Cyproheptadine, primarily a first-generation antihistaminic with antiserotonergic and anticholinergic properties, is used for the treatment of several allergic conditions.1 Though the most common off-label uses are for appetite stimulation and migraine prophylaxis, it is also used in treating cyclical vomiting syndrome in infants, akathisia, tardive dyskinesia in adults, and insomnia and as an antidote for serotonin syndrome.2 Common side effects include excessive sedation, irritability, anxiety, restlessness, and dizziness, with reports of causing obsessive-compulsive disorders and worsening of depression.2,3
Dexamethasone, a corticosteroid of the glucocorticoid group, possesses potent anti-inflammatory effects and is used in various inflammatory conditions such as multiple sclerosis, rheumatoid arthritis, asthma, and drug hypersensitivity reactions.4 The most frequently reported adverse effect is insomnia, with other common side effects including indigestion, fluid retention, electrolyte imbalances, weight gain, increased appetite, nausea, dyspepsia, and truncal obesity.4 Corticosteroids, including dexamethasone, are known to cause psychiatric disturbances such as anxiety, depression, mood lability, mania, and psychosis.5 Cases of cyproheptadine-only or combined cyproheptadine and dexamethasone dependence or abuse seem to be quite common among individuals aiming for rapid weight gain and muscle development. However, there are very few studies worldwide and only a few case reports in India. Hence, we present 3 cases of this rare dependence to add more to the existing literature. This may help raise awareness among the vulnerable, contribute to further research, and aid clinicians in understanding the clinical picture for early intervention and treatment.
Case Series
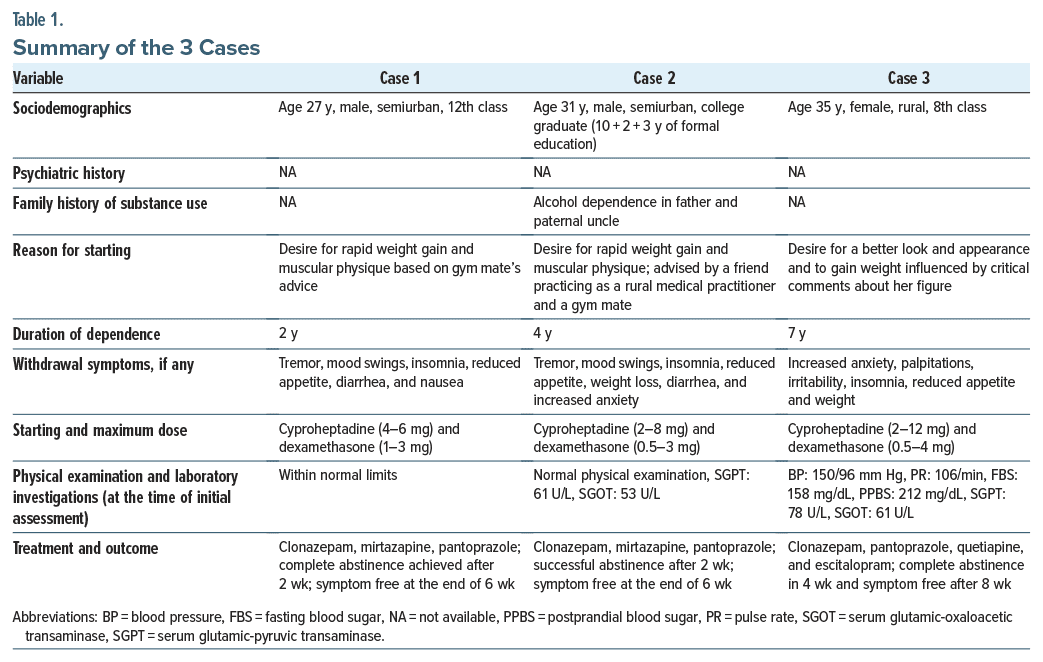
We present 3 cases of cyproheptadine and dexamethasone dependence diagnosed by ICD-10 criteria.6 Two male patients sought outpatient department treatment, and 1 female patient sought emergency psychiatric care at our institute. Case summaries are provided in Table 1.
 Case 1. A 27-year-old man from a semiurban background, educated up to 12th class, was referred to the psychiatry outpatient department due to chronic misuse of cyproheptadine and dexamethasone. Presenting complaints included restlessness, irritability, anxiety, palpitations, and tremors, along with gastrointestinal issues such as dyspepsia, abdominal pain, constipation, and occasional loose stools. The patient had been taking these medications for 2 years, following a gym mate’s advice for rapid weight gain and a muscular physique. Initial dosages were cyproheptadine 4 mg and dexamethasone 1 mg, escalated over time to 6 mg and 3 mg, respectively. Attempts to quit resulted in withdrawal symptoms, prompting psychoeducation and pharmacologic management. Initial physical examination and laboratory investigations were within normal limits. Clonazepam 0.5 mg was prescribed for 1 week alongside pantoprazole 40 mg, and mirtazapine 7.5 mg was prescribed after 1 week due to anxiety and inadequate sleep and was increased to 15 mg/d. Clonazepam was stopped after 2 weeks. Two weeks after beginning treatment, the patient achieved complete abstinence, with mirtazapine continued for 4 more weeks. At the end of 6 weeks, the patient was still abstinent and symptom free.
Case 1. A 27-year-old man from a semiurban background, educated up to 12th class, was referred to the psychiatry outpatient department due to chronic misuse of cyproheptadine and dexamethasone. Presenting complaints included restlessness, irritability, anxiety, palpitations, and tremors, along with gastrointestinal issues such as dyspepsia, abdominal pain, constipation, and occasional loose stools. The patient had been taking these medications for 2 years, following a gym mate’s advice for rapid weight gain and a muscular physique. Initial dosages were cyproheptadine 4 mg and dexamethasone 1 mg, escalated over time to 6 mg and 3 mg, respectively. Attempts to quit resulted in withdrawal symptoms, prompting psychoeducation and pharmacologic management. Initial physical examination and laboratory investigations were within normal limits. Clonazepam 0.5 mg was prescribed for 1 week alongside pantoprazole 40 mg, and mirtazapine 7.5 mg was prescribed after 1 week due to anxiety and inadequate sleep and was increased to 15 mg/d. Clonazepam was stopped after 2 weeks. Two weeks after beginning treatment, the patient achieved complete abstinence, with mirtazapine continued for 4 more weeks. At the end of 6 weeks, the patient was still abstinent and symptom free.
Case 2. A 31-year-old man with a semiurban background, educated up to college graduation (10+2+3 years of formal education) presented with complaints of restlessness, irritability, chronic low mood, anxiety, palpitations, and tremors along with dyspepsia, abdominal pain, and constipation alternating with occasional loose stools. He had a 4-year history of regular cyproheptadine and dexamethasone use, starting at 2 mg and 0.5 mg twice daily, respectively. After a few months, he did not feel as hungry and sleepy as in the initial days of starting the medications; hence, the doses were escalated to 8 mg and 3 mg daily, driven by a desire for more rapid weight gain and a muscular physique. The influence for medication use came from a friend practicing as a quack practitioner in the rural area and from a gym mate. The patient was also a frequent gym goer and reported to have known many people in his gym taking these tablets regularly. Despite initial success with weight gain, the patient encountered issues such as insomnia, loss of appetite, disproportionate abdominal fat accumulation, and subsequent anxiety. Attempts to discontinue the medication resulted in withdrawal symptoms, leading to a relapse. At the time of initial assessment, the physical examination showed no abnormalities, while laboratory results indicated mildly elevated serum glutamic-pyruvic transaminase and serum glutamic oxaloacetic transaminase and alkaline phosphatase levels. Treatment involved psychoeducation. Clonazepam was initially started at 0.5 mg and later increased to 1 mg due to inadequate sleep, in addition to a proton pump inhibitor (PPI). Mirtazapine was added after 1 week to relieve anxiety and depression, starting at 7.5 mg and increased to 15 mg. The patient achieved complete abstinence in 2 weeks. Mirtazapine was tapered off in the next 4 weeks, and clonazepam was tapered off after 2 weeks. He was completely symptom free after 6 weeks.
Case 3. A 35-year-old homemaker, with an education up to the 8th class and residing in a rural area, presented to the psychiatric emergency department with distressing symptoms. She reported experiencing complete insomnia over the past 3 days, accompanied by tremulousness, anxiety, palpitations, dizziness, nausea, and malaise persisting for the last 7 days. The patient disclosed a history of taking cyproheptadine and dexamethasone tablets for the past 7 years, a regimen she recently stopped 10 days prior, as she had travelled from her village to a childhood friend’s house in Kolkata, forgot to bring the medication with her, and could not obtain the medication without a prescription from any pharmacies. Previous attempts to discontinue the medication led to heightened anxiety, insomnia, and weight loss, prompting her to resume its use. The initiation of the medication was influenced by a friend’s suggestion, aiming to enhance her appearance and gain weight in response to critical comments about her figure from her in-laws, husband, and relatives. Commencing with cyproheptadine 2 mg and dexamethasone 0.5 mg tablets twice daily, she gradually increased the doses to 12 mg and 4 mg, respectively. Chronic symptoms included dyspepsia, regurgitation, nausea, frequent diarrhea, cough, and cold, along with persistent fatigue, lack of energy, occasional dizziness, abdominal bloating, and a noticeable disproportion between thin limbs and truncal obesity along with psychiatric symptoms such as depression, anxiety, irritability, and restlessness. At the time of initial assessment, the physical examination revealed hypertension with tachycardia. Initial blood investigations indicated diabetes mellitus, coupled with increased liver enzymes. Treatment initiation involved psychoeducation along with clonazepam 1 mg, supplemented by quetiapine 25 mg due to inadequate sleep and the PPI pantoprazole 40 mg. After 2 weeks, despite improved sleep, anxiety and depressive symptoms persisted, leading to the introduction of escitalopram 10 mg. Over the next 2 weeks, symptomatic improvement allowed for the gradual tapering off of clonazepam and subsequently escitalopram over the following 6 weeks after starting the medicine. Quetiapine was discontinued after 2 weeks of starting treatment. The patient was symptom free after 8 weeks, with improved overall well-being.
Discussion
This cases series highlights the dependence and abuse potential of cyproheptadine and dexamethasone, aligning with existing research.7,8 While adverse effects and withdrawal symptoms are generally mild and manageable on an outpatient basis,7,8 susceptibility to abuse is notably high among those aiming for rapid weight gain and an improved physical appearance. This trend, identified in young individuals, resonates with findings from an African study,9 and cases seem to be common among gym goers as pointed out by case 2, which echoes the finding of a study where individuals treated these drugs as a “gym tonic.”10 It is also possible that individuals may be unaware of the distinction between an anabolic steroid and a corticosteroid, contributing to the misuse. The easy over-the-counter availability from local pharmacies and cheap cost played a role in the abuse of the drugs.
Despite predominantly mild adverse effects, severe reactions such as hypokalemic paralysis10 and withdrawal-induced conditions such as serotonin syndrome11,12 have been reported. Our report underscores the gravity of dependence and withdrawal symptoms, as evidenced by a patient presenting to the emergency department with severe anxiety and insomnia, eventually developing hypertension and diabetes mellitus likely attributable to chronic dexamethasone use. Mirtazapine and escitalopram were started after a washout period of 7 days after stopping cyproheptadine dexamethasone due to reports of unopposed action of serotonin leading to serotonin syndrome after starting serotonergic drugs immediately after stopping the antiserotonergic cyproheptadine.12
Our cases originate from semiurban or rural backgrounds, potentially indicating lower awareness compared to urban settings. Notably, this case series marks the first in India for combined cyproheptadine and dexamethasone dependence, with only one such case report7 and limited existing reports of cyproheptadine abuse,8,10–12 emphasizing the need for increased awareness and vigilance surrounding the misuse of these medications.
Conclusion
In conclusion, more research is warranted due to potential underreporting, particularly in the young rural or semiurban populations frequenting gyms. Easily accessible over-the-counter availability underscores the need for strict regulations for nonprescription drug dispensing. Given their common prescription by rural and family physicians, raising awareness about cyproheptadine and dexamethasone dependence risks, clinical presentations, and management is crucial so that interventions can be done to mitigate long-term adverse consequences.
Article Information
Published Online: December 10, 2024.https://doi.org/10.4088/PCC.24cr03731
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(6):24cr03731
Submitted: February 24, 2024; accepted April 19, 2024.
To Cite: Mukherjee A, Das R, Kumar M, et al. Combined cyproheptadine and dexamethasone dependence: Is it rare or underreported? A case series. Prim Care Companion CNS Disord. 2024;26(6):24cr03731.
Author Affiliations: Department of Psychiatric Epidemiology, Institute of Psychiatry-Centre of Excellence, Institute of Postgraduate Medical Education and Research, Bhowanipore, Kolkata, West Bengal, India (Mukherjee, R. Das); Department of Psychiatric Social Work, Institute of Psychiatry-Centre of Excellence, Institute of Postgraduate Medical Education and Research, Bhowanipore, Kolkata, West Bengal, India (Kumar); Department of Psychiatry, Bankura Sammilani Medical College, Bankura, West Bengal, India (Chakraborty); Somnos Sleep Clinic, Kolkata, West Bengal, India (S. Das).
Corresponding Author: Aritra Chakraborty, MD, Department of Psychiatry, Bankura Sammilani Medical College & Hospital, Lokepur, Kenduadihi, Bankura, West Bengal 722102, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgment: The authors thank the Department of Psychiatry, Institute of Psychiatry-Centre of Excellence, Institute of Postgraduate Medical Education and Research, Kolkata, for referring the cases.
Patient Consent: The patients provided written consent to publish the case reports, and information has been de identified to protect anonymity.
ORCID: Aritra Chakraborty: https://orcid.org/0009-0000-0767-7194
References (12)

- Vardanyan RS, Hruby VJ. Chapter 16-Antihistamine Drugs. Synthesis of Essential Drugs. 2006:219–235.
- Gupta M, Gupta N, Madabushi J. Off-label cyproheptadine in children and adolescents: psychiatric comorbidities, interacting variables, safety, and risks of hepatotoxicity. Cureus. 2023;15(1):e33745. PubMed CrossRef
- Khanam A, Dar SA, Wani ZA. Cyproheptadine hydrochloride and dexamethasone induced de novo obsessive-compulsive symptoms and suicidal attempts: a rare case report. J Med Sci. 2021;41(5):253–255.
- Johnson DB, Lopez MJ, Kelley B. Dexamethasone. [Updated 2023 May 2]. In: StatPearls [Internet]. StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482130/
- Ling MH, Perry PJ, Tsuang MT. Side effects of corticosteroid therapy – psychiatric aspects. Arch Gen Psychiatry. 1981;38(4):471–477. PubMed CrossRef
- World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organization; 1992.
- Karia S, Dave N, De Sousa A, et al. Cyproheptadine and dexamethasone abuse. Natl J Med Res. 2013;3(1):88–89.
- Dewang B, Shah N, Sinha D, et al. Cyroheptadine dependence: a case report. Indian J Ment Health. 2015;2(1).
- Lulebo AM, Bavuidibo CD, Mafuta EM, et al. The misuse of cyproheptadine: a non-communicable disease risk behaviour in Kinshasa population, Democratic Republic of Congo. Subst Abuse Treat Prev Policy. 2016;11:7. PubMed CrossRef
- Bawaskar HS, Bawaskar PH, Bawaskar PH. “Gym tonic” and quadriparesis. J Assoc Physicians India. 2019;67(10):85–86.
- Prakash S, Rathore C. Cyproheptadine-dependent chronic serotonin syndrome. Neurol India. 2016;64(6):1319–1321. PubMed CrossRef
- Bhatia MS, Kaur J, Gautam P. A case of serotonin syndrome following cyproheptadine withdrawal. Prim Care Companion CNS Disord. 2015;17(3):10.4088/ PCC.14l01762. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!


