Abstract
Introduction: Mental health of health care workers (HCWs) was affected during the COVID-19 pandemic due to direct handling of suspected and confirmed cases. While neurobiological mechanisms that mediate stress, depression, and anxiety are well established, psychological mechanisms are not.
Objective: To assess (1) the prevalence of anxiety, depression, insomnia, and perceived stress among accredited social health activists, multipurpose health workers, auxiliary nurse midwives, and other certified HCWs of rural areas of Telangana, India and (2) the factors that mediate stress with depression and anxiety.
Methods: A total of 300 HCWs from across 10 primary health centers across 5 districts were selected. All participants self-reported their anxiety, depression, sleep problems, and perceived stress related to the pandemic. Sociodemographic and other relevant data pertinent to the context of stress and the pandemic were also obtained. The survey used translated and validated self report instruments and was conducted during August and September 2021.
Results: The mean (SD) scores on the Insomnia Severity Index, 7-item Generalized Anxiety Disorder scale, Pandemic-Related Perceived Stress Scale of COVID-19, and 9-item Patient Health Questionnaire were 5.94 (5.6), 4.21 (4.5), 21.94 (5.8), and 3.89 (4.8), respectively. Age <35 years and family members being COVID-19 positive were significant predictors of depression and anxiety, respectively. Greater number of family members and COVID-19–positive status were significant predictors of insomnia. While the effect of stress on anxiety was indirect through the mediation of insomnia and depression, the effect of stress on depression was direct as well as through the mediation of anxiety.
Conclusion: The study results highlight the importance of measures to address sleep-related issues in individuals who are experiencing psychosocial stressors to prevent the development of depression and anxiety.
Prim Care Companion CNS Disord 2025;27(1):24m03723
Author affiliations are listed at the end of this article.
The COVID-19 pandemic, which started in early 2020, had a massive impact on day-to-day activities worldwide. The pandemic ushered in not only anxiety related to acquiring the infection but also significant changes in the way we lived our lives. The measures taken to contain the infection such as lockdowns, isolation, and quarantine were a first-time experience for most of us, which led to disproportionate levels of stress.1
Several studies have reported a higher incidence of psychiatric symptoms following COVID-19 infection. Around 35%–45% of patients admitted with COVID-19 infection developed symptoms of depression and anxiety per 1 study.2 In addition to psychosocial factors, there is a biological underpinning as well for the development of psychiatric issues. The cytokine storm syndrome that occurs in patients with COVID-19 impacts brain functions,3 and interleukin-1β was found to be higher in COVID-19 patients who developed depression and anxiety compared to those who did not.2
However, just as those who acquired COVID-19 went through mental health issues, others who did not acquire COVID-19 infection experienced them as well. The general public was affected significantly due to the overall restrictions that were imposed by governments across the globe to contain the spread of infection. Measures such as lockdown significantly restricted the movement of people, which led to reduced opportunities for recreational activities. Other measures such as work from home also reduced the interactions that would have occurred in the workplace between colleagues, thereby damaging the social support system. Another factor relates to the coverage by the media, which increased the fear of contracting the infection and led to significant stress among the general public. One meta-analysis found that the prevalence of anxiety and depression among the general public during the pandemic was between 30% and 35%.4
The pandemic had an even more significant effect on the mental health of health care workers (HCWs). HCWs were constantly dealing with confirmed and suspected cases of COVID-19, putting them at risk of acquiring the infection, as well as the stress of spreading the infection to their family members. To prevent such mishaps, HCWs had to undergo compulsory isolations after working with COVID 19–positive patients, but again isolation is a factor that increases the stress. Among HCWs working during the COVID pandemic, emotional exhaustion, depression, anxiety, and hopelessness were commonly seen.5
The neurobiological basis for stress and anxiety/ depression is well established, but the psychological mechanism that mediates them is not well understood. There are studies that have proposed disturbed sleep as one of the factors that mediate stress and depression.
There are some studies conducted among frontline HCWs such as doctors and nurses,6 but almost no studies have assessed the impact of COVID on grassroot-level HCWs working in rural settings. The objective of this study was to assess the prevalence of anxiety, depression, insomnia, and perceived stress among accredited social health activists (ASHAs), multipurpose health workers (MPHWs), auxiliary nurse midwives (ANMs), and other certified HCWs in rural areas of Telangana, India.
METHODS
The current study is part of the larger UNICEF sponsored project titled “Mental health assessment of grassroot-level workers during the COVID-19 pandemic in rural Telangana,” which was a cross-sectional survey of a sample of 300 rural HCWs. The survey used translated and validated self-report instruments and was conducted during August and September 2021. Participants were included in the study after written informed consent was obtained.
Sample Size
The sample size of 300 was calculated based on the pooled prevalence of anxiety, depression, and insomnia of 23.2%, 22.8%, and 38.9% reported among the frontline health care providers in a meta-analysis. Therefore, for reporting an average of 25% of anxiety, depression, and insomnia with 95% CI and 20% relative margin of error (ie, 5%), an estimated 300 samples will be required.
Sample
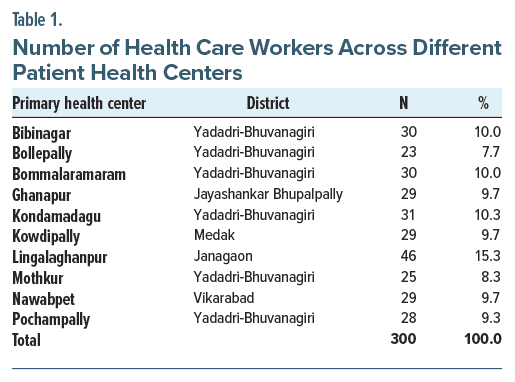
Ten primary health centers (PHCs) across 5 districts were selected. A total of 300 HCWs from those 10 PHCs were included in the study (Table 1). The districts and the PHCs were selected using convenience sampling. All HCWs belonging to any of the 3 cadres (ASHA, MPHW, and ANM) and other certified HCWs in each of the 10 PHCs were eligible for the study. Data from all available participants on the day of assessment were included. All the HCWs included in the study were currently employed and were involved in various community services such as maternal and child health and infectious diseases.
Instruments
The 7-item Generalized Anxiety Disorder (GAD-7) scale,7 the 9-item Patient Health Questionnaire (PHQ 9),8 and the Insomnia Severity Index (ISI)9 were used to assess anxiety, depression, and insomnia. Additionally, the COVID-19 Pandemic-Related Perceived Stress Scale (PSS-10-C)10 was used to assess perceived stress related to the pandemic. All assessment tools were self-report questionnaires, and Telugu-translated versions were used. While Telugu versions of the GAD-7 and PHQ 9 were available as an open source (https://www.phqscreeners.com/select-screener/), the ISI and PSS-10-C were translated and validated as part of the present study.11,12 Pandemic-related and sociodemographic data were collected using semistructured proforma.
Procedure
All participants were invited by telephone or in person by the medical officer in charge of the respective PHCs in the previous 2 weeks to participate on a predecided date. On the specified date, 4 investigators (2 psychiatrists, a junior resident, and a psychiatric nurse) conducted the assessments. The study was explained, and instructions for responding to the self-report questionnaires were provided to all participants. Each of the 4 investigators then had one-to-one and face-to face interaction with the participants for the informed consent process and administration of the self-report tools. Sociodemographic and other relevant data pertinent to the context of stress and the pandemic were also obtained.
Analysis
The sample characteristics were assessed using descriptive measures frequencies and mean (SD). Chi square test was used to assess the univariate association between demographic variables and positive screened status on depression, anxiety, insomnia, and perceived stress. To test for multivariate association, a multinomial logistic regression model was used. A mediation regression analysis was used to assess the mediation models explaining the association between perceived stress, insomnia, depression, and anxiety. The demographic predictors were added as covariates to the model. Analysis was conducted using the Statistical Package for Social Sciences (SPSS) Version 23. PROCESS v.4.0 macro for the SPSS version was used for mediation analysis.
RESULTS
Sample Characteristics
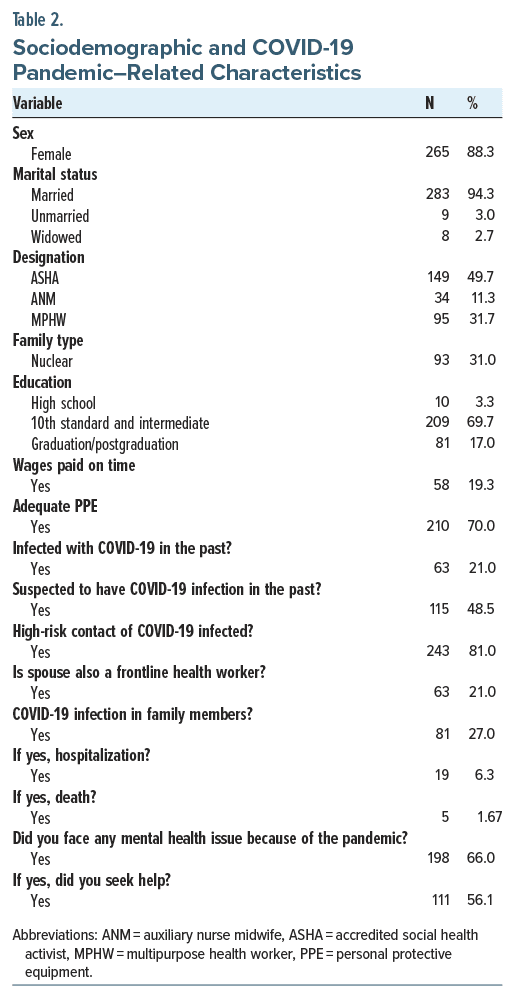
Table 1 shows the number of HCWs included from each of the 10 selected PHCs. Of the 300 participants, the majority were ASHA workers, female, married, and educated at least to matriculation. While 21% of the sample was infected with COVID-19 in the past, 81% had high-risk contact with COVID-19–infected individuals. Table 2 shows sociodemographic and pandemic-related characteristics.
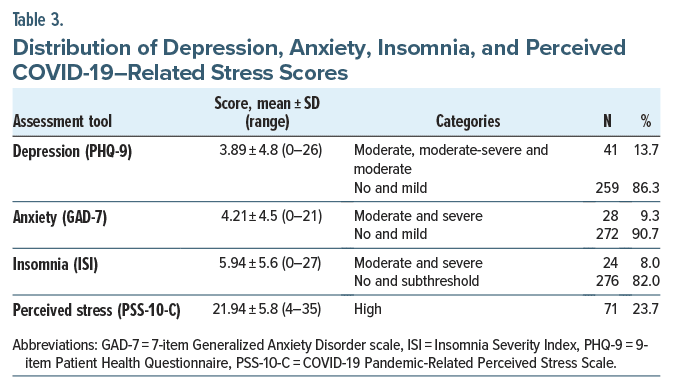
Depression, anxiety, insomnia, and perceived COVID 19–related stress. The mean (SD) score of the PHQ-9 was 3.89 (4.8). On the PHQ-9, 13.78% scored moderate and above levels of depression. The mean (SD) score on the GAD-7 was 4.21 (4.5), and 9.4% had moderate to severe scores on the GAD-7. The mean (SD) score on the ISI was 5.94 (5.6), and 8% had moderate to severe insomnia. The mean (SD) score on the PSS-10-C was 21.94 (5.8), and 23.7% had high levels of perceived stress (Table 3).
Univariate Associations
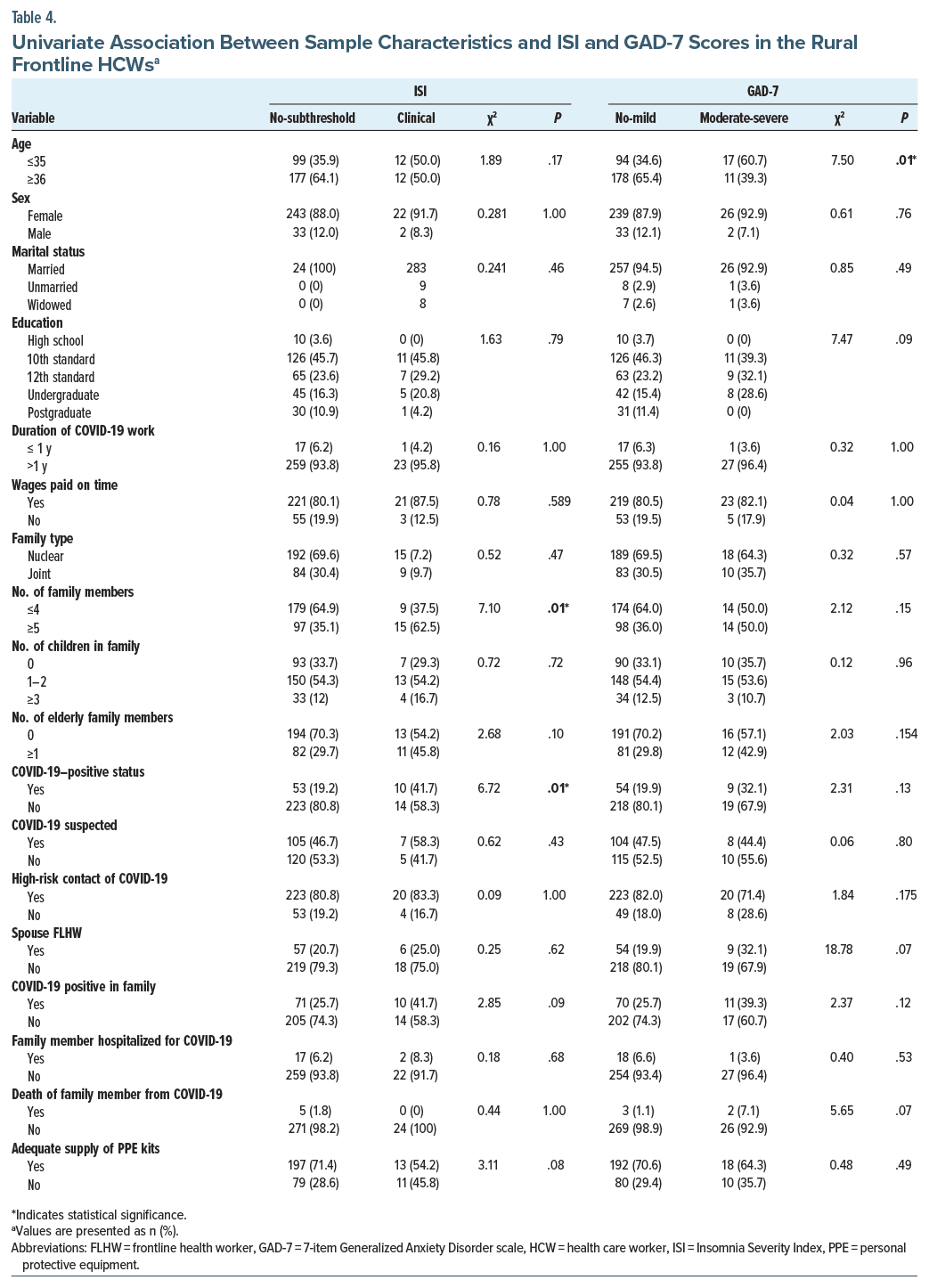
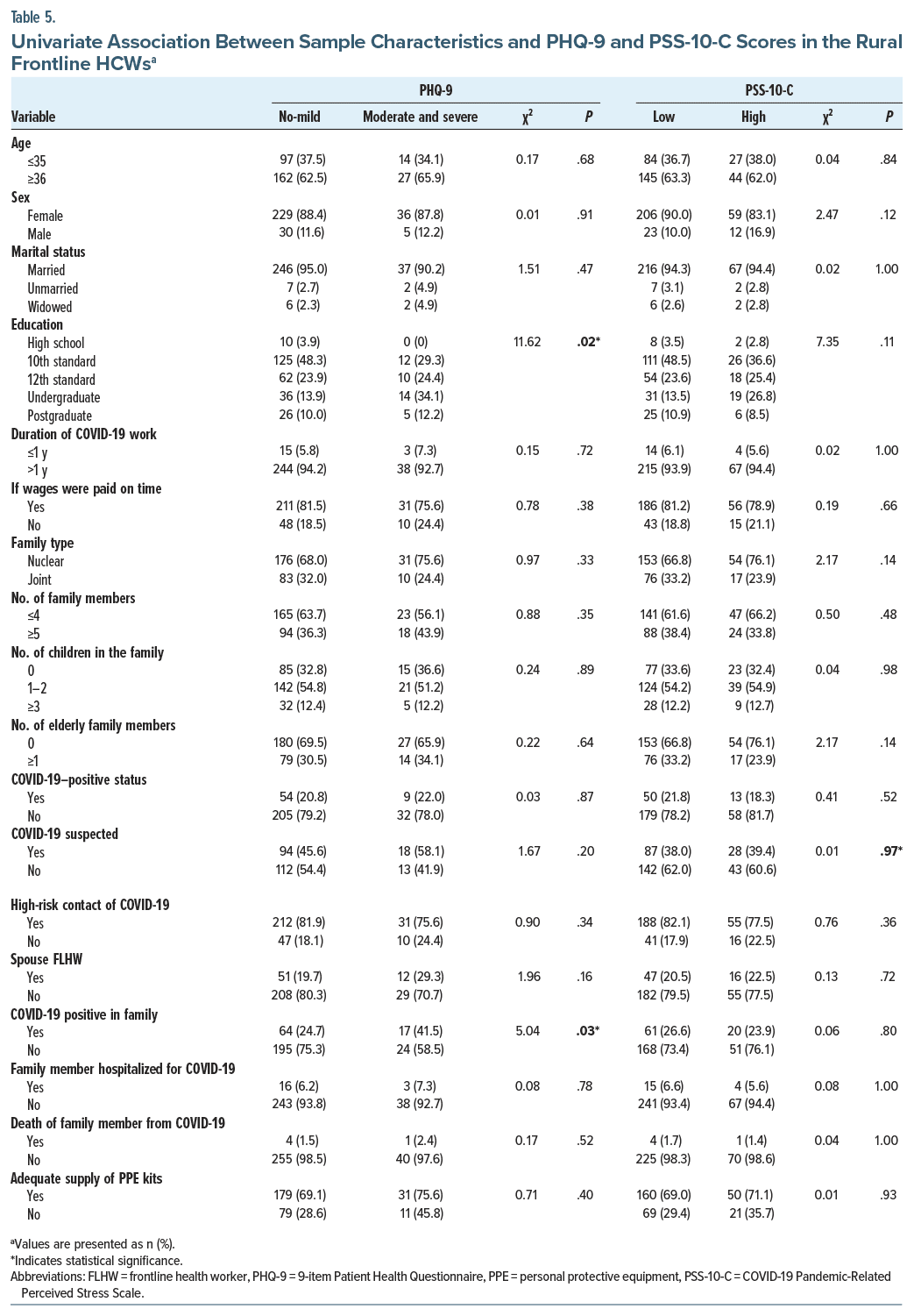
Tables 4 and 5 show univariate associations between demographic and COVID-19–related variables and scores of depression, anxiety, insomnia, and perceived stress. While lower age showed a significant association with moderate and severe anxiety, education of matriculation or lower showed a significant association with no/mild depression. COVID-19–positive status and having a COVID-19–positive family member had positive associations with moderate to severe insomnia and depression respectively.
Multivariate Analysis
The independent variables found to be statistically significant (P < .05) in the univariate analysis were selected and input in the multinomial logistic regression model. While age >35 (B = 1.074; χ2 = 7.151; P = .007) and family members being COVID-19 positive (B = 0.769; χ2 = 4.688; P = .03) were significant predictors of depression and anxiety, respectively, greater number of family members (B = 1.164; χ2 = 7.082; P = .008) and COVID-19–positive status (B = 1.149; χ2 = 6.057; P = .014) were shown to be significant predictors of insomnia in the multinomial regression model. While insomnia was a predictor of anxiety and depression (B = 3.246; χ2 = 34.646; P = <.001), depression was found to be a significant predictor of anxiety (B = 1.45; χ2 = 6.241; P = .011).
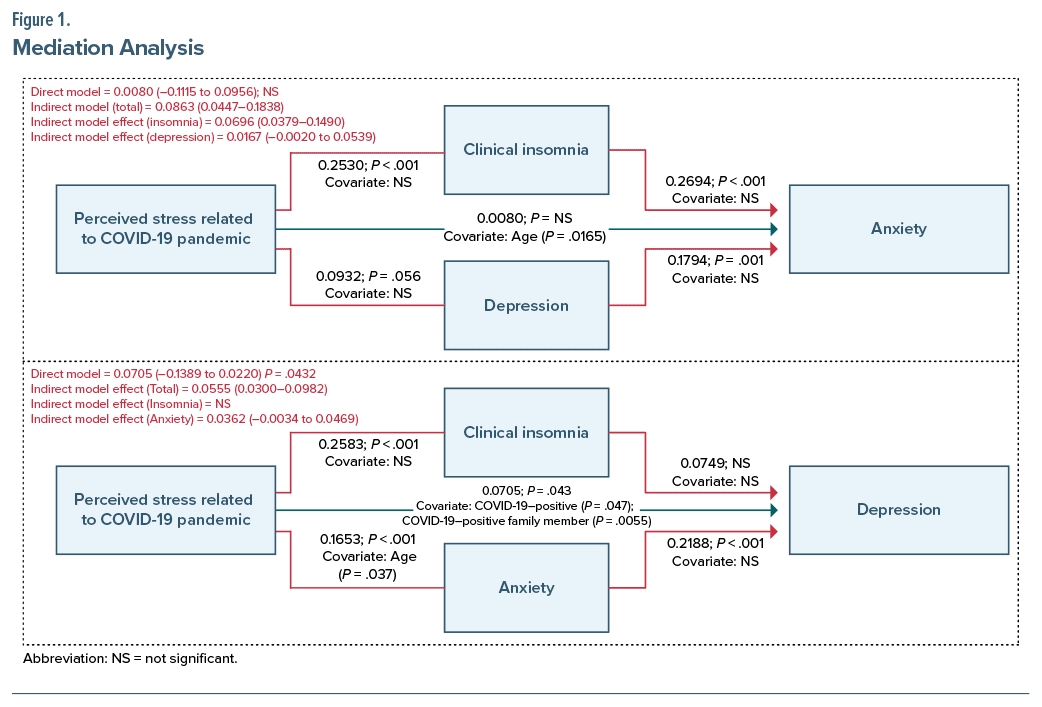
Mediation Analysis
The results of the mediation analysis are shown in Figure 1. While the direct model was statistically significant for depression as an outcome of perceived stress, it was not statistically significant for anxiety as an outcome. COVID-19–positive status for self or for a family member significantly influenced the direct effect of perceived stress on depression. For anxiety as an outcome, the indirect models with insomnia and depression as mediators were statistically significant; no covariates were significantly associated. For depression as an outcome, the indirect model with depression as a mediator was statistically significant; age as a covariate had a significant influence on this association. The indirect model with insomnia as a mediator was not significant. In summary, while the effect of perceived stress on anxiety was indirect through the mediation of insomnia and depression, the effect of stress on depression was direct as well as through the mediation of anxiety.
DISCUSSION
The study of the prevalence of common mental disorders in frontline HCWs during the COVID-19 pandemic is important. We found that depression, anxiety, stress, and insomnia were prevalent in rural HCWs of Telangana. Lower age, higher education, COVID-19–positive or suspected status, and family members being COVID-19 positive were significant predictors of common mental disorders. We found that the effect of stress on depression and anxiety was mediated by insomnia.
The prevalence of anxiety and depression in our study was 9.3% and 13.7%, respectively, which was significantly lower than that found in the meta-analysis by Pappa et al,13 which was done with HCWs during the COVID-19 pandemic. The sample in the meta-analysis by Pappa et al13 consisted of doctors, nurses, or others, but in our study, it consisted exclusively of grassroot HCWs such as ASHAs, MPHWs, and ANMs. This might explain the lower rates of anxiety, as the sample in our study was not involved in the direct handling of the confirmed COVID-19 cases. A study done with ASHA workers in India during the latter part of the first wave of COVID-19 (November 2020) found prevalence of anxiety, depression, or stress to be 56.5%.14 This prevalence is higher than ours because that study included even those with lower threshold symptoms.14 In addition, most of the studies conducted during the peak of the COVID-19 pandemic employed online surveys and found higher rates of anxiety/depression/stress.15 In contrast, our study was conducted after the second wave of COVID-19 and utilized face-to-face interviews, which explains the lower rates of stress, anxiety, and depression.
Age was one of the significant predictors of anxiety in our study, with those aged <35 years having higher anxiety scores compared to those aged >35 years. A similar correlation with age was also observed during the severe acute respiratory syndrome pandemic in 2007.16 Studies from Canada and Spain have also reported similar findings even during the COVID-19 pandemic.17–19 The reason behind this could be that the young people had more access to COVID-19–related news through social media platforms, thereby increasing their stress and anxiety levels. In our study, higher scores on the ISI were associated with bigger family size and COVID-19–positive status of the subject. This finding is due to overcrowded households, which might lead to lower privacy and increased sleep disturbances. COVID-19–positive status would have increased stress levels, thereby leading to increased sleep disturbances.
Multiple studies have established a bidirectional relationship between stress and anxiety/depression.20 Chronic stress leads to changes in basolateral amygdala, thereby dysregulating glutamate release in basolateral amygdala to prefrontal cortex synapse.21 There is enough evidence about neurobiological factors that mediate stress and anxiety/depression, but the studies that have explored psychological factors are sparse. Manzar et al22 conducted a study to understand the mediating effect of insomnia between stress and anxiety and found that insomnia mediates stress and anxiety similar to the finding of our study. Another study by Liu et al23 also established the mediating effect of insomnia between stress and depression. However, in our study, insomnia did not have a mediating effect between stress and depression. The above 2 studies22,23 did not assess the direct relationship between stress and anxiety/ depression. When this was assessed in our study, we found that there is a direct relationship between stress and depression. We also found that anxiety acts as a mediating factor between stress and depression. We did not find a direct relationship between stress and anxiety or a mediating influence of depression on the effect of stress on anxiety. This point highlights the possibility that the stress, apart from causing depression, directly also causes depression through anxiety, which in turn is mediated by insomnia. These findings suggest that strategies aimed at improving the sleep cycle and maintaining regular sleep might be helpful to combat the incidence of anxiety and depression.
Limitations
Restriction of the study sites to only 10 PHCs (samples conveniently based on willingness to participate and available resources) and lack of participation from many other districts where the rates of COVID-19 infection were high are major limitations of our study. The fact that the data were collected during the phase of declining infection rates of the pandemic might have inclined the findings toward lower rates of common mental disorders. The rates might have been different during the peak phases of the pandemic. The mediating effect of insomnia is best established when the subjects are followed up longitudinally from the point of development of stress to the point of insomnia and then to the point of development of either depression or anxiety. Our study being a cross-sectional study is therefore another limitation.
CONCLUSION
We conclude that the rates of depression, anxiety, stress, and insomnia were still prevalent in rural HCWs of Telangana during the declining phase of the COVID-19 pandemic. Demographic and COVID-19–related factors such as lower age, higher education, COVID-19–positive or suspected status, and family members influenced these rates. Further, we conclude that the effect of stress on anxiety is mediated by insomnia.
Article Information
Published Online: January 28, 2025. https://doi.org/10.4088/PCC.24m03723
© 2025 Physicians Postgraduate Press, Inc.
Submitted: February 15, 2024; accepted August 14, 2024.
To Cite: Tikka SK, Bhatia V, Sahoo DP, et al. COVID-19 pandemic–related perceived stress, insomnia, depression, and anxiety among rural primary care health workers: a mediation analysis. Prim Care Companion CNS Disord. 2025;27(1):24m03723.
Author Affiliations: Department of Psychiatry, All Indian Institute of Medical Sciences, Bibinagar, India (Tikka, Malathesh); Department of Community Medicine and Family Medicine, All Indian Institute of Medical Sciences, Bibinagar, India (Bhatia, Sahoo); All Indian Institute of Medical Sciences, Bibinagar, India (Meena, Nuthan).
Corresponding Author: Barikar C. Malathesh, MD, Department of Psychiatry, All Indian Institute of Medical Sciences, Bibinagar, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: Presented at Annual National Conference of Indian Psychiatric Society; January 18–21, 2024; Kochi, Kerala, India.
Clinical points
- Rates of depression, anxiety, stress, and insomnia were still prevalent in rural health care workers during the declining phase of the pandemic.
- Lower age, higher education, COVID-19–positive or suspected status, and family members influenced mental health rates.
- The effect of stress on depression and anxiety is mediated by insomnia.
References (23)

- Pfeifer LS, Heyers K, Ocklenburg S, et al. Stress research during the COVID-19 pandemic and beyond. Neurosci Biobehav Rev. 2021;131:581–596.
- Hu Y, Chen Y, Zheng Y, et al. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav Immun. 2020;89:587–593. PubMed
- Kempuraj D, Selvakumar GP, Ahmed ME, et al. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neuroscientist. 2020;26(5–6):402–414.
- Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):57.
- Akova İ, Kiliç E, Özdemir ME. Prevalence of burnout, depression, anxiety, stress, and hopelessness among healthcare workers in COVID-19 pandemic in Turkey. Inquiry. 2022;59:469580221079684. PubMed
- Iyengar KP, Jain VK, Ish P, et al. Impact of second wave of COVID-19 on health care workers in India. Apollo Med. 2021;18:12.
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307.
- Campo-Arias A, Pedrozo-Pupo JC, Herazo E. Review of the COVID-19 Pandemic Related Perceived Stress Scale (PSS-10-C). Rev Colomb Psiquiatr. 2021;50(3):156–157.
- Tikka SK, Malathesh BC, Bhatia V, et al. Factor structure of the Telugu version of the COVID-19 pandemic-related perceived stress scale (PSS-10-C) administered on grassroots frontline health care workers of rural Telangana. Indian J Psychol Med. 2022;44(3):272–278.
- Tikka SK, Malathesh BC, Sahoo DP, et al. Factor structure of the Telugu version of the Insomnia Severity Index administered to primary care health workers of rural Telangana during the COVID-19 pandemic. Prim Care Companion CNS Disord. 2022;24(2):21m03185. PubMed
- Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. PubMed
- Gowda V, Rani S, Chandrakala, et al. Depression, anxiety, stress among ASHA workers, in selected primary health centres in Southern Bengaluru. Int J Community Med Public Health. 2021;8:5856–5859.
- Sharma R, Tikka SK, Bhute AR, et al. Adherence of online surveys on mental health during the early part of the COVID-19 outbreak to standard reporting guidelines: a systematic review. Asian J Psychiatr. 2021;65:102799. PubMed
- Su TP, Lien TC, Yang CY, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007;41(1):119–130.
- Nwachukwu I, Nkire N, Shalaby R, et al. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health. 2020;17(17):6366. PubMed
- Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, et al. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4):e00054020. PubMed
- González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID 19) in Spain. Brain Behav Immun. 2020;87:172–176.
- Herbison CE, Allen K, Robinson M, et al. The impact of life stress on adult depression and anxiety is dependent on gender and timing of exposure. Dev Psychopathol. 2017;29(4):1443–1454. PubMed
- Lowery-Gionta EG, Crowley NA, Bukalo O, et al. Chronic stress dysregulates amygdalar output to the prefrontal cortex. Neuropharmacology. 2018;139:68–75.
- Manzar MD, Salahuddin M, Pandi-Perumal SR, et al. Insomnia may mediate the relationship between stress and anxiety: a cross-sectional study in university students. Nat Sci Sleep. 2021;13:31–38.
- Liu Z, Liu R, Zhang Y, et al. Association between perceived stress and depression among medical students during the outbreak of COVID-19: the mediating role of insomnia. J Affect Disord. 2021;292:89–94. PubMed
Enjoy this premium PDF as part of your membership benefits!