Abstract
Objective: To investigate the relationship between social isolation and substance abuse among adult hospitalizations to better target prevention and intervention.
Methods: The 2018 National Inpatient Sample dataset was used to identify adult hospitalizations with social isolation and substance abuse in the United States, omitting long-term and rehabilitation facilities. The study analyzed sociodemographic features and health care resource utilization, with primary end points focusing on the prevalence of substance use disorder (SUD) with social isolation and sex/race-based disparities and secondary end points including mental health and costs. Comparisons were analyzed using SPSS Statistics with weighted data and complex survey modules.
Results: The study included 2,050 patients (median age: 48 years, male: 55.6%) with an International Classification of Diseases, Tenth Revision, Clinical Modification social isolation diagnostic code, of which 16.6% had SUD, with higher prevalence in those of younger age, male sex, and black race. Smoking (49.3% vs 36.1%), alcohol disorder (14.4% vs 4.9%), cannabis disorder (14.6% vs 1.4%), stimulant-related disorder (16.3% vs 2.6%), and opioid-related disorder (16.6% vs 3.1%) were the most prevalent SUDs among socially isolated patients. The length of stay was similar among socially isolated patients by substance use; however, hospitalization cost was higher ($6,144 vs $4,745) among patients with SUD.
Conclusion: The link between social isolation and substance use highlights the significance of addressing social isolation as a public health issue. Interventions to nurture social ties and reduce social isolation may have significant potential in preventing and managing SUDs.
Prim Care Companion CNS Disord 2024;26(5):23m03679
Author affiliations are listed at the end of this article.
The National Survey on Drug Use and Health estimated that 20.4 million people in the United States were diagnosed with substance use disorder (SUD) in 2019.1 The environmental, physiological, and psychosocial causes of SUD are multifaceted, and understanding their interplay is critical for prevention and treatment. A growing body of evidence identifies psychosocial factors such as loneliness, anxiety, low self-esteem, and negative interpersonal relationships as significant risk factors for developing SUD.2 In addition, substance abuse can be a way to address emotionally dysphoric experiences, like social rejection, and a way to cope with loneliness.3 As social creatures, we universally need to belong. Conceptualized broadly, belongingness is a deeply rooted human behavior underpinned by ancestral origins with corollaries to various physiological and psychological implications.4,5 Lack of belonging reveals a spectrum of behavior motivated by the need to establish and preserve healthy interpersonal bonds to ease emotional suffering.6 The social rejection or unfavorable interpersonal interaction that distances one from others, termed social exclusion,7 is an emotionally dysphoric experience.6,8 A growing body of research suggests that acute social exclusion or loss, also termed social pain, evokes the same neural circuitry as physical pain.9 In line with the pain overlap theory, μ-opioid–related drugs like morphine reduce vocalized separation anxiety,10 acetaminophen reduces reactivity to a social exclusion manipulation,8 and alcohol reduces acute social pain.11 The belonging and pain overlap theory may contextualize the relationship between chronic social exclusion and substance abuse. However, more research is needed to highlight this relationship and guide future prevention and treatment. To that end, the objective of this study was to investigate the intersection between social isolation and substance abuse among adult hospitalizations.
METHODS
To identify adult hospitalizations with social isolation and concomitant substance abuse, we used the 2018 National Inpatient Sample (NIS). In the United States, the NIS is a publicly accessible dataset that is part of the Healthcare Cost and Utilization Project (HCUP), which the agency funds for the Agency for Healthcare Research and Quality.12 Weighted NIS data comprise about 35 million yearly in-hospital interactions from over 1,000 nonfederal acute care hospital centers in 45 states, omitting long term acute care and rehabilitation facilities. Weighted data represent over 95% of community hospitalizations in the United States. Because the NIS does not divulge patients’ identifiers, no institutional review board permission was required for this study.
For inpatient encounters with social isolation and substance abuse, we used International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnostic code Z60.4 and revised Clinical Classifications Software Refined codes, respectively.13 Sociodemographic features, including age at admission, sex, race/ethnicity, payer status, median household income, and hospitalization characteristics, including hospital location/teaching status and regions, were compared in socially isolated adults hospitalized with versus without substance abuse. Substance abuse studied included cannabis use disorder, alcohol use disorder, stimulant use disorder, opioid use disorder, and tobacco use disorder.
The primary end points were the prevalence of substance abuse with versus without social isolation and sex/race-based disparities and the burden of mental health disorders, including anxiety, depression, psychoses, and bipolar disorders in socially isolated adults with versus without substance abuse. Secondary end points included health care resource utilization (disposition of patients, length of stay, and cost).
We used weighted data and complex survey modules with SPSS Statistics version 25.0 (IBM Corporation, Armonk, New York) for all analyses. We used Pearson χ2 test for categorical measures and the Mann-Whitney U test for continuous variables. A P value <.05 was considered the threshold for statistical significance. Cell sizes less than 11 were not reported per the privacy guidelines of the HCUP.12
RESULTS
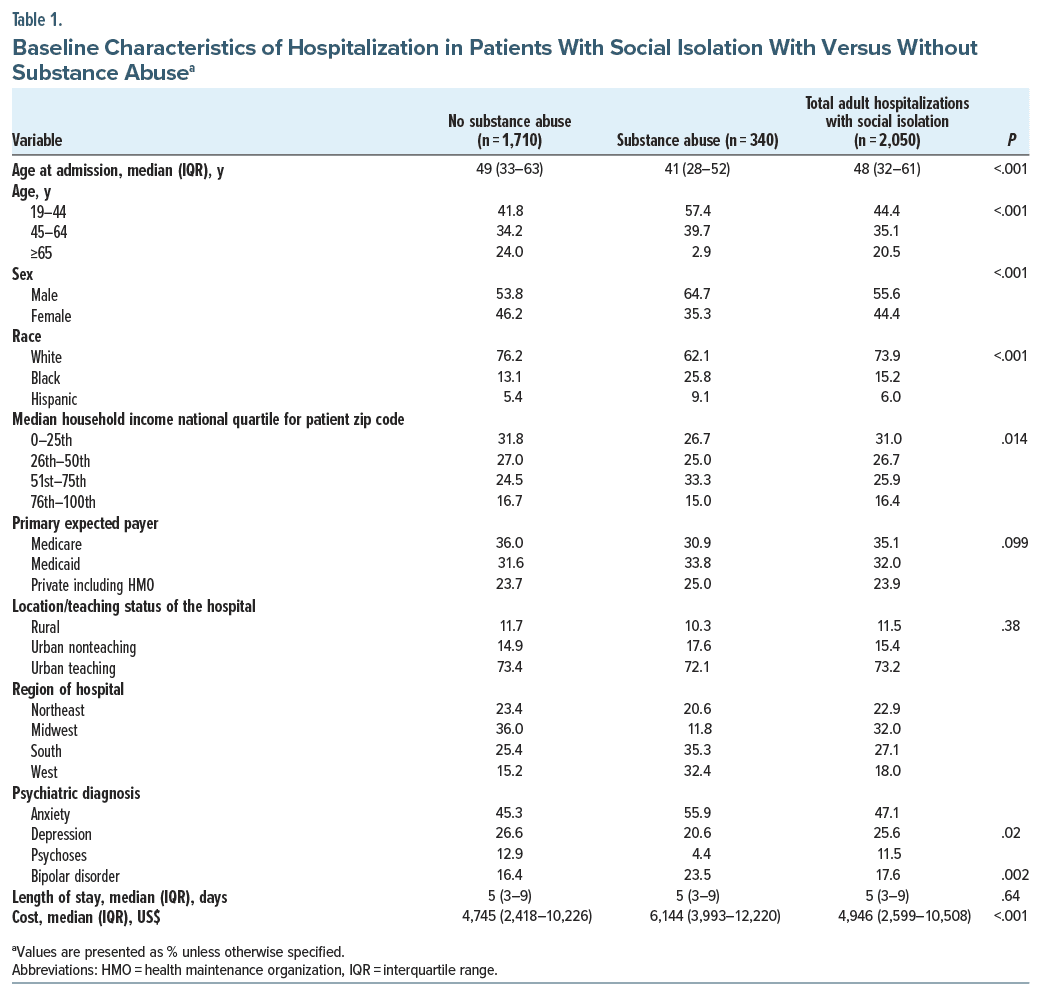
The study included 2,050 patients (median age: 48 years and male: 55.6%) with social isolation diagnostic codes. The baseline characteristics of the study population are presented in Table 1, stratified by substance use. Of the 2,050 patients, 340 (16.6%) were between the ages of 19 and 44 years (57.4% vs 41.8%) and were using substances. Prevalence of substance use was higher among males (64.7% vs 53.8%) and in the black race (25.8% vs 13.1%). There was no significant difference in the prevalence of substance use by median household income; however, it was statistically significant with those in the 51st–75th quartile. Prevalence of substance use among those with social isolation did not differ by location/teaching status of the hospital or primary payer. Regionally, substance use was higher among socially isolated patients in the southern and western United States. Prevalence of bipolar disorder (23.5% vs 16.4%) and anxiety disorder (55.9% vs 45.3%) was high among socially isolated patients with substance abuse. Surprisingly, we observed a lower prevalence of depression and psychosis among those with substance use. Length of stay was similar among socially isolated patients by substance use (smoking, alcohol use disorder, cannabis use disorder, and stimulant- and opioid-related disorder). The cost of hospitalization was higher among socially isolated patients with substance use.
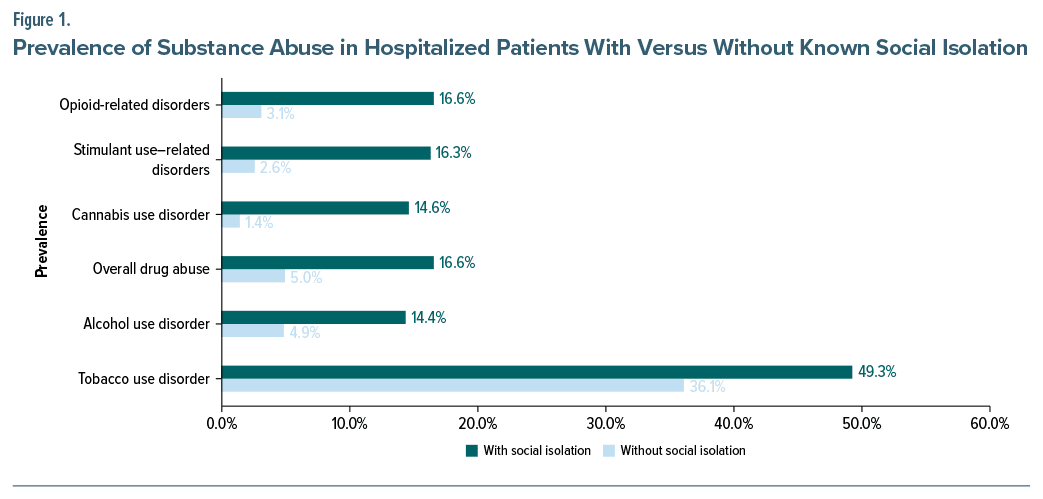
Figure 1 shows the prevalence of substance use among patients with and without social isolation. Prevalence of smoking, alcohol use disorder, cannabis use disorder, and stimulant- and opioid-related disorders was high in patients with social isolation. For example, the prevalence of smoking was 49.3% vs 36.1%, and alcohol abuse was prevalent among 14.4% vs 4.9% of patients. Cannabis use disorder was also high among patients with social isolation (14.6% vs 1.4%).
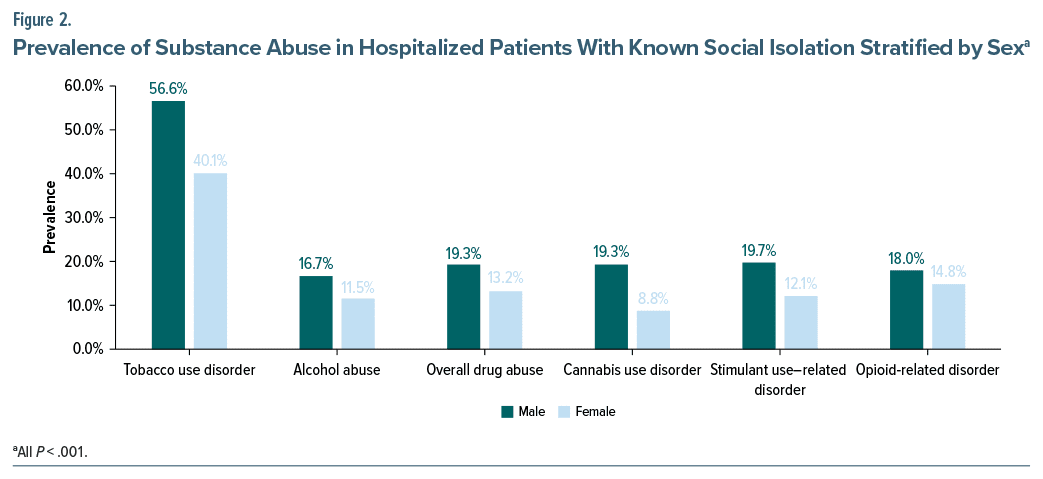
When the prevalence of substance use among patients with social isolation was stratified by sex, all SUDs showed a higher prevalence among males compared to females as shown in Figure 2. For example, smoking prevalence was 56.6% vs 40.1%, alcohol use disorder was 16.7% vs 11.5%, cannabis use disorder was 19.3% vs 8.8%, stimulant use disorder was 19.7% vs 12.1%, and opioid-related disorders were 18.0% vs 14.8%.
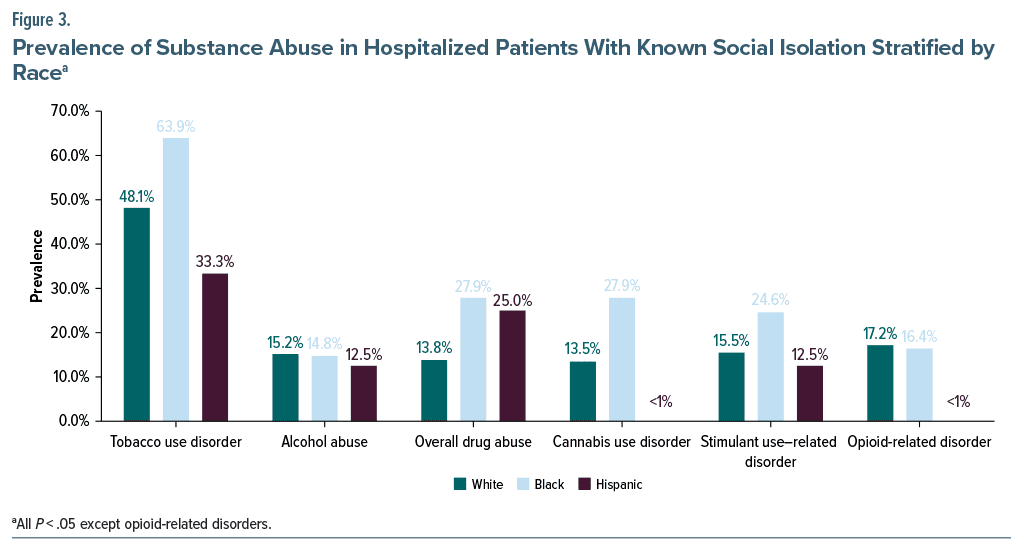
On further classification of SUD by race (Figure 3), smoking (48.1% vs 63.9% vs 33.3%), cannabis use disorder (13.5% vs 27.9% vs <1%), simulant use disorder (15.5% vs 24.6% vs 12.5%), and opioid-related disorder (17.2% vs 16.4% vs <1%) showed higher prevalence among the black race compared to white and Hispanic races. We observed no major differences for alcohol abuse (15.2% vs 14.8% vs 12.5%).
DISCUSSION
Our research examined the association between concurrent substance misuse and social isolation among adult hospitalizations. We also looked at sociodemographic variables of sex, race, payer status, median household income, and hospitalization characteristics. Socially isolated patients had substantially higher rates of substance abuse. We observed these higher rates in cannabis use disorder, alcohol use disorder, opioid-related disorders, stimulant-related disorders, and smoking. Previous research infers similar results in that there is a correlation between loneliness and stigma-based exclusion with reported substance abuse.14 Wesselmann and Parris14 connect trauma with an increase in reports of substance abuse and present social isolation as a trauma linking the two. However, there is a lack of research showing data looking at a direct correlation between social isolation and substance abuse. Alcohol abuse, more so than other substances, has been the center of many studies. Preliminary evidence has shown ostracism to increase alcohol consumption.15 When aimed at vulnerable groups, ostracism research may provide a target for prevention and intervention strategies.15 Our research bridges that gap by looking at a more inclusive dataset regarding substance abuse. We hope our findings will spark more interest in studying targeted prevention and intervention.
Social isolation may not only contribute to the onset or exacerbation of SUD but could also significantly impact various aspects of health care. Individuals experiencing social isolation may face challenges in seeking timely care for chronic conditions, potentially leading to delayed hospitalization. Furthermore, the severity of illness at the time of hospitalization might be influenced by the lack of a support system. The length of hospital stay could also be prolonged due to the absence of family support for post-discharge assistance. These factors, in turn, contribute to increased health care costs. While the lack of clarity regarding the precise mechanisms at play may be frustrating, it underscores the importance of further investigations. Exploring these intricate connections could not only enhance the care for individuals with SUD but also provide insights into therapeutic interventions to address the impact of isolation and loneliness on overall health outcomes.
Our data show a positive correlation between substance abuse and social isolation. By examining this correlation across different sociodemographic variables, we investigate this correlation more thoroughly. For both men and black Americans, we discovered a higher frequency of substance usage. McClendon et al16 found that the likelihood of stress- and age-related diseases was higher and that they manifested earlier among black Americans compared to their white counterparts. The research also confirmed that compared to white adults, black adults are more likely to feel stress and social isolation.16
Although our results show that the length of stay was similar among socially isolated patients with substance abuse, the cost of hospitalization was higher among those who were socially isolated. We found the severity of the illness to be a significant determinant of hospital costs.17 Our findings question whether social isolation plays a part in the severity of substance abuse and its physiological effects. Previous research has shown that patients with lower social support had a higher severity of alcohol and drug abuse.18 Social support and family cohesion have been positively associated with patients’ quality of life.19 Improving social support and connections, especially with families, had beneficial physiological and psychological effects.20 Focusing on social help for those in the hospital may improve patients’ quality of life and their hospitalization costs.
LIMITATIONS
The study’s cross-sectional design provides only a single snapshot of the association being investigated. Although the survey identified appropriate ICD codes for all variables related to the topic, there may still be incomplete capturing of variables in the dataset, making it a limiting factor for regression analysis. Patient visits are recorded instead of specific patients, raising the possibility of duplicate counting. It is also impossible to verify individual ICD codes in the dataset. Finally, the absence of information on current medication or duration of illness may be an important factor that we could not assess through the dataset.
CONCLUSIONS
In conclusion, this study highlights an important connection between social isolation and SUD, emphasizing the need to address social isolation as a public health issue. The higher prevalence of SUD among socially isolated individuals, along with the associated health care costs, underscores the importance of targeted strategies for those who are socially isolated. As clinicians, it is imperative to integrate interventions that promote social connections into clinical practice, such as community-based programs, to effectively prevent and manage SUD by addressing the underlying issue of social isolation.
Article Information
Published Online: September 24, 2024. https://doi.org/10.4088/PCC.23m03679
© 2024 Physicians Postgraduate Press, Inc.
Submitted: December 1, 2023; accepted May 14, 2024.
To Cite: Desai R, Karim S, Freeborn J, et al. Contextualizing the relationship between social isolation and substance abuse. Prim Care Companion CNS Disord. 2024;26(5):23m03679.
Author Affiliation: Department of Psychiatry, Texas Tech University Health Science Center, Midland, Texas.
Corresponding Author: Chintan Trivedi, MD, MPH, Department of Psychiatry, Texas Tech University Health Science Center, 2301 W Michigan Ave, Midland, TX 79701 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Socially isolated patients had substantially higher rates of substance abuse.
- Cannabis use disorder, alcohol abuse, opioid-related disorders, stimulant-related disorders, and smoking were the most prevalent substance use disorders among socially isolated patients.
- Focusing on social help for those in the hospital may improve patients’ quality of life and their hospitalization costs.
References (20)

- NSDUH. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. 2020. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf10
- Trucco EM. A review of psychosocial factors linked to adolescent substance use. Pharmacol Biochem Behav. 2020;196:172969. PubMed CrossRef
- Hosseinbor M, Yassini Ardekani SM, Bakhshani S, et al. Emotional and social loneliness in individuals with and without substance dependence disorder. Int J High Risk Behav Addict. 2014;3(3):e22688. PubMed CrossRef
- Allen KA, Gray DL, Baumeister RF, et al. The need to belong: a deep dive into the origins, implications, and future of a foundational construct. Educ Psychol Rev. 2022;34(2):1133–1156. PubMed CrossRef
- Allen KA, Kern ML, Rozek CS, et al. Belonging: a review of conceptual issues, an integrative framework, and directions for future research. Aust J Psychol. 2021;73(1):87–102. PubMed CrossRef
- Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117(3):497–529. PubMed CrossRef
- Riva P, Montali L, Wirth JH, et al. Chronic social exclusion and evidence for the resignation stage: an empirical investigation. J Social Personal Relat. 2017;34(4):541–564. CrossRef
- Dewall CN, Deckman T, Pond RS, et al. Belongingness as a core personality trait: how social exclusion influences social functioning and personality expression. J Pers. 2011;79(6):1281–1314. PubMed CrossRef
- Eisenberger NI. Broken hearts and broken bones: a neural perspective on the similarities between social and physical pain. Curr Dir Psychol Sci. 2012;21(1):42–47. CrossRef
- Panksepp J. Affective Neuroscience: The Foundations of Human and Animal Emotions. 1998. https://academic.oup.com/book/5353411
- Hales A, Williams K, Eckhardt C. A participant walks into a bar. Social Psychol. 2015;46. CrossRef
- Publishing with HCUP Data. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; 2022. Accessed May 16, 2022. https://hcup-us.ahrq.gov/db/publishing.jsp
- Clinical Classifications Software Refined (CCSR). Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality; 2021. Accessed February 20, 2022. https://hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp
- Wesselmann ED, Parris L. Exploring the links between social exclusion and substance use, misuse, and addiction. Front Psychol. 2021;12:674743. PubMed CrossRef
- Bacon AK, Engerman B. Excluded, then inebriated: a preliminary investigation into the role of ostracism on alcohol consumption. Addict Behav Rep. 2018;8:25–32. PubMed CrossRef
- McClendon J, Chang K, Boudreaux MJ, et al. Black-White racial health disparities in inflammation and physical health: cumulative stress, social isolation, and health behaviors. Psychoneuroendocrinology. 2021;131:105251. PubMed CrossRef
- Averill RF, McGuire TE, Manning BE, et al. A study of the relationship between severity of illness and hospital cost in New Jersey hospitals. Health Serv Res. 1992;27(5):587–606; discussion 607–612. PubMed
- Dobkin PL, De CM, Paraherakis A, et al. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97(3):347–356. PubMed CrossRef
- Birkeland B, Weimand B, Ruud T, et al. Perceived family cohesion, social support, and quality of life in patients undergoing treatment for substance use disorders compared with patients with mental and physical disorders. Addict Sci Clin Pract. 2021;16(1):44. PubMed CrossRef
- Cacioppo JT, Ernst JM, Burleson MH, et al. Lonely traits and concomitant physiological processes: the MacArthur social neuroscience studies. Int J Psychophysiol. 2000;35(2–3):143–154. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!