Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss the diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(3):23f03684
Author affiliations are listed at the end of this article.
Have you ever considered what obstacles a disabled person might face while attempting to receive timely and effective medical care? Have you ever thought about what allows individuals with a disability to thrive and overcome challenges? Have you wondered how the doctor-patient relationship might be affected by a patient’s disability? Have you thought about how health care systems might enhance the care they provide for those with a disability? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, a 36-year-old woman with a history of asthma, presented to the hospital after being struck by a car while riding her bicycle. Ms A was found to lack motor function in her lower extremities. Imaging revealed fractures along her thoracic spine, including a T6 burst fracture that, in combination with ventral and dorsal hematomas, caused severe spinal canal stenosis at the T5-T6 levels, T4-T5 spinous process fractures, and T7-T8 endplate fractures. Within hours of her arrival to the hospital, Ms A underwent decompression of her posterior thoracic spine, along with a T2-T10 fusion, a T6 partial corpectomy, and repair of a cerebrospinal fluid leak. After surgery, Ms A was extubated and transferred to the intensive care unit for blood pressure monitoring and pressor support. She became hemodynamically stable and was transferred to the medical floor on hospital day 7. Ms A was evaluated by the physical medicine and rehabilitation team for the management of severe back pain. During the 2 weeks that followed the neurosurgical intervention, there was partial recovery of motor activity in her left lower extremity (3/5 strength with hip, knee, and ankle flexion and extension). Ms A remained unable to move her right leg. The hospital’s physical therapy service began working with Ms A, noting that she required 2-person assistance and a rolling walker to transition her from a sitting to standing position.
The hospital’s social work team also evaluated Ms A, who described the fast-paced life she had led before her accident, working 50–60 hours a week as a software engineer. She, her husband, and their 12-year-old daughter enjoyed outdoor activities (including biking, hiking, and camping). Ms A admitted that she was concerned about whether she would be able to function again, both at work and with her family. She was tearful while recounting the outpouring of support that she had been receiving from her family and friends, and she was grateful that her accident had not been fatal. She emphasized that her goal was to “get back to where I used to be before all this.”
DISCUSSION
How Is Disability Defined in the Law, and What Conditions Are Categorized as Disabilities?
The Americans with Disabilities Act (ADA) of 19901 and ADA Amendments Act of 20082 established a broad definition of disability that provided individuals with disabilities the protected right to obtain accommodations. Under these federal laws, a disability is defined as “a physical or mental impairment that substantially limits 1 or more major life activities.”2(p3555) Impairments in the ability to conduct major life activities (including caring for oneself, seeing, hearing, walking, communicating, and working) among others2 can be categorized as disabilities. It is often the severity of a person’s condition, rather than the condition itself, that reaches the level of a disability. Disabilities can involve impairment of mobility or the senses and be obvious to others or can involve the sequelae of cancer or systemic conditions. Still others may be less readily apparent (eg, intellectual disabilities, depression, psychotic disorders, and autism spectrum disorder).3 In the United States, more than 67.2 million adults, ie, about 1 in 4 people, have a disability.4 Impaired mobility is the most prevalent disability type, affecting about 13.3% of adults, followed by cognitive or mental disorders (12.1%) and impairments in independent living (7.2%), hearing (6.1%), seeing (5.2%), and engaging in self-care (3.9%).
What Models Have Been Used to Conceptualize Disability?
Throughout history, a variety of frameworks have been used to conceptualize disability. Frequently referred to as models of disability, these frameworks reflect evolving societal perspectives about disabilities. Models of disability inform the language used to describe disability; they can also affect the delivery of medical and psychiatric care to individuals with disabilities. More broadly, models of disability can mirror and dictate health care policy and legislative measures that surround disability.
The moral model. The moral model is the oldest model of disability; it associates disability with sin and commonly considers disability a consequence of moral failing.5,6 Despite seeming outdated in the context of modern Western culture and medicine, the moral model is worth thinking about, especially for a health care workforce that is tasked with caring for individuals from myriad cultural, spiritual, and religious backgrounds. For example, the notion of disability as a punishment, or as a test of faith, by a higher power may influence a patient’s sense of self after acquiring a disability, or it may affect a family’s decision-making regarding treatment.
The medical model. The medical model views disability as pathologic, as a disorder, and as a dysfunctional defect that requires diagnostic clarification and treatment.7 Intervention within the medical model is frequently aimed at the individual with the disability—through surgery, rehabilitation, and adaptive equipment (eg, hearing aids, wheelchairs, and prostheses). Although individuals with disabilities derive significant functional, occupational, and psychological gains from medical and psychiatric care, the medical model of disability is not without its drawbacks. Critics of the medical model note its paternalistic tendencies and emphasize that in the medical model, the onus for adjusting or accommodating to a disability frequently falls on those with the disability. For instance, following a motor vehicle accident that renders an individual paralyzed from the waist down, attention turns to rehabilitation of the individual to accommodate to their environment. However, critics of the medical model might identify an obvious lack of focus on addressing the potential infrastructure failures of a city or town that is not meeting the needs of its residents with limited mobility.
The social model. The social model of disability frames disability within the context of environmental factors, cultural attitudes, and social biases related to disability.5 This model emphasizes the failures of the environment to accommodate people with a disability. Interventions rooted in the social model are aimed at addressing societal concerns (eg, stigma, discrimination, social isolation, inaccessible housing, and high unemployment rates).6
Of note, language used to describe disabilities and people with disabilities has evolved alongside the models of disability. Person-first language places the person before the disability (eg, “person with autism” and “person with quadriplegia”). Person-first language is viewed as an attempt to distinguish a person from their disability and to avoid reducing an individual’s identity to their disability status.
Identity-first language places the disability before the person (eg, “deaf person” and “disabled person”). Advocates of identity-first language in the disability community argue that it promotes positive social identity and is a source of empowerment for traditionally marginalized groups.8 Many clinical providers, including the authors of this article, ask patients if they prefer person-first or identity-first language.
How Are Coping, Adjusting, and Thriving Understood Within the Context of Both Congenital and Acquired Disabilities?
Coping is defined as a problem-solving behavior or thought process that is intended to bring about relief or equilibrium.9 In the medical model of disability, where disability is considered as a disorder, clinicians often consider how individuals cope and adjust to the disability itself. In the social model of disability, where disability is framed in the context of environmental factors and social biases, clinicians often examine how individuals adjust to an unaccommodating environment. While perspectives that are rooted in the medical model of disability remain pervasive in clinical care, it is important for the development of a therapeutic alliance and provision of holistic patient care to consider coping, adjusting, and thriving through the lens of the social model of disability.
For individuals with congenital disabilities, adjusting to and thriving in an unaccommodating external environment starts at an early age. Parents and other caregivers frequently serve as early advocates, fostering an environment in which a child with a disability feels empowered and may be equipped with adaptive devices and other appropriate school accommodations. Self esteem and social support play critical roles in the adjustment to disability. Several studies10,11 have compared adjustment and adaptation of people with congenital and acquired disabilities and found that people with congenital conditions often adjust better to disability, in part because of greater acceptance of disability. A difference in disability self-concept—or the understanding of one’s identity that includes a person’s self-esteem, group identity, and self-efficacy—between individuals with a congenital disability, when compared to those with acquired disabilities, has been postulated as an explanation for better adjustment seen in the former group.12
Individuals with acquired disabilities are often faced with changes in their functional status. Rehabilitative programs, physical therapy, and occupational therapy may be helpful in the adjustment period, particularly for those with newly acquired physical disabilities. Support systems and self-esteem remain important. Support systems frequently evolve because of a decreased ability to participate in prior occupational and recreational activities. Individuals may find themselves turning to trusted coping strategies to manage a new and unaccommodating external environment, and they may become demoralized if their coping techniques fail. The benefits of psychological support through counseling and interventions (such as cognitive-behavioral therapy) are well documented.13
What Contributes to Effective Coping and Adjusting?
No person copes and adjusts exceptionally well in every circumstance. However, individuals who cope and adjust well to disability share some common characteristics.9 Good copers are resilient and remain optimistic. They tend to be practical and prioritize obstacles that require immediate attention and can be overcome. Individuals who cope and adjust well are resourceful, surveying a wide range of strategies when confronted with a challenge. They are pragmatic and creative, and they avoid emotional extremes that might compromise judgement.
Coping is classified in myriad ways. Problem-focused coping encompasses activities that directly change a stressful scenario, while emotion-focused coping involves activities that modify the distress that results from a stressful situation.14 Engaged coping involves confronting a stressor directly (eg, acceptance, support seeking, and cognitive reappraisal), while disengaged coping involves avoidance of the stressor. Coping has also been classified based on its temporality.15 Reactive coping attempts to compensate for loss or harm that has already occurred. Proactive coping aims to address an anticipated challenge.
Optimal methods of coping and adjustment often depend on the nature of the disability as well as on circumstances specific to the individual involved. Coping strategies are effective in most instances. Factors such as utilizing social support and employing self-compassion have been shown to promote the efficacy of adaptive coping techniques.14,16
What Contributes to Ineffective Coping and Adjusting?
The traits commonly observed in individuals who cope inadequately and adjust poorly to challenges are neither fixed nor solely the opposite of characteristics that are observed in good copers. For example, in a person with a newly acquired disability, challenges with coping can precede a sustained period of healthy adjusting to, and subsequently thriving with, a disability. Such a trajectory frequently requires recognition, both by individuals and their clinicians, of characteristics that are associated with poor coping. Individuals who have difficulty coping and adjusting are often passive in their decision-making, inflexible in their outlook and standards, impulsive, and prone to denial and elaborate rationalization.9
Seven different existential states have been identified by Griffith and Gaby17 that move individuals toward (resilience) or away from (vulnerability) assertive coping techniques. In clinical contexts, effective coping techniques are more frequently utilized by patients who feel a sense of coherence, communion, hope, agency, purpose, courage, and gratitude. Ineffective coping techniques are more often used by patients who feel confused, isolated, despairing, helpless, meaningless, cowardly, and resentful. Within this framework, primary care providers and psychiatric providers can use supportive bedside therapies to help patients identify existential postures and mobilize postures of resilience by witnessing, validating, and normalizing patients’ experiences. In their work, Griffith and Gaby17 provided examples of questions that can be asked of patients to elicit adaptation toward postures of resilience.
What Does a Successful Rehabilitation Program Entail?
When assessing success in a rehabilitation program, it is important to consider how success is measured. Traditional biomedical models, which are often oriented toward disease processes, propose disease eradication or limiting progression as a successful outcome; however, this can be of limited value in patients with a chronic illness or disability. An alternative conceptualization, called the outcomes model, has argued that the goals of health care should be enhanced life expectancy and quality of life. This model is directed toward increasing function; it considers the chronicity of illness, the impact of diagnosis and treatment, patient reports and experiences, and the determinants of patient outcomes.18 This system has the advantage of weighing both the benefits and side effects of treatment, and it avoids consideration of survival as the ultimate objective; instead, it takes an approach toward global well-being. Multiple studies conducted in rehabilitation settings have used quality-of-life measures as primary outcomes; however, defining measures or operationalizing improvement in quality of life remains difficult due to the heterogeneity of instruments and interpretations.19
Improved quality of life is likely individual-specific in relation to one’s value system and preferences. Thus, 1 characteristic of a successful rehabilitation program is individualization of care to the patient’s disability, needs, and goals. Specialized or individualized programs for a patient’s disabilities can achieve significant gains in activities of daily living, shorter hospital stays, and fewer hospitalizations.20,21 Elements of specialized rehabilitation programs that are thought to contribute to improved outcomes include skilled and educated staff members, organized services, higher intensity of therapies, and more aggressive attention paid to the treatment and prevention of medical issues. Individualizing care for patients also promotes collaboration and shared decision making that can enhance interactions among patients and providers. A qualitative study22 for successful outcomes in patients with chronic pain noted that a good match within the patient-professional interaction seems essential for positive patient outcomes. Factors that are associated with a high quality of interactions include listening to the patient’s experience and engaging in an open interaction between patients and their providers.22 Therefore, a successful rehabilitation program should focus on improving quality of life, aligning with the patient’s needs and disability, coordinating care among services, cooperating with other providers, and having positive interactions among providers and patients.
What Types of Protection Does the ADA Offer to Individuals With Disabilities?
The ADA (1990) sought to achieve 4 goals for people with disabilities: equal opportunity, full participation in the community, independent living, and economic self sufficiency.1,23 In a medical context, titles II (state and local government services) and III (private businesses and nonprofit organizations) of the ADA mandate full and equal access to health care for people with disabilities. More specifically, health care providers must ensure that their facilities are accessible to people with disabilities and that auxiliary aids and services are provided for effective communication and patient care.
Three decades after the ADA was signed, limited awareness and compliance of ADA accessibility standards remains an issue within health care settings.24–26 As a result, the Affordable Care Act of 2010 contains provisions specific to disability, including increased public health surveillance of health care disparities that impact people with disabilities, bolstered federal funding of medical education on topics related to disability, and a call for establishing standards for accessible medical diagnostic equipment.1,27
Protections for people with disabilities in the medical setting should also be considered from the perspective of medical professionals or trainees with disabilities. One of the primary protections provided by the ADA is the requirement for reasonable accommodations. As such, employers and academic institutions must engage in an interactive process with qualified employees and students to identify and implement accommodations that mitigate barriers to working and learning. Additionally, the ADA reinforces the principle of nondiscrimination in the context of hiring and admitting trainees. Finally, the ADA’s emphasis on accessibility in health care spaces extends to the needs of health care workers and trainees.
In Which Ways Might Individuals With Disabilities Need to Navigate Legal Systems (and What Role Might Physicians Play in This Process)?
Many individuals with disabilities (particularly acquired disabilities) are tasked with traversing legal pathways. Initial legal interactions may be related to establishing liability, documenting current and expected functioning, and outlining the need for specific accommodations. Impairment ratings function as objective measures of the severity of loss of structure and function; they are frequently performed by primary care providers or specialists—such as physical medicine and rehabilitation physicians or psychiatrists—during the process in which a disabled person is preparing a claim for personal injury or worker’s compensation.28 From the provider perspective, assisting patients through the worker’s compensation system can feel overwhelming and confusing, in part due to time constraints, intensive paperwork, and a lack of financial incentives.29 In addition, health care providers may be unsure of their roles within a legal landscape that includes the patient, the patient’s employer, each party’s legal counsel, insurers, and regulatory agencies—each having their own interests and incentives.
Meanwhile, navigating the legal and bureaucratic arena is made more challenging for patients who have newly acquired disabilities, as they are frequently targets of fraud, coercion, and abuse. Individuals with a newly acquired, work-related disability may be approached soon after their injury to sign waivers for modest compensation, and they may be subject to physical and emotional abuse at work due to their perceived increased needs. In interactions with providers, individuals seeking legal recourse or worker’s compensation often have little control over the timeliness or comprehensiveness of the reports submitted by physicians.30
At a systemic level, an increased focus on the legal aspects of disability and impairment determinations during medical education would help future physicians better assist patients who are pursuing worker’s compensation, personal injury claims, and appropriate accommodations. Individual physicians and providers, particularly those in academic medical centers, should seek guidance when they are uncertain about their roles and responsibilities from their hospital’s office of legal counsel. In addition to clarifying the role of the physician in legal interactions, such offices can direct physicians to state resources, volunteer community groups, and appropriate legal clinics.
What Obstacles Do Individuals With Disabilities Face in Their Attempts to Receive Timely and Effective Medical Care?
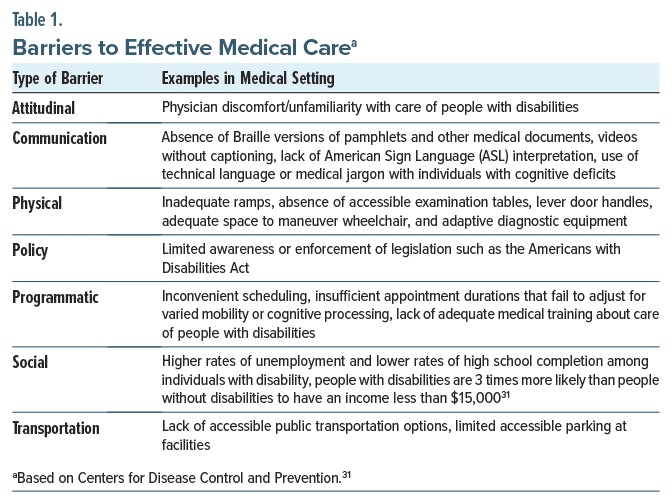
The Centers for Disease Control and Prevention has identified 7 barriers (ie, socioeconomic challenges, a lack of transportation, physical obstacles, insufficient communication options, programmatic hurdles, a lack of policy enforcement, and attitudes toward disability) that people with disabilities may face while navigating through their communities.31 Notably, each of these barriers is manifest in the medical arena (Table 1).
Socioeconomic challenges, particularly financial adversity, result in people with disabilities deferring both care for their immediate health needs and participation in routine preventive screening.32 In addition, studies show that primary care offices and specialty clinics frequently fail to meet the accessibility standards set by the ADA, with patients noting inadequate ramps, limited accessible parking, insufficient communication options, and a lack of adaptive diagnostic equipment among other concerns.26,33,34 Finally, patients perceive that providers of clinical care are often uncomfortable when caring for individuals with disabilities; providers attest to this discomfort, citing insufficient medical training related to the care of patients with disabilities as a primary contributor.32,35
How Might the Doctor-Patient Relationship Be Affected by the Patient’s or Provider’s Disability?
Patients with disabilities are often subject to health care providers’ biases, which lead patients to worry that physicians do not understand how their disability interacts with their daily lives.36 A survey of US physicians found that 82.4% believed that people with significant disabilities have a worse quality of life than people without a disability,36 despite that many individuals have adjusted to their disability and have enjoyed an excellent or good quality of life.37 The same survey found that only about half of physicians “strongly agree” that they welcome patients with disability into their practice.36 These biases can lead to mistreatment and discrimination.38 For example, some women with disabilities may not be offered Pap smears or contraceptives based on the assumption that they are not sexually active.36 During the COVID-19 pandemic, initial triage guidelines for intensive care unit beds and ventilators were alleged to have discriminated against individuals with disabilities, many of which were revised after disability rights advocacy groups filed complaints with the Department of Health and Human Services Office of Civil Rights.36
These health inequities underscore the deficits of medical training in preparing physicians to care for those with disabilities. Notably, only about 40% of physicians feel “very confident” in their ability to provide the same quality of care to people with disabilities as they do for patients without disabilities.36 In addition to curricular reform, the inclusion of medical students with disabilities may help to address this need and improve doctor-patient relationships. One study38 found that medical students with disabilities may have increased empathy, perhaps through lived experiences of having a disability and a personal understanding of illness. To our knowledge, there has been no direct study of how a provider’s disability impacts a patient’s experience. However, prior research has found that patients from minoritized backgrounds often prefer physicians from a similar background; doctor-patient concordance of demographic traits (like race/ethnicity and language) may enhance care and improve health-related outcomes.39 Ultimately, a diversified medical workforce that is supportive of physicians with disabilities would likely benefit both patients and other providers.38
How Can Health Care Systems Adapt to Facilitate Care of Those With Disabilities?
People with disabilities experience health care disparities (such as difficulty accessing services), and health care systems can implement physical and educational modifications to address barriers to access care. Multiple national reports have demonstrated that people with disabilities experience disadvantages and disparities in health care services and in well-being when compared with those in the general population. Many factors (including limitations in accessible health care equipment and facilities) contribute to these disparities in care.40 Availability and utilization of adaptive and assistive devices (such as lifts and transfer equipment) can bridge the gap in access to health care facilities. For patients with speech or language impairments, intellectual disabilities, or physical or sensory disabilities, the availability of supportive tools (such as picture boards, assistive communication technologies, Braille or large print, and teletypewriter machines) can be essential for effective communication.
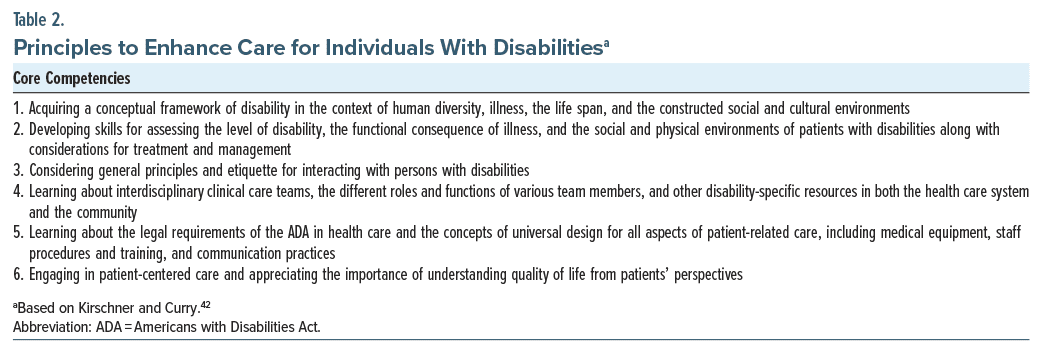
Promoting education for providers can play a vital role in facilitating care of those with disabilities. The US Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilities,41 released in 2005, identified the failure of medical education programs to teach concepts of disability as a root cause for individuals with disabilities having worse health status than those without disabilities. Clinicians specializing in the care of individuals with disabilities and medical education have subsequently suggested core competencies to guide the development of disability-related curricula in medical schools. An example of suggested core competencies, from Kirschner and Curry, is provided in Table 2.42
Augmenting existing clinical education to make it specific to caring for persons with a disability can provide an avenue for patients to access skilled health care. For example, a principle taught in the curriculum for patient-clinician communication is the maintenance of eye contact when communicating with patients; this can be expanded to include sitting down to speak eye-to-eye with a patient who is wheelchair-bound.
How Are Individuals With Disabilities Portrayed in Popular Media?
The media plays a critical role in both shaping and reflecting public perception of disability. A 1982 review of media representations of disability found classic literature promoted 2 stereotypes of disability, with some characters’ disability representing virtue and others representing their moral deficits.43 Examples of the latter include tying Captain Ahab’s missing leg to his “mad” obsession with Moby Dick and Shakespeare’s Richard III’s hunchback manifesting his murderous pursuit of the throne. Television and film also promoted harmful stereotypes about disability, predominantly portraying individuals with disability as pitiable, burdensome, or maladapted.43,44 One of the most widespread depictions of disability was through telethons, which reinforced these stereotypes to make an emotional appeal for fundraising.43
From these traditional, helpless portrayals of disability emerged the “supercrip” narrative where individuals with disabilities are portrayed as heroic for accomplishing feats while “overcoming” their disabilities, even if these feats are mundane.45 This is often recognized in sports, particularly the Paralympic Games where athletes with disabilities are depicted in an overwhelmingly positive light. On the surface, supercrip narratives are an empowering portrayal of disability, as people with disability are featured. However, critics have noted how these narratives often reflect and reinforce the distorted, low expectations that the public has for individuals with disabilities.45
Supercrip narratives encapsulate the difficulty in balanced and authentic representation of individuals with disabilities in the media. The volume of disability inclusive representations has increased over time, although only 4.2% of films and television featured a disability theme in 2019.46 Individuals with disabilities are more likely than those in the general population to feel that there is insufficient and inaccurate representation of their identity group in the media.46 To meet this gap, individuals with disabilities are increasingly telling their own stories on social media, helping to dispel stereotypes and reframe how disability is portrayed.46
In What Ways Can Representation and Mentorship Improve the Quality of Medical Care Delivered to Individuals With Disabilities?
Representation and mentorship play pivotal roles in shaping a health care landscape that is attuned to the needs of individuals with disabilities. The inclusion of individuals with disabilities holds transformative potential to elevate the quality of medical care for this population.
Representation of individuals with disabilities in the medical field helps to reduce stereotypes through the tenets of contact theory.47 When individuals with disabilities are visible in health care professions, it challenges stereotypes and dispels misconceptions. This, in turn, contributes to a more empathetic and informed approach among health care providers, thereby leading to improved patient care.48–50
The inclusion of health care professionals with disabilities also encourages cultural humility of emerging providers. This disconnect with the medical model views of disability helps to create new perspectives and humility in the assumed knowledge one has of disability. The prevailing belief is that this will cross over to patient care, with providers approaching the care of disabled patients with an increased sensitivity, respect, and a patient-as-expert focus.
Finally, the inclusion of people with disabilities contributes to ongoing advocacy and policy influence. Representation in health care positions empowers individuals with disabilities to advocate for systemic changes that ultimately improve patient care. With disabled providers serving as advocates, the health care system becomes more attuned to the inequities faced by individuals with disabilities, leading to policy improvements that positively impact the quality of care and nurturing of an environment where the delivery of medical care becomes inherently inclusive, respectful, and tailored to the diverse needs of all patients, including those with disabilities.
What Happened to Ms A?
Two weeks after her biking accident, Ms A was transferred to an inpatient rehabilitation facility, where she stayed for approximately 1 month for treatment of ongoing back pain. Her medical course was complicated by a urinary tract infection (that required antibiotics) and urinary retention (that required intermittent catheterization). After she developed increasing spasticity in her lower extremities, Ms A was started on baclofen.
At the rehabilitation hospital, Ms A wished to prioritize exercises and rehabilitative interventions that would improve her capacity to care for, and engage in recreational activities with, her daughter. Slowly, movement and strength in Ms A’s right lower extremity began to improve, particularly with hip flexion and extension. Much of Ms A’s physical therapy centered on improving her mobility through effective use of a wheelchair. At the time of discharge from the rehabilitation unit, Ms A was mostly using a wheelchair for mobility, although she could walk 75–100 feet with a rolling walker.
The physical and occupational therapists also provided recommendations to Ms A and her husband for adaptive devices—such as car modifications, a chair lift for stairs in Ms A’s home, and grab bars for her shower and bathroom. Social work and case management helped the family navigate acquiring and receiving financial assistance for these devices. Case management also offered guidance on work leave and provided information on acquiring accommodations once Ms A was closer to a return to work.
Two weeks into her rehabilitation stay, a psychiatry consultation was requested. In her discussions with the consultant psychiatrist, Ms A reported how overwhelmed and anxious she felt about her current physical debility. Over the coming days and weeks, Ms A discussed with her psychiatrist and social worker her helplessness and isolation that accompanied her prolonged hospitalization. Both the psychiatrist and social worker recognized Ms A’s desire for a community that could be empathic and offer practical advice. With Ms A’s permission, members of the wheelchair tennis team that partnered with the rehabilitation facility were asked to visit with Ms A. She was encouraged by her interaction with individuals who shared her values for physical fitness and who could provide tips for adjusting to life following a spinal cord injury.
On the day of discharge from her rehabilitation facility, Ms A was both excited (to spend time with her husband and daughter) and apprehensive (about adjusting to life with a spinal cord injury without the supervision of nurses and physicians). Ms A expressed gratitude for the care that she had received. She remained steadfast in her desire to adjust and thrive.
CONCLUSION
Since many people have disabilities, physicians should develop skills that assess the level of disability, the functional consequence of illness, and the social and physical environments of patients with disabilities to enhance the quality of care they provide these individuals. In addition, health care providers can learn about interdisciplinary clinical care teams, the different roles and functions of various team members, and disability specific resources in the health care system and the community, as well as the legal requirements of the ADA in health care (including medical equipment, staff procedure, training, and communication practices) to improve care. Moreover, as the representation of individuals with disabilities in the medical field increases, stereotypes and misconceptions about disability will diminish.
Article Information
Published Online: June 6, 2024. https://doi.org/10.4088/PCC.23f03684
© 2024 Physicians Postgraduate Press, Inc.
Submitted: December 15, 2023; accepted March 15, 2024.
To Cite: Baig M, Chun AS, Bains A, et al. The impact of disability on medical care. Prim Care Companion CNS Disord. 2024;26(3):23f03684.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (Baig, Chun, Bains, Stern); Department of Psychiatry, McLean Hospital, Belmont, Massachusetts (Baig, Chun); Department of Learning Health Sciences, University of Michigan Medical School, Ann Arbor, Michigan (Meeks); Department of Family Medicine, University of Michigan Medical School, Ann Arbor, Michigan (Meeks); Harvard Medical School, Boston, Massachusetts (Stern).
Corresponding Author: Mirza Baig, MD ([email protected]).
Relevant Financial Relationships: Dr Meeks has received grants from the Ford Foundation (no. 142636) and the Robert Wood Johnson Foundation (no. 80317) and a Rehabilitation Research and Training Centers Equity award AWD022045 from the National Institute on Disability and Rehabilitation Research Equity. Drs Baig, Chun, Bains, and Stern report no relevant financial relationships.
Funding/Support: None.
Clinical Points
- Disability is defined as a physical or mental impairment that substantially limits 1 or more major life activities.
- Person-first language places the person before the disability (eg, “person with autism” and “person with quadriplegia”) and attempts to distinguish a person from their disability, while identity-first language places the disability before the person (eg, “deaf person” and “disabled person”) to promote a positive social identity.
- Coping with, and adjusting to, a disability often depends on the nature of the disability and the circumstances specific to the individual involved, as well as on individualized programs to achieve significant gains in activities of daily living, shorter hospital stays, and fewer hospitalizations.
- Barriers to effective adaptation often include socioeconomic challenges, a lack of transportation, physical obstacles, insufficient communication options, programmatic hurdles, a lack of policy enforcement, and attitudes toward disability as well as health care providers’ biases, which lead patients to worry that physicians do not understand how their disability interacts with their daily lives.
References (50)

- United States. Americans with Disabilities Act of 1990. Public Law No. 101–336. US Statut Large. 1990;104:327–378. PubMed
- United States. Americans with Disabilities Act Amendements Act of 2008. Public Law No. 110-325. US Statut Large. 2008;122:3553–3559.
- Introduction to the Americans with Disabilities Act. ADA.gov. December 1, 2023. Accessed December 3, 2023. https://www.ada.gov/topics/intro-to-ada/
- Varadaraj V, Deal JA, Campanile J, et al. National prevalence of disability and disability types among adults in the US, 2019. JAMA Netw Open. 2021;4(10):e2130358. PubMed CrossRef
- Andrews EE, Powell RM, Ayers K. The evolution of disability language: choosing terms to describe disability. Disabil Health J. 2022;15(3):101328. PubMed CrossRef
- Olkin R. Disability-affirmative therapy: a case formulation template for clients with disabilities. Oxford University Press; 2017.
- Smart JF. The power of models of disability. J Rehabil. 2009;75(2):3–11.
- Vivanti G. Ask the editor: what is the most appropriate way to talk about individuals with a diagnosis of autism? J Autism Dev Disord. 2020;50(2):691–693. PubMed CrossRef
- Scholzman SC, Groves JE, Gross AF. Coping with illness and psychotherapy of the medically ill. In: Stern TA, Freudenreich O, Smith FA, eds, et al. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 7th ed. Saunders Elsevier;2018:397–403.
- Bogart KR, Tickle-Degnen L, Ambady N. Compensatory expressive behavior for facial paralysis: adaptation to congenital or acquired disability. Rehabil Psychol. 2012;57(1):43–51. PubMed CrossRef
- Li L, Moore D. Acceptance of disability and its correlates. J Soc Psychol. 1998;138(1):13–25. PubMed CrossRef
- Bogart KR. The role of disability self-concept in adaptation to congenital or acquired disability. Rehabil Psychol. 2014;59(1):107–115. PubMed CrossRef
- Craig A, Hancock K, Dickson H. Improving the long-term adjustment of spinal cord injured persons. Spinal Cord. 1999;37(5):345–350. PubMed CrossRef
- Reuman LR, Mitamura C, Tugade MM. Coping and disability. In: Wehmeyer ML, ed. The Oxford Handbook of Positive Psychology and Disability. 1st ed. Oxford University Press; 2013:91–104.
- Aspinwall LG, Taylor SE. A stitch in time: self-regulation and proactive coping. Psychol Bull. 1997;121(3):417–436. PubMed CrossRef
- Sirois FM, Danielle SM, Hirsch JK. Self-compassion, stress, and coping in the context of chronic illness. Self Identity. 2015;14(3):334–347.
- Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109–116. PubMed CrossRef
- Kaplan RM. Quality of life: an outcomes perspective. Arch Phys Med Rehabil. 2002;83(12 suppl 2):S44–S50. PubMed CrossRef
- Costa DSJ, Mercieca-Bebber R, Rutherford C, et al. How is quality of life defined and assessed in published research? Qual Life Res. 2021;30:2109–2121. PubMed CrossRef
- Teasell RW, Foley NC, Bhogal SK, et al. How is quality of life defined and assessed in published research? Can J Neurol Sci. 2005;32(4):512–517. PubMed
- Clark AM, Catto S, Bowman G, et al. Design matters in secondary prevention: individualization and supervised exercise improves the effectiveness of cardiac rehabilitation. Eur J Cardiovasc Prev Rehabil. 2011;18(5):761–769. PubMed CrossRef
- Oosterhof B, Dekker JHM, Sloots M, et al. Success or failure of chronic pain rehabilitation: the importance of good interaction–a qualitative study under patients and professionals. Disabil Rehabil. 2014;36(22):1903–1910. PubMed CrossRef
- Peacock G, Iezzoni LI, Harkin TR. Health care for Americans with disabilities – 25 Years after the ADA. N Engl J Med. 2015;373(10):892–893. PubMed CrossRef
- Graham CL, Mann JR. Accessibility of primary care physician practice sites in South Carolina for people with disabilities. Disabil Health J. 2008;1(4):209–214. PubMed CrossRef
- Lagu T, Hannon NS, Rothberg MB, et al. Access to subspecialty care for patients with mobility impairment: a survey. Ann Intern Med. 2013;158(6):441–446. PubMed CrossRef
- Mudrick NR, Breslin ML, Liang M, et al. Physical accessibility in primary health care settings: results from California on-site reviews. Disabil Health J. 2012;5(3):159–167. PubMed CrossRef
- United States. Affordable Care Act. Public Law No. 111-148. US Statut Large. 2010;124:119–1024.
- Rondinelli RD, Eskay-Auerbach M. Healthcare provider issues and perspective: impairment ratings and disability determinations. Phys Med Rehabil Clin N Am. 2019;30(3):511–522. PubMed CrossRef
- Reynolds CA, Wagner SL, Harder HG. Physician-stakeholder collaboration in disability management: a Canadian perspective on guidelines and expectations. Disabil Rehabil. 2006;28(15):955–963. PubMed CrossRef
- Kosny A, MacEachen E, Ferrier S, et al. The role of health care providers in long term and complicated workers’ compensation claims. J Occup Rehabil. 2011;21(4):582–590. PubMed CrossRef
- Disability and Health Promotion. Common Barriers to Participation Experienced by People with Disabilities. Centers for Disease Control and Prevention. Updated September 16, 2020. Accessed December 1, 2023. https://www.cdc.gov/ncbddd/disabilityandhealth/disability-barriers.html
- de Vries McClintock HF, Barg FK, Katz SP, et al. Health care experiences and perceptions among people with and without disabilities. Disabil Health J. 2016;9(1):74–82. PubMed
- Kroll T, Jones GC, Kehn M, et al. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: a qualitative inquiry. Health Soc Care Community. 2006;14(4):284–293. PubMed CrossRef
- Pharr JR. Accommodations for patients with disabilities in primary care: a mixed methods study of practice administrators. Glob J Health Sci. 2013;6(1):23–32. PubMed CrossRef
- Morrison EH, George V, Mosqueda L. Primary care for adults with physical disabilities: perceptions from consumer and provider focus groups. Fam Med. 2008;40(9):645–651. PubMed
- Iezzoni LI, Rao SR, Ressalam J, et al. Physicians’ perceptions of people with disability and their health care. Health Aff (Millwood). 2021;40(2):297–306. PubMed CrossRef
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48(8):977–988. PubMed CrossRef
- Meeks LM, Pereira-Lima K, Plegue M, et al. Disability, program access, empathy and burnout in US medical students: a national study. Med Educ. 2023;57(6):523–534. PubMed CrossRef
- Kelly-Blake K, Garrison NA, Fletcher FE, et al. Rationales for expanding minority physician representation in the workforce: a scoping review. Med Educ. 2018;52(9):925–935. PubMed CrossRef
- Iezzoni LI. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff (Millwood). 2011;30(10):1947–1954. PubMed CrossRef
- Office of the Surgeon General (US); Office on Disability (US). The Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilities. Rockville (MD): Office of the Surgeon General (US); 2005.
- Kirschner KL, Curry RH. Educating health care professionals to care for patients with disabilities. JAMA. 2009;302(12):1334–1335. PubMed CrossRef
- Elliott TR, Byrd EK. Media and disability. Rehabil Lit. 1982;43(11–12):348–355. PubMed
- Black RS, Pretes L. Victims and victors: representation of physical disability on the silver screen. Res Pract Persons Severe Disabilities. 2007;32(1):66–83.
- Silva CF, Howe PD. The (in)validity of supercrip representation of paralympian athletes. J Sport Social Issues. 2012;36(2):174–194.
- Closing the Inclusion Gap for People with Disabilities. Nielsen. Accessed December 3, 2023. https://www.nielsen.com/insights/2022/closing-the-inclusiongap-for-people-with-disabilities/
- Meeks LM, Poullos P, Swenor BK. Creative approaches to the inclusion of medical students with disabilities. AEM Educ Train. 2020;4:292–297. PubMed CrossRef
- Meeks LM, Maraki I, Singh S, et al. Global commitments to disability inclusion in health professions. Lancet. 2020;395(10227):852–853. PubMed CrossRef
- Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540–543. PubMed CrossRef
- Iezzoni LI. Why increasing numbers of physicians with disability could improve care for patients with disability. AMA J Ethics. 2016;18(10):1041–1049. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!