Abstract
Importance: When patients present with cognitive impairment, consults to neuropsychology can assist internists and psychiatrists in diagnosis, treatment planning, and determination of functional status. Neuropsychological evaluation and treatment have been shown to improve health outcomes and patient and family satisfaction. The objective of this narrative review is to explore the role of neuropsychologists in their collaboration with care teams to improve patient outcomes.
Observations: Neuropsychologists have specialized education and training in brain behavior relationships and neurocognitive functioning. The consultation process for neuropsychology can be made more efficient by the referring physician clearly delineating the reason for the referral, ordering relevant laboratory tests and imaging studies, performing screenings for treatable conditions, and providing historical records to the neuropsychologist prior to the consult. Neuropsychological assessment can assist in diagnosis, identification of neuropsychological status, establishing a baseline, treatment planning, determination of functional ability, and monitoring the effectiveness of treatments.
Conclusions and Relevance: Primary care teams and psychiatrists can benefit from collaboration with neuropsychologists. The most effective process for engaging neuropsychologists in the care of patients is through full communication, including properly placed consults.
Prim Care Companion CNS Disord 2024;26(5):24nr03766
Author affiliations are listed at the end of this article.
Clinical neuropsychology is a specialty of clinical psychology that focuses on brain-behavior relationships and neurocognitive functioning.1 Neuropsychologists use this expertise in the assessment and treatment of cognitive disorders, most typically with neurological, psychiatric, and rehabilitation patients. Primary care physicians can benefit from collaboration with neuropsychologists to provide better patient care. The objective of this narrative review is to explore the role of neuropsychologists in their collaboration with care teams to improve patient outcomes. The history of neuropsychology is available elsewhere.2
NEUROPSYCHOLOGIST QUALIFICATIONS
In the United States, education and training in clinical neuropsychology require specific functional competencies in the specialty.3 A doctoral degree in clinical psychology, including a 1-year internship and research dissertation, followed by a 2-year fellowship or residency is the foundation. Required graduate instruction includes neuropsychological assessment and the neurological basis of behavior. Additional coursework in neuroanatomy, neurophysiology, neuropathology, psychopharmacology, psychopathology, personality, psychometrics, and research methods is common. Predoctoral training occurs prior to internship at clinical externship placements. Following the postdoctoral fellowship, the neuropsychologist can qualify for state licensure as a psychologist.
Board certification involves rigorous peer review to ensure competency in the specialty.4 This entails review and approval of the applicant’s credentials and experience, a written examination, blinded review of case reports, and passing an oral examination. Two national organizations certify neuropsychologists: the American Board of Clinical Neuropsychology through the American Board of Professional Psychology (ABPP) and the American Board of Professional Neuropsychology (ABN). Under ABPP, there is a maintenance of certification (MOC) process that involves self-examination and documentation of continuing professional development activities that maintain specialty-related competence. MOC was optional for those boarded before January 2015. It is now required that board-certified specialists demonstrate MOC every 10 years. ABN does not currently have a MOC process.
USE OF NEUROPSYCHOLOGY IN PATIENT CARE
Primary care physicians frequently perform brief cognitive screenings to assess mental status.4 Their purpose includes early detection of individuals at risk for specific disorders but is limited in scope and specificity with resultant cutoff scores. A positive screening test and/or a need for diagnosis or determination of functional status may lead to a physician referral to a neuropsychologist for a more comprehensive and sensitive neuropsychological assessment.5,6 To do this, providing full communication about the patient is crucial.
Neuropsychologists receive most of their referrals from neurologists, psychiatrists, and primary care physicians.7 Clark8 found that exposure to neuropsychology during residency had the strongest impact on referral intentions. Those authors8 and others9 found psychiatry and neurology residents to have had more exposure to neuropsychological services and recommended increased education specifically to internal medicine and family medicine residents. Hopps10 identified 4 components of referral questions that must be provided by the referral source: information about the patient’s diagnosis and history; the type of assessment requested (ie, assessment of IQ, differential diagnosis, etc); any specific requests for testing (ie, baseline determination, reevaluation); and requests and needs for specific recommendations. Information provided guides the examiner in shaping the testing battery and report to more accurately answer the referring question. Similarly, Schoenberg and Scott11 delineated 3 aspects of the referral as most important: providing a specific question to be answered by the consultation, providing previous medical and psychiatric records and laboratory and study results, and reviewing the purpose of the referral to the patient, including an explanation of what to expect and how the consultation results will be used to assist in their care. To optimize neuropsychology’s utility, the referral question must be clarified and defined specifically (including the needs and expectations of the referring physician), and, ideally, all laboratory tests and imaging are conducted and provided with historical records to the neuropsychologist prior to the consultation. The latter avoids redundancy and delay by ruling out certain reversible or treatable conditions in advance of any referral, especially since neuropsychologists cannot order laboratory tests or radiological studies.
When a patient’s primary complaint is related to cognitive deficits, an assessment may need to be broader than a typical review of systems. Additional evidence based factors that should be considered prior to patient referral are detailed below.
Laboratory Tests
Patients benefit from a medical workup to first exclude reversible causes of cognitive impairment. Laboratory tests are often critical for identifying causes of cognitive deficits, and different laboratory studies may be necessary depending on the suspected etiology of the cognitive deficits. Older individuals with cognitive deficits may be experiencing nutritional deficits that mimic dementia. Laboratory tests can also reveal hormonal dysfunction, metabolic disorders, and vascular disease.
As a guide, the American Academy of Neurology recommends the following workup when assessing for dementia12:
- Complete blood count: to screen for anemia, infection, and other deficiencies. Vitamins B12 (cobalamin) and B9 (folate) can have significant impacts on cognition. Vitamin D is important for neurotransmitter synthesis and may impact dementia risk. Vitamin B3 (niacin) deficiencies can result in pellagra, with a triad of symptoms that include dermatitis, diarrhea, and dementia. Malabsorption syndromes should also be ruled out. HIV, hepatitis, syphilis, and meningitis should be ruled out if there is an indication of an infection, especially with known exposures, with the addition of more specific testing. Older patients can present with cognitive deficits from other infective states, such as urosepsis, without expressing organ-related symptoms. They may experience confusion, delirium, lethargy, and lower fever response.13 Consideration must be given to subclinical presentations in the face of inadequately treated infections.
- Comprehensive metabolic panel: to reveal abnormalities in glucose, electrolytes, and renal and hepatic function, which can impact cognitive health. Hyponatremia is the most common electrolyte disorder and may arise from multiple conditions and medication side effects and can result in a range of cognitive symptoms, from mild confusion to marked delirium. Conversely, hypernatremia can also result in lethargy and cognitive deficits. Older adults are particularly vulnerable to sodium imbalance.14
- Hemoglobin A1c, may be indicated: diabetes is an independent risk factor for multiple cerebrovascular risk factors, and studies suggest that it increases the risk of mild cognitive impairment and dementia.15
- Thyroid panel: to include assessment of hyper- and hypothyroidism, both of which may masquerade as depression and negatively impact cognition.16
- Therapeutic drug monitoring studies, as indicated: certain steroids, antibiotics, cardiovascular medications, antiepileptics, opiates, benzodiazepines, anticholinergics, chemotherapeutics, and psychiatric medications.
Medication Side Effects and Polypharmacy
Medications may be the crux of the problem for a patient with cognitive complaints. Some medications are more frequently associated with adverse cognitive symptoms than others. In a fast-paced clinical environment, medication reconciliation can be challenging but is a critical step in the assessment of an individual presenting with cognitive abnormalities.
Drug-induced neurological disorders are well characterized in the clinical literature.17 First-generation antihistamines, muscle relaxants, tricyclic antidepressants, antipsychotics, benzodiazepines, and antiparkinsonian medications can all negatively impact cognition and increase rates of delirium and dementia. Diuretics disrupt electrolyte balance and lead to changes in consciousness and increased risk of seizures. Many medications can increase the risk of serotonin syndrome and neuroleptic malignant syndrome, both of which have a cognitive profile. Stimulants, adrenergic agents, antidepressants, corticosteroids, and sudden discontinuation of sleep medications all impact concentration, thinking, reasoning, arousal, and alertness.17
Multiple classes of antibiotics may result in neurotoxicity. Penicillin can result in confusion and disorientation. Carbapenems may result in headaches, seizures, and encephalopathy. Macrolides, metronidazoles, and quinolones can increase confusion, delirium, and risk of seizures.17 Although rare (∼5% of patients), steroid-induced psychotic symptoms should also be considered. Symptoms may include mood changes, such as mania and depression, and behavioral disturbances, such as agitation and cognitive deficits. Factors that increase the risk of steroid-induced psychosis include higher doses or concurrent medications that inhibit the cytochrome P450 enzyme, thus increasing the bioavailability of steroids.18
Anticholinergic medications affect cognitive function and dementia risk. In a case-control study, Coupland et al19 demonstrated an increased risk of dementia, particularly for individuals prescribed antidepressants, bladder antimuscarinics, antiepileptics, or antiparkinsonian medications. A meta-analysis also demonstrated a positive association between anticholinergic medications and dementia, with evidence of a dose-dependent relationship; higher cumulative daily doses were associated with a greater risk of dementia.20
Polypharmacy is a frequently encountered clinical conundrum faced by many primary care physicians, particularly when patients mix prescribed medication with various over-the-counter medicine or other supplements that impact converting enzymes or when patients have medications prescribed by multiple providers. Unfortunately, polypharmacy is common among older adults and is a frequent cause of cognitive symptoms.21 Studies demonstrate that the higher the number of medications an individual is prescribed, the greater the risk of cognitive decline and dementia.22
Thus, a comprehensive medication review is necessary when a patient presents with cognitive complaints, and physicians should consider reducing or eliminating certain medications. A recent systematic review suggests that deprescribing is well-tolerated, even among older frail patients, and reduction of polypharmacy improves clinical outcomes related to mental health and cognition.23 As a resource, the American Geriatric Society regularly updates the Beers Criteria of Potentially Inappropriate Medications in Older Adults.24
Substance Abuse
Substance abuse, including illicit drugs and alcohol, can negatively impact cognitive function, with multiple meta-analyses demonstrating cognitive impairment.25–28 In addition to clinical history and collateral reports, short screening tools may aid in assessing substance use disorder in a busy outpatient setting.29
- The Drug Abuse Screening Test-10 is a brief self administered questionnaire that has high sensitivity and specificity for substance use disorder.30
- The Alcohol Use Disorders Identification Test is a fast and reliable measure of alcohol abuse.31
Imaging Studies
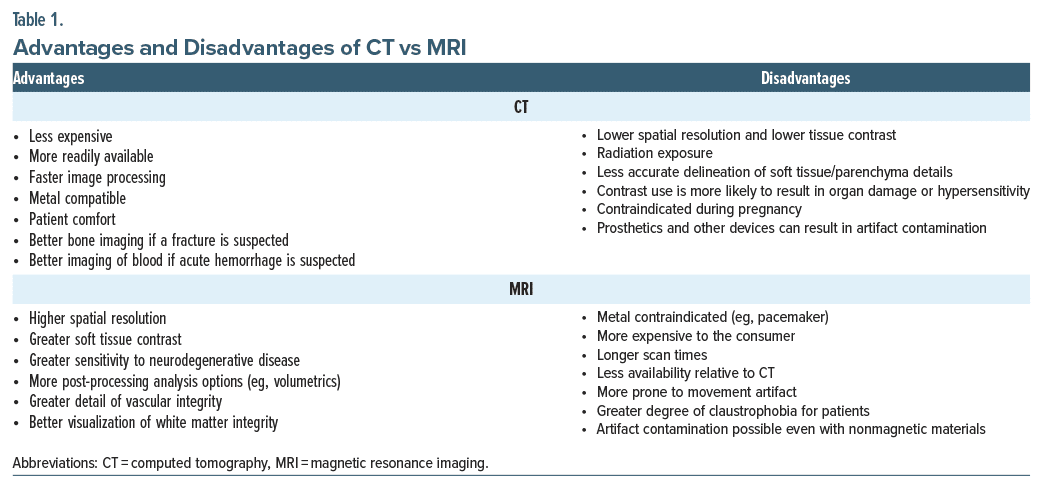
Radiological examinations can assist with identifying stroke, chronic small vessel disease, space-occupying lesions, hydrocephalus, focal or generalized atrophy, and infectious processes, among other conditions. Even with mild or subjective complaints, imaging may reveal an emerging pathology. Unless contraindicated, some type of imaging should be considered routine. Table 1 compares the strengths and weaknesses of computed tomography and magnetic resonance imaging (MRI).
As it relates to cognitive complaints, the imaging studies should examine the following32:
- The pattern of atrophy may be indicative of certain pathological processes. For example, predominantly frontal atrophy may be indicative of frontotemporal dementia, while medial temporal atrophy is common in Alzheimer disease.
- The degree of small vessel disease can contribute to cerebrovascular pathology and white matter burden. Moderate-to-severe white matter change will negatively impact cognition and contribute to a worsening of other degenerative conditions.33
- Other pathologies, such as infection, chronic encephalomalacia, hydrocephalus, or space occupying lesions, may be determined.
Functional imaging (ie, positron emission tomography scan and functional MRI) may also be warranted, and electroencephalogram can help identify abnormal brainwave patterns underlying cognitive changes.34,35
Sensory-Perceptual Declines
While hearing loss may occur at any age, older adults have an increased likelihood of declines. Hearing loss increases social isolation and depression and reduces quality of life.36 There are converging lines of research demonstrating that hearing loss is an independent risk factor for cognitive decline and dementia,37 and hearing aids and other amplification therapies seem to ameliorate these effects.38 Vision loss may also be associated with cognitive decline. Aside from the obvious impact of low vision, macular degeneration, cataracts, or blindness limit engagement in certain cognitive tasks and daily activities. Multiple studies underscore the importance of eye health in maintaining cognitive function, particularly in older adults. For example, one study demonstrated that lower visual acuity is associated with lower scores on a measure of global cognitive function,39 and 2 recent systematic reviews further bolster these findings, demonstrating that visual impairment is associated with cognitive decline and increased risk of dementia longitudinally.40,41 Together, vision and hearing screening should always be evaluated in patients presenting with concerns of cognitive decline, particularly in older adults, and steps should be taken to mitigate any impairments toward maximizing cognitive functioning.
Sleep Disorders
Studies demonstrate that physicians may not routinely evaluate sleep health during an office visit, and there is a general underdiagnosis of sleep disorders in primary care.42 Primary sleep disorders can be easily screened in a routine office visit, allowing for additional polysomnography assessment if needed. Sleep health, primarily insomnia and obstructive sleep apnea (OSA), should consistently be assessed when a patient presents with concerns of cognitive decline. Insomnia is associated with cognitive and affective symptoms,43 and cognitive-behavioral treatment protocols for insomnia ameliorate cognitive sequelae.44 Sleep apnea is a significant risk factor for multiple cardiovascular and cerebrovascular illnesses but is also associated with cognitive deficits, depression, and anxiety. Meta analyses of the neuropsychological consequences of OSA demonstrate reduced executive function, attention, and processing speed, as well as reduced verbal and nonverbal memory.45,46 The underlying mechanisms of OSA’s impact on cognition may include a disruption of sleep architecture, chronic hypoxemia, and increased inflammation.47 These factors result in increased hypertension and white matter burden and negatively impact cognitive function. Fortunately, studies demonstrated that apneic patients who maintain regular sleep with continuous positive airway pressure treatment improved cognitive function over time.48,49
Screening tools include the Epworth Sleepiness Scale50 and the STOP-Bang questionnaire.51 Screening tools should be coupled with clinical history to determine if more comprehensive polysomnography testing is indicated. Regardless, the patient will require education on not only the general health benefits of good sleep hygiene and treatment but also the cognitive consequences of untreated sleep apnea.
Depression and Other Psychiatric Presentations
Patients with current or recurring psychiatric symptoms often present to the primary care visit with cognitive complaints. The occurrence of subjective and objective cognitive deficits among patients with affective symptoms is quite high.52 There is a known association between psychiatric conditions and cognitive deficits, including longitudinal increased risk of dementia among those with depression or anxiety.53,54 A recent meta analysis demonstrated that individuals with depression have moderate cognitive deficits relative to healthy controls, and the greatest degree of cognitive impairment was among treatment-resistant depression and older adults with depression.55 Additionally, depression among older adults often masquerades as dementia (ie, “pseudodementia”). As such, mental health should be routinely screened when a patient presents with cognitive complaints.
Although the neuropsychologist will include a more comprehensive assessment of mental health, common screening tools often used in primary care include the following:
- Patient Health Questionnaire–9: the 9-item questionnaire effectively assesses symptoms of depression and aligns with diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders.56
- Generalized Anxiety Disorder–7: this 7-item measure is appreciated for its brevity and ability to assess general anxiety and anxiety severity.57
- Hospital Anxiety and Depression Scale: this scale is frequently used in nonpsychiatric hospital settings and effectively differentiates between depression and anxiety.58
Chronic Pain
The estimated prevalence of chronic pain is 20% in the United States, with a lifetime prevalence of up to 40%.59,60 Additionally, more than 50% of older adults and 80% of individuals in nursing homes experience chronic pain.61 Unfortunately, chronic pain is accompanied by multiple psychiatric and cognitive comorbidities.62,63 Older adults with high levels of pain are more susceptible to memory deficits.64 Furthermore, individuals with chronic pain have difficulty recalling medical instructions and adhering to treatment protocols.65 Several studies suggest that cognitive function improves following effective mitigation of pain, with concomitant improved sleep quality, decreased emotional distress, and increased participation in daily activities.66 Given these factors, the presence of pain and pain severity should be evaluated among patients who present with cognitive complaints.
Expertise and Skills Contributed by the Neuropsychologist
Neuropsychological assessment requires the neuropsychologist to interpret test results as well as integrate the patient’s history, symptoms, behavior, and performance into the clinical decision-making.6 The unique contribution of neuropsychology is its use of deficit measurement11 or the comparison of test performance to normative and/or individual standards. Normative comparison standards include population averages, whereby a patient’s scores are compared to those of healthy people of the same age, sex, and education level. The individual standard compares a patient’s scores to where they “should” be by estimating a patient’s premorbid functioning or their original level of functioning before the onset of disease or injury. An individual is only considered to have a deficit if there is a significant decrease in performance compared to one (or both) of these standards.11,67
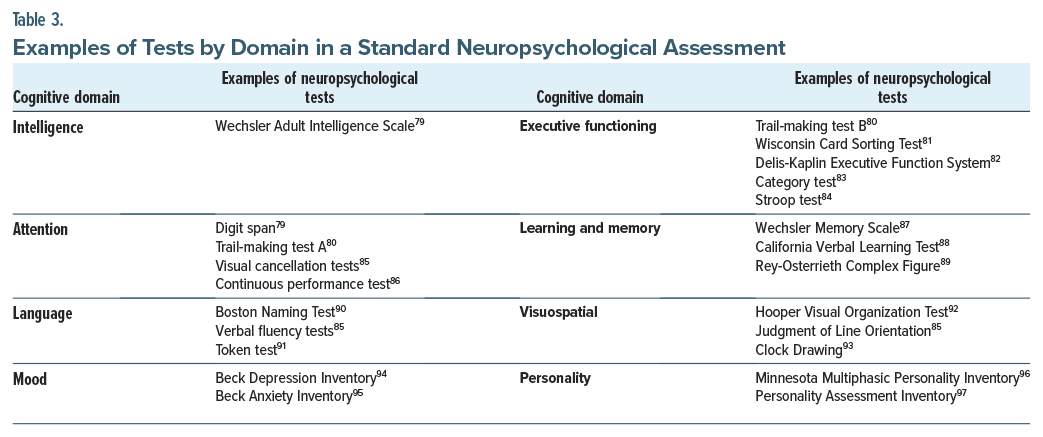
Neuropsychological assessment involves several parts.68,69 First, there is a review of all available medical records germane to the referral question, which is why clarification of the referral question and provision of records is so important. Next, a detailed clinical interview and neurobehavioral status examination are conducted with a focus on the onset and progression of symptoms and current psychological functioning. Pertinent medical history, relevant surgeries, injuries, psychological stressors, social history, education, family medical history, family involvement, and behavioral observations are also obtained. Assessment can last up to several hours, with tests administered in a standardized fashion. Neuropsychological evaluation assesses cognitive functions, including intellectual functioning, attention, language, visuospatial functioning, memory, executive functioning, and motor functioning, in addition to mood assessment.70 This differs from the typical psychological assessment, which is limited to the evaluation of intellectual (and sometimes academic achievement) functioning, mood, and personality. The test battery must be individualized; the neuropsychologist’s training and expertise guide the selection of tests administered for a given situation, as well as the integration of results into clinical decision-making. The detailed report, including recommendations, is then provided to the referring physicians. Common recommendations may include cognitive strategies to compensate for any weaknesses, referrals for psychotherapy/psychiatry, brain health strategies (ie, sleep hygiene, exercise, and diet), and referrals to support services, organizations, and legal assistance. Ideally, feedback is also provided to the patient, the patient’s family, and care team members after the assessment to review and explain results and discuss recommendations. Following the initial consultation, the neuropsychologist may continue to be involved in the patient’s care, such as participating in the formulation of a care plan and later reassessment, if needed (after which the care plan may be revised).
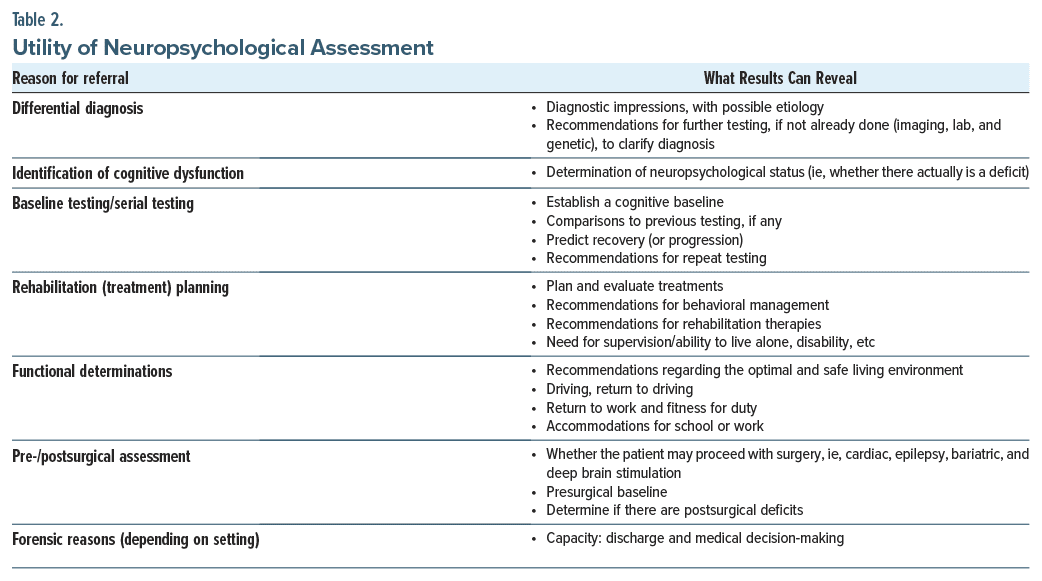
In order, the most commonly received referrals involve brain injury and cerebrovascular accident, epilepsy, dementia, general cognitive concerns, psychiatric concerns, developmental delay, and vocational planning.71 Refinement of diagnosis is the most common reason for referral.72,73 Other reasons include identification of neuropsychological status, establishing a baseline, treatment planning, determination of functional ability, monitoring the effect of treatments, and forensic applications such as capacity determinations.11,69,74 The utility and benefits of neuropsychological assessment are shown in Table 2.
Neuropsychological assessment results in high patient satisfaction and improved health outcomes.1 Numerous survey studies have also demonstrated that neuropsychological assessment is respected and appreciated by referral sources.72,73 For example, in a survey study, referral sources cited the neuropsychological report, specialty knowledge, assessment of functional abilities, diagnostic clarification, and recommendations as particularly useful.75 In primary care encounters, neuropsychology integration is becoming more common and has been shown to increase referrals as well as improve patient and physician satisfaction.1,76 The “stepped model” of care in this setting, with varied levels of assessment according to need, has also resulted in better patient access and added efficiency.77,78
What Tools Do Neuropsychologists Bring?
As mentioned earlier, every assessment battery is individualized for the specific patient’s concerns and tailored to answer the referral questions. Thus, there is no one-size-fits-all test battery. Nevertheless, the standard assessment battery (Table 3) will always seek to assess the various cognitive domains, as well as measure the patient’s estimated premorbid functioning. There will also typically be free-standing and embedded tests of effort and performance validity included, as well as sometimes assessment of functional ability or daily living.98
CONCLUSION
Collaboration with neuropsychologists can be beneficial for primary care physicians, psychiatrists, patients, and families. The specialized training, expertise, skills, and tools of the neuropsychologist can assist in diagnosis, treatment planning, baseline assessment, and determination of functional status. Referrals for neuropsychology consults can be optimized by ruling out certain reversible or treatable conditions in advance of any referral and by clarifying the referral question. Good communication between providers greatly improves the overall effectiveness of the collaboration.
Article Information
Published Online: October 31, 2024. https://doi.org/10.4088/PCC.24nr03766
© 2024 Physicians Postgraduate Press, Inc.
Submitted: May 7, 2024; accepted August 13, 2024.
To Cite: Schaefer LA, Farrer TJ, Dowling DJ. Improving the effectiveness of
collaboration between neuropsychology and primary care. Prim Care Companion CNS Disord. 2024;26(5):24nr03766.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, Nassau University Medical Center, East Meadow, New York (Schaefer); Idaho WWAMI Medical Education Program, University of Idaho, Moscow, Idaho (Farrer); Department of Physical Medicine and Rehabilitation, Nassau University Medical Center, East Meadow, New York (Dowling).
Corresponding Author: Lynn A. Schaefer, PhD, ABPP, Nassau University Medical Center, 2201 Hempstead Turnpike, Box 48, East Meadow, NY 11554 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
ORCID: Lynn A. Schaefer: https://orcid.org/0000-0002-0943-5380; Thomas J. Farrer: https://orcid.org/0000-0001-8092-6214
Clinical Points
- Collaboration between neuropsychologists and physicians significantly improves patient care by enhancing diagnostic precision and treatment planning.
- Effective referrals should include specific questions and prior comprehensive medical evaluations to exclude reversible cognitive impairments.
- Neuropsychological assessments are comprehensive and integrate patient history with standardized tests for accurate diagnosis and treatment planning.
References (98)

- Lanca M, Meisinger K. A model of collaboration between primary care and neuropsychology. In: Sanders KM, ed. Physician’s Field Guide to Neuropsychology: Collaboration through Case Example. Springer; 2019:31–44.
- Bogousslavsky J, Boller F, Iwata M, eds. A History of Neuropsychology. S. Karger AG; 2019.
- Smith G; CNS. Education and training in clinical neuropsychology: recent developments and documents from the clinical neuropsychology synarchy. Arch Clin Neuropsychol. 2018;34(3):418–431. PubMed CrossRef
- Grote C, Soble JR, León A. Board Certification in Neuropsychology. In: Block C, ed. The Neuropsychologist’s Roadmap: A Training and Career Guide. American Psychological Association; 2021:89–108.
- Block CK, Johnson-Greene D, Pliskin N, et al. Discriminating cognitive screening and cognitive testing from neuropsychological assessment: implications for professional practice. Clin Neuropsychol. 2017;31(3):487–500. PubMed CrossRef
- Roebuck-Spencer TM, Glen T, Puente AE, et al. Cognitive screening tests versus comprehensive neuropsychological test batteries: a National Academy of Neuropsychology education paper. Arch Clin Neuropsychol. 2017;32(4):491–498. PubMed CrossRef
- Sweet JJ, Benson LM, Nelson NW, et al. The American Academy of Clinical Neuropsychology, National Academy of Neuropsychology, and Society for Clinical Neuropsychology (APA Division 40) 2015 TCN professional practice and “salary survey”: professional practices, beliefs, and incomes of U.S. neuropsychologists. Clin Neuropsychol. 2015;29(8):1069–1162. PubMed CrossRef
- Clark H. Factors Linked to Future Neuropsychology Referral Practices Among Medical Residents. Undergraduate thesis. 2022.
- Chowhan S, Martin PK, Macaluso M, et al. How much education and training do residents across specialties receive in neuropsychology? Kans J Med. 2021;14:197–200. PubMed CrossRef
- Hopps J. Pattern and Content of Neuropsychological Referral Questions Across 25 Years of Outpatient Visits in a Hospital Based Clinic. The University of Iowa; 2009.
- Schoenberg MR, Scott JG. The neuropsychology referral and answering the referral question. In: Schoenberg MR, Scott JG, eds. The Little Black Book of Neuropsychology. Springer; 2011:1–37.
- Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the quality standardssubcommittee of the American Academy of Neurology. Neurology. 2001;56(9):1143–1153. PubMed CrossRef
- Rodriguez-Mañas L. Urinary tract infections in the elderly: a review of disease characteristics and current treatment options. Drugs Context. 2020;9:2020-4–13.
- Nowak KL, Yaffe K, Orwoll ES, et al. Serum sodium and cognition in older community-dwelling men. Clin J Am Soc Nephrol. 2018;13(3):366–374. PubMed CrossRef
- Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591–604. PubMed CrossRef
- 16. Yuan L, Tian Y, Zhang F, et al. Decision-making in patients with hyperthyroidism: a neuropsychological study. PLoS One. 2015;10(6):e0129773. PubMed CrossRef
- Hurkacz M, Dobrek L, Wiela-Hojeńska A. Antibiotics and the nervous system which face of antibiotic therapy is real, Dr. Jekyll (Neurotoxicity) or Mr. Hyde(Neuroprotection)? Molecules. 2021;26(24):7456. PubMed
- Lu Y, Ann L, McCarron R. Steroid-induced psychiatric symptoms: what you need to know. Curr Psychiatry. 2021;20(4):33–38.
- Coupland CAC, Hill T, Dening T, et al. Anticholinergic drug exposure and the risk of dementia: a nested case-control study. JAMA Intern Med. 2019;179(8):1084–1093. PubMed CrossRef
- Zheng YB, Shi L, Zhu XM, et al. Anticholinergic drugs and the risk of dementia: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;127:296–306. PubMed CrossRef
- Rasu RS, Shrestha N, Karpes Matusevich AR, et al. Polypharmacy and cognition function among rural adults. J Alzheimers Dis. 2021;82(2):607–619. PubMed
- Chippa V, Roy K. Geriatric cognitive decline and polypharmacy. In: StatPearls. StatPearls Publishing; 2024.
- Ibrahim K, Cox NJ, Stevenson JM, et al. A systematic review of the evidence for deprescribing interventions among older people living with frailty. BMC Geriatr. 2021;21(1):258. PubMed
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052–2081. PubMed
- Stephan RA, Alhassoon OM, Allen KE, et al. Meta-analyses of clinical neuropsychological tests of executive dysfunction and impulsivity in alcohol use disorder. Am J Drug Alcohol Abuse. 2017;43(1):24–43. PubMed CrossRef
- Potvin S, Pelletier J, Grot S, et al. Cognitive deficits in individuals with methamphetamine use disorder: a meta-analysis. Addict Behav. 2018;80:154–160. PubMed CrossRef
- Sullivan RM, Perlman G, Moeller SJ. Meta-analysis of aberrant post-error slowing in substance use disorder: implications for behavioral adaptation and self-control. Eur J Neurosci. 2019;50(3):2467–2476. PubMed CrossRef
- Hall MG, Hauson AO, Wollman SC, et al. Neuropsychological comparisons of cocaine versus methamphetamine users: a research synthesis and meta-analysis. Am J Drug Alcohol Abuse. 2018;44(3):277–293. PubMed CrossRef
- Shapiro B, Coffa D, McCance-Katz EF. A primary care approach to substance misuse. Am Fam Physician. 2013;88(2):113–121. PubMed
- Skinner HA. The Drug Abuse Screening Test. Addict Behav. 1982;7(4):363–371. PubMed CrossRef
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcohol Clin Exp Res. 2002;26(2):272–279. PubMed
- Budson AE, Solomon PR. Memory Loss, Alzheimer’s Disease, and Dementia: A Practical Guide for Clinicians. Elsevier Health Sciences; 2021.
- Vemuri P, Graff-Radford J, Lesnick TG, et al. White matter abnormalities are key components of cerebrovascular disease impacting cognitive decline. Brain Commun. 2021;3(2):fcab076. PubMed CrossRef
- Kazmierska-Grebowska P, Jankowski MM, MacIver MB. Missing puzzle pieces in dementia research: HCN channels and theta oscillations. Aging Dis. 2024;15(1):22–42. PubMed
- Wan W, Gao Z, Zhang Q, et al. Resting state EEG complexity as a predictor of cognitive performance. Phys A Stat Mech Appl. 2023;624:128952.
- Cuoco S, Cappiello A, Scarpa A, et al. Neuropsychological profile of hearing impaired patients and the effect of hearing aid on cognitive functions: an exploratory study. Sci Rep. 2021;11(1):9384. PubMed
- Wang HF, Zhang W, Rolls ET, et al; Alzheimer’s Disease Neuroimaging Initiative. Hearing impairment is associated with cognitive decline, brain atrophy and tau pathology. EBioMedicine. 2022;86:104336. PubMed CrossRef
- Lin FR, Pike JR, Albert MS, et al; ACHIEVE Collaborative Research Group. Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. Lancet. 2023;402(10404):786–797. PubMed
- Zheng DD, Swenor BK, Christ SL, et al. Longitudinal associations between visual impairment and cognitive functioning: the salisbury eye evaluation study. JAMA Ophthalmol. 2018;136(9):989–995. PubMed CrossRef
- Cao GY, Chen ZS, Yao SS, et al. The association between vision impairment and cognitive outcomes in older adults: a systematic review and meta-analysis. Aging Ment Health. 2023;27(2):350–356. PubMed CrossRef
- Nagarajan N, Assi L, Varadaraj V, et al. Vision impairment and cognitive decline among older adults: a systematic review. BMJ Open. 2022;12(1):e047929. PubMed CrossRef
- Senthilvel E, Auckley D, Dasarathy J. Evaluation of sleep disorders in the primary care setting: history taking compared to questionnaires. J Clin Sleep Med. 2011;7(1):41–48. PubMed
- Walker MP. Cognitive consequences of sleep and sleep loss. Sleep Med. 2008;9(suppl 1):S29–S34. PubMed CrossRef
- Roniger DDG, Lechuga YA, León EE, et al. Cognitive behavioral therapy for insomnia helps to reverse cognitive impairment in insomnia patients. Sleep Sci. 2022;15(Spec 2):355–360. PubMed CrossRef
- Beebe DW, Groesz L, Wells C, et al. The neuropsychological effects of obstructive sleep apnea: a meta-analysis of norm-referenced and case-controlled data. Sleep. 2003;26(3):298–307. PubMed CrossRef
- Stranks EK, Crowe SF. The cognitive effects of obstructive sleep apnea: an updated meta-analysis. Arch Clin Neuropsychol. 2016;31(2):186–193. PubMed CrossRef
- Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and OSA: implications for comorbidities. Chest. 2015;147(1):266–274. PubMed CrossRef
- Costa YS, Lim ASP, Thorpe KE, et al. Investigating changes in cognition associated with the use of CPAP in cognitive impairment and dementia: a retrospective study. Sleep Med. 2023;101:437–444. PubMed CrossRef
- Castronovo V, Scifo P, Castellano A, et al. White matter integrity in obstructive sleep apnea before and after treatment. Sleep. 2014;37(9):1465–1475. PubMed CrossRef
- Doneh B. Epworth Sleepiness Scale. Occup Med (Lond). 2015;65(6):508. PubMed
- Chung F, Abdullah HR, Liao P. STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149(3):631–638. PubMed CrossRef
- Svendsen AM, Kessing LV, Munkholm K, et al. Is there an association between subjective and objective measures of cognitive function in patients with affective disorders? Nord J Psychiatry. 2012;66(4):248–253. PubMed CrossRef
- Valkanova V, Ebmeier KP, Allan CL. Depression is linked to dementia in older adults. Practitioner. 2017;261(1800):11–15. PubMed
- Li XX, Li Z. The impact of anxiety on the progression of mild cognitive impairment to dementia in Chinese and English data bases: a systematic review and meta analysis. Int J Geriatr Psychiatry. 2018;33(1):131–140. PubMed CrossRef
- Rhee TG, Shim SR, Manning KJ, et al. Neuropsychological assessments of cognitive impairment in major depressive disorder: a systematic review and meta analysis with meta-regression. Psychother Psychosom. 2024;93(1):8–23. PubMed
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed CrossRef
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. PubMed CrossRef
- Katz J, Rosenbloom BN, Fashler S. Chronic pain, psychopathology, and DSM-5 somatic symptom disorder. Can J Psychiatry. 2015;60(4):160–167. PubMed CrossRef
- Rahman S, Kidwai A, Rakhamimova E, et al. Clinical diagnosis and treatment of chronic pain. Diagnostics (Basel). 2023;13(24):3689. PubMed CrossRef
- Larsson C, Hansson EE, Sundquist K, et al. Chronic pain in older adults: prevalence, incidence, and risk factors. Scand J Rheumatol. 2017;46(4):317–325. PubMed CrossRef
- van Hecke O, Torrance N, Smith BH. Chronic pain epidemiology - where do lifestyle factors fit in? Br J Pain. 2013;7(4):209–217. PubMed CrossRef
- Hedges D, Farrer TJ, Bigler ED, et al. The Brain at Risk: Associations between Disease and Cognition. Springer International Publishing; 2019.
- van der Leeuw G, Ayers E, Leveille SG, et al. The effect of pain on major cognitive impairment in older adults. J Pain. 2018;19(12):1435–1444. PubMed
- Hnatešen D, Radoš I, Dimitrijević I, et al. Influence of the cognitive and emotional status of patients with chronic pain on treatment success (reduction in pain intensity and adherence to pharmacotherapy): a prospective study. Int J Environ Res Public Health. 2022;19:15968. PubMed
- Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol. 2011;93(3):385–404. PubMed CrossRef
- Schoenberg MR, Soble JR, Osborn KE. Psychometrics of assessment: understanding what neuropsychology adds to the physician’s understanding of the patient. In: Sanders KM, ed. Physician’s Field Guide to Neuropsychology: Collaboration Through Case Example. Springer; 2019:45–60.
- American Academy of Clinical Neuropsychology. American Academy of Clinical Neuropsychology (AACN) practice guidelines for neuropsychological assessment and consultation. Clin Neuropsychol. 2007;21(2):209–231. PubMed CrossRef
- Braun MM. The Value of Neuropsychological Evaluation in Medical Practice. In: Sanders KM, ed. Physician’s Field Guide to Neuropsychology: Collaboration Through Case Example. Springer; 2019:3–15.
- Lezak MD, Howieson DB, Bigler ED, et al. Neuropsychological Assessment. Oxford University Press; 2012.
- Mahoney JJ 3rd, Bajo SD, De Marco AP, et al. Referring providers’ preferences and satisfaction with neuropsychological services. Arch Clin Neuropsychol. 2017;32(4):427–436. PubMed CrossRef
- Temple RO, Carvalho J, Tremont G. A national survey of physicians’ use of and satisfaction with neuropsychological services. Arch Clin Neuropsychol. 2006;21(5):371–382. PubMed CrossRef
- Tremont G, Westervelt HJ, Javorsky DJ, et al. Referring physicians’ perceptions of the neuropsychological evaluation: how are we doing? Clin Neuropsychol. 2002;16(4):551–554. PubMed CrossRef
- Schaefer LA, Farrer TJ. The role of the psychologist in the assessment of capacity. In: Schaefer LA, Farrer TJ, A Casebook of Mental Capacity in US Legislation: Assessment and Legal Commentary. Routledge; 2022:12–23.
- Hilsabeck RC, Hietpas TL, McCoy KJM. Satisfaction of referring providers with neuropsychological services within a Veterans Administration medical center. Arch Clin Neuropsychol. 2014;29(2):131–140. PubMed CrossRef
- Fallows R. Integration of neuropsychology into primary care: a retrospective analysis of outcomes and lessons learned from a single provider practice. Prof Psychol Res Pract. 2019;50(6):419–426.
- Lanca M. Integration of neuropsychology in primary care. Arch Clin Neuropsychol. 2018;33(3):269–279. PubMed CrossRef
- Schroeder RW, Martin PK, Walling A. Neuropsychological evaluations in adults. Am Fam Physician. 2019;99(2):101–108. PubMed
- Wechsler D. Wechsler Adult Intelligence Scale–Fourth Edition (WAIS-IV). APA PsycTests; 2008.
- Army Individual Test Battery. Manual of Directions and Scoring. War Department, Adjutant General’s Office; 1994.
- Grant DA, Berg EA. Wisconsin Card Sorting Test [Database Record]. APA PsycTests; 1948.
- Delis DC, Kaplan E, Kramer JH. Delis-Kaplan Executive Function System (D–KEFS). APA PsycTests; 2001.
- Defilippis NA, McCampbell E. The Booklet Category Test Professional Manual. Psychological Assessment Resources; 1991.
- Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–662.
- Benton AL, Hamsher K, Varney NR, et al. Contributions to Neuropsychological Assessment: A Clinical Manual. Oxford; 1983.
- Kao GS, Thomas HM. Test review: C. Keith Conners Conners 3rd edition Toronto, Ontario, Canada: multi-health systems, 2008. J Psychoeduc Assess. 2010;28(6):598–602.
- Wechsler D. Wechsler Memory Scale–Fourth Edition (WMS-IV) Technical and Interpretive Manual. Pearson; 2009.
- Delis DC, Kramer JH, Kaplan E, et al. California Verbal Learning Test–3. 3rd edition. The Psychological Corporation; 2017.
- Rey A, Osterrieth PA. Rey-Osterrieth Complex Figure Copying Test [Database Record]. APA PsycTests; 1941.
- Kaplan E, Goodglass H, Weintraub S. Boston Naming Test (BNT) [Database Record]. APA PsycTests; 1983.
- De Renzi E, Vignolo LA. The Token Test: a sensitive test to detect receptive disturbances in aphasics. Brain. 1962;85:665–678. PubMed CrossRef
- Hooper HE. Hooper Visual Organization Test Manual. Western Psychological Services; 1983.
- Kaplan E. A Process Approach to Neuropsychological Assessment. In: Boll T, Bryant BK, eds. Clinical Neuropsychology and Brain Function: Research, Measurement, and Practice. American Psychological Association; 1988.
- Beck AT, Ward CH, Mendelson M, et al. Beck Depression Inventory (BDI) [Database Record]. APA PsycTests; 1961.
- Beck AT, Epstein N, Brown G, et al. Beck Anxiety Inventory [Database Record]. APA PsycTests; 1988.
- Ben-Porath YS, Tellegen A. Minnesota Multiphasic Personality Inventory-2- Restructured Form (MMPI-2-RF): Manual for Administration, Scoring, and Interpretation. University of Minnesota Press; 2008.
- Morey LC. The Personality Assessment Inventory (PAI). In: Maruish ME, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. 3rd ed. Lawrence Erlbaum Associates Publishers; 2004:509–551.
- Schaefer LA. Functional assessment. In: Bush, SS, Yochim, BP, eds. A Handbook of Geriatric Neuropsychology: Practice Essentials (Second Edition). Routledge; 2022: 324-340.
This PDF is free for all visitors!