Camptocormia, or “bent spine syndrome” (Greek Kamptein meaning “to bend” and Kormos meaning “trunk”), refers to an abnormal posture with marked flexion of the thoracolumbar spine that increases during walking and resolves in the supine position.1 This last feature is a characteristic differential sign.2 It is an often overlooked adverse effect of antipsychotics.2 Camptocormia can be a part of Parkinson disease (prevalence: 3%–18%) or associated with various neuromuscular disorders.3 Camptocormia can be fatal due to falls, dyspnea, dysphagia, and deep venous thrombosis.4 Diagnosing and treating this condition early is essential to prevent any severe consequences. Due to the paucity of literature, we present this rare concept with an updated literature review.
Literature Review
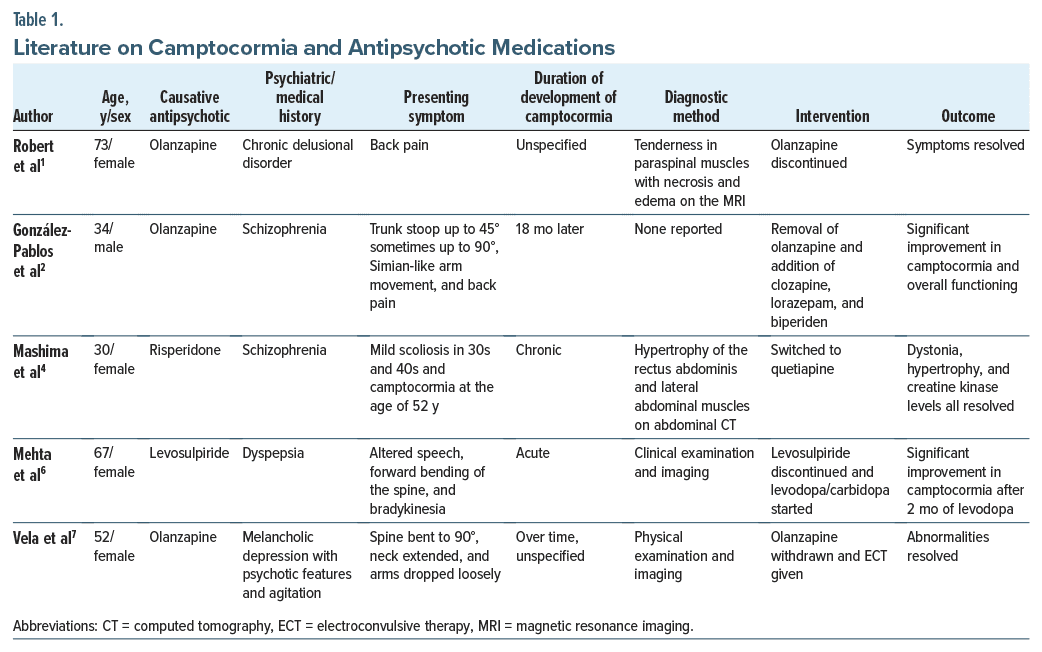
Our literature review (Table 1) shows that camptocormia is a neuromuscular condition and a dystonia spectrum of extrapyramidal syndrome (EPS) resulting from antipsychotic medications.1–7 Dystonic reactions in camptocormia affect the paraspinal and abdominal muscle groups, causing disfigurement. Other complications comprise symptoms worsening on standing and remitting when lying down. Complications include pain, arthritis (if it persists), breathing difficulties, sleep impairment, and difficulty sitting or walking. The condition may arise acutely or chronically. The early signs and symptoms are back pain and tenderness in the paraspinal muscles.1–7 The most implicated antipsychotics associated with camptocormia are risperidone and olanzapine.1–7 Removal of olanzapine and adding clozapine or quetiapine in addition to electroconvulsive therapy are the suggested interventions to address camptocormia.1–7 Evidence points to a disorder in the basal ganglia, with many lines of evidence suggesting the involvement of the dopaminergic system.5 All antipsychotics modulate dopamine, and most can affect the acetylcholine systems.5 Both systems have been implicated in the development of EPS through the nigrostriatal dopaminergic pathway. These drugs block dopamine nigrostriatal tracts along with a relative increase in cholinergic activity.5
Conclusion
It is crucial for clinicians to carefully monitor patients who are undergoing antipsychotic treatment and quickly identify and manage this condition to improve treatment outcomes and patients’ quality of life. More research is required to fully understand the mechanisms and risk factors of this adverse drug reaction.
Article Information
Published Online: May 23, 2024. https://doi.org/10.4088/PCC.23br03678
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(3): 23br03678
Submitted: August 23, 2023; accepted October 19, 2023.
To Cite: Subhedar R, Perugula ML, Shah K, et al. Camptocormia and antipsychotic medications.
Prim Care Companion CNS Disord. 2024;26(3):23br03678.
Author Affiliations: Department of Psychiatry, Bergen New Bridge Medical Centre, Paramus, New Jersey (Subhedar); Department of Psychiatry, Texas Tech University Health Science Center at Odessa/Permian Basin Odessa, Midland, Texas (Perugula, Jain); Department of Psychiatry, Wake Forest University School of Medicine, Winston-Salem, North Carolina (Shah); Department of Psychiatry, Yale University School of Medicine, New Haven, Connecticut (Mansuri).
Corresponding Author: Rashmi Subhedar, MD, Department of Psychiatry, Bergen New Bridge Medical Centre, 8 Danielle Lane, Monroe Township, Paramus, NJ 08831 ([email protected]).
Author Information: Drs Mansuri and Jain share equal credit for the senior authorship.
Relevant Financial Relationships: None.
Funding/Support: None.
References (7)

- Robert F, Koenig M, Robert A, et al. Acute camptocormia induced by olanzapine: a case report. J Med Case Reports. 2010;4:192. PubMed CrossRef
- González-Pablos E, Valles-de la Calle JM, Iglesias Santa Polonia F, et al. A case report of camptocormia coinciding with olanzapine use. J Clin Psychopharmacol. 2016;36(2):183–184. PubMed
- Srivanitchapoom P, Hallett M. Camptocormia in Parkinson’s disease: definition, epidemiology, pathogenesis and treatment modalities. J Neurol Neurosurg Psychiatry. 2016;87(1):75–85. PubMed CrossRef
- Mashima Y, Uchida H, Kinoshita S, et al. Camptocormia secondary to antipsychotic associated dystonia of the rectus abdominis muscles detected by abdominal computed tomography: a case report. J Clin Psychopharmacol. 2021;1(5):608–610.
- Karimi M, Perlmutter JS. The role of dopamine and dopaminergic pathways in dystonia: insights from neuroimaging. Tremor Other Hyperkinet Mov (N Y). 2015;5:280. PubMed CrossRef
- Mehta S, Kumar R, Lal V. An unusual cause of camptocormia. Tremor Other Hyperkinet Mov (N Y). 2019;9:608. PubMed CrossRef
- Vela L, Jiménez Morón D, Sánchez C, et al. Camptocormia induced by atypical antipsychotics and resolved by electroconvulsive therapy. Movement Disord. 2006;21(11):1977–1980. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!