Perceived partner support in pregnancy predicts lower maternal and infant distress. J Fam Psychol. 2012;26(3):453–463.
- Sedigheh A, Keramat A. The relationship between perceived social support from family and postpartum empowerment with maternal wellbeing in the postpartum period. J Midwifery Reprod Health. 2016;4(4):779–787.
- Gan Y, Xiong R, Song J, et al. The effect of perceived social support during early pregnancy on depressive symptoms at 6 weeks postpartum: a prospective study. BMC Psychiatry. 2019;19(1):232.
- Shafaie FS, Mirghafourvand M, Rahmati M, et al. Association between psychological status with perceived social support in pregnant women referring to Tabriz health centers. J Matern Fetal Neonatal Med. 2018;31(12):1554–1560.
- Somerville S, Byrne SL, Dedman K, et al. Detecting the severity of perinatal anxiety with the Perinatal Anxiety Screening Scale (PASS). J Affect Disord. 2015;186:18–25.
- Somerville S, Dedman K, Hagan R, et al. The Perinatal Anxiety Screening Scale: development and preliminary validation. Arch Womens Ment Health. 2014;17(5):443–454.
- Huizink AC, Delforterie MJ, Scheinin NM, et al. Adaption of Pregnancy Anxiety Questionnaire-Revised for all pregnant women regardless of parity: PRAQ-R2. Arch Womens Ment Health. 2016;19(1):125–132.
- Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study. J Clin Psychol. 1991;47(6):756–761.
- Fawcett EJ, Fairbrother N, Cox ML, et al. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate bayesian meta analysis. J Clin Psychiatry. 2019;80(4):18r12527.
- Sun F, Zhu J, Tao H, et al. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynaecol. 2021;42(2):91–99.
- Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2021;300:113912.
- Nwafor JI, Okedo-Alex IN, Ikeotuonye AC. Prevalence and predictors of depression, anxiety, and stress symptoms among pregnant women during COVID 19-related lockdown in Abakaliki, Nigeria. Malawi Med J. 2021;33(1):54–58.
- Sinaci S, Ozden Tokalioglu E, Ocal D, et al. Does having a high-risk pregnancy influence anxiety level during the COVID-19 pandemic? Eur J Obstet Gynecol Reprod Biol. 2020;255:190–196.
- He L, Wang T, Xu H, et al. Prevalence of depression and anxiety in women with recurrent pregnancy loss and the associated risk factors. Arch Gynecol Obstet. 2019;300(4):1061–1066.
- van de Loo KFE, Vlenterie R, Nikkels SJ, et al. Depression and anxiety during pregnancy: the influence of maternal characteristics. Birth. 2018;45(4):478–489.
- Biaggi A, Conroy S, Pawlby S, et al. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. 2016;191:62–77.
- González-Mesa E, Kabukcuoglu K, Körükcü O, et al. Correlates for state and trait anxiety in a multicultural sample of Turkish and Spanish women at first trimester of pregnancy. J Affect Disord. 2019;249:1–7.
- Berthelot N, Lemieux R, Garon-Bissonnette J, et al. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. 2020;99(7):848–855.
- Shangguan F, Wang R, Quan X, et al. Association of stress-related factors with anxiety among Chinese pregnant participants in an online crisis intervention during COVID-19 epidemic. Front Psychol. 2021;12:633765.
- Silva MMdeJ, Nogueira DA, Clapis MJ, et al. Anxiety in pregnancy: prevalence and associated factors. Rev Esc Enferm USP. 2017;51:e03253.
- Tang X, Lu Z, Hu D, et al. Influencing factors for prenatal Stress, anxiety and depression in early pregnancy among women in Chongqing, China. J Affect Disord. 2019;253:292–302.
- Akiki S, Avison WR, Speechley KN, et al. Determinants of maternal antenatal state-anxiety in mid-pregnancy: role of maternal feelings about the pregnancy. J Affect Disord. 2016;196:260–267.
- Waqas A, Raza N, Lodhi HW, et al. Psychosocial factors of antenatal anxiety and depression in Pakistan: is social support a mediator? PLoS One. 2015;10(1):e0116510.
- Nath A, Venkatesh S, Balan S, et al. The prevalence and determinants of pregnancy-related anxiety amongst pregnant women at less than 24 weeks of pregnancy in Bangalore, Southern India. Int J Womens Health. 2019;11:241–248.
- Bedaso A, Adams J, Peng W, et al. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. 2021;18(1):162.
- Dunkel Schetter C, Niles AN, Guardino CM, et al. Demographic, medical, and psychosocial predictors of pregnancy anxiety. Paediatr Perinat Epidemiol. 2016;30(5):421–429.
- Azimi M, Fahami F, Mohamadirizi S. The relationship between perceived social support in the first pregnancy and fear of childbirth. Iran J Nurs Midwifery Res. 2018;23(3):235–239.
- Khwepeya M, Lee GT, Chen S-R, et al. Childbirth fear and related factors among pregnant and postpartum women in Malawi. BMC Pregnancy Childbirth. 2018;18(1):391.
- van Heyningen T, Honikman S, Myer L, et al. Prevalence and predictors of anxiety disorders amongst low-income pregnant women in urban South Africa: a cross sectional study. Arch Womens Ment Health. 2017;20(6):765–775.
- Jonsdottir SS, Thome M, Steingrimsdottir T, et al. Partner relationship, social support and perinatal distress among pregnant Icelandic women. Women Birth. 2017;30(1):e46–e55.
Enjoy this premium PDF as part of your membership benefits!