Abstract
Objective: Insomnia and some insomnia treatments can impact an individual’s daytime functioning. Here, we performed post hoc analyses of patient-reported outcomes from a phase 3 clinical trial to assess the impact of lemborexant (LEM), a dual orexin receptor antagonist, on daytime functioning.
Methods: Adults with insomnia were randomized 1:1:1 to receive placebo, LEM 5 mg (LEM5) or LEM 10 mg (LEM10) for 6 months. Treatment impact on subjects’ perceptions of their insomnia symptoms and daytime functioning was assessed by the Insomnia Severity Index (ISI) and Fatigue Severity Scale (FSS) questionnaires. Safety assessments included monitoring of treatment emergent adverse events.
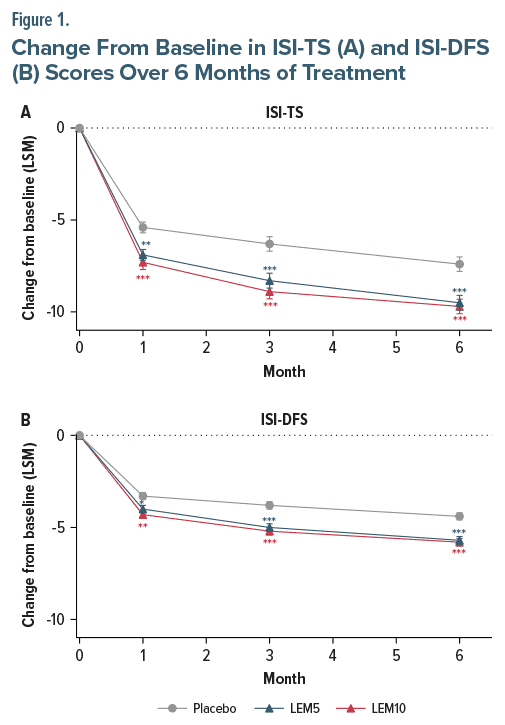
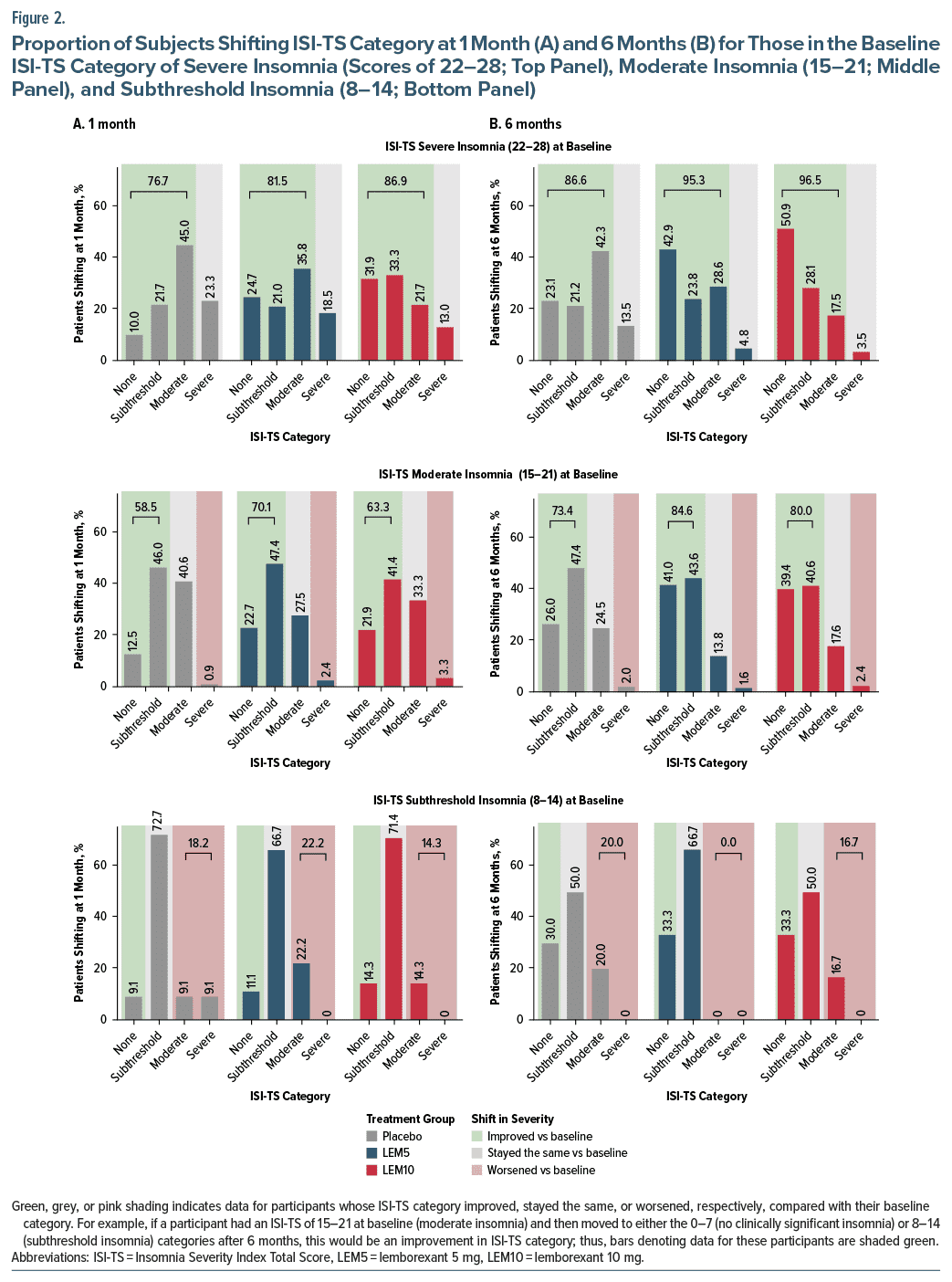
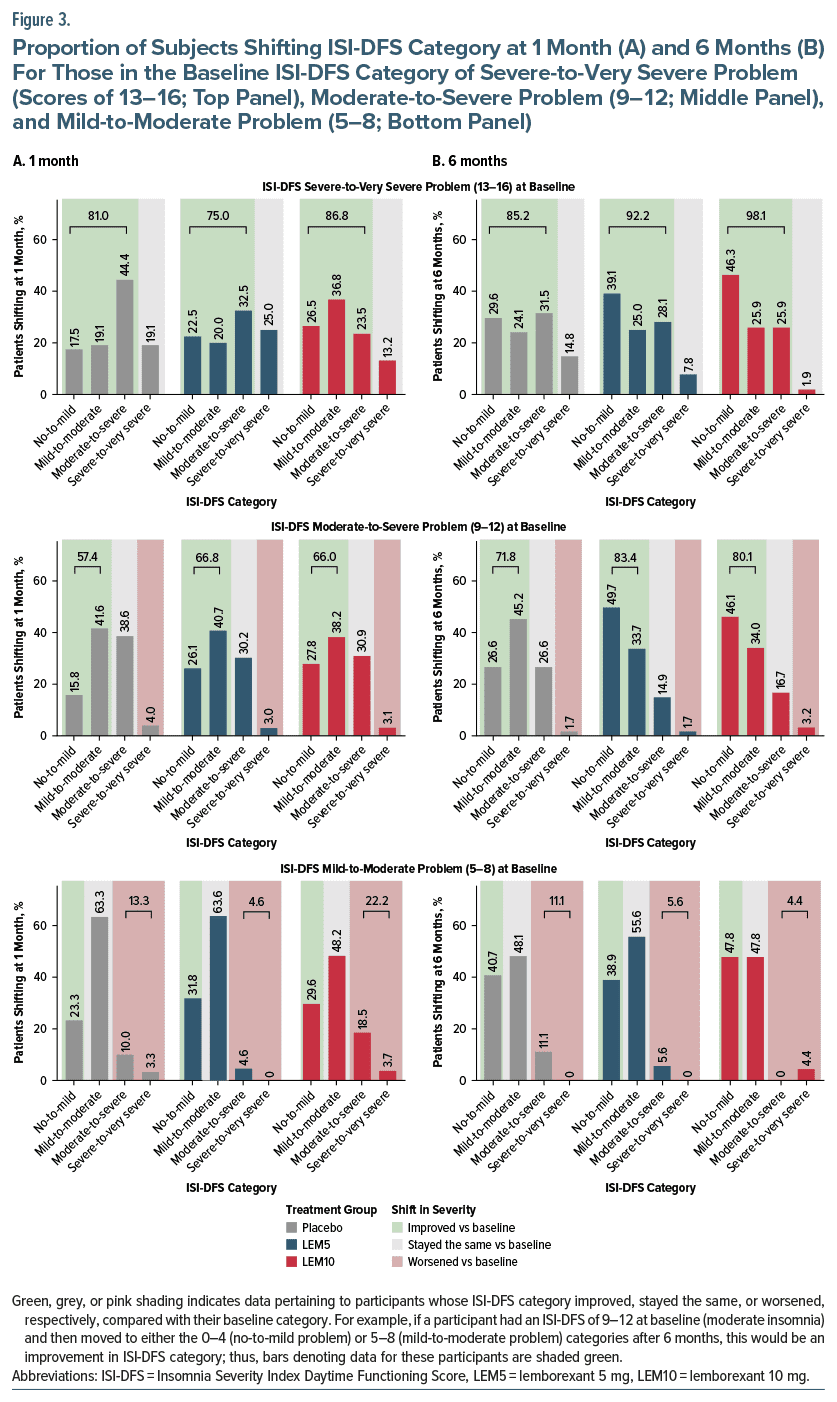
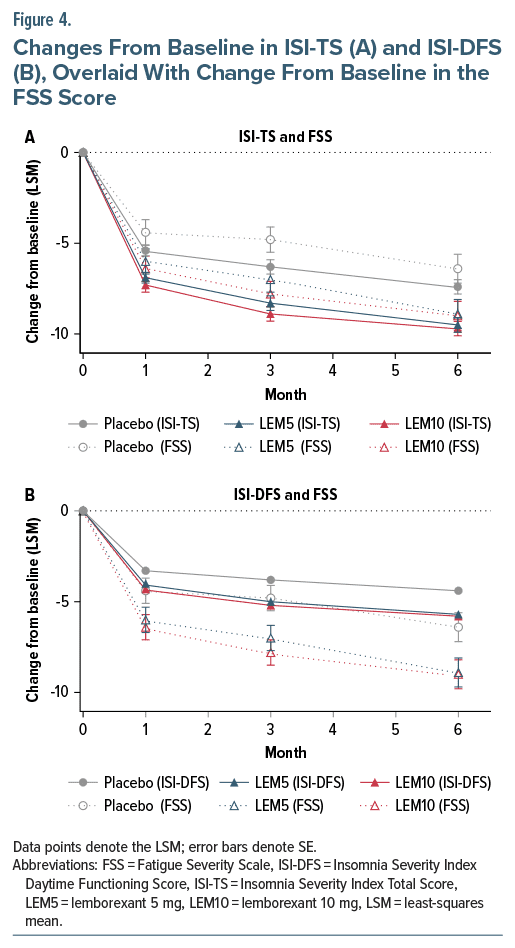
Results: Compared with placebo, LEM5 and LEM10 treatment significantly improved ISI Total Score (ISI-TS) (LEM5, P < .01; LEM10, P < .0001) and ISI Daytime Functioning Score (ISI-DFS) (LEM5, P < .05; LEM10, P < .01) at 1 month; these improvements were maintained at the end of 6 months (P < .0001 for LEM5 and LEM10, both scores). In separate analyses, baseline ISI-TS or ISI-DFS was used to classify subjects’ symptom severity into 1 of 4 categories. At 1 and 6 months, greater proportions of subjects treated with LEM5 and LEM10 shifted to a category associated with less severe symptoms (P < .01 for all comparisons vs placebo). FSS score also improved with LEM treatment vs placebo as assessed at month 3; improvements were maintained at month 6 (P < .05). LEM5 and LEM10 treatment was well tolerated.
Conclusion: Improved insomnia symptoms with LEM treatment may translate into improved daytime functioning, suggesting LEM may be appropriate for adults experiencing daytime impairment with their nighttime symptoms.
Trial Registration: ClinicalTrials.gov identifier: NCT02952820.
Prim Care Companion CNS Disord 2025;27(1):24m03810
Author affiliations are listed at the end of this article.
Individuals with insomnia experience daytime impairment that has a substantial impact on quality of life and also presents potential safety concerns. Impacts of daytime impairment include fatigue, daytime sleepiness, impaired cognitive performance, lost productivity, impaired driving, social isolation (including adverse effects on familial relationships), and depression/anxiety.1–3
Many options exist to improve sleep, but these can have different effects on daytime functioning. For example, reductions in insomnia symptoms with cognitive behavioral therapy for insomnia (CBT-I) have been associated with positive effects on daytime symptoms such as sleepiness, fatigue, social functioning, and mental state.4,5 In contrast, γ-aminobutyric acid type A (GABA-A) receptor modulators that improve nighttime sleep, such as benzodiazepines and nonbenzodiazepine Z-drugs, may negatively impact daytime functioning,2,6,7 increasing the likelihood of motor vehicle and industrial accidents.8,9 Since CBT-I may not be effective, appropriate, or available for all individuals suffering from insomnia, an important unmet need exists for pharmacologic therapies that improve sleep quality with limited next-day impairment.10
Lemborexant (LEM) is a competitive dual orexin receptor antagonist (DORA).11,12 DORAs suppress orexin signaling, which regulates arousal and the sleep-wake cycle, in contrast with the broader central nervous system–depressing effects of GABA-A receptor modulators that promote sedation. Inhibition of orexin receptors allows sleep to occur by selectively reducing the activity of neurons promoting wakefulness, and this unique mechanism of action may be less likely to trigger some of the side effects associated with the broader neuronal inhibition induced by GABA-A receptor modulators, including impairments in motor function, cognition, and memory.13 A difference in daytime impairment is also supported by differing effects on sleep architecture: benzodiazepines suppress N3 slow-wave and rapid eye movement (REM) sleep, whereas in studies in older individuals with insomnia, LEM did not suppress N3 slow-wave sleep and instead increased REM sleep and total non-REM sleep while also reducing latency to REM sleep.14,15 The suppression of some aspects of sleep architecture with benzodiazepines might result in reduced daytime functioning due to cognition and memory deficits, whereas the maintenance and enhancement of REM sleep with LEM may preserve some of the functional benefits of REM sleep on memory and cognition.14,15 Comorbid conditions such as obstructive sleep apnea (OSA) also disrupt REM sleep, and LEM has been shown to increase both total sleep time and REM sleep relative to zolpidem extended release in subjects with mild OSA.16 The effects of LEM on sleep architecture may therefore impact daytime functioning and fatigue, including in individuals with comorbid conditions that affect sleep structure.14,15
In light of the potential impact of LEM on daytime functioning, patient-reported outcomes on daytime and nighttime symptoms were collected in 2 pivotal phase 3 studies.17–19 The results showed that sleep onset and sleep maintenance were significantly improved in subjects treated with LEM compared with placebo. Here, we present data comparing the effects of LEM versus placebo on daytime functioning during the 6-month, placebo-controlled portion of Study E2006-G000-303 (Study 303; SUNRISE-2).
METHODS
Study Design
Study 303 was a 12-month, global, multicenter, randomized, placebo-controlled, double-blind, parallel group phase 3 study. Full details of the study design have been published previously.19
Subjects were randomized 1:1:1 to receive placebo, LEM 5 mg (LEM5), or LEM 10 mg (LEM10) during the study’s initial 6-month, placebo-controlled treatment period 1 (TP1). This was followed by a 6-month treatment period 2 (TP2), where subjects who received placebo in TP1 were rerandomized 1:1 to receive LEM5 or LEM10; those assigned to LEM during TP1 remained on their original treatment regimen for TP2. Only results from TP1 are reported in this analysis.
The protocol for the study was approved by the relevant institutional review boards or ethics committees, and the studies were conducted in accordance with the Declaration of Helsinki, Good Clinical Practice guidelines, and applicable laws and regulations. All participants provided written informed consent before participation. The study was registered at ClinicalTrials.gov (identifier: NCT02952820).
Study Population
Subjects were adults (aged ≥18 years) who met the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for insomnia disorder.20 Inclusion criteria included an Insomnia Severity Index total score (ISI-TS) ≥15 and either sleep onset (subjective sleep onset latency ≥30 minutes) or sleep maintenance (subjective wake after sleep onset ≥60 minutes ≥3 times a week in the previous 4 weeks) problems, or both. Subjects with controlled medical and/or psychiatric conditions were eligible for the study; however, those with other sleep disorders, including OSA, periodic limb movement disorder, restless leg syndrome, circadian rhythm sleep disorder, narcolepsy, and certain parasomnias, were excluded. Full exclusion and inclusion criteria have been published previously.19
Assessments
Subjects’ perceptions of the severity of their insomnia were assessed via the 7-item ISI questionnaire, with items rated on a 5-point Likert scale ranging from 0 (no problem) to 4 (very severe problem).21 The ISI survey was administered at baseline (at the end of the placebo run-in) and at the end of months 1, 3, and 6. Responses to the 7 items were summed to produce the ISI-TS, which has a maximum score of 28. The ISI daytime functioning score (ISI-DFS) was calculated as the sum of scores for ISI items 4–7, which are related to daytime functioning. The ISI-DFS has a maximum score of 16. The score for the ISI “interference with daily functioning” item was also analyzed separately here.
The Fatigue Severity Scale (FSS) questionnaire was administered at baseline and at the end of months 1, 3, and 6.22,23 Subjects rated their responses to 9 items using a 7-point Likert scale (range, 1–7), with higher scores indicating a greater degree of fatigue.
Safety assessments included monitoring of treatment emergent adverse events (TEAEs), clinical laboratory evaluations, vital signs, assessment of falls, weight, electrocardiograms, suicidality, and physical examinations.
Statistical Analyses
The full analysis set was defined as all randomized subjects receiving ≥1 dose of study drug who had ≥1 postdose primary efficacy measurement.
For ISI-TS, ISI-DFS, the ISI “interference with daily functioning” item, and the FSS, least-squares mean (LSM) change from baseline was calculated for months 1, 3, and 6, and treatment differences relative to placebo were calculated based on a mixed-effect model repeated measurement analysis, with age group, region, treatment, clinic visit, and treatment-by-visit interaction as fixed effects and baseline score as a covariate.
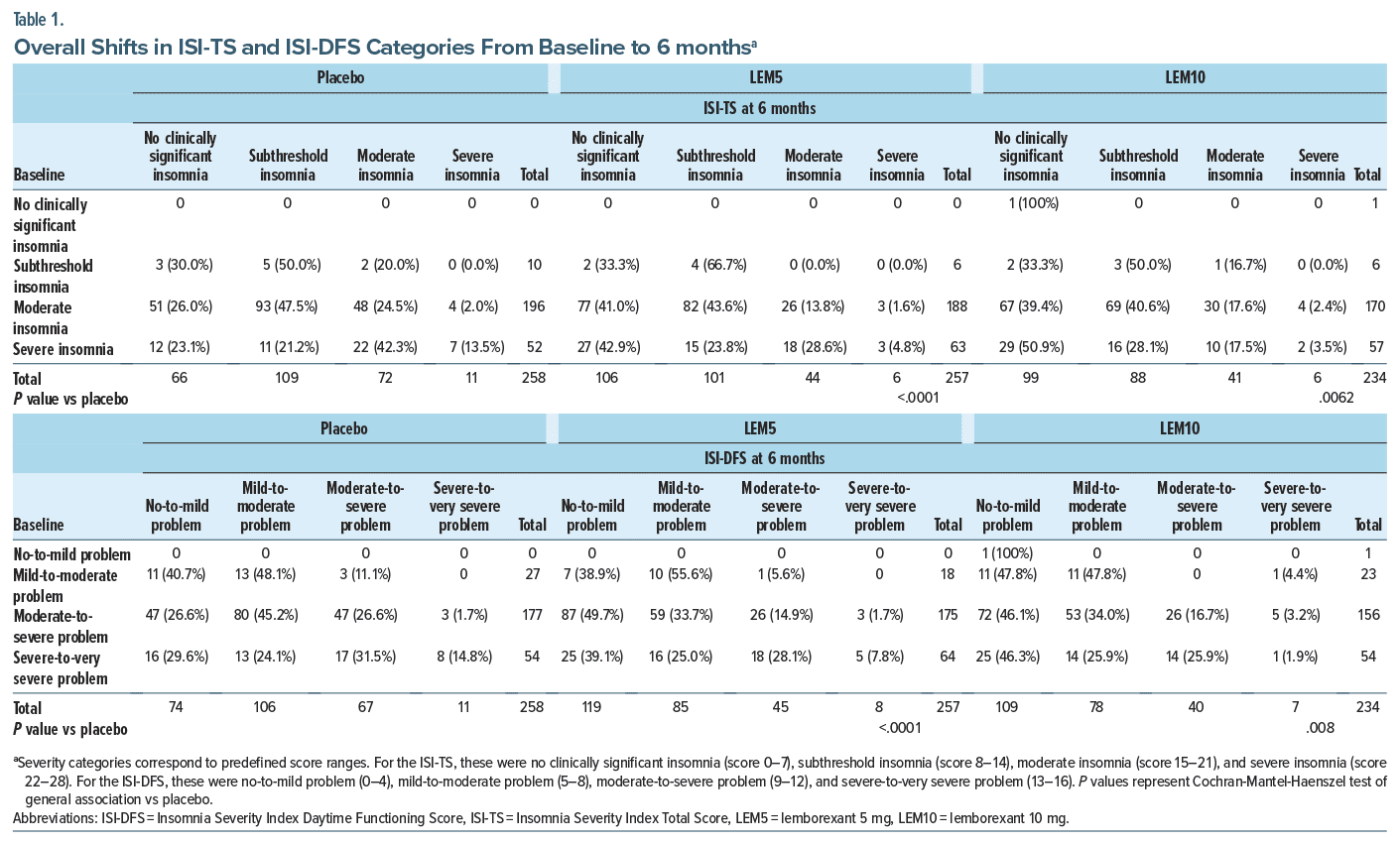
The impact of treatment on ISI-TS, ISI-DFS, and FSS score was assessed as follows: (1) Subjects with clinically significant fatigue were defined as those with FSS ≥36.24,25 (2) A subject’s ISI-TS was categorized as no clinically significant insomnia (score 0–7), subthreshold insomnia (score 8–14), moderate insomnia (score 15–21), and severe insomnia (score 22–28). (3) A subject’s ISI-DFS was categorized as no-to-mild problem (score 0–4), mild-to-moderate problem (score 5–8), moderate-to-severe problem (score 9–12), and severe to-very severe problem (score 13–16). (4) For the ISI “interference with daily functioning” item, subjects more severely affected (baseline score 3 or 4) were compared with those less affected (score 0–2).
The proportion of subjects shifting from one symptom-severity category at baseline to another at months 1 and 6 was assessed to determine differences versus placebo.
The ISI-TS and ISI-DFS shift data were analyzed by a Cochran-Mantel-Haenszel test of general association for LEM5 or LEM10 compared with placebo and χ2 tests comparing improvement to staying the same or worsening within each baseline group for LEM5 or LEM10 compared with placebo. For the FSS score, comparisons of proportions of responders to treatment (those achieving FSS scores <36) between treatment groups were based on a Cochran-Mantel-Haenszel test stratified by region and age group.24
All statistical analyses were performed using SAS v9.4 (SAS Institute Inc, Cary, North Carolina).
RESULTS
Baseline Demographic and Clinical Characteristics
Baseline characteristics were similar across treatment groups and have been reported previously (Supplementary Table 1).18,19,24 Most subjects were female (68.2%) and white (71.5%); 17.0% were Japanese, and 8.0% were black or African American. The median age was 55 years (range, 18–88 years), and most subjects (61.6%) had a body mass index ≥25 kg/m2. Mean ISI-TS at baseline was in the moderate insomnia range for all treatments (19.0 in the placebo group, 19.6 in the LEM5 group, and 19.1 in the LEM10 group). Mean ISI-DFS at baseline was in the moderate-to-severe problem range (11.0 in the placebo group, 11.4 in the LEM5 group, and 11.1 in the LEM10 group), and the mean ISI “interference with daily functioning” score was in the somewhat-to-much range (item score of 2 or 3) at baseline (2.6 in the placebo and LEM10 groups and 2.7 in the LEM5 group). Mean FSS score was relatively consistent among treatment groups (mean [SD]: placebo 35.1 [13.6], LEM5 37.4 [12.7], and LEM10 36.0 [13.0]).
Change From Baseline in ISI-TS and DFS
LSM ISI-TS and ISI-DFS decreased from baseline across all treatment groups, as assessed at the end of 1 month and 6 months (Figure 1). These decreases at 6 months were significantly greater with LEM5 and LEM10 compared with placebo (both P < .0001; Figure 1). The ISI-TS data were previously reported by Roth et al as means (and not LSMs).26
Change in ISI-DFS accounted for approximately 60% of the change in ISI-TS (range, 58.0–61.1), roughly proportional to the percentage of ISI items included in the DFS (4/7; 57%).
Shifts in ISI and FSS Score Categories From Baseline
Shifts in ISI-TS category at 1 month and 6 months for subjects in the severe (22–28), moderate (15–21), and subthreshold insomnia (8–14) categories at baseline are shown graphically in Figure 2 and with numbers of subjects and statistical comparisons in Table 1 and Supplementary Table 2. Shifts in ISI-DFS category at 1 month and 6 months for subjects in the severe-to-very severe problem (13–16), moderate-to-severe problem (9–12), and mild-to-moderate problem (5–8) categories are shown in Figure 3, Table 1, and Supplementary Table 2. Data for those with no clinically significant insomnia at baseline (ISI-TS 0–7) and no-to-mild problems with daytime functioning (ISI-DFS 0–4) are not depicted in the figures, as there was only 1 subject in this category at baseline (in the LEM10 group).
At 1 and 6 months, the overall shift changes for both ISI-TS and ISI-DFS (indicating improvement from more severe symptoms/impairment) indicated beneficial changes with both LEM5 and LEM10 compared with placebo (P < .05 for all comparisons; Table 1). Of note, about twice as many subjects in the LEM5 (42.9%) and LEM10 (50%) groups shifted from severe insomnia to no clinically significant insomnia than in the placebo group (23.1%) at month 6 for ISI-TS (Figure 2). Comparisons of shifts from baseline in ISI-DFS category at 6 months indicated that subjects receiving LEM significantly improved in terms of insomnia symptom severity post treatment versus placebo (P < .01). Analysis of the overall shift from baseline categories in the ISI “interference with daily functioning” item score for those reporting more interference with daily functioning (a score of 3 or 4) showed significant improvements (P < .05) for LEM over placebo at 6 months but not at 1 month (Supplementary Table 3).
As reported previously, 170/318 (53.5%) of the subjects receiving placebo had clinically significant fatigue (FSS score ≥36) at baseline, decreasing to 113/296 (38.2%) at the end of 1 month (57 responders) and 105/257 (40.9%) at 6 months (65 responders).24 For LEM5, 181/316 (57.3%) had clinically significant fatigue at baseline, decreasing to 108/300 (36.0%) at 1 month (73 responders; P = .249 vs placebo) and 102/258 (39.5%) at 6 months (79 responders; P = .2838 vs placebo). For LEM10, 173/315 (54.9%) had clinically significant fatigue at baseline, decreasing to 97/286 (33.9%) at 1 month (76 responders; P = .0402 vs placebo) and 91/234 (38.9%) at 6 months (82 responders; P = .0765 vs placebo).
Comparison of Changes From Baseline in ISI-DFS, ISI-TS, and FSS Score
Plots showing the LSM changes from baseline in ISI TS and ISI-DFS overlaid with the FSS score are shown in Figure 4. FSS score change from baseline was previously reported.24 At the end of 1 month, only the change from baseline in FSS score for LEM10 in Study 303 was significantly improved over placebo; by 3 months, both LEM5 and LEM10 demonstrated significant improvement over placebo, which was maintained at 6 months. The changes over time in the ISI scores mirror the changes in the FSS score, indicating the trends in FSS score reduction are consistent with the trends in ISI-TS and ISI-DFS over 6 months.
Safety
Adverse reactions observed in this clinical trial have been reported elsewhere17,19 and are summarized in the supplementary material (Supplementary Table 4). The most frequent TEAEs (>5% in any treatment group) were headache, somnolence, and influenza.
Study drug discontinuations due to the TEAE of somnolence occurred in 2 subjects in the placebo group, 3 in the LEM5 group, and 9 in the LEM10 group. These TEAEs were generally rated mild or moderate in severity, except for 1 subject in the placebo group who reported severe somnolence. Half of those subjects discontinuing due to somnolence were within the first 30 days of treatment. All those who discontinued due to somnolence reported that the TEAE had resolved subsequently.
DISCUSSION
Post hoc analyses of patient-reported outcomes reflecting insomnia symptom severity and impact on daytime functioning in this phase 3 study indicate that the insomnia symptom improvement associated with LEM treatment compared with placebo may translate into improved daytime functioning. Significant improvements with LEM versus placebo were apparent at 1 month and maintained for 6 months. Data regarding the percentage of participants who experienced a shift from worse to better score categories for ISI-TS, ISI DFS, and the ISI “interference with daily functioning” item indicate that a significantly greater proportion of subjects treated with LEM experienced meaningful improvements in ISI symptom severity and daytime functioning than those receiving placebo, particularly those in the more severe score categories at baseline.
These improvements were mirrored by decreases in fatigue severity according to changes in FSS scores. However, FSS score change from baseline and ISI “interference with daily functioning” item shift data did not show significant improvements over placebo for both doses until 3 months24 and 6 months, respectively, indicating that improvements in fatigue and interference with daily functioning potentially lag improvements in overall symptoms and daytime functioning. Finally, LEM was well tolerated during the study, with most TEAEs being of mild/moderate severity.
A lack of impairment at the time of awakening in subjects treated with LEM has already been reported, and these new analyses supplement those previously published by providing additional details regarding improvement in specific daytime functioning measures.27 Assessment of next-morning cognitive impairments through analysis of driving capabilities after administration of LEM has shown no clinically meaningful residual effects.28 In contrast, benzodiazepines and benzodiazepine receptor agonists are associated with increased risk of vehicular and other accidents due to psychomotor impairment.9,29,30
The strengths of this study include the large number of participants and the global, multicenter, randomized, double-blind, parallel-group, placebo-controlled design. Additionally, subjects with controlled medical/ psychiatric conditions were eligible for this study, reflecting the heterogeneous subject pool encountered by primary care physicians. Limitations include the fixed dosing, which prevented dose titration, and the post hoc nature of the analyses. Nonetheless, these data provide useful insights for further investigation.
In conclusion, these results suggest that LEM may be appropriate for individuals with insomnia who experience fatigue or impaired daytime functioning in addition to their nighttime symptoms.
Article Information
Published Online: January 16, 2025. https://doi.org/10.4088/PCC.24m03810
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 9, 2024; accepted September 20, 2024.
To Cite: Chepke C, Cote KA, Pinner K, et al. Effect of lemborexant on daytime functioning in adults with insomnia: patient-reported outcomes from a phase 3 clinical trial. Prim Care Companion CNS Disord. 2025;27(1):24m03810.
Author Affiliations: Excel Psychiatric Associates, Huntersville, North Carolina (Chepke); Atrium Health, Charlotte, North Carolina (Chepke); Psychology Department, Brock University, St. Catharines, Ontario, Canada (Cote); Eisai Ltd, Hatfield, United Kingdom (Pinner, Yardley); Eisai Inc, Nutley, New Jersey (Lundwall, Moline); Former Employee of Eisai, Inc (Lundwall).
Corresponding Author: Margaret Moline, PhD, Eisai Inc, 200 Metro Blvd, Nutley, NJ 07110 ([email protected]).
Relevant Financial Relationships: Dr Chepke has received grant or research support from Acadia, Axsome, Harmony, Neurocrine, and Teva; served as a consultant for AbbVie, Arcadia, Alkermes, Axsome, Biogen, Boehringer Ingelheim, Corium, Intra Cellular, Janssen, Karuna, Lundbeck, MedinCell, Moderna, Neurocrine, Noven, Otsuka, Sage, Sumitomo, Supernus, and Teva; received payment or honoraria for educational activities from AbbVie, Acadia, Alkernes, Axsome, Bristol Myers Squibb, Corium, Intra Cellular, Janssen, Karuna, Lundbeck, Merck, Neurocrine, Noven, Otsuka, Sumitomo, and Teva; received support for attending meetings/travel from AbbVie, Acadia, Alkermes, Axsome, Bristol-Myers Squibb, Corium, Intra-Cellular, Janssen, Karuna, Lundbeck, Merck, Neurocrine, Noven, Otsuka, Sumitomo, and Teva; and has served on advisory or data safety monitoring boards for AbbVie, Acadia, Alkermes, Axsome, Biogen, Bristol-Myers Squibb, Corium, Idorsia, Intra-Cellular, Janssen, Karun, Lundbeck, Moderna, Neurocrine, Noven, Otsuka, Sage, Sumitomo, and Teva. Dr Cote has served as a consultant for Eisai and received payment for lectures from Eisai. Ms Pinner and Dr Yardley are both employees of Eisai. Dr Lundwall is a current employee of and holds stock in Amgen and is a former employee of Eisai. Dr Moline is an employee of Eisai and a holder of patent WO2021127359-PAMPH-20210624-3482.
Funding/Support: The study and this analysis were supported by Eisai Inc, the owner and manufacturer of lemborexant.
Role of the Sponsor: Eisai Inc was involved in the study design, data collection, data analysis, and preparation of the manuscript. The authors had access to the data and control of the final approval and decision to submit the manuscript for publication.
Previous Presentations: Data from this manuscript have been presented in part as posters at: SLEEP 2019, the 33rd Annual Meeting of the Associated Professional Sleep Societies (APSS); 8–12 June 2019; San Antonio, Texas (Roth et al Poster 108). The American Society of Clinical Psychopharmacology (ASCP) 2020 Meeting (Virtual); 29–30 May 2020 (Moline et al and Chepke et al). SLEEP 2021, the 35th Annual Meeting of the APSS (Virtual); 10–13 June 2021 (Lenderking et al Poster 338). The Psych Congress 2022; 17–20 September 2022; New Orleans, Louisiana (Chepke et al Poster 26). SLEEP 2023, the 37th Annual Meeting of the APSS; 3–7 June 2023; Indianapolis, Indiana (Chepke et al Poster 301). Data from this manuscript in part are presented in Roth et al. Sleep Med. 2022;90:249–257.
Acknowledgments: Medical writing assistance was provided by Amy Volpert, MA, CMPP, Samantha Agron, MD, and Abigail Killen-Devine, DPhil, CMPP (Healthcare Consultancy Group), and editorial assistance by Kyle Lambe, MPH, CMPP (Healthcare Consultancy Group), with funding from Eisai Inc. They report no other conflicts of interest related to the subject of this article.
Supplementary Material: Available at Psychiatrist.com.
Clinical Points
- Improved insomnia symptoms with lemborexant (LEM) treatment may translate into improved daytime functioning.
- Larger and significant improvements in insomnia severity with LEM versus placebo were apparent at 1 month and maintained for 6 months.
- LEM may be appropriate for adults experiencing daytime impairment with their nighttime symptoms.
References (30)

- Muehlan C, Roch C, Vaillant C, et al. The orexin story and orexin receptor antagonists for the treatment of insomnia. J Sleep Res. 2023;32(6):e13902. PubMed
- Watson NF, Bertisch SM, Morin CM, et al. Do insomnia treatments improve daytime function? J Clin Med. 2023;12(9):3089.
- Gordon AM, Carrillo B, Barnes CM. Sleep and social relationships in healthy populations: a systematic review. Sleep Med Rev. 2021;57:101428.
- Kjørstad K, Sivertsen B, Vedaa Ø, et al. The effects of digital CBT-I on work productivity and activity levels and the mediational role of insomnia symptoms: data from a randomized controlled trial with 6-month follow-up. Behav Res Ther. 2022;153:104083. PubMed
- Benz F, Knoop T, Ballesio A, et al. The efficacy of cognitive and behavior therapies for insomnia on daytime symptoms: a systematic review and network meta-analysis. Clin Psychol Rev. 2020;80:101873. PubMed CrossRef
- De Crescenzo F, D’Alò GL, Ostinelli EG, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet. 2022;400(10347):170–184. PubMed
- Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504. PubMed
- Liu Y, Wheaton AG, Chapman DP, et al. Prevalence of healthy sleep duration among adults — United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. PubMed CrossRef
- Brandt J, Leong C. Benzodiazepines and Z-drugs: an updated review of major adverse outcomes reported on in epidemiologic research. Drugs R D. 2017;17(4):493–507. PubMed CrossRef
- Campbell R, Chabot I, Rousseau B, et al. Understanding the unmet needs in insomnia treatment: a systematic literature review of real-world evidence. Int J Neurosci. 2023;133(8):864–878. PubMed
- Beuckmann CT, Suzuki M, Ueno T, et al. In vitro and in silico characterization of lemborexant (E2006), a novel dual orexin receptor antagonist. J Pharmacol Exp Ther. 2017;362(2):287–295.
- Wang C, Wang Q, Ji B, et al. The orexin/receptor system: molecular mechanism and therapeutic potential for neurological diseases. Front Mol Neurosci. 2018;11:280.
- Roch C, Bergamini G, Steiner MA, et al. Nonclinical pharmacology of daridorexant: a new dual orexin receptor antagonist for the treatment of insomnia. Psychopharmacology (Berl). 2021;238(10):2693–2708. PubMed
- Moline M, Zammit G, Cheng JY, et al. Comparison of the effect of lemborexant with placebo and zolpidem tartrate extended release on sleep architecture in older adults with insomnia disorder. J Clin Sleep Med. 2021;17(6):1167–1174.
- Monti JM, Torterolo P, Pandi-Perumal SR. The effects of benzodiazepine and nonbenzodiazepine agents, ramelteon, low-dose doxepin, suvorexant, and selective serotonin 5-HT2A receptor antagonists and inverse agonists on sleep and wakefulness. Clin Med Insights Ther. 2016;8:CMT.S38232.
- Kushida C, Zammit G, Cheng J, et al. 0354 effect of lemborexant on sleep architecture in subjects with comorbid insomnia and mild obstructive sleep apnea from a Ph 3 trial. Sleep. 2023;46(Suppl 1):A157.
- Yardley J, Kärppä M, Inoue Y, et al. Long-term effectiveness and safety of lemborexant in adults with insomnia disorder: results from a phase 3 randomized clinical trial. Sleep Med. 2021;80:333–342.
- Rosenberg R, Murphy P, Zammit G, et al. Comparison of lemborexant with placebo and zolpidem tartrate extended release for the treatment of older adults with insomnia disorder: a phase 3 randomized clinical trial. JAMA Netw Open. 2019;2(12):e1918254. PubMed
- Kärppä M, Yardley J, Pinner K, et al. Long-term efficacy and tolerability of lemborexant compared with placebo in adults with insomnia disorder: results from the phase 3 randomized clinical trial SUNRISE 2. Sleep. 2020;43(9):zsaa123. PubMed
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5�. 5th ed. American Psychiatric Association; 2013.
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. PubMed CrossRef
- Valko PO, Bassetti CL, Bloch KE, et al. Validation of the fatigue severity scale in a Swiss cohort. Sleep. 2008;31(11):1601–1607. PubMed CrossRef
- Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. PubMed CrossRef
- Chepke C, Jain R, Rosenberg R, et al. Improvement in fatigue and sleep measures with the dual orexin receptor antagonist lemborexant in adults with insomnia disorder. Postgrad Med. 2022;134(3):316–325.
- Rosti-Otajärvi E, Hämäläinen P, Wiksten A, et al. Validity and reliability of the Fatigue Severity Scale in Finnish multiple sclerosis patients. Brain Behav. 2017;7(7):e00743. PubMed CrossRef
- Roth T, Rosenberg R, Morin CM, et al. Impact of lemborexant treatment on insomnia severity: analyses from a 12-month study of adults with insomnia disorder. Sleep Med. 2022;90:249–257.
- Moline M, Zammit G, Yardley J, et al. Lack of residual morning effects of lemborexant treatment for insomnia: summary of findings across 9 clinical trials. Postgrad Med. 2021;133(1):71–81.
- Vermeeren A, Jongen S, Murphy P, et al. On-the-road driving performance the morning after bedtime administration of lemborexant in healthy adult and elderly volunteers. Sleep. 2019;42(4):zsy260. PubMed
- Dassanayake T, Michie P, Carter G, et al. Effects of benzodiazepines, antidepressants and opioids on driving: a systematic review and meta-analysis of epidemiological and experimental evidence. Drug Saf. 2011;34(2):125–156. PubMed CrossRef
- Smink BE, Egberts AC, Lusthof KJ, et al. The relationship between benzodiazepine use and traffic accidents: a systematic literature review. CNS Drugs. 2010;24(8):639–653. PubMed CrossRef
This PDF is free for all visitors!