Abstract
Objective: Proactive consultation-liaison (C-L) psychiatry aims to meet the mental health needs of medical-surgical populations—many of which go unmet by the conventional C-L model—through systematic screening and integrated care. We implemented an automated screening list to enhance case identification of an existing proactive C-L service and evaluated service metrics along with clinician- and patient-reported outcomes.
Methods: Service outcomes were evaluated using historical and contemporary comparison data. Adjusted difference-in-difference analyses were used to determine change in consult characteristics, mean length of stay (LOS), and scores on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Practitioners and nurses were surveyed regarding service satisfaction, perceived safety, and burnout.
Results: During the intervention, the consult rate was 3-fold higher than at baseline. Change in time to consultation was equivocal. Overall mean LOS was not reduced, but observed LOS was 1.2 days shorter than expected among non-COVID patients receiving psychiatric consultation (P = not significant). Mean patient-rated hospital satisfaction on HCAHPS was 1 point higher on intervention units during the intervention. Surveys revealed broad satisfaction with this model among practitioners and improved perception of safety among nurses.
Conclusions: Proactive C-L psychiatry enhanced by automated screening was associated with improved service utilization and evidence suggestive of LOS reduction among those most likely to receive direct benefit from this model of care. Further, both patient and clinician ratings were improved during the intervention. Proactive C-L psychiatry provides benefits to patients, clinicians, and health systems and may be poised to achieve the Triple Aim in health care.
Prim Care Companion CNS Disord 2024;26(2):23m03647
Author affiliations are listed at the end of this article.
Psychiatric comorbidity is present in roughly a half of medical inpatients1,2 and associated with longer length of stay (LOS), higher health care costs, and lower staff satisfaction.3,4 Mental health care in acute medical-surgical settings is traditionally delivered “reactively” by consultation-liaison (C-L) psychiatry services after clinical needs are identified by primary medical-surgical clinicians.5 However, traditional C-L services usually address only a minority of actionable mental health needs.1,6,7 By contrast, interdisciplinary proactive C-L services screen medical inpatient populations systematically for mental health concerns and deliver integrated care with primary teams, aiming to prevent crises and to manage a broad range of mental health issues.5 Proactive C-L has been associated with reduced LOS, enhanced psychiatric service utilization, reduced time to psychiatric consultation, and improved practitioner and nurse satisfaction.5,8
Whereas screening for actionable mental health needs is the defining aspect of proactive C-L, how best to screen for them remains unclear. Screening in published work has ranged from the use of mental health questionnaires9 to co-rounding with medical teams1 and in-person visits by psychiatrists.10 Currently, most proactive C-L services use a combination of manual chart review supplemented by direct collaboration with primary teams,5,11 as has been done at our institution.12 The electronic medical record (EMR) has also been used to enhance case identification,13 though the outcomes of using an automated EMR list have yet to be reported. Moreover, with growing disposition challenges and prolonged emergency department (ED) boarding times across the United States,12 the use of an automated EMR report stands to enhance service capabilities by improving efficiency and reliability in identifying mental health needs.
Patient satisfaction, which now impacts Medicare reimbursements,14 is another outcome that remains unexplored in association with proactive C-L. A recent study suggests that psychology consultations among medical inpatients were associated with improved patient satisfaction,15 whereas the overall number of inpatient consultations (not restricted to mental health) has been associated with lower patient satisfaction.16 Optimizing who receives consultations is important; however, to our knowledge, patient satisfaction with hospital care has not been assessed in relation to any type of psychiatric consultation. One suspects that patient satisfaction could be improved by addressing unmet mental health needs among medical-surgical inpatients.
We created an automated EMR screening list to enhance our screening process (previously reported17) and then evaluated service outcomes after a year-long implementation project. Our primary aim was to evaluate change in mean unit LOS using a regression-adjusted difference-in-difference (ΔΔa) model with historical and contemporary comparator units and sensitivity analyses, restricting our analysis to non-COVID patients receiving psychiatric consultation (ie, patients likeliest to receive direct benefit). Secondary aims evaluated additional service metrics, including patient- and clinician-reported outcomes.
METHODS
Model Innovation
In 2018, the Proactive Integration of Mental health care in Medicine (PRIME) service was developed at Strong Memorial Hospital (SMH) to serve 3 hospital medicine units staffed by advanced practice provider (APP) hospitalist teams. For this project, we created an automated EMR list to identify patients on APP-staffed hospital medicine services with acute mental health needs. This automated list, published in the EMR September 1, 2021, populated patients based on discrete form data that could index mental health acuity, severity, or complexity (Supplementary Table 1).17
During this project, PRIME consisted of a 0.8 full-time–equivalent (FTE) psychiatric nurse practitioner and 0.6 FTE psychiatrist, and it covered 3 hospital medicine units (“PRIME units”), as published previously.12 This project expanded the scope of chart screening 2-fold, as it included patients in the ED awaiting transfer to a medicine unit. Both PRIME and general C-L psychiatry clinicians participated in daily screening; however, PRIME clinicians consulted only on patients on PRIME units, and general C-L service clinicians consulted on patients elsewhere. The screening clinician reviewed any potentially actionable mental health needs identified on chart review with the assigned primary team clinician.
Project Definitions
Comparison units consisted of the same 2 teaching hospital medicine units at SMH (SMH comparison) as previously described12 plus 2 comparison medical-surgical units at Highland Hospital (HH comparison), an affiliate hospital in the same city, to account for regional care trends. Academic years are specified as follows: July 2017–June 2018 (pre-PRIME, the year prior to initial PRIME pilot), 2018–2019 (PRIME pilot, previously reported12), 2019–2020 (intervening year, not included in current analyses), 2020–2021 (pre–quality improvement [QI] [early COVID]), 2021–2022 (QI intervention [later COVID waves]). Unless otherwise specified, ΔΔa analyses compare QI intervention to the pre-PRIME period, the last year prior to initial PRIME implementation. Consistent with prior analyses,12 we exclude July/August due to staffing changes and onboarding.
All ΔΔa analyses are adjusted for age, sex, race/ethnicity, Charlson comorbidity index (CCI), payer type, boarding time (arrival on unit minus time of admission order), discharged home (binary), failure to thrive (binary), and mental health diagnosis categories. We exclude the following outliers: LOS > 30, in-hospital mortality, discharge against medical advice, non-ED admission source, and patients with an eating disorder diagnosis (rationale previously described12).
Service Evaluation
We first characterized our sample; then we described change in consult rate and boarding times for each set of units and 3 periods. We evaluated time to consultation for PRIME and SMH comparison units (HH comparator units excluded for low volume) for the same 3 periods. Given the effect of boarding time on time to consult, we conducted a post hoc ΔΔa analysis, setting time to consult ≥ 1 day as the dependent variable.
Next, we characterized the quarterly LOS trends on the 3 sets of units. All main ΔΔa LOS analyses compare the change in LOS from pre-PRIME to QI intervention on PRIME units versus LOS change on comparison units. For sensitivity analysis, we repeat ΔΔa restricted to non-COVID patients who received psychiatric consultation—the patients likeliest to receive direct benefit.
We evaluated ΔΔa in the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) items analogous to the primary analysis (see Supplement A for description). Responses were converted to numerical values, with higher values being more favorable. Included items were scored ordinally 1–4 except for “overall rating of hospital,” whose responses range from 0 to 10. To calculate aggregate section scores and account for skip patterns, all valid scores in each section were added, and each total was divided by the number of valid scores. The “overall rating of hospital” item was declared a priori as the HCAHPS item of primary interest.
Clinician-Related Evaluation
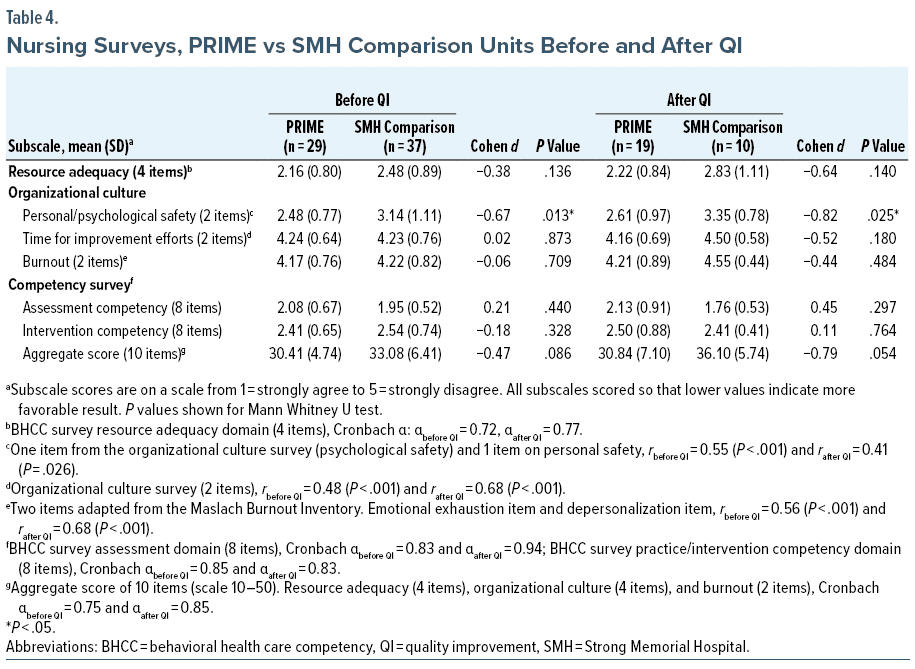
Before and after this project (August 2021 and 2022), we invited nurses and practitioners on PRIME and SMH comparison units to complete the same surveys as before.4 Nursing respondents on PRIME and SMH comparison units are analogous; practitioners on PRIME units include physicians and APPs, whereas practitioner respondents on SMH comparison units included only attending physicians (resident physicians excluded for frequent turnover). Surveys were distributed by nursing and hospital medicine leadership, with 2 reminder e-mails per survey.
Responses were combined for each unit group (PRIME/SMH comparison), clinician type (practitioner/nurse), and time (before/after QI). Lower values represent more favorable responses. An average sum of the 10 main survey items was calculated for each clinician subgroup (range, 10–50). Subscale items were aggregated, and internal consistency was evaluated with Cronbach α or bivariate correlation.
We conducted pairwise comparisons between average sums using nonparametric, exact Mann Whitney U tests to determine change over time on PRIME and SMH comparison units. Next, we evaluated pre-post practitioner responses. Average sum and aggregated subscale items were reported. A low number of responses of SMH comparison unit practitioners precluded pairwise comparisons between PRIME and SMH comparison units. We also reported Cohen d values for effect sizes (≥ 0.2 small, ≥ 0.5 medium, ≥ 0.8 large). Nursing survey analyses were analogous to that of practitioners except that PRIME and SMH comparison nurse responses were compared given an adequate number of SMH comparison respondents.
RESULTS
Service Outcomes
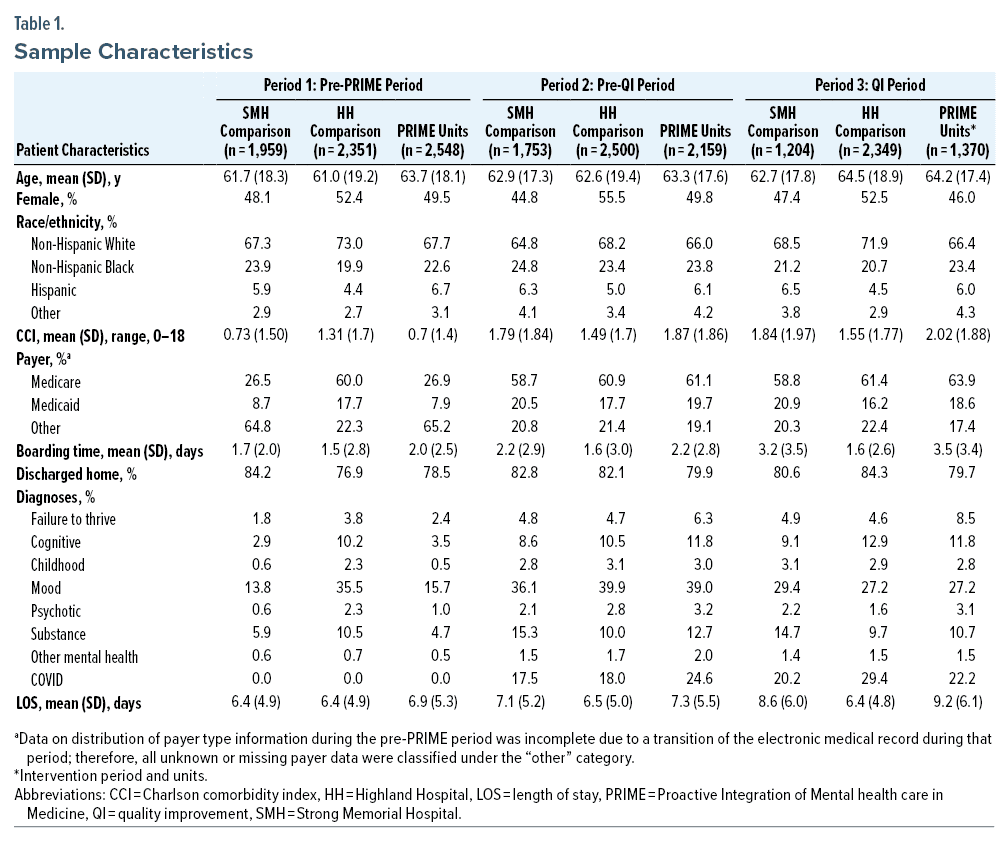
Sample characteristics are reported in Table 1. The proportion of patients on PRIME units who received a consultation during the pre-PRIME year was 3.2% versus 9.6% during QI intervention (without exclusions, the QI intervention consult rate was 13.5%). The SMH comparison unit consult rate was effectively unchanged, from 3.2% to 3.5%. On ΔΔa analysis, the consult rate on PRIME units was 2.7 times higher during the QI intervention period than expected after adjusting for covariates (P < .001).
In absolute terms, mean boarding time was substantially higher during the QI intervention period than the pre-PRIME period, increasing from 2.0 to 3.5 days for patients admitted to PRIME units and from 1.7 to 3.2 days for patients admitted to SMH comparison units. Boarding time for HH comparison units was unchanged, from 1.5 days to 1.6 days.
During the QI intervention, unadjusted mean time to consult on PRIME units was slightly less than it was during the pre-PRIME year (1.5 days vs 1.7 days, respectively). This was despite substantially longer boarding time, suggesting that a larger proportion of psychiatric consultation orders were placed on patients prior to arrival on PRIME units. Curiously, time to psychiatric consult order on SMH comparison units was lower during QI intervention period than the pre-QI period (0.7 days vs 1.2 days, respectively), in the absence of proactive screening on these units and, as above, with an unchanged consult rate.
On ΔΔa analysis, consult latency was not reduced compared to the pre-PRIME year; rather, it was 0.36 days longer than expected (1.15 days expected vs 1.51 days observed, P = .65), which was due in large part to the shorter time to consultation on SMH comparison units during the QI intervention. In a post hoc ΔΔa analysis that defined prolonged time to consult categorically as ≥ 1 day, we found that that the likelihood of consultation within a day of admission order was nearly identical to the expected value (0.44% observed, 0.46% expected, P = .81). This provides further evidence that proactive screening among boarding patients was effective given that boarding times were even longer during the QI intervention period.
Length of Stay
The mean LOS increased on both PRIME and SMH comparison units over the prior few years (Supplementary Figure 1). For the primary ΔΔa analysis, we found that the expected LOS during the QI intervention year was 9.3 days compared to 6.9 days during the pre-PRIME year, indicating a marked increase in overall care complexity of PRIME unit patients during the QI intervention. However, the observed LOS was 9.6, or 0.3 days (3.3%) higher than expected (P = not significant). Our QI project was not associated with a reduction in unit-wide mean LOS.
Secondary ΔΔa analyses found that patients receiving psychiatric consultation (n = 131) had a 0.5 day (3.8%) shorter LOS than expected (12.6 vs 12.2 days, P = not significant). Excluding patients with COVID did not affect the primary LOS analysis (expected 9.2 vs observed 9.5 days, or 3.4% higher); however, it did reveal an even more favorable point estimate of LOS reduction among patients receiving psychiatric consultation of 1.2 days (n = 108; expected 12.4 vs observed 11.2 days, 9.1% reduction, P = not significant).
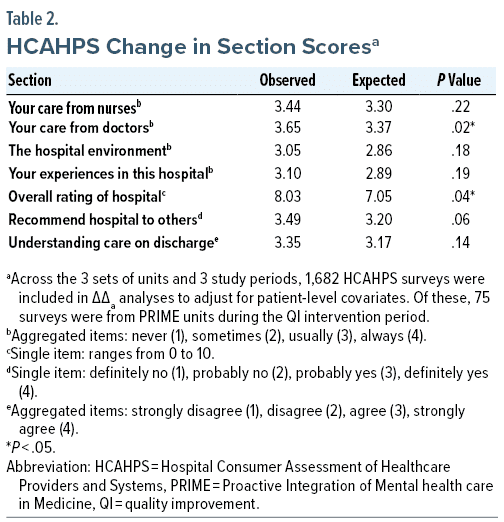
HCAHPS Item
Across units, the response rate was 9.3%; this includes 6.9% for PRIME units, 7.7% for SMH comparison units, and 12.3% for HH comparison units. On ΔΔa analysis, each of the mean HCAHPS section scores was higher than expected during the intervention (Table 2). Of these, patient ratings of “care from doctors” was statistically improved, and the single item “overall rating of hospital,” an a priori outcome of interest, was statistically improved as well (P = .036). Improvement in likelihood of recommending the hospital to others trended toward statistical significance.
Clinician-Rated Outcomes
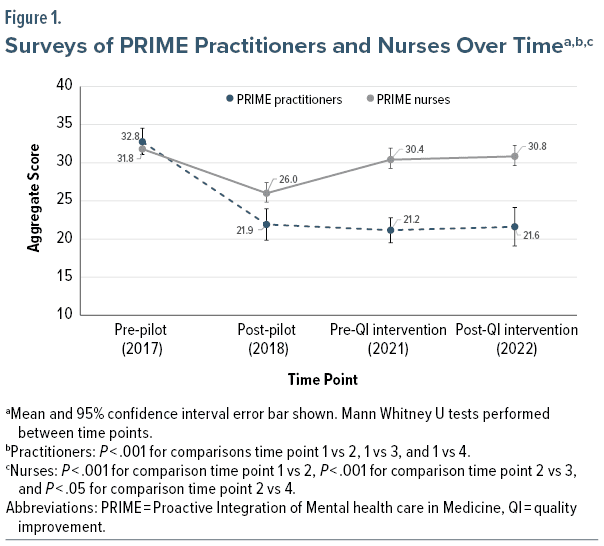
The number of surveys completed by each subgroup is shown in Supplementary Table 2. Figure 1 depicts responses by PRIME clinicians over time. Practitioner responses before QI were improved relative to responses before PRIME originally launched (P < .001). Practitioner responses after QI remained improved relative to pre-PRIME baseline (P < .001). Nurse responses before this QI project had largely returned to pre-PRIME levels and remained similar at the end of the QI project.
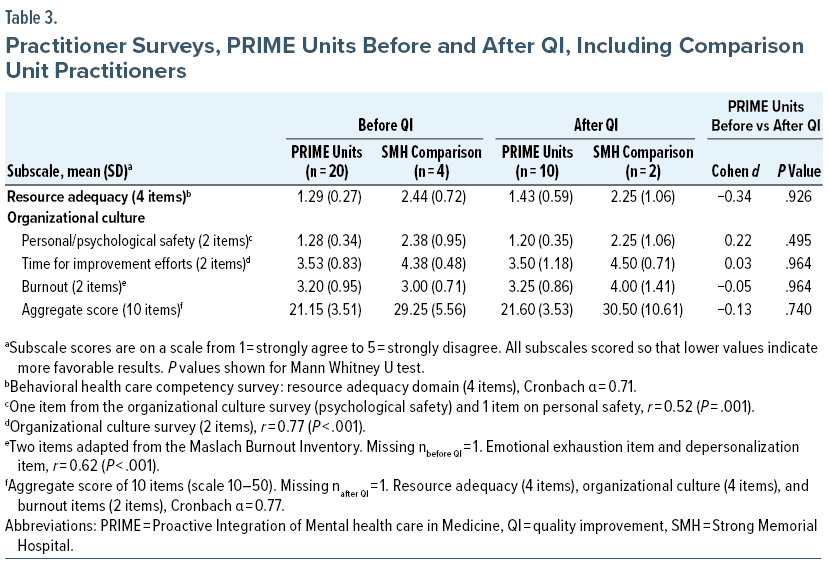
Although mean PRIME practitioner responses were considerably more favorable than practitioner responses on SMH comparison units (statistical comparison omitted due to small SMH comparison sample size), there was no change in overall aggregate or subscale scores over the course of this QI project (Table 3).
Before the QI project, nurses on PRIME units reported moderately higher safety than nurses on comparison units (Cohen d = −0.67) (Table 4). There was a trend of greater overall favorability among nurses on PRIME units versus nurses on comparison units (30.4 vs 33.1, Cohen d = −0.47, P = .086). After the QI intervention period, nurses on PRIME units continued to report moderately higher safety ratings than nurses on comparison units (Cohen d = −0.82). Consistent with responses before QI, there was a continued trend of greater overall favorability among nurses on PRIME units versus nurses on comparison units (Cohen d = −0.79, P = .054). Before/after subscale scores of PRIME nurses and comparison unit nurses did not change (Supplementary Tables 3 and 4).
Discussion
This current report of mixed results expands upon our prior work describing the clinical value of a proactive C-L service by characterizing service outcomes after implementing an automated screening list. We did not find proactive C-L to be associated with unit-wide LOS reduction, yet sensitivity analyses restricted to non-COVID patients receiving psychiatric consultation favored PRIME, with average LOS 1.2 days shorter than expected. If this point estimate is correct, then PRIME might have reduced up to 155 hospital days, annualized, consistent with prior evidence of financial benefit with this model.18
During this project, the consult rate was 3-fold higher than during the pre-PRIME year, indicating that this model continued to address previously unmet mental health needs. Additionally, these analyses excluded patients with LOS > 30 days, a subpopulation with a considerably higher psychiatric consult rate, hence the pre-exclusion QI consult rate of 13.5% across PRIME units. Despite the further lengthening of boarding times and no change on main time-to-consult ΔΔa analysis, the absolute time to psychiatric consultation was unchanged, implying that screening was effective. The results of a post hoc analysis defining prolonged time to consult as ≥ 1 day was consistent with greater degree of proactivity.
Supplementary Figure 1 reveals that the unadjusted hospital LOS increased considerably, especially about a year into the COVID pandemic, with the expected LOS during the QI intervention year more than 2 days longer than pre-QI when adjusting for the rising prevalence of covariates associated with LOS. The rising LOS is attributable to a reduced number of available skilled nursing facility beds in the community related to workforce impacts of COVID. Delayed disposition and increased inpatient census were also likely responsible for upstream delays in transfer from the ED to inpatient units.19
Results of patient-reported outcomes on HCAHPS were broadly favorable, with statistical improvements in ratings of doctors and the hospital overall. In fact, the mean hospital rating was higher than expected by nearly a full point on a 10-point scale. Although we cannot attribute these changes in full to our project, it is at least plausible that PRIME’s presence accounted for a portion of this effect. To our knowledge, the finding of improved patient-reported outcomes during a C-L psychiatry intervention is novel, and it deserves replication.
Practitioner-reported improvements evident after the original pilot were maintained through COVID. Going from 32.8 (note: 30 is neutral) to 21 implied that the rating of each item was, on average, a full point improved on the Likert scale. Although statistical comparison was omitted between PRIME and SMH comparison practitioners, the before and after point estimates of the SMH comparison unit practitioners were nearly identical to the pre-PRIME baseline.
Nurse perceptions of safety on PRIME units appeared to be more favorable than SMH comparison unit respondents before and after this project (Cohen d = −0.67 [medium effect size] and 0.82 [large], respectively). This is especially encouraging in view of the greater medical complexity of unit populations during the QI intervention period. The lack of improvement on overall composite scores could be explained by higher nurse distress and burnout since COVID,20 leading to increased turnover and a higher proportion of travel nurses to fill vacancies. Additionally, PRIME provided greater collaborative support to practitioners than to nurses. There is an opportunity for further interprofessional mental health collaboration with nurses.21
Similar to how collaborative care aims to provide population-level benefits in outpatient settings, proactive C-L aims to provide benefits for inpatient medical populations.5,22 Our results suggest that proactive C-L, as enhanced with automated screening, could help to achieve the Institute for Healthcare Improvement’s Triple Aim and even the informal Quadruple Aim, which adds clinician wellness.23,24 Although the proactive C-L literature is expanding, it remains primarily limited to academic hospital medicine services, with rare publications elsewhere such as critical care25 or rural settings.6 Expanding into settings with higher per-patient care costs may make for an even stronger argument for proactive C-L. Another gap in the proactive C-L literature is the absence of randomized controlled trials,26 though the results of the HOME Study27 are forthcoming.
This study was subject to the following limitations. First, this was QI rather than research, and our population was not necessarily generalizable to other settings. Second, the intervention was delivered in a nonrandomized fashion without blinding. Nevertheless, other than clinician surveys, these data were collected without clinician awareness, and survey respondents knew survey responses were anonymous. Third, we could not rule out the potential effects of variably overlapping QI projects that may have affected our reported outcomes. Fourth, HCAHPS scores represented responses from a subpopulation of inpatients who chose to respond and thus could be partly confounded by response rate bias28; however, this potential was mitigated via regression-adjusted analyses of HCAHPS data that controlled for patient-level covariates.
Our proactive C-L service enhanced by automated EMR screening resulted in an increased consult rate, evidence consistent with earlier consultation, and a trend of reduced hospital LOS among patients expected to receive direct benefit. Patients’ mean hospital rating improved on PRIME units. Our service was rated more favorably by practitioners overall and by nurses in terms of safety. Our year-long QI project therefore provides evidence of how proactive C-L could be poised to meet the Triple Aim of health care.
Clinical Points
- Automated screening can facilitate enhanced psychiatric service utilization in hospital medicine.
- Data on length of stay reduction associated with this project were inconclusive.
- Patient- and clinician-reported outcomes were improved with this model of care.
Article Information
Published Online: March 19, 2024.
https://doi.org/10.4088/ PCC.23m03647
© 2024 Physicians Postgraduate Press, Inc.
Submitted: September 25, 2023; accepted December 14, 2023.
To Cite: Oldham MA, Maeng DD, Heaney B, et al. Automated screening to enhance proactive consultation-liaison psychiatry services in acute medicine units: evaluation of service outcomes. Prim Care Companion CNS Disord. 2024;26(2):23m03647.
Author Affiliations: Department of Psychiatry, University of Rochester Medical Center, Rochester, New York (Oldham, Maeng, Heaney, Walsh, Gleber, Nasra, Lee); Department of Medicine, University of Rochester Medical Center, Rochester, New York (Gleber, Hopkin).
Corresponding Author: Mark A. Oldham, MD, 300 Crittenden Blvd, Box PSYCH, Rochester, NY 14642 ([email protected]).
Funding/Support: This project was supported by a quality improvement grant from University of Rochester Medical Faculty Group Healthcare Innovation Pilot Awards Program (Rochester, New York).
Role of Sponsor: The funding source had no role in the design of this project and no role during its execution, analyses, interpretation of the data, or decision to submit results.
Relevant Financial Relationships: None.
Supplementary Material: Available at Psychiatrist.com.
References (28)

- Desan PH, Zimbrean PC, Weinstein AJ, et al. Proactive psychiatric consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011;52(6):513–520. PubMed CrossRef
- van Niekerk M, Walker J, Hobbs H, et al. The prevalence of psychiatric disorders in general hospital inpatients: a systematic umbrella review. J Acad Consult Liaison Psychiatry. 2022;63(6):567–578. PubMed CrossRef
- Bourgeois JA, Kremen WS, Servis ME, et al. The impact of psychiatric diagnosis on length of stay in a university medical center in the managed care era. Psychosomatics. 2005;46(5):431–439. PubMed CrossRef
- Oldham MA, Walsh P, Maeng DD, et al. Integration of a proactive, multidisciplinary mental health team on hospital medicine improves provider and nursing satisfaction. J Psychosom Res. 2020;134:110112. PubMed CrossRef
- Oldham MA, Desan PH, Lee HB, et al; Council on Consultation-Liaison Psychiatry. Proactive consultation-liaison psychiatry: American Psychiatric Association resource document. J Acad Consult Liaison Psychiatry. 2021;62(2):169–185. PubMed CrossRef
- Kugler J, Key R, Murthy S, et al. The C-L Psychiatrist as Expert in Value-based Care Models: Three Diverse C-L Led Initiatives for Increasing Access to Care and Improving Treatment Outcomes. CLP 2018: The Annual Meeting of the Academy of Consultation-Liaison Psychiatry. Orlando, FL; 2018.
- Chen KY, Evans R, Larkins S. Why are hospital doctors not referring to consultation-liaison psychiatry? A systemic review. BMC Psychiatry. 2016;16(1):390. PubMed CrossRef
- Oldham MA, Chahal K, Lee HB. A systematic review of proactive psychiatric consultation on hospital length of stay. Gen Hosp Psychiatry. 2019;60:120–126. PubMed CrossRef
- Camus V, Viret C, Porchet A, et al. Effect of changing referral mode to C-L psychiatry for noncognitively impaired medical inpatients with emotional disorders. J Psychosom Res. 2003;54(6):579–585. PubMed CrossRef
- Strain JJ, Lyons JS, Hammer JS, et al. Cost offset from a psychiatric consultation-liaison intervention with elderly hip fracture patients. Am J Psychiatry. 1991;148(8):1044–1049. PubMed CrossRef
- Sledge WH, Gueorguieva R, Desan P, et al. Multidisciplinary proactive psychiatric consultation service: impact on length of stay for medical inpatients. Psychother Psychosom. 2015;84(4):208–216. PubMed CrossRef
- Oldham MA, Lang VJ, Hopkin JL, et al. Proactive integration of mental health care in hospital medicine: PRIME medicine. J Acad Consult Liaison Psychiatry. 2021;62(6):606–616. PubMed CrossRef
- Finn CT, Thakur D, Shea KM, et al. Electronic medical record reporting enhances proactive psychiatric consultation. Psychosomatics. 2018;59(6):561–566. PubMed CrossRef
- Mazurenko O, Collum T, Ferdinand A, et al. Predictors of hospital patient satisfaction as measured by HCAHPS: a systematic review. J Healthc Manag. 2017;62(4):272–283. PubMed CrossRef
- Bullock AJ, Sorbello A, Gilrain KL, et al. Patient satisfaction with a psychology consultation-liaison service at an academic medical center. J Clin Psychol Med Settings. 2022;29(4):717–726. PubMed CrossRef
- Schmocker RK, Holden SE, Vang X, et al. The number of inpatient consultations is negatively correlated with patient satisfaction in patients with prolonged hospital stays. Am J Surg. 2016;212(2):282–288. PubMed CrossRef
- Oldham MA, Heaney B, Gleber C, et al. Using discrete form data in the electronic medical record to predict the likelihood of psychiatric consultation. J Acad Consult Liaison Psychiatry. 2023 Oct 17: S2667-2960(23)00132-5. PubMed CrossRef
- Sledge WH, Bozzo JE, White-McCullum BA, et al. The cost-benefit from the perspective of the hospital of a proactive psychiatric consultation service on inpatient general medicine services. Health Econ Outcome Res Open Access. 2016;2(4):122.
- NEJM Catalyst. What is patient flow? NEJM Catal. 2018;4(1).
- Galanis P, Vraka I, Fragkou D, et al. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. PubMed CrossRef
- Pannick S, Davis R, Ashrafian H, et al. Effects of interdisciplinary team care interventions on general medical wards: a systematic review. JAMA Intern Med. 2015;175(8):1288–1298. PubMed CrossRef
- Kathol RG, Kunkel EJ, Weiner JS, et al. Psychiatrists for medically complex patients: bringing value at the physical health and mental health/substance-use disorder interface. Psychosomatics. 2009;50(2):93–107. PubMed CrossRef
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. PubMed CrossRef
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769. PubMed CrossRef
- Bui M, Thom RP, Hurwitz S, et al. Hospital length of stay with a proactive psychiatric consultation model in the medical intensive care unit: a prospective cohort analysis. Psychosomatics. 2018. PubMed CrossRef
- Toynbee M, Walker J, Clay F, et al. The effectiveness of inpatient consultation-liaison psychiatry service models: a systematic review of randomized trials. Gen Hosp Psychiatry. 2021;71:11–19. PubMed CrossRef
- Walker J, Burke K, Toynbee M, et al. The HOME Study: study protocol for a randomized controlled trial comparing the addition of proactive psychological medicine to usual care, with usual care alone, on the time spent in hospital by older acute hospital inpatients. Trials. 2019;20(1):483. PubMed CrossRef
- Siddiqui ZK, Wu AW, Kurbanova N, et al. Comparison of Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction scores for specialty hospitals and general medical hospitals: confounding effect of survey response rate. J Hosp Med. 2014;9(9):590–593. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!