Abstract
Objective: To provide an updated summary of the literature on dextromethorphan quinidine for the treatment of agitation in dementia.
Data Sources: PubMed, Medline, APA PsycINFO, Embase, and Cochrane Collaboration were searched from inception to January 7, 2024 using the keywords dementia, dextromethorphan, and quinidine. The search was limited to the English language and human subjects.
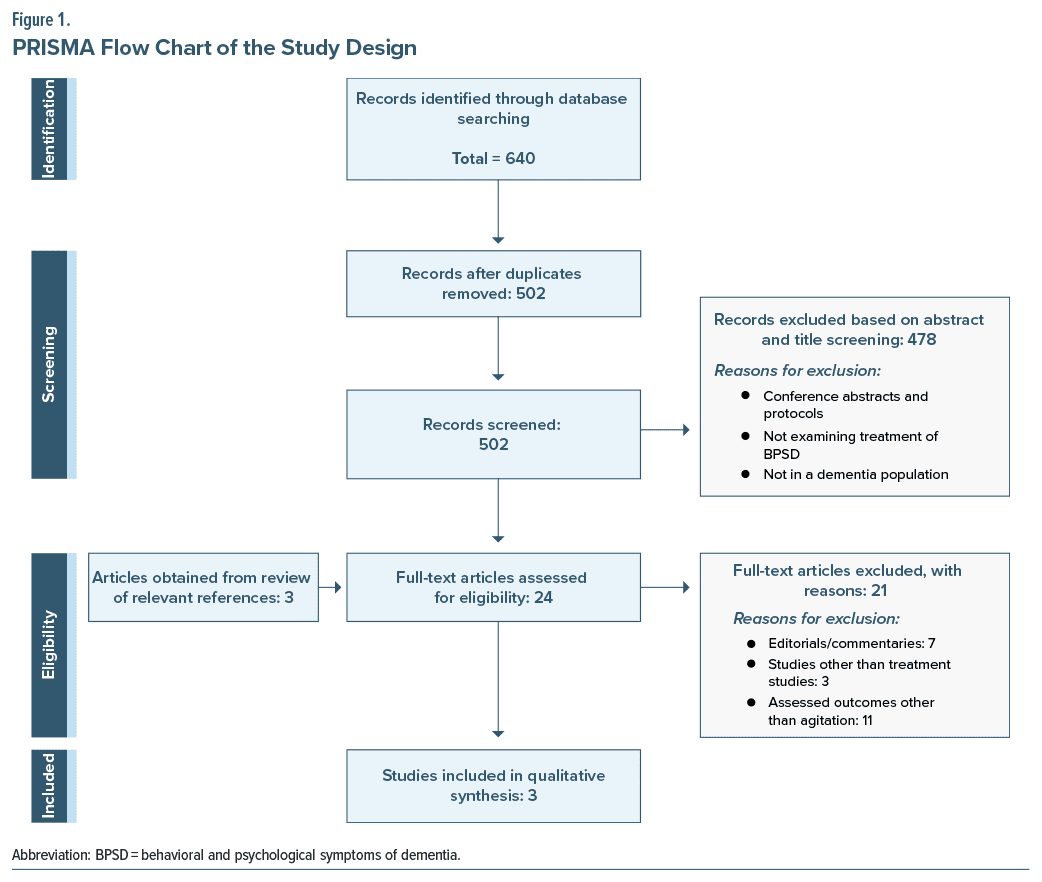
Study Selection: Twenty-four articles underwent full-text review. One randomized controlled trial (RCT) and 2 case reports were included. Twenty one studies were excluded because they were editorials or commentaries, were not treatment studies, or were assessing outcomes other than agitation.
Data Extraction: The 3 included studies underwent full-text review. A qualitative analysis of the data was performed, and abstracted data included patient diagnosis and symptoms, treatment dose and duration of dextromethorphan-quinidine, and symptom response.
Data Synthesis: One RCT and 2 case reports showed an improvement in dementia-related agitation with dextromethorphan-quinidine treatment; however, the data are limited.
Conclusion: Though all the identified studies demonstrated that treatment with dextromethorphan improved agitation, more evidence is needed to establish its potential efficacy and associated risks for this patient population. Future studies should include diverse types of dementia, a variety of treatment settings, and longer duration of treatment.
Prim Care Companion CNS Disord 2024;26(6):24nr03737
Author affiliations are listed at the end of this article.
Behavioral and psychological symptoms of dementia (BPSD) are commonly experienced by patients with dementia and include psychosis, aggression, agitation, mood and sleep changes, apathy, and aberrant motor activity. Up to 1 in 4 people with dementia may have agitation/aggression.1 A retrospective study by Jost and Grossberg2 looking at patients with autopsy-confirmed Alzheimer disease showed that agitation occurred in up to 81% of patients 10 months after their diagnosis. Early recognition and management of these symptoms is crucial since BPSD are associated with increased health care costs, increased risk of institutionalization, significant caregiver burden, and reduced quality of life for both caregivers and patients.3–5
Current data support nonpharmacologic interventions as the first-line treatment for BPSD. Systematic reviews by Livingston et al6 and Abraha et al7 on nonpharmacologic interventions for BPSD found that individual interventions focused on the patient’s specific behavior, along with caregiver education, are most effective. A meta-analysis by Brodaty and Arasaratnam8 found that providing education on nonpharmacologic interventions to family caregivers in their home was also effective. DICE (Describe, Investigate, Create, and Evaluate) is another effective tool for understanding and responding in an individualized way to BPSD. Consensus guidelines recommend the DICE approach as the first line to all other interventions.9 Importantly, reality orientation therapy was not helpful for BPSD and likely causes more distress.6
Additionally, some BPSD may be an expression of unmet needs, like bowel incontinence or pain. Therefore, intentional assessment of these needs followed by appropriate intervention seems to be effective.9,10 Music therapy, one easily implemented intervention, has also shown promising effects on BPSD in multiple studies.7,9
It remains challenging to prove that a specific behavioral or nonpharmacologic intervention can be generalized for all BPSD, simply because of the challenge in conducting robust randomized controlled trials (RCTs) in this area and the heterogeneity of BPSD. Additionally, many long-term care facilities do not have access to the resources and staffing required for implementation.6,10 However, because of the adverse effects associated with pharmacologic interventions, nonpharmacologic strategies remain the best treatment option.9
The primary pharmacologic treatment for BPSD is atypical antipsychotics; however, they are associated with increased mortality and risks of adverse effects.11,12 Among atypical antipsychotics, no single option has been found to be both safe and effective. In addition, in particular subtypes of dementia, such as dementia with Lewy bodies, antipsychotics may worsen parkinsonian symptoms.13 Therefore, risks and benefits must be carefully weighed in each situation.14 The antidepressants citalopram, trazodone, and sertraline have also been found to reduce agitation and psychosis and may be considered prior to the initiation of antipsychotics, since they carry fewer adverse effects.15 Meta-analyses have demonstrated modest improvement with cholinesterase inhibitors and minimal evidence for potential benefit with memantine and cannabinoids.16–18 However, pharmacologic therapies with improved efficacy and tolerability are needed.
Dextromethorphan is approved by the US Food and Drug Administration (FDA) for the treatment of pseudobulbar affect (PBA) when used in combination with quinidine. This FDA-approved indication followed several RCTs demonstrating the efficacy and tolerability of dextromethorphan-quinidine for the treatment of PBA in patients with multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS).19–21 Since its approval, an open label trial22 has demonstrated the efficacy of dextromethorphan-quinidine for the treatment of PBA in patients with stroke, dementia, and traumatic brain injury.
Dextromethorphan is primarily a noncompetitive N-methyl-D-aspartate (NMDA) receptor antagonist. In addition to NMDA receptors, dextromethorphan also interacts with serotonin transporters, noradrenaline transporters, sigma-1 receptors, and α3β4 receptors. Dextromethorphan undergoes rapid first-pass metabolism in the liver via the cytochrome P450 (CYP) 2D6 enzyme and, therefore, has low oral bioavailability. Quinidine increases the bioavailability of dextromethorphan through CYP2D6 inhibition.23
Due to dextromethorphan’s action at multiple receptor sites and its previously demonstrated efficacy for PBA, it is under investigation for several other therapeutic indications, including the treatment of agitation in dementia. An editorial24 published in 2020 reviewed the current RCTs evaluating the efficacy and safety of dextromethorphan-quinidine for agitation in dementia and concluded that there was a need for further research. The goal of this review is to provide an updated summary of the existing literature.
METHODS
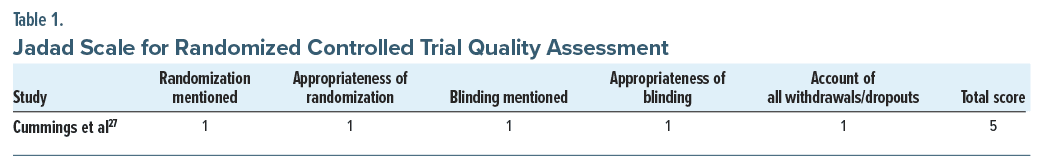
Two authors (A.N.K. and K.S.M.) searched PubMed, Medline, Embase, APA PsycINFO, and Cochrane Collaboration from inception to January 7, 2024. Keywords used in the search were dementia, dextromethorphan, and quinidine. The database searches were limited to human subjects and the English language. A total of 640 abstracts were obtained for initial review from PubMed (dextromethorphan OR quinidine and dementia=63), Medline (dextromethorphan OR quinidine and dementia = 572), and Cochrane Collaboration (dextromethorphan OR quinidine and dementia = 5). The authors (A.N.K. and K.S.M.) independently reviewed all abstracts to remove 138 duplicates and select 24 studies for full-text review. After full-text review, 3 articles were included in this analysis. All articles that evaluated the use of dextromethorphan or quinidine for the treatment of agitation in dementia were included. Articles were excluded if participants did not have dementia, the intervention did not target agitation, articles were not treatment studies, or there was no English-language text or official translation of the article. All disagreements regarding which reports to include were resolved with a consensus discussion with the senior author (R.R.T.). Figure 1 shows a flow diagram for how studies in the literature were identified.25 The Jadad scale, shown in Table 1, was used to assess the quality of the one RCT included in this review. This scale uses a 5-point rating to assess randomization, blinding, and withdrawals and dropouts from the trial. Studies that receive a score of 3 or greater are considered high quality.26 The trial by Cummings et al27 was considered high quality after receiving a score of 5 by using the Jadad scale. The other 2 studies included were case reports and, therefore, were not assessed using this quality scale.
RESULTS
The search strategy produced 3 relevant articles that evaluated the use of dextromethorphan for the treatment of agitation in dementia. This included 1 RCT and 2 case reports. Tables 2 and 3 show the characteristics and results of the included articles.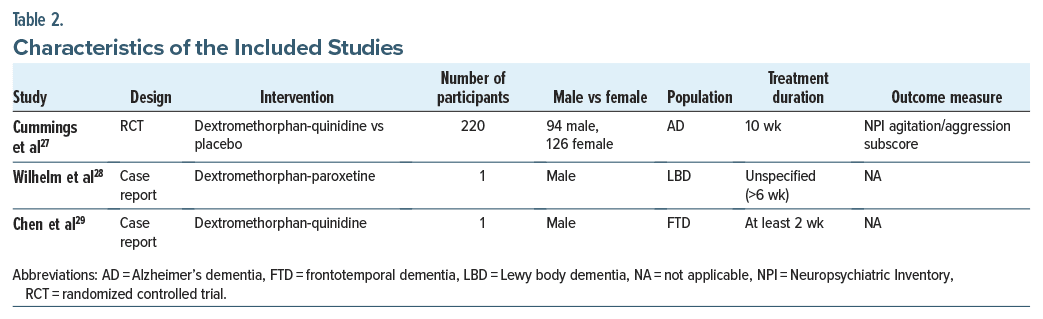
 Cummings et al27 published a 10-week, multicenter, double-blind, placebo-controlled RCT using a sequential parallel comparison design that evaluated the efficacy of dextromethorphan-quinidine for the treatment of agitation in Alzheimer’s dementia. Two hundred twenty participants (126 women and 94 men) were recruited primarily from outpatient clinics, and about 11% of the study group was recruited from assisted living facilities and nursing homes. Enrolled participants had probable Alzheimer’s disease based on the National Institute on Aging and Alzheimer’s Association criteria and clinically significant agitation. In addition, participants had behavioral symptoms that were severe enough to require pharmacologic treatment, interfered with daily routine, were consistent with a rating of 4 or higher on the Clinical Global Impressions–Severity scale for agitation, and had a Mini-Mental State Examination (MMSE) score of 8–28.27
Cummings et al27 published a 10-week, multicenter, double-blind, placebo-controlled RCT using a sequential parallel comparison design that evaluated the efficacy of dextromethorphan-quinidine for the treatment of agitation in Alzheimer’s dementia. Two hundred twenty participants (126 women and 94 men) were recruited primarily from outpatient clinics, and about 11% of the study group was recruited from assisted living facilities and nursing homes. Enrolled participants had probable Alzheimer’s disease based on the National Institute on Aging and Alzheimer’s Association criteria and clinically significant agitation. In addition, participants had behavioral symptoms that were severe enough to require pharmacologic treatment, interfered with daily routine, were consistent with a rating of 4 or higher on the Clinical Global Impressions–Severity scale for agitation, and had a Mini-Mental State Examination (MMSE) score of 8–28.27
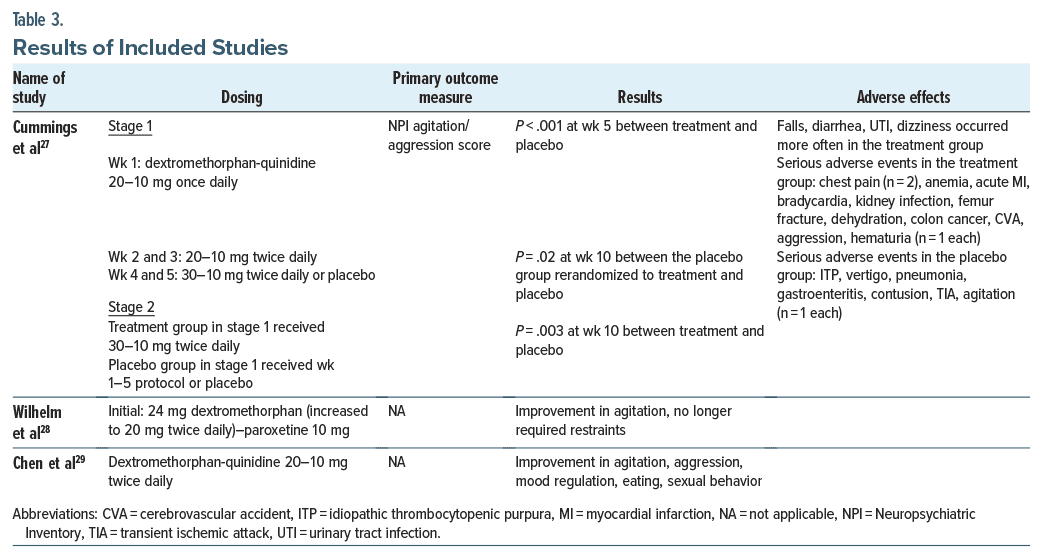
The 10-week trial was divided into two 5-week stages. In the first stage of the trial, participants were stratified and randomized to receive dextromethorphan-quinidine or placebo. Dextromethorphan-quinidine was dosed at 20–10 mg once daily at the start of the trial. Over the course of 5 weeks, dextromethorphan-quinidine was increased to 30–10 mg twice daily. In stage 2, participants receiving the active medication for stage 1 continued to receive active treatment for 5 weeks. Participants who received placebo in the first stage were stratified and randomized to receive dextromethorphan quinidine or placebo. The primary outcome of the study was the change from baseline in the Neuropsychiatric Inventory (NPI) subscore for agitation/aggression. Several secondary outcomes assessed other NPI domains, caregiver distress, and patient functional status and quality of life.
After randomization, 152 participants received dextromethorphan-quinidine (93 from stage 1 and an additional 59 after randomization in stage 2) and 127 participants received placebo. One hundred ninety four participants completed the study. Adverse events were reported by 93 participants (61.2%) in the treatment group and 55 participants (43.3%) in the placebo group. Adverse events occurring more often in the treatment group included falls (8.6% vs 3.9%), diarrhea (5.9% vs 3.1%), urinary tract infection (5.3% vs 3.9%), and dizziness (4.6% vs 2.4%). Of the 13 participants in the treatment group who fell, 9 had a history of falls. Serious adverse events occurred among 12 participants within the treatment group and 6 participants within the placebo group.
At the end of stage 1, the mean NPI agitation/ aggression subscores decreased significantly more in the treatment group than in the placebo group (P < .001). At the end of stage 2, the mean NPI agitation/aggression subscores decreased significantly more in the group rerandomized to receive dextromethorphan-quinidine than in the placebo group (P = .02). Finally, the NPI agitation/aggression subscores decreased significantly more in the group only receiving dextromethorphan quinidine than in the group only receiving placebo throughout the 10-week trial (P = .003). Post hoc analysis showed similar improvements in the NPI agitation/aggression subscore between active treatment participants taking psychotropics and those who were not. Dextromethorphan-quinidine had a statistically significant effect on the primary endpoint. In addition, this outcome was considered clinically meaningful based on the percent reduction in the NPI agitation/aggression subscore, and dextromethorphan was generally well tolerated for the treatment of agitation associated with Alzheimer’s dementia.27
Wilhelm et al28 published a case report on the use of dextromethorphan and paroxetine for the treatment of agitation and aggression in a patient with Lewy body dementia. A 78-year-old man, who was diagnosed with Lewy body dementia at age 76, was admitted to the hospital for pneumonia. During this hospitalization, he developed hyperactive delirium and was transferred to the geropsychiatric unit. He had unpredictable outbursts of aggression and violence toward other patients and staff, requiring physical restraints almost daily. During admission, he was trialed on rivastigmine in combination with many different antipsychotics, antidepressants, benzodiazepines, and an anticonvulsant. He also received dronabinol; all these interventions had limited benefit.28
Finally, dextromethorphan was prescribed with paroxetine, another CYP2D6 inhibitor, since the quinidine combination is not readily available in Germany where the patient was hospitalized.28 The patient received 24 mg of dextromethorphan and 10 mg of paroxetine, after which he had no periods of aggression requiring restraints. There were no reported side effects from the treatment. Dextromethorphan was increased to 40 mg daily divided into 2 doses. His behavior and sleep cycle continued to improve, and physical restraints were no longer required. The patient remained in the hospital for 14 months, after which he was successfully transferred to a specialized nursing home. However, 6 weeks after transfer, he killed himself by hanging. The authors reported not observing suicide in other patients they had treated with this combination.28
Chen et al29 also published a case report on the effectiveness of dextromethorphan-quinidine in frontotemporal dementia. The patient was a 55-year old man who was admitted to the hospital due to agitation. He was diagnosed with right anterior variant frontotemporal dementia and experienced aggression, agitation, and persistent delusions. He had previously received olanzapine, escitalopram, and trazodone with limited improvement in these symptoms. He was initiated on dextromethorphan-quinidine 20–10 mg twice a day, and after 2 weeks, he had significant improvement in agitation, aggression, sexual behaviors, mood, and eating.29
DISCUSSION
This review provides a summary of the current evidence on the use of dextromethorphan for the treatment of BPSD. The RCT by Cummings et al27 was published in 2015 and included 220 participants, and it remains the first and only RCT testing this medication for dementia-related agitation. The 2 case reports, published in 2017 and 2018, each described a patient who received treatment with dextromethorphan in combination with quinidine or paroxetine for the treatment of agitation. All 3 studies found benefits in using dextromethorphan for treating agitation in dementia based on the designated outcome measures or general clinical impression. However, the data are limited.
Strengths of the Cummings et al27 trial include use of a validated BPSD assessment tool and sequential parallel comparison study design that minimizes placebo response and maximizes the number of participants receiving active treatment. Limitations of the Cummings et al27 study include use of a wide range of participant baseline MMSE scores (8–28). Generally, MMSE scores above 26 are considered normal.30 Therefore, participants included in this study fell within a normal range of cognition. The broad range of included scores makes it difficult to determine the degree of cognitive impairment and associated agitation that may benefit from treatment with dextromethorphan. In addition, falls were the most common adverse event and occurred more often in the treatment group. However, at baseline, the treatment group had a higher percentage of participants with a fall history. Therefore, it is difficult to attribute fall risk to the treatment alone. More information is needed to determine the fall risk associated with dextromethorphan in this population. These limitations highlight the need for additional trials.
The case reports by Wilhelm et al28 and Chen et al29 showed clinical improvement in agitation after initiating dextromethorphan. Each of the patients in these reports presented with severe agitation requiring seclusion and/ or restraints and both reportedly benefited from treatment with dextromethorphan. However, these were only clinical observations of improvement without use of a validated assessment tool. Additionally, there is limited description of the patients’ history and other contextual factors that may have co-occurred with the initiation of dextromethorphan. Therefore, it is difficult to draw conclusions about the effectiveness of dextromethorphan for agitation from these case reports.
Notably, dextromethorphan-quinidine is listed on the Beers list as a potentially inappropriate medication to use in older adults, due to the fall risk of both medications and possible cardiac side effects of quinidine. This is especially important when older adults have a history of falls or cardiac disease. Finally, both dextromethorphan and quinidine interact with various CYP enzymes, and, therefore, interactions between these and other medications must be closely monitored.31
In this limited sample of studies, dextromethorphan appeared to be relatively well tolerated. In the trial by Cummings et al,27 adverse effects were reported in 61.2% of participants in the treatment group and 43.3% of participants in the placebo group. The most common adverse effects included falls, diarrhea, urinary tract infections, and dizziness. No adverse events were reported in the case report by Chen et al.29 The patient in the case report by Wilhelm et al28 hung himself 6 weeks after discharge from the hospital. The report does not specify how long this occurred after he started dextromethorphan and paroxetine. The report also did not include details about other psychiatric comorbidities or life factors (such as loss, substance use, isolation, and medical comorbidities such as chronic pain) that may have increased suicide risk. There is no description in the case report about interval or discharge assessment of suicide risk. Periodic suicide risk assessment is of utmost importance when frequently adjusting psychotropics and, of course, when discharging from a psychiatric hospitalization. Risk assessment should still be attempted in individuals with dementia. The patient in the Wilhelm et al28 case initially presented with hyperactive delirium prior to psychiatric admission, which could have complicated the agitation observed during his hospitalization. Other causes of agitation should be continuously considered and assessed, including delirium, undiagnosed premorbid psychiatric conditions, medical illness, and polypharmacy, or serious adverse events from psychotropics like neuroleptic malignant syndrome. The authors28 note suicidal behavior did not occur in other patients they treated with dextromethorphan paroxetine.
Despite dextromethorphan-quinidine being predominantly studied for the treatment of PBA in MS and ALS, it is prescribed most often for people with diagnoses of dementia and/or Parkinson’s disease.32 In a review of commercial health care databases, 57% of individuals prescribed dextromethorphan-quinidine had a diagnosis of dementia and/or Parkinson’s disease.32 This study32 evaluated Medicare Part D prescriptions for dextromethorphan-quinidine and found that they increased 51.2-fold in a 5-year span between 2011 and 2016. Given the current prescribing patterns of dextromethorphan-quinidine, more RCTs are warranted to evaluate safety, tolerability, and efficacy.
This review on the use of dextromethorphan for the treatment of agitation in dementia has several limitations. This review was limited to English-language articles, and, therefore, studies without English translation were not considered. This review is also limited by the available evidence. There is only 1 RCT available in which participants without Alzheimer’s dementia were excluded. Studies that include participants with other forms of dementia, including vascular dementia, Lewy body dementia, frontotemporal dementia, and Parkinson’s disease dementia, are needed. In addition, this trial was limited to 220 participants observed over 10 weeks. Therefore, more RCTs with longer duration and more participants are needed. While the case reports discussed hospitalized patients, the RCT primarily recruited from outpatient clinics. There is a need for more data on the efficacy of dextromethorphan for patients in residential facilities and inpatient settings where agitation in dementia is frequently encountered.
CONCLUSION
Dextromethorphan-quinidine has limited evidence for treating agitation in dementia. There is only 1 high quality RCT showing that dextromethorphan-quinidine decreases agitation in patients with dementia when compared to placebo. The generalizability of this RCT to all forms of dementia and treatment settings is limited. There is a need for safe and efficacious pharmacologic treatments for dementia-related agitation. Therefore, dextromethorphan-quinidine should be further investigated since it is being used clinically, and there is currently limited evidence regarding efficacy and safety. More studies with larger sample sizes, heterogeneous forms of dementia, and longer treatment times are needed to establish its efficacy and safety for the treatment of agitation in dementia.
Article Information
Published Online: November 14, 2024. https://doi.org/10.4088/PCC.24nr03737
© 2024 Physicians Postgraduate Press, Inc.
Submitted: February 29, 2024; accepted August 14, 2024.
To Cite: Khan AN, Murphy KS, Tampi RR. A review of dextromethorphan-quinidine for the treatment of agitation in dementia. Prim Care Companion CNS Disord. 2024;26(6):24nr03737.
Author Affiliations: Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Khan, Tampi); Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, Texas (Murphy); Department of Psychiatry, Creighton University School of Medicine, Omaha, Nebraska (Tampi).
Amber N. Khan and Kayla S. Murphy contributed equally to this work and are considered co-first authors.
Corresponding Author: Rajesh R. Tampi, MD, MS, DFAPA, DFAAGP, Department of Psychiatry, Creighton University Education, Bldg, 7710 Mercy Rd, Ste 601, Omaha, NE 68124-2370 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgments: The authors acknowledge the contributions of Krishna Priya Bodicherla, MD (Harlem Hospital Center, New York, New York), to this manuscript through her participation in discussions of data collection. Dr. Bodicherla reports no conflicts of interest related to the subject of this article.
Clinical Points
- There are limited data to support the use of dextromethorphan for dementia-related agitation.
- More randomized controlled trials are needed to ascertain whether dextromethorphan demonstrates clinical efficacy for improving dementia-related agitation.
References (32)

- Lyketsos CG, Steinberg M, Tschanz JT, et al. Mental and behavioral disturbances in dementia: findings from the cache county study on memory in aging. Am J Psychiatry. 2000;157(5):708–714. PubMed CrossRef
- Jost BC, Grossberg GT. The evolution of psychiatric symptoms in Alzheimer’s disease: a natural history study. J Am Geriatr Soc. 1996;44(9):1078–1081. PubMed CrossRef
- Beeri MS, Werner P, Davidson M, et al. The cost of behavioral and psychological symptoms of dementia (BPSD) in community dwelling Alzheimer’s disease patients. Int J Geriatr Psychiatry. 2002;17(5):403–408. PubMed CrossRef
- O’Donnell BF, Drachman DA, Barnes HJ, et al. Incontinence and troublesome behaviors predict institutionalization in dementia. J Geriatr Psychiatry Neurol. 1992;5(1):45–52. PubMed
- Coen RF, Swanwick GR, O’Boyle CA, et al. Behaviour disturbance and other predictors of carer burden in Alzheimer’s disease. Int J Geriatr Psychiatry. 1997;12(3):331–336. PubMed
- Livingston G, Johnston K, Katona C, et al. Systematic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. Am J Psychiatry. 2005;162(11):1996–2021. PubMed CrossRef
- Abraha I, Rimland JM, Trotta FM, et al. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series. BMJ Open. 2017;7(3):e012759. PubMed CrossRef
- Brodaty H, Arasaratnam C. Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. Am J Psychiatry. 2012;169(9):946–953. PubMed CrossRef
- Kales HC, Lyketsos CG, Miller EM, et al. Management of behavioral and psychological symptoms in people with Alzheimer’s disease: an international Delphi consensus. Int Psychogeriatr. 2019;31(1):83–90. PubMed CrossRef
- Seitz DP, Brisbin S, Herrmann N, et al. Efficacy and feasibility of nonpharmacological interventions for neuropsychiatric symptoms of dementia in long term care: a systematic review. J Am Med Dir Assoc. 2012;13(6):503–506.e2. PubMed CrossRef
- Bessey LJ, Walaszek A. Management of behavioral and psychological symptoms of dementia. Curr Psychiatry Rep. 2019;21(8):66. PubMed CrossRef
- Magierski R, Sobow T, Schwertner E, et al. Pharmacotherapy of behavioral and psychological symptoms of dementia: state of the art and future progress. Front Pharmacol. 2020;11:1168. PubMed CrossRef
- Kyle K, Bronstein JM. Treatment of psychosis in Parkinson’s disease and dementia with Lewy Bodies: a review. Parkinsonism Relat Disord. 2020;75:55–62. PubMed CrossRef
- Yunusa I, Alsumali A, Garba AE, et al. Assessment of reported comparative effectiveness and safety of atypical antipsychotics in the treatment of behavioral and psychological symptoms of dementia: a network meta-analysis. JAMA Netw Open. 2019;2(3):e190828. PubMed CrossRef
- Seitz DP, Adunuri N, Gill SS, et al. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011;(2):CD008191. PubMed CrossRef
- Bahji A, Meyyappan AC, Hawken ER. Cannabinoids for the neuropsychiatric symptoms of dementia: a systematic review and meta-analysis. Can J Psychiatry. 2020;65(6):365–376. PubMed CrossRef
- Maidment ID, Fox CG, Boustani M, et al. Efficacy of memantine on behavioral and psychological symptoms related to dementia: a systematic meta-analysis. Ann Pharmacother. 2008;42(1):32–38. PubMed CrossRef
- Trinh NH, Hoblyn J, Mohanty S, et al. Efficacy of cholinesterase inhibitors in the treatment of neuropsychiatric symptoms and functional impairment in Alzheimer disease: a meta-analysis. JAMA. 2003;289(2):210–216. PubMed CrossRef
- Panitch HS, Thisted RA, Smith RA, et al. Randomized, controlled trial of dextromethorphan/quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol. 2006;59(5):780–787. PubMed CrossRef
- Brooks BR, Thisted RA, Appel SH, et al. Treatment of pseudobulbar affect in ALS with dextromethorphan/quinidine: a randomized trial. Neurology. 2004;63(8):1364–1370. PubMed CrossRef
- Pioro EP, Brooks BR, Cummings J, et al. Dextromethorphan plus ultra low dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68(5):693–702. PubMed CrossRef
- Hammond FM, Alexander DN, Cutler AJ, et al. PRISM II: an open-label study to assess effectiveness of dextromethorphan/quinidine for pseudobulbar affect in patients with dementia, stroke or traumatic brain injury. BMC Neurol. 2016;16:89. PubMed CrossRef
- Taylor CP, Traynelis SF, Siffert J, et al. Pharmacology of dextromethorphan: relevance to dextromethorphan/quinidine (Nuedexta®) clinical use. Pharmacol Ther. 2016;164:170–182. PubMed CrossRef
- Tampi RR, Joshi P, Marpuri P, et al. Evidence for using dextromethorphan quinidine for the treatment of agitation in dementia. World J Psychiatry. 2020;10(4):29–33. PubMed CrossRef
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. PubMed CrossRef
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. PubMed CrossRef
- Cummings JL, Lyketsos CG, Peskind ER, et al. Effect of dextromethorphan quinidine on agitation in patients with Alzheimer disease dementia: a randomized clinical trial. JAMA. 2015;314(12):1242–1254. PubMed CrossRef
- Wilhelm R, Ahl B, Anghelescu IG. Dextrometorphan-paroxetine, but not dronabinol, effective for treatment-resistant aggression and agitation in an elderly patient with Lewy body dementia. J Clin Psychopharmacol. 2017;37(6):745–747. PubMed CrossRef
- Chen Q, Ermann A, Shad MU. Effectiveness of dextromethorphan/quinidine in frontotemporal dementia. Am J Geriatr Psychiatry. 2018;26(4):506. PubMed CrossRef
- Salis F, Costaggiu D, Mandas A. Mini-Mental State Examination: optimal cut-off levels for mild and severe cognitive impairment. Geriatr (Basel). 2023;8(1):12.
- Lee HC, Tl Huang K, Shen WK. Use of antiarrhythmic drugs in elderly patients. J Geriatr Cardiol. 2011;8(3):184–194. PubMed CrossRef
- Fralick M, Sacks CA, Kesselheim AS. Assessment of use of combined dextromethorphan and quinidine in patients with dementia or Parkinson disease after US Food and Drug administration approval for pseudobulbar affect. JAMA Intern Med. 2019;179(2):224–230. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!