ABSTRACT
Objective: To examine the potential of using l-methylfolate (LMF) as an adjunctive therapy for major depressive disorder (MDD) and assess its role in filling current treatment gaps for patients who are overweight/obese and have chronic inflammation.
Data Sources: The PubMed database was searched using the key words l-methylfolate, adjunctive, and depression to identify studies published from January 2000 to April 2021.
Study Selection: Identified studies included 2 randomized controlled trials (RCTs), an open-label extension of these RCTs, and a real-world prospective study. Post hoc analyses that explored subgroups and their response to LMF treatment, including patients who were overweight and had elevated inflammatory biomarkers, were also included.
Results: These studies support the use of LMF as an adjunctive treatment in patients with MDD not responding to antidepressant monotherapy. The most effective dose tested was 15 mg/day. Treatment response was higher in individuals with a body mass index (BMI) ≥ 30 kg/m2 and elevated levels of inflammatory biomarkers. Inflammation is associated with increased production of proinflammatory cytokines, which interferes with the synthesis and turnover of monoamine neurotransmitters, thereby contributing to expression of depressive symptomatology. LMF may mitigate these effects by facilitating the synthesis of tetrahydrobiopterin (BH4), a critical coenzyme in neurotransmitter production. Furthermore, LMF does not cause adverse reactions commonly associated with other adjunctive MDD treatment agents (eg, atypical antipsychotics), such as weight gain, metabolic perturbations, and movement disorders.
Conclusion: LMF is effective as an adjunctive treatment in MDD and may especially benefit patients with higher BMI and inflammation.
Prim Care Companion CNS Disord 2023;25(3):22nr03361
To cite: Maletic V, Shelton R, Holmes V. A review of l-methylfolate as adjunctive therapy in the treatment of major depressive disorder. Prim Care Companion CNS Disord. 2023;25(3):22nr03361
To share: https://doi.org/10.4088/PCC.22nr03361
© 2023 Physicians Postgraduate Press, Inc.
aUniversity of South Carolina School of Medicine, Greenville, South Carolina
bUniversity of Alabama at Birmingham, Birmingham, Alabama
cUniversity of North Carolina, Chapel Hill, North Carolina
*Corresponding author: Vladimir Maletic, MD, University of South Carolina School of Medicine, 607 Grove Rd, Greenville, SC 29605 ([email protected]).
Major depressive disorder (MDD) is a commonly occurring mood disorder that is associated with significant disability and frequent treatment challenges.1,2 In 2018, the lifetime prevalence of MDD was estimated to be 21% in the United States, with a 23.2% projected lifetime risk at 75 years of age.3,4 The annual prevalence of a major depressive episode in adults in the United States in 2019 was estimated to be 7.8%.1 This high prevalence in adults is in addition to the rapidly escalating rate of depression and suicide among adolescents.5 Although there is a large number of currently available options for the treatment of MDD, substantial challenges persist, as a considerable percentage of patients fail to achieve an adequate response to treatment.2,6 A 2021 study estimated that 30.9% of adults with MDD have treatment-resistant depression (TRD), which represents 2.76 million people.7 There is therefore a need for new therapeutic approaches to treat MDD.
There has been interest since the mid-1960s in the role of folate (vitamin B9) and the other B vitamins in the pathophysiology and treatment of depression.8 A 2007 systematic review and meta-analysis demonstrated a significant relationship between low folate status and risk for depression (odds ratio [OR]: 1.55; 95% confidence interval [CI] = 1.26–1.91).9 Additional studies have examined the adjunctive use of the B vitamins as treatments for depression. A systematic review from 2015 concluded that prolonged consumption of a combination of folate and vitamins B6 and B12 added to antidepressant pharmacotherapy may delay the onset of depressive symptoms and reduce the risk of relapse for depressive episodes.10 A randomized controlled trial from 2014 demonstrated that a combination of folate, B6, and B12 and citalopram generated a greater reduction of depressive symptoms over a 52-week treatment period compared with citalopram plus placebo.11 A systematic review and meta-analysis from 2021 concluded that adjunctive folate provided a greater treatment response rate than selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) alone for the treatment of patients with MDD (adjunctive therapy: n = 279, monotherapy: n = 287; risk ratio [RR]: 1.36; 95% CI, 1.16–1.59; P = .0001).12
Dietary folate or folic acid supplements are metabolized via several steps in the human body.13 Folate is available in several different forms including dietary folate (dihydrofolate), synthetic folic and folinic acid supplements, and the terminal metabolite l-methylfolate (LMF) (also referred to as 6-[S]-5-methyltetrahydrofolate). A major difference between folate consumed through the diet, synthetic folic acid supplements, and LMF relates to the activity of the methylated and reduced form of the folate molecule.14 LMF is a reduced metabolite of folate. Unlike dietary folate or folic acid, LMF readily crosses the blood-brain barrier (Figure 1A).14 LMF is available in multiple forms, including as a prescription medical food (Deplin, Alfasigma). According to the Orphan Drug Act, prescription medical foods are intended for the dietary management of diseases or conditions that have specific nutritional requirements and are to be supervised by a physician.15 LMF is approved for the clinical dietary management of patients with MDD and is formulated to meet the specific nutritional requirements of patients with MDD who also have suboptimal LMF levels in the cerebrospinal fluid, plasma, or red blood cells.15,16
The key regulatory enzyme that metabolizes folate into biologically active LMF is methylenetetrahydrofolate reductase (MTHFR). There are common polymorphisms in the gene coding for this enzyme affecting its activity, with one such variant (ie, MTHFR C677T) being present in up to 60% of the US population.17 A 2007 meta-analysis concluded that the homozygous TT, compared with the CC variant of the MTHFR C677T gene, was associated with an increased risk of depression, bipolar disorder, and schizophrenia.18
The mechanism by which LMF augments antidepressant therapy has been primarily linked to monoamine synthesis (Figure 1B).19 LMF promotes the synthesis of the key monoamine neurotransmitters associated with MDD (ie, serotonin, norepinephrine, dopamine) by increasing the conversion of dihydrobiopterin to tetrahydrobiopterin (BH4).19 BH4 is an enzymatic cofactor, which has a crucial role in the synthesis of monoamine neurotransmitters by enhancing the rate-limiting enzymes tryptophan and tyrosine hydroxylase, required for the production of serotonin, norepinephrine, and dopamine.20 Restitution of BH4 from BH2, via the LMF-dependent “salvage pathway,” is of particular importance in circumstances of increased oxidative stress and inflammation, as they are associated with greater reduction of BH4 due to more rapid monoamine turnover.20,21 The monoamines play critical roles in the actions of commonly used antidepressants, and their depletion may lead to poor antidepressant response. Therefore, maintaining the level of central nervous system BH4 is critical.19,21
In this article, we will review several controlled and open-label studies that assess the effectiveness of LMF as an adjunctive therapy for MDD. We will further discuss a number of studies focusing on the subpopulation of depressed patients with elevated BMI and increased inflammatory markers and how those specific markers can influence the course of depression and treatment outcomes. We will conclude by describing the mechanism of action of LMF and its role in filling current treatment gaps for depressed patients with obesity and chronic inflammation.
METHODS
We searched the PubMed database to identify studies evaluating the use of adjunctive LMF therapy in patients with MDD from January 2000 to April 2021. Relevant search terms included l-methylfolate, adjunctive, and depression. Additional post hoc analyses were also included to identify potential subgroups that demonstrated greater response.
RESULTS
The search retrieved 6 studies that are described in Table 1.22–26 Among these were 2 multicenter, double-blind, randomized, placebo-controlled, sequential parallel comparison trials using LMF studies conducted by the same authors, which were presented in the same article.22 A 12-month open-label extension of these trials was also identified.24 One real-world prospective observational study was identified that evaluated patients who were prescribed LMF to treat their MDD.26 Additionally, 2 post hoc exploratory analyses evaluated patients who were treated with either LMF or placebo and stratified by genetic or other biological markers to identify possible predictors of LMF response.23,25
Papakostas et al22 conducted 2 multicenter, double-blind, randomized, placebo-controlled, sequential parallel comparison trials of LMF versus placebo as an adjunctive to SSRI therapy in SSRI-resistant patients. Patients between the ages of 18 and 65 years were included in the trials if they had MDD (determined using DSM-IV criteria) and were receiving treatment with an adequate dose of SSRI for at least 8 weeks during the current episode of MDD. Adequate dosages were defined as 20 mg or more of fluoxetine, citalopram, or paroxetine; 10 mg or more of escitalopram; or 50 mg or more of sertraline. Subjects were required to have a stable dose for at least 4 weeks prior to baseline and to have failed to achieve sufficient symptom improvement following ≥ 2 antidepressant trials during the current major depressive episode. To be classified as SSRI resistant, patients had a minimum score of 12 on the Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR) at both screening and baseline visits. Patients who reported a > 25% decrease in the QIDS-SR between screening and baseline were excluded.22
Both trials were conducted using a sequential parallel comparison design.27 The studies were divided into two 30-day phases (phases 1 and 2), and patients were assessed every 10 days using the 17-item Hamilton Depression Rating Scale (HDRS-17), QIDS-SR, and Clinical Global Impressions severity (CGI-S) and improvement (CGI-I) scales. Doses of the SSRI were maintained throughout the study period. In trial 1, participants were randomized to placebo or LMF 7.5 mg/d in phase 1. Placebo patients then continued to take placebo for the subsequent 30 days, while those who were nonresponders to 7.5 mg of LMF were increased to 15 mg for the next 30-day period. In the subsequent trial, patients were randomized to receive placebo in both phases, placebo in phase 1 followed by LMF 15 mg in phase 2 or LMF 15 mg in both phases.22
In this trial (N = 148, 69.5% female), the mean (SD) age at baseline was 47.9 (11.6) years and mean (SD) baseline HDRS-17 score was 19.7 (4.7). In the second trial (N = 75, 70.6% female), the mean (SD) age at baseline was 48.4 (12.1) years and mean (SD) baseline HDRS-17 score was 21.2 (3.9). Response was defined as ≥ 50% reduction in HDRS-17 score during treatment or a final HDRS-17 score ≤ 7. Patients who received LMF 7.5 mg did not achieve efficacy superior to placebo plus SSRI. Patients receiving 15 mg/d of LMF for 30 days showed significantly greater mean reduction in HDRS-17 scores (–5.6 vs –3.0, P = .05) and higher response rates (32.3% vs 14.6%, P = .04) compared with placebo plus SSRI (Figure 2).22
Adverse events were recorded for both trials, and there were no significant differences between the treatment and control groups in changes in heart rate, supine or standing blood pressure, or in weight. The most common categories of adverse events in the first trial were gastrointestinal in 20.1% (n = 23) of the placebo group, 9.6% (n = 9) of the LMF 7.5 mg group, and 10% (n = 3) of the LMF 15 mg group; somatic in 19.6% (n = 22) of the placebo group, 9.6% (n = 9) of the LMF 7.5 mg group, and 10% (n = 3) of the LMF 15 mg group; and infectious in 11.6% (n = 13) of the placebo group, 6.4% (n = 6) of the LMF 7.5 mg group, and 6.7% (n = 2) of the LMF 15 mg group.22 In the second trial, the most common categories of adverse events were somatic in 29.6% (n = 16) of the placebo group and 14.3% (n = 6) of the LMF 15 mg group; gastrointestinal in 14.8% (n = 8) of the placebo group and 16.7% (n = 7) of the LMF 15 mg group; and psychological in 16.7% (n = 9) of the placebo group and 9.5% (n = 4) of the LMF 15 mg group. There was one incident of a patient developing manic symptoms in the treatment group of the second trial, and the participant was withdrawn from the study.22
Open-Label Extension of Randomized Controlled Trials
Zajecka et al24 conducted a 12-month open-label extension study using the population from the 2 previously described double-blind, multicenter, randomized controlled trials.28 Only patients who received 15 mg/d of LMF for most of the open-label phases were included in the efficacy analysis. Patients were evaluated every 3 months for primary outcome measures of response (≥ 50% improvement in HDRS-17 scores from start of double-blind phase), remission (total HDRS-17 score ≤ 7), recovery (≥ 6 months of remission from start of open-label phase), relapse (HDRS-17 score > 15 within 6 months of achieving remission), and recurrence (HDRS-17 score > 15 after recovery).
A total of 68 patients were included in the final analysis, 38% of whom achieved recovery and 61% of whom achieved remission at any point during the study. Of patients meeting the criteria for recovery, none experienced a recurrence of MDD. Remission and recovery rates are shown in Figure 3 for patients entering the open-label phase in remission, as responders and as nonresponders, as well as the total patient sample. Among initial nonresponders, 60% eventually reached remission. There were no serious adverse events among patients included in the efficacy analysis.24 These results indicate that patients who respond well to shorter-term treatment are likely to maintain that response over the subsequent year and show that those not adequately responding within the first 8 weeks of therapy may benefit from longer-term LMF treatment.
Real-World Prospective Observational Study
Shelton et al26 conducted a prospective observational study evaluating patients prescribed LMF for the treatment of MDD in real-world clinical sites. Patients ≥ 18 years old who completed a patient experience program between November 2010 and April 2012 were included. Eligibility for the program required a prescription of 7.5 mg/d or 15 mg/d of LMF. Patients completed a baseline survey prior to starting LMF and a follow-up survey 90 days post treatment. Primary endpoints included change in depression severity (as measured using mean change in 9-item Patient Health Questionnaire [PHQ-9]), treatment response (≥ 50% reduction in PHQ-9 score from baseline), and remission (PHQ-9 score < 5 at 90 days post treatment). Secondary endpoints included change in the effect of depression on quality of life (scale of 1–5) and medication satisfaction (scale of 1–9). Patients with a baseline PHQ-9 score ≥ 5 were included in the analysis.
A total of 554 patients completed the baseline and post-baseline surveys and had initial PHQ-9 scores ≥ 5. At baseline, the mean (SD) age was 49.9 (14.1) years, and the majority of patients were female (76.5%) and had a duration of depression for > 2 years at baseline (77.1%). More patients used LMF adjunctively with antidepressants (90.6%) than as monotherapy (9.4%). The most commonly used antidepressant medications were SSRIs and SNRIs (42.2% and 30.3%, respectively). Adherence to LMF therapy was high, with 90.8% of patients reporting to have taken every or nearly every dose. Pooled mean (SD) change in PHQ-9 was −8.5 (6.3), and PHQ-9 response and remission rates were 67.9% and 45.7%, respectively. The impact of depression on quality of life is reported in Supplementary Figure 1. Patients reported a significantly higher medication satisfaction score on a scale of 1 (worst) to 9 (best) compared with their previous medication (mean: 7.0 vs 5.2, P < .001).26 These outcomes suggest that the results seen in the controlled trial are likely to extend to patients in real-world practice.
Post Hoc Exploratory Analysis of Randomized Controlled Trials
Two post hoc analyses were published that further explored the data from the previously described randomized controlled trials.22 Papakostas et al23 published a study in 2014 that stratified patients based on data collected from the second trial22 randomized to placebo or LMF 15 mg to explore differences in response to LMF based on biomarkers, body mass index (BMI), and genotype. Patients were stratified into higher and lower biomarker groups by a median split of the data for BMI and status of other biomarkers, including high-sensitivity C-reactive protein (hsCRP), S-adenosylmethionine/S-adenosylhomocysteine (SAM/SAH) ratio, and 4-hydroxy-2-nonenal (4-HNE). DNA was extracted from blood samples and genotyped for common polymorphisms of genes of enzymes of interest in the folate and methionine metabolism pathways: MTHFR, methionine synthase reductase (MTRR), and methionine synthase (MTR). The primary outcome measure was the effect of BMI and biomarkers on the response to the 28-item HDRS (HDRS-28) with LMF versus placebo. The authors23 note that the HDRS-28 score was used instead of the 17-item score because the adapted 28-item version is more sensitive to the responses of patients with either atypical or melancholic depression. BMI was categorized into ≥ 30 or < 30 kg/m2, and the biomarker values were separated as above or below the median: hsCRP level ≥ 2.25 or < 2.25 mg/L, SAM/SAH ratio ≥ 2.71 or < 2.71, and 4-HNE level ≥ 3.28 or < 3.28 μg/mL (Supplementary Table 1). A total of 61 patients were included in the study. The pooled mean changes on the HDRS-28 were significantly greater (P ≤ .05) among patients with lower SAM/SAH ratio, higher hsCRP or 4-HNE levels, or BMI ≥ 30 kg/m2 at baseline. Analysis of the genetic polymorphisms yielded significant changes (P ≤ .05) among patients with polymorphisms in MTR or MTRR genes, but not in MTHFR. The number of patients genotyped in this study23 was relatively small (n = 59), and analyses of larger samples might show more significant effects.
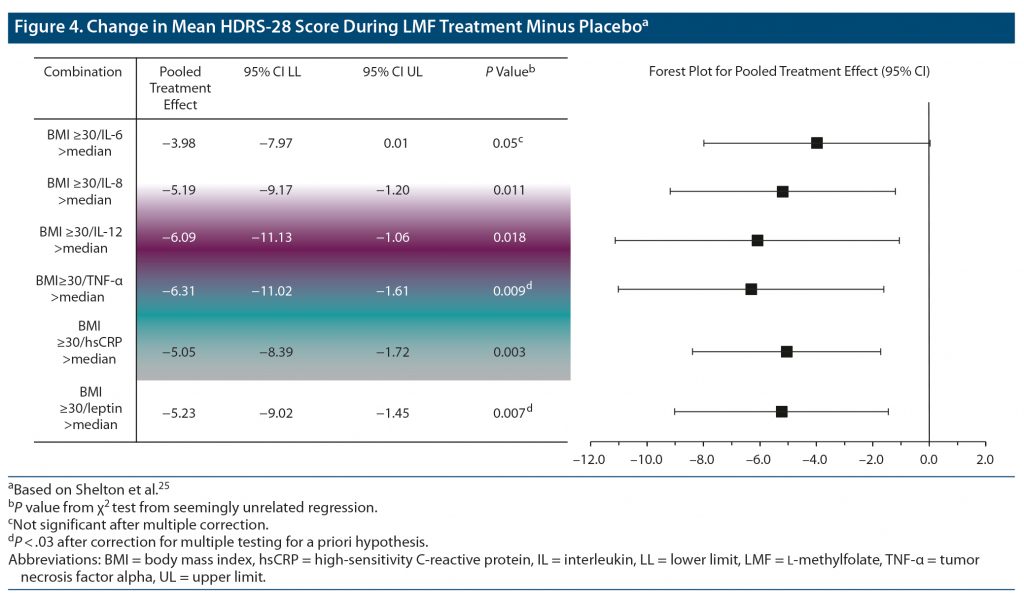
To further explore the effects of inflammatory biomarkers on LMF treatment response in this patient set, an additional post hoc analysis evaluated levels of cytokines (tumor necrosis factor α [TNF-α], interferon γ [IFN-γ], and various interleukins (IL-1α, −1β, −2, −4, −5, −6, −8, −10, −12p70, −13, −17) and other biomarkers, including adiponectin, leptin, insulin, and hsCRP.22,25 The authors25 hypothesized that patients with higher levels of inflammatory biomarkers would show a greater response, and that interactions between certain biomarkers (IL-6, TNF-α, and hsCRP) and elevated BMI may enhance treatment effect. Treatment effects were analyzed separately for BMI and levels of the biomarkers at baseline. Systemic inflammation was denoted by biomarker concentrations in samples that were above the median value. Data for 74 patients were available in the primary analysis, and of those, the data of 69 patients were evaluable.
Results from the second analysis25 found that individuals with BMI < 30 did not have a significant change from baseline with LMF treatment, and those with a BMI ≥ 30 did (pooled treatment effect –4.66; 95% CI, –7.22 to –1.98; P = .001). The separation was striking; the higher BMI patients experienced a much greater change in depression severity compared with placebo, but low BMI patients did not (–4.66 vs +0.63). Levels of TNF-α, IL-8, hsCRP, and leptin above the median value were associated with a significant greater treatment effect (P < .05), and differences remained significant after adjustment for BMI. In addition, a significant effect was seen for the interaction of BMI ≥ 30 with TNF-α, IL-6, IL-8, IL-12, hsCRP, and leptin as is presented in Figure 4. The combination of high BMI and TNF-α showed the greatest overall effect (6.31 vs placebo) compared with the total sample (–2.7). While each individual factor (BMI and cytokines) showed significant main effects, the synergy between BMI and TNF-α, IL-6, and hsCRP suggest that these risk factors may interact with each other to influence response to LMF.
DISCUSSION
The 2 randomized controlled trials22 described in this review demonstrated that patients treated with LMF 15 mg/d (but not 7.5 mg/d) as an adjunct to SSRI therapy had significantly greater efficacy compared with placebo. Furthermore, results from the post hoc analyses23,25 indicate that patients with elevated BMI, elevated inflammatory biomarkers, and the combination of elevated BMI and inflammatory biomarkers demonstrated a greater response to adjunctive LMF compared with those with lower levels of inflammation and BMI. These results highlight important links between depression, overweight status, and chronic inflammation, suggesting that LMF may be particularly effective for overweight depressed patients, especially those with indicators of systemic inflammation. These indicators would include the presence of metabolic diseases like hypertension, type II diabetes, and dyslipidemia.
The common functional polymorphism of MTHFR C677T is often used as a clinical biomarker for response to LMF. In the genetic analysis described earlier, LMF was effective in both C and T carriers.23 Therefore, MTHFR C677T should not be used as a primary indicator to identify those who are likely to respond to LMF, but this does not mean that loss-of-function polymorphisms of genes in the folate metabolic pathway are irrelevant. For example, there were significant links between the MTR or MTRR gene biomarkers and better response to LMF; moreover, MTHFR C677T polymorphisms approached statistical significance (P = .087).23 In summary, response to LMF can be expected for both homozygous C and CT/TT carriers.
Bidirectional relationships have been found between obesity or overweight status and depression in longitudinal studies.29–31 A 2010 meta-analysis found that obese individuals had a 55% increased risk of becoming depressed compared with nonobese persons, and depressed individuals had a 58% increased risk of becoming obese compared with people who were not depressed.29 Additionally, severity of depressive symptoms may increase with higher BMI. In a study30 evaluating the association between obesity and depression in women aged 40 to 65 years, the severity of depression, using the PHQ-9, increased incrementally when BMI increased from normal (< 25) to morbidly obese (≥ 35). Furthermore, a large prospective community sample study noted an association between dietary inflammatory index, BMI, and the risk of developing depression.32 Depression may also be more difficult to treat in individuals with elevated BMI. A 5-week study of hospitalized depressed patients found delayed treatment response to antidepressants in overweight patients (25 < BMI ≤ 30) compared with those with a normal BMI (< 25), with even slower treatment response in the patients with morbid obesity (> 30).33 The results of this study33 demonstrated that overweight/obese patients make up a subgroup of patients whose difficult-to-treat depression warrants particular attention, especially in regard to the future development of antidepressant medications. Additional studies reported that baseline BMI in MDD patients predicted reduction in depression scores, remission rate, and functional improvement at the conclusion of antidepressant treatment.34,35 Moreover, depression in the context of metabolic syndrome confers a higher risk of chronic, recurrent depression, which has been referred to as a depressive subtype labeled “metabolic depression.”36 In a community-based study of older patients, Vogelzangs et al36 concluded that in the context of metabolic syndrome, depression is 3 times more likely to be persistent or recurrent. Abdominal obesity was also associated with the onset of depression.
Inflammation also appears to be related to both overweight status and the development of depression. Studies37,38 have shown that high levels of inflammatory biomarkers, such as IL-6 and CRP, have been associated with increased depressive symptoms and risk of TRD. Theories regarding the pathophysiology of depression suggest that chronic inflammation and obesity may play a role in the development and recurrence of MDD in some patients.39 A 2021 study40 in which participants were stratified according to BMI established a relationship between systemic inflammation and degrees of obesity with increased neuropsychiatric comorbidity. The type of adipose tissue may play a factor in the relationship between inflammation and depression, as visceral (intraabdominal) adipose tissue has been more closely related to depressive symptoms than subcutaneous adipose tissue.41 Visceral adipose tissue has been described as metabolically active, atherogenic, and secreting inflammatory markers.41 A study of women with obesity, pre- and post-bariatric surgery, found that baseline BMI correlated significantly with adipokines, leptin, adiponectin, IL-6, and hsCRP. Extending these findings, a regression analyses showed that higher depression and anxiety scores were associated with higher levels of the inflammatory markers IL-6 and hsCRP, even after adjusting for adiposity or BMI.42 Furthermore, a 2018 study of obese individuals with chronic low-grade systemic inflammation, denoted by hsCRP but not metabolic abnormalities, predicted scores on the Montgomery-Asberg Depression Rating Scale.43 These studies indicate depression and anxiety may have impacts on systemic inflammation.
Mechanism of Inflammation in Depression
Commonly used antidepressant medications require intact monoamine neurotransmitter systems. In particular, reuptake inhibitors (eg, SSRIs and SNRIs) require constant monoamine synthesis. In several studies,44,45 depressed patients who were successfully treated with SSRIs experienced a rapid return of depression symptoms when tryptophan, the precursor for serotonin, was rapidly depleted, and the antidepressant response was restored with the administration of tryptophan. A similar return of depression symptoms was shown with depletion of tyrosine, the precursor of norepinephrine, in patients whose depression remissions were maintained on norepinephrine reuptake inhibitors (NRIs).46 These studies show that SSRIs require continuous synthesis of serotonin, and NRIs require continuous synthesis of norepinephrine.
Inflammation affects the monoamine neurotransmitters in a variety of ways. The use of the cytokine interferon-α (IFN-α) in the treatment of hepatitis C and cancers is illustrative of how an increase in inflammatory proteins can be linked to depression.47 IFN-α is known to induce clinically significant depression in 30%–50% of treated patients.47 There are several mechanisms to describe this relationship. IFN-α induces p38 mitogen activated protein kinase (MAPK), which upregulates serotonin transporters.47 Serotonin transporters are responsible for the reuptake of serotonin at the presynaptic terminal and are the target of the blockade action of SSRIs.48 Additionally, IFN-α activates indoleamine 2,3 dioxygenase (IDO), which converts tryptophan to kynurenine, thereby leading to serotonin depletion.47 A study of suicidal patients, half of whom suffered from MDD (n = 32/63), described a positive correlation between cerebrospinal fluid (CSF) IL-6 levels and CSF metabolites of serotonin (5-HIAA = 5-hydroxyindoleacetic acid) and dopamine(HVA = homovanillic acid) and between TNFα levels and 5-HIAA, suggesting increased turnover of serotonin and dopamine.49 The findings of this study establish a key link between elevated inflammatory cytokines in the cerebrospinal fluid and increased monoamine turnover, presumably taxing the cellular synthetic apparatus.
Proinflammatory cytokines can also impact the availability of neurotransmitters by reducing BH4 levels (Figure 1). Increased cytokine levels activate inducible nitric oxide synthase (iNOS) that converts L-arginine to nitric oxide, a gaseous signaling molecule in cells and an important component of cellular immune response.50,51 iNOS requires BH4 as a cofactor, which is converted to BH2 in the process. Chronic iNOS activation can result in depletion of BH4.52,53 Both IFN-α and the cytokine IL-6 have been shown to reduce BH4, the essential cofactor for tryptophan hydroxylase and tyrosine hydroxylase, which are the rate-limiting enzymes involved in the production of serotonin, norepinephrine, and dopamine, respectively.20 Cytokines can induce oxidative stress, which can also irreversibly degrade BH4 to dihydroxanthopterin (XPH2).20 In summary, increased peripheral and central inflammatory signaling in the context of combined depression and obesity may be associated with a gap between increased monoamine turnover and depleted monoamine synthetic capacity, which may interfere with emotional regulation and efficacy of commonly used antidepressant agents.
The Role of LMF in Treating Depression in Individuals With Obesity and Inflammation
Although the mechanisms by which LMF has a greater effect in individuals with obesity and inflammation are not fully understood, there are several possible avenues by which LMF may be more effective in obese patients, particularly those who have chronic systemic inflammation associated with visceral adiposity. Studies23 that stratified patients treated with adjunctive LMF by biomarker status showed significant changes in HDRS-28 scores among patients with MTR and MTRR genetic polymorphisms, but not in MTHFR, suggesting LMF is an effective treatment in patients who are not only genotype positive. There is some evidence that indicates folate may decrease inflammation. In a study from 2020,54 increased dietary folate (a precursor molecule to biologically active LMF) was linked to reduced levels of inflammatory biomarkers in obese/overweight women with the homozygous C677T MTHFR gene polymorphism. This indicates that folate may help reduce inflammation in the obese/overweight population, at least in those with possible LMF deficiency.54 There is also evidence that LMF can enhance production of monoamines despite inflammation. As stated previously, LMF increases the conversion of BH2 to BH4 (Figure 1) and thus has the potential to mitigate inflammation-driven decreases in BH4.19 Consequently, it may increase the availability of monoamine neurotransmitters, even in the context of inflammation and increased oxidative stress, by counteracting the processes that deplete neurotransmitters, as previously described.19 This may explain, to a certain extent, why LMF seems to have a greater effect size in patients with heightened inflammatory markers and obesity.
As LMF has shown some efficacy in this population, it is noteworthy that LMF may also be an adjunctive treatment choice that confers less risk of weight gain than alternative treatment options (eg, atypical antipsychotics). Adverse side effects, including weight gain, are common with atypical antipsychotic medications when used as adjunctive treatments to antidepressant pharmacotherapy.55 Currently, aripiprazole, brexpiprazole, and quetiapine have been approved by the US Food and Drug Administration as adjunctive treatments for MDD.56 Olanzapine, in combination with the SSRI fluoxetine, has been approved for TRD.56,57 A 2016 meta-analysis55 concluded that the atypical antipsychotics aripiprazole, olanzapine, and quetiapine have also been associated with weight gain in a significant proportion of patients. A 2021 systematic review and meta-analysis58 found that in patients treated long term (defined as 24 to 52 weeks) with aripiprazole at a daily dose > 5 mg, the incidence of medically significant weight gain, defined as ≥ 7% of body weight, was observed in 25%–28% of patients. In contrast, none of the studies identified associated LMF with significant weight gain, including a 12-month open-label extension study.24 In addition, a safety and toxicology evaluation was published in 2019,59 using animal models, with LMF dosages of up 400 mg/kg body weight/d. The authors reported that after 13 weeks, mean body weights in the treatment group were not significantly different from those in the control group. They concluded that their results support the safety of LMF as a dietary supplement for depressed patients.59
CONCLUSION
Two randomized controlled trials, a 12-month open-label extension, and a real-world prospective observational study have been conducted that provide evidence for the use of LMF as an adjunctive treatment to antidepressants in MDD.22,24,26 Additional data from 2 post hoc analyses suggest a link between chronic inflammation, elevated BMI, and depression.23,25 A 15-mg/d dose of LMF was found to be most effective, and the highest degree of treatment response was seen in individuals who had BMI ≥ 30 and in those who had elevated levels of inflammatory markers.22,23,25 Obesity and inflammation are easy to assess in clinical practice using an office scale and laboratory analysis of hsCRP. Notably, LMF does not have to be reserved only for obese patients with elevated hsCRP. However, those who have both obesity and chronic inflammation may be particularly responsive. Given that this population may be prone to depression that is more difficult to treat, and that currently available adjunctive treatment options (eg, atypical antipsychotics) have unfavorable side effect profiles, patients in this subpopulation may see additional benefit from LMF as an adjunctive treatment option for MDD that is not responsive to antidepressant pharmacotherapy.
Submitted: July 27, 2022; accepted November 4, 2022.
Published online: May 9, 2023.
Relevant financial relationships: Dr Maletic has received writing support from Alfasigma USA; consulting/advisory fees from AbbVie/Allergan, Acadia, Alfasigma USA, Alkermes, Eisai-Purdue, Intra-Cellular Therapies, Janssen, Lundbeck A/S, Jazz, Noven, Otsuka America, Sage, Sunovion, Supernus, and Takeda; and honoraria for lectures from AbbVie, Acadia, Alkermes, Allergan, Eisai, Ironshore, Intra-Cellular, Janssen, H. Lundbeck A/S, Otsuka America, Sunovion, Supernus, and Takeda. Dr Shelton has participated on data safety monitoring or advisory boards for Janssen and has received writing support from Alfasigma USA; payments to institution (grants or contracts) from Acadia, Alkermes, Allergan, Assurex, Avanir, Cerecor, Intracellular Therapies, Janssen, LivaNova, Navitor, NeuroRx, Novartis, Otsuka America, and Takeda; royalties from Wolters Kluwer; and consulting fees from Acadia, Allergan, Alfasigma USA, Myriad Neuroscience, Novartis International AG, Evecxia Therapeutics, Seelos Therapeutics, Sunovion, and NeuroRx. Dr Holmes has participated on an advisory board for and received writing support from Alfasigma USA.
Funding/support: This work was funded by Alfasigma USA. The authors did not receive payment for their participation.
Role of the sponsor: The authors received editorial support in the preparation of this manuscript from Peloton Advantage, LLC, an OPEN Health company, Parsippany, New Jersey, sponsored by Alfasigma USA. The authors directed and are fully responsible for all content and editorial decisions for this manuscript.
Supplementary material: See accompanying pages.
CLINICAL POINTS
- Major depressive disorder is associated with being overweight/obese and having chronic inflammation.
- l-methylfolate 15 mg/d has been shown to be an effective adjunctive treatment for major depressive disorder in those not responding to antidepressant pharmacotherapy.
- Post hoc analyses suggest that the treatment effect of adjunctive l-methylfolate 15 mg/d may be more pronounced among individuals with a body mass index ≥ 30 kg/m2 and elevated levels of inflammatory biomarkers.
References (59)

- Major depression. National Institute of Mental Health website. Accessed November 15, 2021. https://www.nimh.nih.gov/health/statistics/major-depression.shtml#part_155029
- Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–1917. PubMed CrossRef
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. PubMed CrossRef
- Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. PubMed CrossRef
- Twenge JM. Increases in depression, self‐harm, and suicide among US adolescents after 2012 and links to technology use: possible mechanisms. Psychiatr Res Clin Pract. 2020;2(1):19–25. PubMed CrossRef
- Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40. PubMed CrossRef
- Zhdanava M, Pilon D, Ghelerter I, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82(2):82. PubMed CrossRef
- Carney MW. Serum folate values in 423 psychiatric patients. BMJ. 1967;4(5578):512–516. PubMed CrossRef
- Gilbody S, Lightfoot T, Sheldon T. Is low folate a risk factor for depression? a meta-analysis and exploration of heterogeneity. J Epidemiol Community Health. 2007;61(7):631–637. PubMed CrossRef
- Almeida OP, Ford AH, Flicker L. Systematic review and meta-analysis of randomized placebo-controlled trials of folate and vitamin B12 for depression. Int Psychogeriatr. 2015;27(5):727–737. PubMed CrossRef
- Almeida OP, Ford AH, Hirani V, et al. B vitamins to enhance treatment response to antidepressants in middle-aged and older adults: results from the B-VITAGE randomised, double-blind, placebo-controlled trial. Br J Psychiatry. 2014;205(6):450–457. PubMed CrossRef
- Altaf R, Gonzalez I, Rubino K, et al. Folate as adjunct therapy to SSRI/SNRI for major depressive disorder: systematic review & meta-analysis. Complement Ther Med. 2021;61:102770. PubMed CrossRef
- Farah A. The role of L-methylfolate in depressive disorders. CNS Spectr. 2009;14(suppl 2):2–7. PubMed CrossRef
- Stahl SM. Novel therapeutics for depression: L-methylfolate as a trimonoamine modulator and antidepressant-augmenting agent. CNS Spectr. 2007;12(10):739–744. PubMed CrossRef
- Orphan drug act - relevant excerpts. US Food and Drug Administration website. 2018. Accessed November 15, 2021. https://www.fda.gov/industry/designating-orphan-product-drugs-and-biological-products/orphan-drug-act-relevant-excerpts
- Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178(3):200–206. PubMed CrossRef
- Miller AL. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Altern Med Rev. 2008;13(3):216–226. PubMed
- Gilbody S, Lewis S, Lightfoot T. Methylenetetrahydrofolate reductase (MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol. 2007;165(1):1–13. PubMed CrossRef
- Stahl SM. L-methylfolate: a vitamin for your monoamines. J Clin Psychiatry. 2008;69(9):1352–1353. PubMed CrossRef
- Haroon E, Raison CL, Miller AH. Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior. Neuropsychopharmacology. 2012;37(1):137–162. PubMed CrossRef
- Vancassel S, Capuron L, Castanon N. Brain kynurenine and BH4 pathways: relevance to the pathophysiology and treatment of inflammation-driven depressive symptoms. Front Neurosci. 2018;12:499. PubMed CrossRef
- Papakostas GI, Shelton RC, Zajecka JM, et al. L-methylfolate as adjunctive therapy for SSRI-resistant major depression: results of two randomized, double-blind, parallel-sequential trials. Am J Psychiatry. 2012;169(12):1267–1274. PubMed CrossRef
- Papakostas GI, Shelton RC, Zajecka JM, et al. Effect of adjunctive L-methylfolate 15 mg among inadequate responders to SSRIs in depressed patients who were stratified by biomarker levels and genotype: results from a randomized clinical trial. J Clin Psychiatry. 2014;75(8):855–863. PubMed CrossRef
- Zajecka JM, Fava M, Shelton RC, et al. Long-term efficacy, safety, and tolerability of L-methylfolate calcium 15 mg as adjunctive therapy with selective serotonin reuptake inhibitors: a 12-month, open-label study following a placebo-controlled acute study. J Clin Psychiatry. 2016;77(5):654–660. PubMed CrossRef
- Shelton RC, Pencina MJ, Barrentine LW, et al. Association of obesity and inflammatory marker levels on treatment outcome: results from a double-blind, randomized study of adjunctive L-methylfolate calcium in patients with MDD who are inadequate responders to SSRIs. J Clin Psychiatry. 2015;76(12):1635–1641. PubMed CrossRef
- Shelton RC, Manning JS, Barrentine LW, et al. Assessing effects of L-methylfolate in depression management: results of a real-world patient experience trial. Prim Care Companion CNS Disord. 2013;15(4):15. PubMed
- Fava M, Evins AE, Dorer DJ, et al. The problem of the placebo response in clinical trials for psychiatric disorders: culprits, possible remedies, and a novel study design approach. Psychother Psychosom. 2003;72(3):115–127. PubMed CrossRef
- Mischoulon D, Zajecka J, Freeman MP, et al. Does folic acid interfere with lamotrigine? Lancet Psychiatry. 2016;3(8):704–705. PubMed CrossRef
- Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. PubMed CrossRef
- Simon GE, Ludman EJ, Linde JA, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30(1):32–39. PubMed CrossRef
- Pan A, Sun Q, Czernichow S, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes. 2012;36(4):595–602. PubMed CrossRef
- Ma Y, Li R, Zhan W, et al. Role of BMI in the relationship between dietary inflammatory index and depression: an intermediary analysis. Front Med (Lausanne). 2021;8:748788. PubMed CrossRef
- Kloiber S, Ising M, Reppermund S, et al. Overweight and obesity affect treatment response in major depression. Biol Psychiatry. 2007;62(4):321–326. PubMed CrossRef
- Lin CH, Chen CC, Wong J, et al. Both body weight and BMI predicts improvement in symptom and functioning for patients with major depressive disorder. J Affect Disord. 2014;161:123–126. PubMed CrossRef
- Xiao L, Zhou J, Galling B, et al. The association of body mass index (BMI) with treatment outcomes in patients with major depressive disorder. J Affect Disord. 2021;281:799–804. PubMed CrossRef
- Vogelzangs N, Beekman AT, Boelhouwer IG, et al. Metabolic depression: a chronic depressive subtype? findings from the InCHIANTI study of older persons. J Clin Psychiatry. 2011;72(5):598–604. PubMed CrossRef
- Chamberlain SR, Cavanagh J, de Boer P, et al. Treatment-resistant depression and peripheral C-reactive protein. Br J Psychiatry. 2019;214(1):11–19. PubMed CrossRef
- Alesci S, Martinez PE, Kelkar S, et al. Major depression is associated with significant diurnal elevations in plasma interleukin-6 levels, a shift of its circadian rhythm, and loss of physiological complexity in its secretion: clinical implications. J Clin Endocrinol Metab. 2005;90(5):2522–2530. PubMed CrossRef
- Kiecolt-Glaser JK, Derry HM, Fagundes CP. Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry. 2015;172(11):1075–1091. PubMed CrossRef
- Huet L, Delgado I, Dexpert S, et al. Relationship between body mass index and neuropsychiatric symptoms: evidence and inflammatory correlates. Brain Behav Immun. 2021;94:104–110. PubMed CrossRef
- Everson-Rose SA, Lewis TT, Karavolos K, et al. Depressive symptoms and increased visceral fat in middle-aged women. Psychosom Med. 2009;71(4):410–416. PubMed CrossRef
- Capuron L, Poitou C, Machaux-Tholliez D, et al. Relationship between adiposity, emotional status and eating behaviour in obese women: role of inflammation. Psychol Med. 2011;41(7):1517–1528. PubMed CrossRef
- Delgado I, Huet L, Dexpert S, et al. Depressive symptoms in obesity: Relative contribution of low-grade inflammation and metabolic health. Psychoneuroendocrinology. 2018;91:55–61. PubMed CrossRef
- Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of antidepressant action: reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry. 1990;47(5):411–418. PubMed CrossRef
- Delgado PL, Miller HL, Salomon RM, et al. Tryptophan-depletion challenge in depressed patients treated with desipramine or fluoxetine: implications for the role of serotonin in the mechanism of antidepressant action. Biol Psychiatry. 1999;46(2):212–220. PubMed CrossRef
- Miller HL, Delgado PL, Salomon RM, et al. Clinical and biochemical effects of catecholamine depletion on antidepressant-induced remission of depression. Arch Gen Psychiatry. 1996;53(2):117–128. PubMed CrossRef
- Raison CL, Borisov AS, Majer M, et al. Activation of central nervous system inflammatory pathways by interferon-alpha: relationship to monoamines and depression. Biol Psychiatry. 2009;65(4):296–303. PubMed CrossRef
- Bull SJ, Huezo-Diaz P, Binder EB, et al. Functional polymorphisms in the interleukin-6 and serotonin transporter genes, and depression and fatigue induced by interferon-alpha and ribavirin treatment. Mol Psychiatry. 2009;14(12):1095–1104. PubMed CrossRef
- Lindqvist D, Janelidze S, Hagell P, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry. 2009;66(3):287–292. PubMed CrossRef
- Picón-Pagès P, Garcia-Buendia J, Muñoz FJ. Functions and dysfunctions of nitric oxide in brain. Biochim Biophys Acta Mol Basis Dis. 2019;1865(8):1949–1967. PubMed CrossRef
- Coleman JW. Nitric oxide in immunity and inflammation. Int Immunopharmacol. 2001;1(8):1397–1406. PubMed CrossRef
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732–741. PubMed CrossRef
- McNeill E, Channon KM. The role of tetrahydrobiopterin in inflammation and cardiovascular disease. Thromb Haemost. 2012;108(5):832–839. PubMed CrossRef
- Lisboa JVC, Ribeiro MR, Luna RCP, et al. Food intervention with folate reduces TNF-α and interleukin levels in overweight and obese women with the MTHFR C677T polymorphism: a randomized trial. Nutrients. 2020;12(2):361. PubMed CrossRef
- Spielmans GI, Berman MI, Linardatos E, et al. Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of Life, and safety outcomes. Focus Am Psychiatr Publ. 2016;14(2):244–265. PubMed CrossRef
- Atypical antipsychotics: US food and drug administration-approved indications and dosages for use in adults. Centers for Medicare & Medicaid Services. CMS website. 2015. Accessed November 18, 2021. https://www.cms.gov/Medicare-Medicaid-Coordination/Fraud-Prevention/Medicaid-Integrity-Education/Pharmacy-Education-Materials/Downloads/atyp-antipsych-adult-dosingchart11-14.pdf
- Symbyax [package insert]. Indianapolis, IN: Eli Lilly and Company; 2009.
- Seshadri A, Wermers ME, Habermann TJ, et al. Long-term efficacy and tolerability of adjunctive aripiprazole for major depressive disorder: systematic review and meta-analysis. Prim Care Companion CNS Disord. 2021;23(4):23. PubMed CrossRef
- Niederberger KE, Dahms I, Broschard TH, et al. Safety evaluation of calcium L-methylfolate. Toxicol Rep. 2019;6:1018–1030. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!