Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(1):24f03793
Author affiliations are listed at the end of this article.
Have you ever wondered whether sedative hypnotics are necessary for most patients admitted to general hospitals? Have you been uncertain about which agents (and in what doses and for how long) and other nonpharmacologic interventions to use? Have you wondered whether the use of sedative-hypnotics is safe and effective in hospitalized patients? Have you been unclear about whose responsibility it is to discuss the potential side effects of these agents with patients? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Mr A, a 70-year-old man with coronary artery disease (CAD), diabetes mellitus, and chronic kidney disease, was admitted to the coronary care unit to rule out a myocardial infarction following the onset of substernal chest pain. His psychiatric history included a distant history of major depressive disorder (MDD) and generalized anxiety disorder (GAD). His outpatient psychotropic regimen included lorazepam (1 mg by mouth twice a day) and trazodone (50 mg by mouth at bedtime) for anxiety and sleep, respectively.
Not surprisingly, he was exceptionally worried about his diagnosis and prognosis; this prevented him from resting comfortably and falling asleep at bedtime. Despite reassurance that his medical workup and assessment was proceeding smoothly, he remained highly anxious. The medical team ordered several sedating agents (ie, melatonin [2 mg by mouth at bedtime] and diphenhydramine [50 mg by mouth at bedtime]), and they continued his lorazepam and increased his trazodone (to 100 mg by mouth at bedtime).
WHAT IS INSOMNIA?
Insomnia is an acute or chronic condition characterized by difficulty in falling asleep, staying asleep, and awakening too early and/or by having sleep of poor quality or nonrestorative sleep.1 Symptoms of acute insomnia last for less than 3 months and are usually precipitated by a life stressor or event. Insomnia is considered chronic when symptoms persist for longer than 3 months.1 To meet the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria for insomnia disorder, symptoms must cause clinically significant distress or functional impairment, occur for at least 3 nights a week for at least 3 months, and not be better explained by a medical or psychiatric disorder or be linked to another sleep disorder (eg, sleep apnea and narcolepsy).1
The 4-factor model of insomnia2 adds the role of hyperarousal/conditioned responses to the behavioral model of insomnia,3 which is a 3-factor diathesis-stress model that highlights the interplay of predisposing (eg, biological, psychological, social, and genetic factors that predispose to worry or rumination), precipitating (eg, new-onset medical/psychiatric illness or injury, environmental disruptions, or circadian rhythm changes), and perpetuating (eg, behavioral) factors in the development and maintenance of chronic insomnia.3,4
HOW COMMON IS INSOMNIA IN THE GENERAL POPULATION?
Insomnia occurs in up to two-thirds of adults.5 Insomnia attributed to a medical (eg, chronic pain, chronic obstructive pulmonary disorder [COPD]) or psychiatric disorder (eg, MDD, anxiety) or to use of medications (eg, substance use disorder [SUD]) is common.6–11 Moreover, insomnia is more common among women and older individuals12–16; in those with less education and income; in those who are separated, divorced, or widowed17,18; and in those with psychiatric disorders (eg, MDD, GAD, and SUDs)19–21 or medical conditions (including cancer, chronic pain, heart disease, and diabetes).22 Maladaptive behaviors (eg, spending too much time in bed, having irregular sleep-wake schedules, napping frequently, and engaging in non–sleep-related activities in the bedroom) can also perpetuate insomnia.23–26
HOW CAN INSOMNIA BE MANAGED WITHOUT MEDICATION?
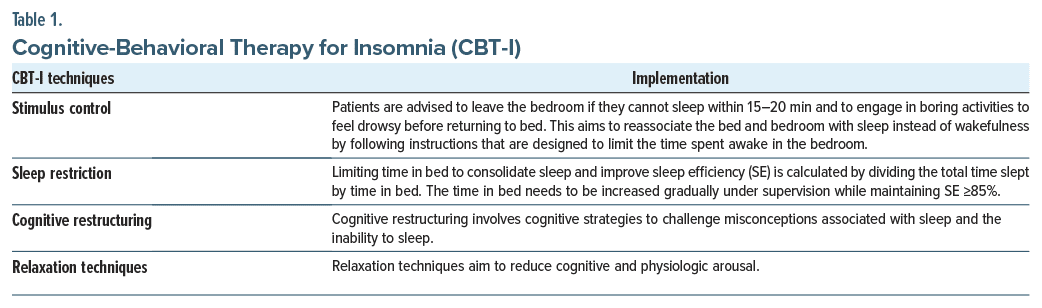
Cognitive-behavioral therapy for insomnia (CBT-I) is recommended as a first-line treatment for insomnia by multiple professional organizations (eg, the American College of Physicians, the National Cancer Institute, and the National Comprehensive Cancer Network).27–29 CBT-I reduces acute insomnia to an extent that is comparable to hypnotic medications; however, over the long term, CBT-I outperforms medications regarding relief from insomnia.30 CBT-I is thought to work via the principles of classical and operant conditioning, a form of learning in which certain behaviors (eg, getting into bed) and stimuli (eg, seeing one’s bed) are paired with a physical sensation of sleepiness, whereas behaviors and stimuli associated with wakefulness are systematically reduced. It consists of 4 key components: stimulus control, sleep restriction, cognitive restructuring, and relaxation techniques (Table 1). Stimulus control therapy trains patients to reassociate the bed and bedroom with sleep instead of wakefulness by following instructions that are designed to limit the time spent awake in the bedroom. Sleep restriction therapy improves sleep quality and continuity by establishing a fixed bedtime and awakening time and by limiting time in bed (as documented by the creation of daily sleep logs); in practice, this technique does not involve “restricting” sleep but rather restricting time in bed. Relaxation training encompasses a variety of clinical procedures aimed at reducing bodily tension that interferes with sleep; it includes a combination of progressive muscle relaxation, diaphragmatic breathing, autogenic training, and meditation/imagery training. This type of training is often most suitable for patients whose insomnia is driven by an inability to relax (eg, manifest by a racing heart or thoughts) at bedtime or those who have multiple somatic complaints. Cognitive therapy involves myriad psychological methods aimed at challenging and changing misconceptions about insomnia, sleep, and the patient’s perceived consequences of impaired sleep. This type of intervention is most suitable for patients who experience intrusive thoughts or worries or who are preoccupied with the potential consequences of their insomnia.
CBT-I is typically delivered in 4–10 sessions (synchronously or asynchronously31–33); it has been efficacious across a variety of modalities (to individuals and groups; in-person and remotely via telehealth, website, and apps). Ultimately, the modality needs to match patients’ preferences, in part facilitated by knowledge of perceived or logistical barriers noted at the outset of treatment.26,34 In addition, patients undergoing CBT-I are often asked to complete daily sleep diaries or sleep logs to evaluate their progress and adjust their “sleep prescriptions” (ie, time into and out of bed) to maximize their sleep efficiency (SE). CBT-I has been efficacious across populations (including adolescents, adults, and those facing comorbid physical and psychiatric illnesses).26,32–42
HOW COMMON IS INSOMNIA AMONG GENERAL HOSPITAL INPATIENTS?
According to a community hospital–based prospective observational study of insomnia (excluding those with a history of insomnia), new-onset insomnia occurred in roughly one-third (36%) of hospitalized patients.43 The most common causes of dysregulated sleep were staff disruptions and symptoms of medical conditions. Typically, such insomnia was brief, and it tended to reduce patients’ satisfaction scores. A longitudinal observational study of hospitalized older adults (ie, aged 65 years and older) found a similar rate of insomnia.44
WHY SHOULD INSOMNIA BE TREATED IN THE HOSPITAL?
Since insomnia often leads to adverse effects on emotional, cognitive, and physical health45 and can impair recovery, extend one’s length of stay, reduce perceptions of wellness, and decrease patient satisfaction regarding care, it should be treated. Moreover, sleep deprivation leads to endothelial dysfunction, oxidative stress, progression of atherosclerosis, inflammation, autonomic dysfunction, hypothalamic-pituitary-adrenal axis disruption, insulin resistance/metabolic effects, and mood and cognitive changes.45 Poor sleep also increases the likelihood of developing delirium (ie, “acute brain failure” or “encephalopathy”), a neuropsychiatric condition that can increase morbidity, hospital length of stay, health care costs, and mortality.46
HOW CAN INSOMNIA BE ASSESSED AND MANAGED IN GENERAL HOSPITAL SETTINGS?
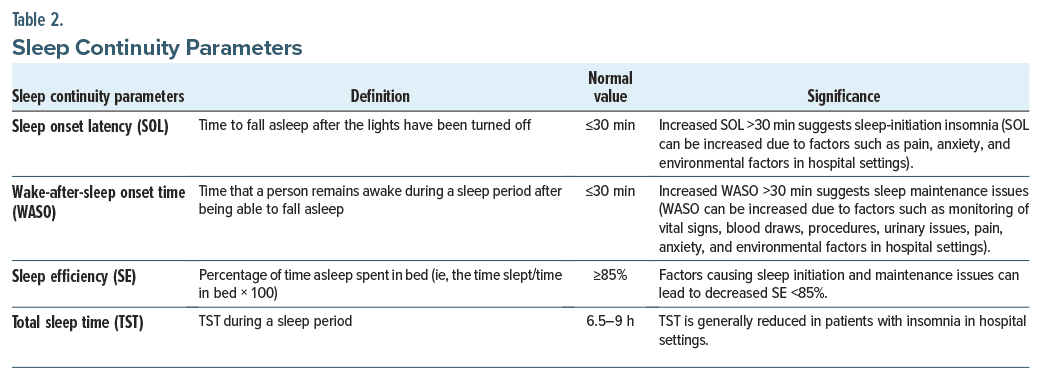
Assessment of insomnia in the hospital setting should involve a multi-modal approach that includes taking a thorough sleep history, evaluating comorbid conditions and medications, and considering environmental factors that may interfere with sleep. A comprehensive sleep history assesses sleep continuity parameters (such as sleep onset latency [SOL], wake-after-sleep onset time [WASO], SE, and total sleep time [TST]) as shown in Table 2.
The duration, nature, and severity of insomnia should be established, including the sleep patterns experienced by the patient prior to admission, to identify the worsening of preexisting insomnia or new-onset insomnia in the setting of a hospitalization.47 Preexisting sleep disorders are thought to occur in nearly one-fourth (22.5%) of hospitalized patients.48 New-onset insomnia has been reported in roughly one-third (36%) of medically admitted individuals, using the Insomnia Severity Index (ISI).43 Difficulty maintaining sleep was most often reported, and insomnia lasted for <2 weeks in most of the patients during the follow-up period, suggesting that it can be called short-term insomnia or adjustment insomnia (ie, insomnia that resolves when the stressor has been removed or when the individual adapts to the stressor).43 The consequences of insomnia (including fatigue, irritability, and cognitive changes) should be determined. Moreover, poor sleep among inpatients has been associated with more medical complications, disability, and short and long-term functional impairments and less health care satisfaction in medical and psychiatric inpatients.49
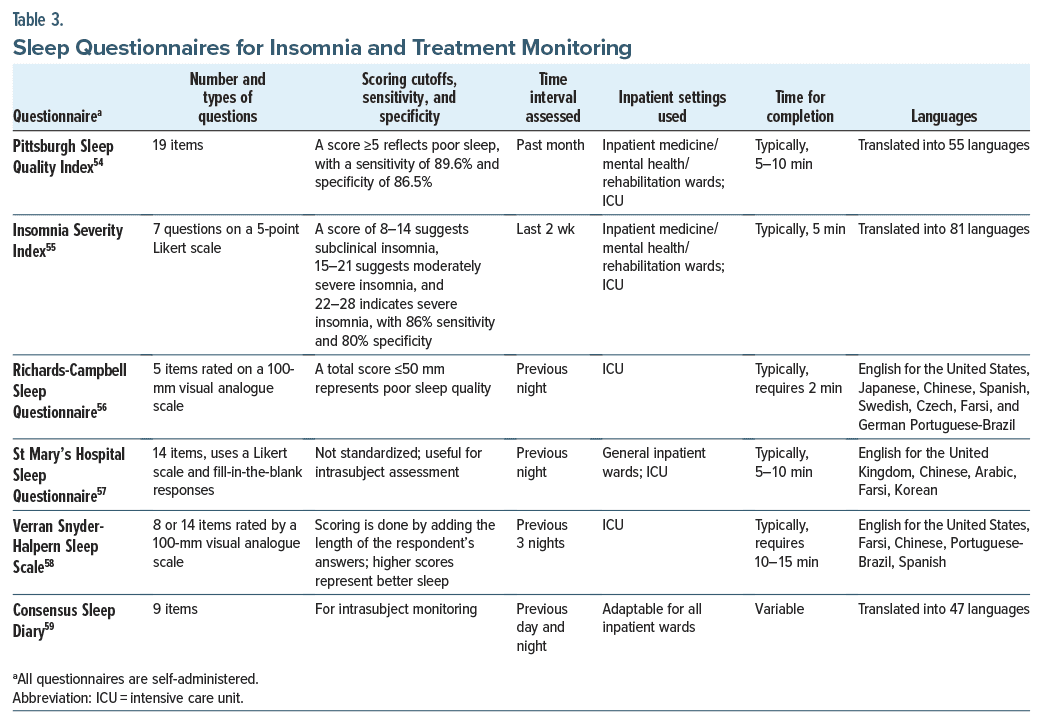
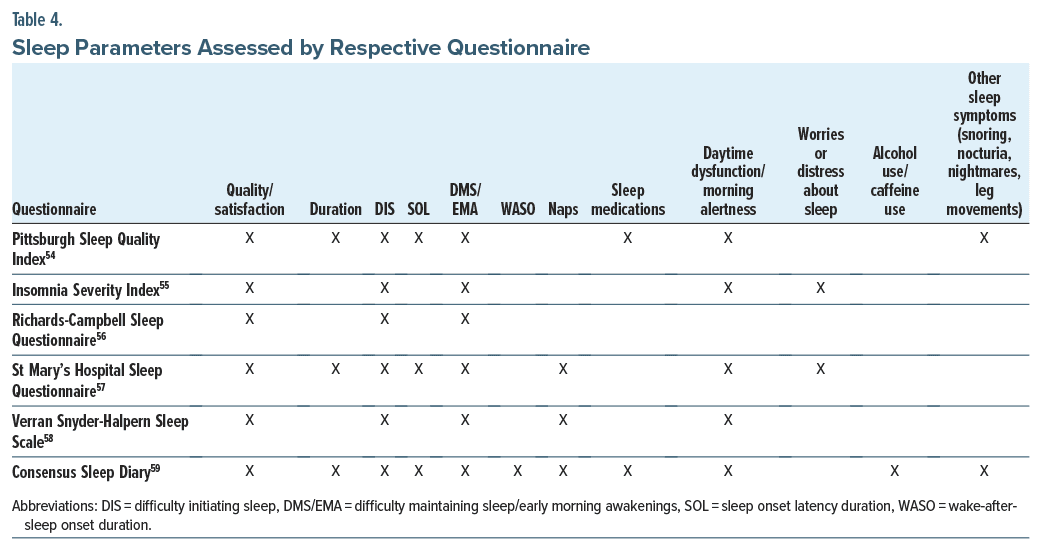
While there are a multitude of tools to assess sleep disturbances and insomnia, standardized instruments and methods for use in general hospitals are lacking.50 Most hospitals attempt to monitor sleep; however, the implementation of sleep monitoring is inconsistent.51 Assessment of insomnia in the general hospital should incorporate bedtime, SOL, WASO, SE, TST during the night, wake time, daytime sleep time, and subjective sleep quality.51–53 These may be assessed by taking a sleep history or by using validated tools, such as the Pittsburgh Sleep Quality Index (PSQI),54 ISI,55 Richards-Campbell Sleep Questionnaire (RCSQ),56 St Mary’s Hospital Sleep Questionnaire,57 and Verran Snyder-Halpern Sleep Scale,58 as well as sleep diaries (eg, the Consensus Sleep Diary).59 The most widely used questionnaires for insomnia and treatment monitoring are the PSQI, ISI, and RCSQ (Table 3). The parameters assessed by the above questionnaires are described in Table 4.
Differential Diagnosis
Sleep disorders that may mimic or accompany insomnia (eg, restless leg syndrome [RLS], circadian rhythm sleep-wake disorders, and sleep-related breathing disorders) should be assessed. RLS is characterized by an urge to move the legs while at rest, usually associated with leg discomfort, especially during the evening or at night. RLS is relieved transiently with movement; prolonged bed rest during hospitalization often worsens RLS symptoms, which can mimic sleep onset insomnia. RLS can be idiopathic or secondary (eg, associated with iron deficiency, renal failure, and psychotropic medications, except bupropion). Circadian rhythm sleep-wake disorders can also mimic insomnia with complaints of difficulty with sleep initiation or maintenance and excessive daytime sleepiness (EDS) due to misalignment of an individual’s internal circadian clock with the Earth’s near 24-hour light-dark cycle. For example, circadian rhythm sleep-wake disorder, delayed phase type, may mimic sleep-initiation insomnia, and advanced phase type may manifest as sleep-maintenance insomnia.
Sleep-related breathing disorders (eg, obstructive sleep apnea [OSA] and central sleep apnea [CSA]), should be evaluated in patients presenting with insomnia complaints. OSA is characterized by snoring and repetitive episodes of breathing pauses (apnea/hypopnea) associated with significant oxygen desaturations and sleep fragmentation. Comorbid insomnia and OSA are well-recognized, with 39%–58% of patients having OSA reporting insomnia, while 29%–67% of those with insomnia fulfill criteria for OSA.60 Those with OSA who have disturbed nocturnal sleep tend to have insomnia, and they use sedative-hypnotic medications frequently and continuous positive airway pressure (CPAP) therapy less often.60,61 CSA syndromes are a group of sleep-related breathing disorders that are characterized by recurrent cessations of airflow due to the absence of respiratory effort, which results in repetitive periods of insufficient ventilation and compromised gas exchange.62 Patients with CSA often experience sudden awakenings during sleep that are accompanied by shortness of breath, insomnia, and EDS, as well as by changes in cognition and mood. Primary or idiopathic CSA is rare; however, CSA syndromes associated with underlying conditions are more commonly observed in clinical settings. CSA occurs in almost half of patients with congestive heart failure, involving Cheyne-Stokes breathing.63 Roughly one-fourth of patients who take opioids chronically have CSA. Key risk factors for more severe CSA in this patient population include a morphine-equivalent daily dose or >200 mg and a low or normal body mass index.64
Several medical conditions (eg, cardiovascular disease, COPD, diabetes mellitus, gastroesophageal reflux disease, thyroid disorders, renal disease, and severe liver disease) can adversely affect sleep physiology and lead to sleep complaints.65 Symptoms related to medical conditions (such as cough, pruritus, pain, shortness of breath, and frequent urination) may also interfere with sleep.47 Alleviation of these symptoms with simple measures, such as administering a cough suppressant, administering an analgesic for pain relief, limiting fluid intake during the evening hours, and administering diuretics before the evening hours, can improve sleep.47 Insomnia can also be caused or exacerbated by using certain medications (including antidepressants, stimulants, corticosteroids anticholinergics, antiepileptics, β-blockers, and theophylline).65 Appropriate measures aimed at reconciling and avoiding medications that are likely to cause insomnia may improve sleep.
Several psychological and psychiatric factors contribute to insomnia in hospital settings. For example, anxiety that is related to current illnesses, anticipated procedures, unaddressed personal matters, and unfamiliar surroundings is common among hospitalized patients.47 In addition, hospitalized patients with chronic medical issues often suffer from coexisting psychiatric illnesses, such as MDD, that can contribute to sleep disturbances.66 The presence of manic or psychotic symptoms can cause agitation and interfere with sleep in hospitalized patients. Moreover, patients with history of SUDs often suffer from insomnia due to intoxication or withdrawal associated with substance use (eg, alcohol, tobacco, illicit drugs).67
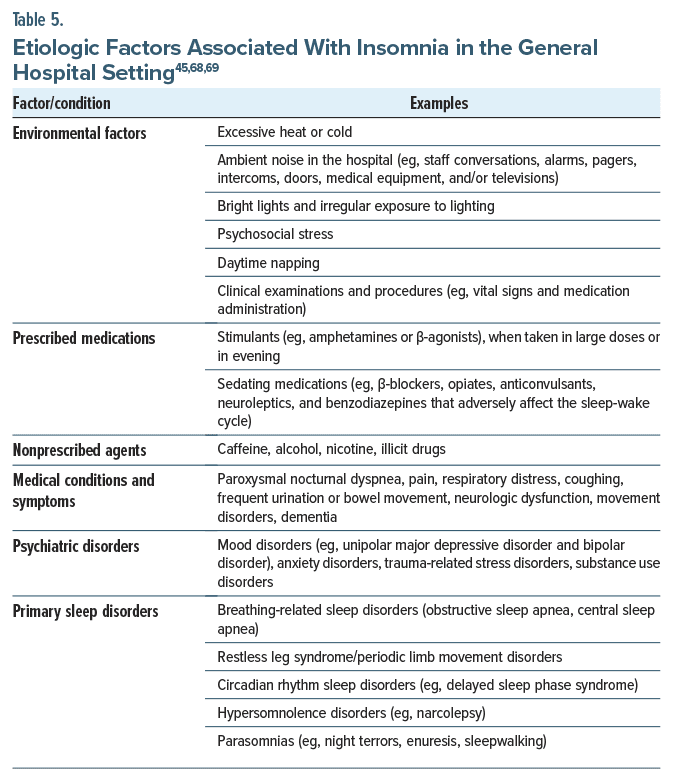
Environmental factors can also interfere with sleep. Hospital wards and intensive care units (ICUs) are usually noisy, and nocturnal assessments (eg, checking vital signs, drawing blood samples) can lead to middle-of-the night awakenings.47 Constant lighting also disrupts one’s sense of day and night.43 Environmental factors that intrude on sleep can be minimized in health care settings by ensuring that health care staff respond to alarms promptly, keeping patient doors closed, enforcing visiting hour restrictions, displaying “quiet” signs, providing eye masks or earplugs, and keeping drapes closed at night and open during the day. In addition, whenever possible, clinical care should be performed during the day, and assessments at night should be kept to a minimum.11 Table 5 summarizes the etiological factors associated with insomnia in general hospital settings.45,68,69
In summary, it is important to determine the source(s) of sleep disruption to develop an effective management plan for hospitalized patients. Factors that prolong SOL/WASO, presence of insomnia preadmission, anxiety concerns (such as worry about prognosis, procedure, pain, financial concerns, and the impact of illness on family/work), physical symptoms (such as nocturia, pain), medication side effects, and environmental factors contributing to insomnia should be identified to create an effective management plan for insomnia in hospitalized patients.
Medical Workup
The diagnosis of insomnia is based on subjective sleep complaints, and it requires no specific medical workup or investigation. However, specific screening tools and tests may facilitate diagnosis and treatment, especially if comorbid sleep, medical, and psychiatric conditions are present. For patients with symptoms of RLS, iron studies (eg, serum iron, iron binding capacity, transferrin saturation, and ferritin) should be considered. Iron supplementation (oral or intravenous [IV] iron) can treat RLS symptoms in the hospital setting, especially when transferrin saturation is <45%. Actigraphy devices are typically worn on the wrist. They use movement as a proxy for wakefulness and a relative lack of movement as a proxy for sleep. Depending on the specific device, useful sleep parameters (such as sleep latency, mid-sleep awakenings, sleep onset, and offset timing) and light exposure can be measured. When used serially for at least 7–14 days, actigraphy may facilitate objective assessment of insomnia treatment progress. It can also be helpful when assessing whether insomnia symptoms are due to a circadian rhythm disorder or to behavioral curtailment of sleep.70 A general limitation of actigraphy is that it tends to overestimate sleep time as compared to polysomnography. The cost of actigraphy varies with the device used, but it is less expensive than polysomnography (PSG). Previous use of actigraphy in the hospital setting has mostly focused on its utility in measuring sleep in ICUs. The accuracy of the results has been conflicting, with some reporting moderate levels of accuracy when compared to PSG,71 while others report low agreement when compared to an electroencephalogram72 and with a PSG.73 Specific to its use for in-patient mental health populations, actigraphy has been used to measure sleep and its relationship with suicide among adolescents,74 how differences in room lighting affected sleep and mood on a cardiology ward,75 and delayed circadian phase in patients with obsessive compulsive disorder.76
If sleep-disordered breathing is suspected, a high resolution pulse oximetry test is a valuable screening tool, while inpatient PSG may be considered, particularly in those with heart failure, acute stroke, COPD, or obesity hypoventilation syndrome.77 The logistics required to arrange for an in-patient to attend a PSG laboratory are often cumbersome. The unfamiliar environment of the laboratory itself may also disturb sleep. In addition, its cost may be prohibitive. Level 3 sleep studies (measuring saturation, airflow, snoring, and respiratory effort) and level 2 sleep studies (measuring the same parameters as an in-lab PSG that is unattended) are often more accessible for patients in general hospitals.
A urine drug screen is recommended if symptoms of substance use or withdrawal exist; prompt management of substance use–related symptoms may alleviate sleep complaints. If delirium is suspected, then a detailed workup should be done to rule out any potential medical causes and associated sleep complaints.
Management
Although nonpharmacologic interventions are first line treatments for insomnia, the short-term use of oral hypnotic agents may be necessary to treat insomnia in hospital settings.49 A 2023 systematic review of CBT-I delivered during inpatient psychiatric care identified challenges to feasibility, including characteristics of the admission ward and the need for individually tailored delivery (eg, not scheduling sleep restriction).78 Currently approved medication categories for insomnia include benzodiazepines/nonbenzodiazepine hypnotics, dual orexin receptor antagonists (DORAs), melatonin receptor agonists, and histamine (H1) receptor antagonists. The selection and dose of a hypnotic should be based on the patient’s age, use of concomitant medications, concomitant disease states, and pharmacokinetic and pharmacodynamic properties and side effect profiles of each agent to ensure its efficacy while minimizing the risk of adverse events.47 Hypnotics should be prescribed at the lowest effective dose for the shortest duration possible to address insomnia.
Benzodiazepines/Nonbenzodiazepine Hypnotics
Benzodiazepines and nonbenzodiazepine hypnotics are among the most prescribed medications for the treatment of insomnia in hospital settings.79 These medications act as positive allosteric modulators of γ-aminobutyric acid (GABA) type A receptors, and they facilitate inhibitory GABA receptor agonist transmission. The current US Food and Drug Administration (FDA)–approved benzodiazepines for the treatment of insomnia include triazolam and temazepam. Nonbenzodiazepine hypnotics that stimulate only a subset of benzodiazepine receptors (eg, the benzodiazepine α1 receptor) include zaleplon, zolpidem, and eszopiclone. The effects of benzodiazepines on sleep architecture include decreasing sleep latency, increasing stage 2 non–rapid eye movement (NREM) sleep, and decreasing stage 3 NREM sleep and REM sleep.47
Based on their half-life, benzodiazepines are often classified as short, intermediate, and long acting. Short acting benzodiazepines are more likely to cause rebound insomnia and withdrawal symptoms upon their discontinuation, whereas long-lasting benzodiazepines are more likely to cause residual daytime effects.47 Differences in their pharmacokinetic profiles can be used to clinical advantage in the treatment of insomnia, as those with sleep-onset difficulties or morning sedation from the use of hypnotics may benefit from use of a drug with a short half-life, and those with sleep maintenance difficulties may benefit from a longer-lasting agent. Triazolam (0.25–0.5 mg), a short-acting benzodiazepine, is indicated for sleep-initiation insomnia, while temazepam (7.5–30 mg) is indicated for sleep-initiation and sleep maintenance insomnia complaints due to its longer half-life. Based on the half-life of nonbenzodiazepine hypnotics, zaleplon (10–20 mg) is indicated for use in sleep-initiation insomnia; zolpidem (5–10 mg) and eszopiclone (1–3 mg) are indicated for sleep-initiation and sleep-maintenance insomnia complaints. Nonbenzodiazepine hypnotics have been shown to be efficacious for up to 6 months of nightly or intermittent use in double-blind placebo-controlled studies.80,81
Common side effects include anterograde amnesia, respiratory depression, and impairment of cognitive and motor functions. Paradoxical effects (such as nightmares, hallucinations, bizarre behavior, and hostility and rage) are collectively referred to as “disinhibition” and have been reported with these medications.47 Benzodiazepines may be misused, and their long-term use can lead to dependence. The risk of abuse and dependence is especially severe for patients with an SUD. In older patients, long-term use of benzodiazepines has increased the risk of developing cognitive decline, dementia, and delirium.82,83 Given the increased risk of falls and hip fractures with benzodiazepine use,84 these medications should be avoided in individuals over the age of 65 years. Because of these side effects, use of benzodiazepines/ nonbenzodiazepine hypnotics should be limited to healthy, young (aged <45 years) individuals who are expected to have brief hospital stays.85
While benzodiazepines are commonly prescribed in general hospitals for sleep problems, the evidence for their effectiveness in improving sleep quality is inconclusive. These medications reduce the time it takes to fall asleep, but they do not significantly improve the duration or quality of sleep.79 One systematic review found that sedative-hypnotics are equally effective to each other and to placebo or to no treatment at all.86
Melatonin Agonists
Ramelteon is a melatonin receptor agonist (MT1 and MT2) with properties like those of endogenous melatonin.87 Ramelteon reduces sleep latency, but it does not improve sleep maintenance. Ramelteon is an FDA-approved medication for insomnia, and it is specifically indicated for sleep-initiation insomnia complaints. Doses of 8 mg/day are effective; higher doses provide no additional benefit. Ramelteon does not cause rebound insomnia, and it has not been associated with rebound insomnia, tolerance, or withdrawal symptoms.88 Melatonin, a widely used non–FDA approved sleep aid in outpatient settings, has been increasingly prescribed for the management of insomnia in hospital settings. This is likely due to increased recognition of the potential side effects of hypnotics and to low incidence of adverse effects and drug-drug interactions with melatonin.79 Side effects of melatonin are minor and include daytime sleepiness, headache, dizziness, vivid dreams, or mood changes. Based on data from randomized-controlled trials among inpatients, ramelteon and melatonin have been associated with improved sleep quality, a longer average night’s sleep, and fewer nighttime awakenings.89
Melatonin agonists may also have a role in managing delirium.90 A systematic review of 2 studies showed that doses of exogenous melatonin/ramelteon ranging from 0.5 mg to 5 mg helped reduce the incidence of delirium by 75% in comparison to a placebo in elderly patients.90 However, another systematic review found that while melatonin had no effect on delirium in medical inpatients, it decreased delirium in surgical and ICU patients.89 A recent large, multicenter ICU trial found no significant difference in delirium incidence between use of melatonin (4 mg) and placebo.91 Based on current evidence, it is unclear whether melatonin can prevent delirium. However, research suggests that it does not increase the risk more than a placebo, unlikebenzodiazepines. Additionally, studies indicate that ramelteon may be more effective in preventing delirium than melatonin due to its stronger binding affinity with MT1 and MT2 receptors.92
Dual Orexin Receptor Antagonists
The neuropeptide orexin/hypocretin plays an important role in the stabilization and maintenance of wakefulness by reinforcing wake-promoting signaling in the brain via orexin/hypocretin receptors (OX1R and OX2R).93 DORAs, including suvorexant (10–20 mg), lemborexant (5–10 mg), and daridorexant (25–50 mg), have been FDA approved for the treatment of insomnia. DORAs are thought to diminish the wakefulness drive, thus allowing sleep to occur. Their common side effects include somnolence, abnormal dreams, fatigue, and dry mouth; these medications are contraindicated in patients with narcolepsy, a condition characterized by the deficiency of orexin/hypocretin. DORAs may have some abuse potential, and these currently are US Drug Enforcement Administration schedule IV medications.
DORAs are not associated with rebound insomnia, tolerance, or withdrawal symptoms, and they are deemed safer in patients with comorbid OSA and respiratory compromise.94 In addition, DORAs have shown efficacy and safety in elderly patients with insomnia.95 Lemborexant quickly binds to human OXRs, and a network meta-analysis found that patients who took lemborexant improved sleep initiation and nighttime sleep maintenance more than those who took suvorexant.96 Relative differences in receptor-binding and pharmacokinetic properties between lemborexant and suvorexant may explain their differences in clinical efficacy and safety. Based on these findings, 5 mg of lemborexant may be considered as the most suitable first line drug and may be followed by the administration of 10 mg of lemborexant or suvorexant.96
The potential role of DORAs has been examined in the prevention of delirium in ICU settings. In a meta-analysis, comprising 7 studies with 402 patients receiving suvorexant treatment and 487 patients receiving a control treatment, the incidence of delirium was reduced (OR =0.30, P<.001) and time to delirium onset was lengthened (SMD =0.44, P =.006) in patients undergoing suvorexant treatment compared with controls. Suvorexant had no beneficial effects on the secondary outcomes, time on ventilation, drug-related adverse events, or mortality.97 The efficacy of DORAs has yet to be systematically assessed in hospitalized patients with insomnia, and these agents may not yet be present on hospital formularies, as they are relatively new and costly.93
H1 Receptor Blockers
Doxepin, a tricyclic antidepressant with selective affinity for the H1 receptor at low doses, is FDA approved for insomnia at doses of 3–6 mg daily. Low dose doxepin has been shown to reduce WASO and increase SE and TST with little effect on sleep latency in clinical trials.98 Doxepin improves WASO and SE across the entire night as compared to short half-life nonbenzodiazepine hypnotics that have a limited effect in the final third of the night, thus making it ideal treatment of sleep-maintenance insomnia complaints. Common side effects include drowsiness, fatigue, nausea, and flu-like symptoms. Ultra–low-dose doxepin (1–3 mg) has also been found to treat insomnia in older adults with no evidence of next-day residual sedation or other significant adverse effects.99 Low-dose doxepin has not been studied for the treatment of insomnia in hospitalized patients, and it also may not be widely available on hospital formularies.
Other Medications
Medications, such as antihistamines (eg, diphenhydramine), antidepressants (eg, mirtazapine, trazodone), and atypical antipsychotics (eg, quetiapine), are used as off-label sleep aids in hospitalized patients.79 None of these medications are FDA approved for the treatment of insomnia. Antihistamines with anticholinergic activity can cause confusion and should be avoided in older adults.100 Mirtazapine, at low doses (7.5–15 mg), has sedative effects and appetite-stimulating properties. This makes it potentially useful for patients with cancer or AIDS who suffer from insomnia, depression, and anorexia.85 Trazodone (25–100 mg) may be useful in patients with a history of substance abuse, but it can cause gastrointestinal side effects, orthostatic hypotension, and cardiac arrhythmias.47 Atypical antipsychotics may be indicated for the management of sleep disturbance associated with mania, psychosis, or severe agitation. In older adults with dementia, atypical antipsychotics have been associated with an increased risk of stroke and death.101,102 In a retrospective study comparing the risk of harm with trazodone or atypical antipsychotic use in older adults with dementia, trazodone was not a safer alternative to atypical antipsychotics, as it had a similar risk of falls and fractures among older adults with dementia.103
Comparative Efficacy and Safety of Pharmaceutical Agents for Insomnia in Hospital Settings
A systematic review revealed that there is insufficient evidence to suggest that pharmacotherapy can improve the quality or quantity of sleep for hospitalized patients who suffer from poor sleep.86 Even when compared to placebo or no treatment, no drug class or specific drug was identified as superior. Although 15 studies were included in the review, the quality of evidence was limited by their size and quality. Therefore, larger, better-designed trials involving hospitalized adults are necessary to ascertain the efficacy and safety of medications for insomnia.86
In another study,104 falls occurred in 2,427 (1.1%) out of 225,498 hospitalizations (median age of 57 years; 57.9% female). The study reported that 84,911 patients (37.7%) were exposed to at least 1 of the 5 medication classes (ie, benzodiazepines, diphenhydramine, trazodone, nonbenzodiazepine hypnotics, and atypical antipsychotics) of interest and concluded that there was a correlation between each of the sedating medications examined and in hospital falls, with benzodiazepines, nonbenzodiazepine hypnotics, and atypical antipsychotics having the strongest associations.104
WHICH SIDE EFFECTS ARE ASSOCIATED WITH THE USE OF SEDATIVE-HYPNOTIC AGENTS?
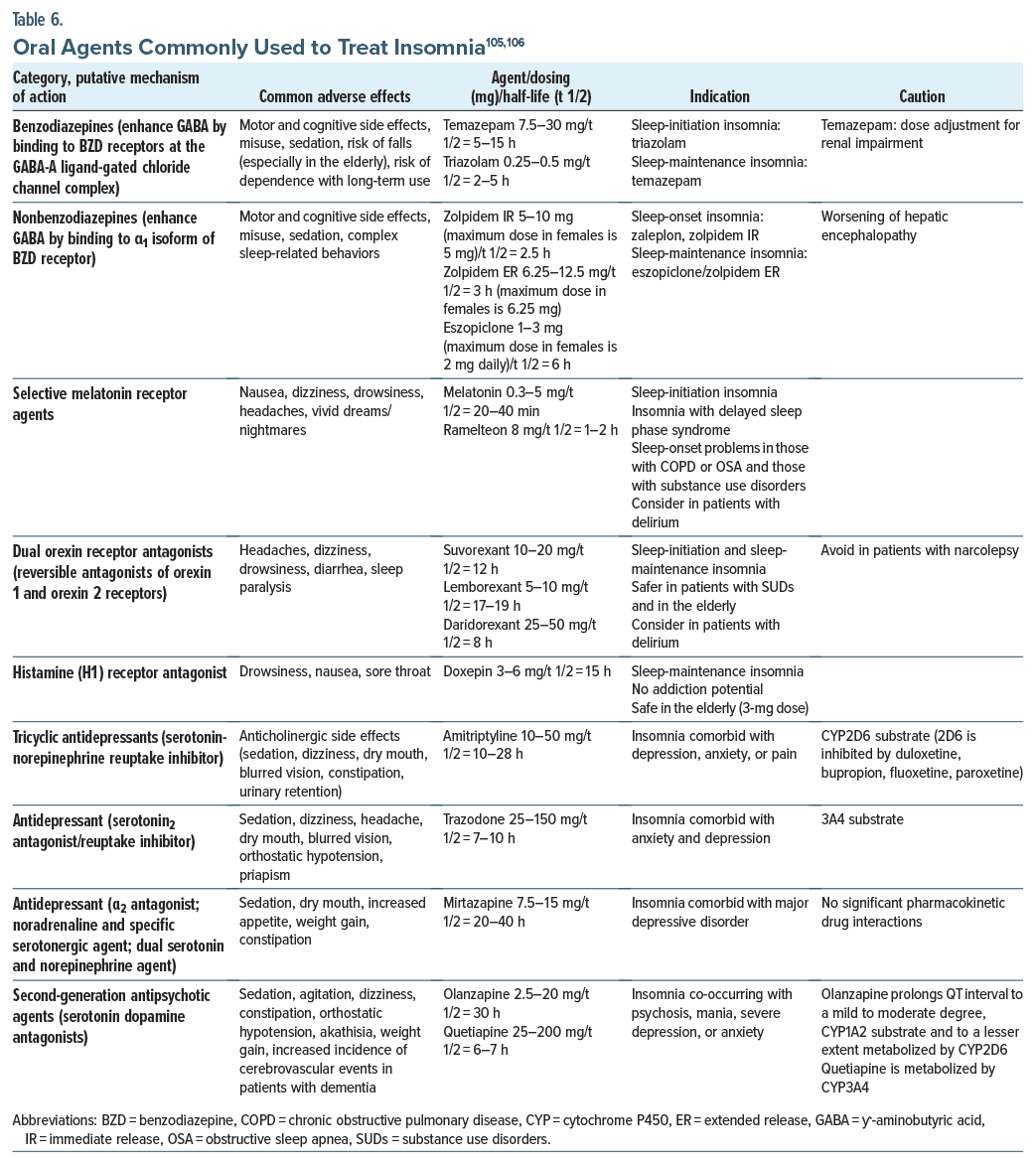
Table 6 summarizes the list of oral agents commonly used to treat insomnia and common associated side effects.105,106
HOW LONG SHOULD PHARMACOLOGIC INTERVENTIONS FOR INSOMNIA BE CONTINUED?
Most patients treated for insomnia during hospitalization do not require continued therapy after discharge.47 Moreover, most hospitalized patients who received a medication for sleep had no history of insomnia and did not use pharmacologic sleep aids (68.5%), and roughly one-third (34.4%) were discharged with a new prescription.107 New benzodiazepine prescriptions lead to ongoing use in some patients.108 After prolonged use, attempts to wean these medications can cause withdrawal symptoms, such as insomnia, anxiety, and tremors.109 For patients who need a hypnotic after discharge, short-term prescription (2 weeks) of the lowest effective dose should be provided.110 Patients should be educated about nonpharmacologic techniques for the management of insomnia, and daily use of hypnotic medications should be discouraged. Patients should also be informed about potential adverse effects and advised to avoid alcohol, as it is associated with sleep maintenance difficulties, particularly during the second half of the night. If alcohol is consumed, the hypnotic dose should be skipped. The hypnotic should be taken approximately 30 minutes before bedtime to reduce the risk of confusion and falls.111 After 2–4 weeks, the patient should be reevaluated to determine if continued treatment is necessary. For patients with ongoing sleep complaints after hospital discharge, follow-up with a primary care provider and referral to a sleep medicine provider for evaluation and treatment of insomnia and comorbid sleep disorders is recommended.
WHAT HAPPENED TO MR A?
Although administration of sedating agents helped him achieve some sleep that night, Mr A was drowsy, relatively hypotensive (110/70 mm Hg), and confused the next morning on rounds. As a result, a psychiatric consultation was requested. While taking Mr A’s history, the consultant identified that Mr A was a loud snorer and determined that he also suffered from OSA. The consultant made several interventions, including discontinuation of diphenhydramine and trazodone (as precipitants for hypotension and confusion), addition of quetiapine (25 mg by mouth at bedtime), and use of a CPAP mask, and he also guided Mr A through progressive muscle relaxation exercises and willful dissociation with mental imagery to promote relaxation.
Mr A was not diagnosed with a myocardial infarction. His hypoactive delirium resolved quickly as the highly anticholinergic agent diphenhydramine and hypotension-inducing agent trazodone were discontinued. Quetiapine was maintained for 1 more day and discontinued before his hospital discharge. Mr A was provided education about sleep hygiene and referral information for accessing CBT-I if insomnia symptoms return and persist.
CONCLUSION
Insomnia is an acute or chronic condition characterized by difficulty falling asleep, staying asleep, and awakening too early and/or by having sleep of poor quality, which is common among inpatients and outpatients. Although the etiology of insomnia is often multifactorial, both nonpharmacologic (eg, CBT-I and reassurance) and a variety of pharmacologic approaches (eg, use of benzodiazepines, antihistamines, melatonin agonists, antipsychotics) can provide rapid relief; unfortunately, each is associated with drug-drug interactions and potentially problematic side effects that may interfere with the management of myriad medical conditions. Moreover, chronic use of benzodiazepines has been linked with problems of drug dependence and abuse. Therefore, a thoughtful risk-benefit analysis should accompany efforts to resolve acute and chronic insomnia (which may involve time-limited use of sedating agents).
Article Information
Published Online: January 21, 2025. https://doi.org/10.4088/PCC.24f03793
© 2025 Physicians Postgraduate Press, Inc.
Submitted: June 21, 2024; accepted October 1, 2024.
To Cite: Chopra A, Rustad JK, Hall DL, et al. Management of insomnia in the general hospital. Prim Care Companion CNS Disord. 2025;27(1):24f03793.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts (Chopra, Hall, Stern); Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire (Rustad); White River Junction VA Medical Center, White River Junction, Vermont (Rustad); Burlington Lakeside VA Community Based Outpatient Clinic, Burlington, Vermont (Rustad); Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario (Mak); Centre for Addiction and Mental Health, Toronto, Ontario (Mak).
Corresponding Author: Amit Chopra, MBBS, Massachusetts General Hospital, Harvard Medical School, 55 Fruit St, Boston, MA 02114 ([email protected]).
Relevant Financial Relationships: Dr Chopra has received royalties from Oxford University Press for editing a textbook in Psychiatry. Dr Rustad is employed by the US Department of Veterans Affairs, but the opinions expressed in this article do not reflect those of the Department of Veterans Affairs. Dr Hall has received consulting fees from Goodpath. Dr Mak received unrestricted education grants from Paladin Labs, Jazz Pharmaceuticals and Eisai; consulting fees from Eisai, Idorsia, and Jazz
Pharmaceuticals; and speaker’s honoraria from Eisai and Jazz Pharmaceuticals. Dr Stern has received royalties from Elsevier for editing textbooks on psychiatry.
Funding/Support: None.
Clinical Points
- Insomnia (an acute or chronic condition that is common among both inpatients and outpatients) is characterized by difficulty falling asleep, staying asleep, and awakening too early; fortunately, a variety of nonpharmacologic and pharmacologic interventions can provide immediate and lasting relief.
- Cognitive-behavioral therapy for insomnia is a first-line nonpharmacologic treatment that has been recommended by multiple professional organizations; it trains patients to reassociate the bed (and bedroom) with sleep instead of wakefulness by following instructions that are designed to limit time spent awake in the bedroom.
- Pharmacologic treatments (eg, use of benzodiazepines, antihistamines, melatonin agonists, and antipsychotics) encompass myriad mechanisms of action; however, clinicians should be mindful of their side effect profiles (eg, propensity to induce respiratory depression, hypotension, and delirium) and synergistic effects as well as the need for dose adjustments in the context of renal or hepatic impairment.
References (111)

- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Perlis ML, Jungquist C, Smith MT, et al. Cognitive Behavioral Treatment of Insomnia: A Session-By-Session Guide. Vol. 1. Springer Science & Business Media; 2005.
- Spielman AJ, Saskin P, Thorpy MJ. Treatment of chronic insomnia by restriction of time in bed. Sleep. 1987;10(1):45–56. PubMed
- Bootzin RR. Stimulus control treatment for insomnia. Proc Am Psychol Assn. 1972;7:395–396.
- Chung K-F, Yeung W-F, Ho FY-Y, et al. Cross-cultural and comparative epidemiology of insomnia: the Diagnostic and statistical manual (DSM),International classification of diseases (ICD) and International classification of sleep disorders (ICSD). Sleep Med. 2015;16(4):477–482. PubMed CrossRef
- Bahouq H, Allali F, Rkain H, et al. Prevalence and severity of insomnia in chronic low back pain patients. Rheum Int. 2013;33(5):1277–1281. PubMed CrossRef
- Budhiraja R, Parthasarathy S, Budhiraja P, et al. Insomnia in patients with COPD. Sleep. 2012;35(3):369–375. CrossRef
- Desai K, Mao JJ, Su I, et al. Prevalence and risk factors for insomnia among breast cancer patients on aromatase inhibitors. Support Care Cancer. 2013;21(1):43–51. PubMed CrossRef
- Bélanger L, Morin CM, Langlois F, et al. Insomnia and generalized anxiety disorder: effects of cognitive behavior therapy for gad on insomnia symptoms. J Anxiety Disord. 2004;18(4):561–571.
- Sunderajan P, Gaynes BN, Wisniewski SR, et al. Insomnia in patients with depression: a STAR*D report. CNS Spectr. 2010;15(6):394–404. CrossRef
- Flaherty JH. Insomnia among hospitalized older persons. Clin Geriatr Med. 2008;24(1):51–67, vi. PubMed CrossRef
- Jaussent I, Dauvilliers Y, Ancelin M-L, et al. Insomnia symptoms in older adults: associated factors and gender differences. Am J Geriatr Psychiatry. 2011;19(1):88–97. CrossRef
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 suppl):S7–S10. PubMed
- Johnson EO, Roth T, Schultz L, et al. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117(2):e247–e256. CrossRef
- Suh S, Cho N, Zhang J. Sex differences in insomnia: from epidemiology and etiology to intervention. Curr Psychiatry Rep. 2018;20(9):69. PubMed CrossRef
- Patel D, Steinberg J, Patel P. Insomnia in the elderly: a review. J Clin Sleep Med. 2018;14(6):1017–1024. CrossRef
- Gellis LA, Lichstein KL, Scarinci IC, et al. Socioeconomic status and insomnia. J Abnorm Psychol. 2005;114(1):111–118. CrossRef
- Sutton DA, Moldofsky H, Badley EM. Insomnia and health problems in Canadians. Sleep. 2001;24(6):665–670. PubMed CrossRef
- Brower KJ. Assessment and treatment of insomnia in adult patients with alcohol use disorders. Alcohol. 2015;49(4):417–427. PubMed CrossRef
- Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–481. PubMed CrossRef
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. PubMed CrossRef
- Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Fam Med Prim Care. 2016;5(4):780–784. PubMed CrossRef
- Induru RR, Walsh D. Cancer-related insomnia. Am J Hosp Palliat Care. 2014;31(7):777–785. CrossRef
- Jungquist CR, Tra Y, Smith MT, et al. The durability of cognitive behavioral therapy for insomnia in patients with chronic pain. Sleep Disord. 2012;2012:679648. PubMed CrossRef
- Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19(3):895–908. CrossRef
- Hall DL, Arditte Hall KA, Gorman MJ, et al. The Survivorship Sleep Program (SSP): a synchronous, virtual cognitive behavioral therapy for insomnia pilot program among cancer survivors. Cancer. 2022;128:1532–1544. PubMed CrossRef
- Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. PubMed CrossRef
- National Cancer Institute. Follow-Up Medical Care. 2021. Accessed February 26, 2021. https://www.cancer.gov/about-cancer/coping/survivorship/follow-up-care
- National Comprehensive Cancer Network. Survivorship Care for Cancer Related Late and Long-Term Effects. 2020. Accessed February 26, 2021. https://www.nccn.org/patients/guidelines/content/PDF/survivorship-crl-patient.pdf
- Morin CM, Vallières A, Guay B, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009;301(19):2005–2015. PubMed CrossRef
- Laurel Franklin C, Walton JL, Raines AM, et al. Pilot study comparing telephone to in-person delivery of cognitive-behavioural therapy for trauma-related insomnia for rural veterans. J Telemed Telecare. 2018;24(9):629–635. PubMed CrossRef
- Gehrman P, Barilla H, Medvedeva E, et al. Randomized trial of telehealth delivery of cognitive-behavioral treatment for insomnia vs. in-person treatment in veterans with PTSD. J Affective Disord Rep. 2020;1:100018. CrossRef
- Holmqvist M, Vincent N, Walsh K. Web-vs telehealth-based delivery of cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep Med. 2014;15(2):187–195. PubMed CrossRef
- Cvengros JA. One size does not fit all: matching patients with insomnia treatment modality. Sleep Med. 2014;15(2):161–162. CrossRef
- Geiger-Brown JM, Rogers VE, Liu W, et al. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. 2015;23:54–67. PubMed CrossRef
- Zachariae R, Lyby MS, Ritterband LM, et al. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–a systematic review and meta analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10. PubMed CrossRef
- Ho FY-Y, Chung K-F, Yeung W-F, et al. Self-help cognitive-behavioral therapy for insomnia: a meta-analysis of randomized controlled trials. Sleep Med Rev. 2015;19:17–28. PubMed CrossRef
- Johnson JA, Rash JA, Campbell TS, et al. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med Rev. 2016;27:20–28. PubMed CrossRef
- Luo C, Sanger N, Singhal N, et al. A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: a systematic review and meta-analysis. EClinMed. 2020;24:100442. PubMed CrossRef
- Ma Y, Hall DL, Ngo LH, et al. Efficacy of cognitive behavioral therapy for insomnia in breast cancer: a meta-analysis. Sleep Med Rev. 2021;55:101376. PubMed CrossRef
- Morin CM, Beaulieu-Bonneau S. Cognitive-behavioral approach to treating insomnia. Rev Pract. 2017;67(8):862–867.
- van Straten A, van der Zweerde T, Kleiboer A, et al. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3–16. CrossRef
- Ho A, Raja B, Waldhorn R, et al. New onset of insomnia in hospitalized patients in general medical wards: incidence, causes, and resolution rate. J Community Hosp Intern Med Perspect. 2017;7(5):309–313. PubMed CrossRef
- Isaia G, Corsinovi L, Bo M, et al. Insomnia among hospitalized elderly patients: prevalence, clinical characteristics, and risk factors. Arch Gerontol Geriatr. 2011;52(2):133–137. PubMed CrossRef
- Morse AM, Bender E. Sleep in hospitalized patients. Clocks Sleep. 2019;1(1):151–165. CrossRef
- Stern TA, Celano CM, Gross AF, et al. The assessment and management of agitation and delirium in the general hospital. Prim Care Companion J Clin Psychiatry. 2010;12(1):PCC.09r00938. PubMed CrossRef
- Lenhart SE, Buysse DJ. Treatment of insomnia in hospitalized patients. Ann Pharmacother. 2001;35(11):1449–1457. CrossRef
- Dobing S, Frolova N, McAlister F, et al. Sleep quality and factors influencing self reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6):e0156735. PubMed CrossRef
- Miller MA, Renn BN, Chu F, et al. Sleepless in the hospital: a systematic review of non-pharmacological sleep interventions. Gen Hosp Psychiatry. 2019;59:58–66. PubMed CrossRef
- Ye L, Keane K, Johnson SH, et al. How do clinicians assess, communicate about, and manage patient sleep in the hospital? Nurs Admin. 2013;43(6):342–347. CrossRef
- Morse AM, Bender E. Sleep in hospitalized patients. Clocks Sleep. 2019;1(1):151–165. CrossRef
- Shahid A, Wilkinson K, Shai M, et al, eds. STOP, THAT and One Hundred Other Sleep Scales. 1st ed. Springer New York; 2012.
- Burger P, Van den Ende ES, Lukman W, et al. Sleep in hospitalized pediatric and adult patients - a systematic review and meta-analysis. Sleep Med X. 2022;4:100059.
- Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. PubMed CrossRef
- Morin CM, Belleville G, Bélanger L, et al. The Insomnia Severity Index:psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. PubMed CrossRef
- Richards KC, O’Sullivan PS, Phillips RL. Richards-Campbell Sleep Questionnaire (RCSQ) [Database Record]. APA PsycTests; 2000. https://doi.org/10.1037/t66848-000
- Ellis BW, Johns MW, Lancaster R, et al. The St. Mary’s Hospital Sleep Questionnaire: a study of reliability. Sleep. 1981;4(1):93–97. PubMed CrossRef
- Shahid A, Wilkinson K, Marcu S, et al, eds. Verran and Snyder-Halpern sleep scale (VSH). In: STOP, THAT and One Hundred Other Sleep Scales. Springer; 2011. https://doi.org/10.1007/978-1-4419-9893-4_99
- Carney CE, Buysse DJ, Ancoli-Israel S, et al. The Consensus Sleep Diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. PubMed CrossRef
- Luyster FS, Buysse DJ, Strollo PJ Jr. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. PubMed
- Ye L, Pien GW, Ratcliffe SJ, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014;44(6):1600–1607. PubMed CrossRef
- Eckert DJ, Jordan AS, Merchia P, et al. Central sleep apnea: pathophysiology and treatment. Chest. 2007;131(2):595–607. PubMed
- Costanzo MR. Central sleep apnea in patients with heart failure-how to screen, how to treat. Curr Heart Fail Rep. 2020;17(5):277–287. PubMed CrossRef
- Correa D, Farney RJ, Chung F, et al. Chronic opioid use and central sleep apnea: a review of the prevalence, mechanisms, and perioperative considerations. Anesth Analg. 2015;120(6):1273–1285. PubMed CrossRef
- Young JS, Bourgeois JA, Hilty DM, et al. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482. PubMed CrossRef
- Hertenstein E, Trinca E, Wunderlin M, et al. Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2022;62:101597. CrossRef
- Brower KJ, Krentzman A, Robinson EAR. Persistent insomnia, abstinence, and moderate drinking in alcohol-dependent individuals. Am J Addict. 2011;20(5):435–440. PubMed CrossRef
- Park LT, Matthews JD, Maytal G, et al. Evaluation and treatment of poor sleep. Prim Care Companion J Clin Psychiatry. 2007;9(3):224–229.
- Koski RR. Treatment of insomnia in hospitalized patients. US Pharm. 2011;36(1):HS-12-HS-18. https://www.uspharmacist.com/article/treatment-of-insomnia-inhospitalized-patients
- Riemann D, Espie CA, Altena E, et al. The European Insomnia Guideline: an update on the diagnosis and treatment of insomnia 2023. J Sleep Res. 2023;32(6):e14035. PubMed CrossRef
- Delaney LJ, Litton E, Melehan KL, et al. The feasibility and reliability of actigraphy to monitor sleep in intensive care patients: an observational study. Crit Care. 2021;25(1):42. PubMed CrossRef
- Darbyshire JL, Borthwick M, Edmonds P, et al. Measuring sleep in the intensive care unit: electroencephalogram, actigraphy, or questionnaire?. J Intensive Care Soc. 2020;21(1):22–27. CrossRef
- Beecroft JM, Ward M, Younes M, et al. Sleep monitoring in the intensive care unit: comparison of nurse assessment, actigraphy and polysomnography. Int Care Med. 2008;34(11):2076–2083. PubMed CrossRef
- Ratzon R, Reiter J, Goltser-Dubner T, et al. Sleep measures as a predictor of suicidal ideation among high-risk adolescents. Eur Child Adolesc Psychiatry. 2024;33:2781–2790. PubMed CrossRef
- Giménez MC, Geerdinck LM, Versteylen M, et al. Patient room lighting influences on sleep, appraisal, and mood in hospitalized people. J Sleep Res. 2017;26(2):236–246. PubMed CrossRef
- Drummond LM, Wulff K, Rani RS, et al. How should we measure delayed sleep phase shift in severe, refractory obsessive-compulsive disorder?. Int J Psychiatry Clin Pract. 2012;16(4):268–276. PubMed CrossRef
- Stansbury R, Abdelfattah M, Chan J, et al. Hospital screening for obstructive sleep apnea in patients admitted to a rural, tertiary care academic hospital with heart failure. Hosp Pract. 2020;48(5):266–271. PubMed CrossRef
- Schneider CL, Hertenstein E, Nissen C. Cognitive behavioural therapy for insomnia in inpatient psychiatric care: a systematic review. J Sleep Res. 2023;32(6):e14041. PubMed CrossRef
- White B, Snyder HS, Patel MVB. Evaluation of medications used for hospitalized patients with sleep disturbances: a frequency analysis and literature review. J Pharm Pract. 2023;36(1):126–138. PubMed CrossRef
- Walsh JK, Krystal AD, Amato DA, et al. Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations. Sleep. 2007;30(8):959–968. PubMed CrossRef
- Krystal AD, Erman M, Zammit GK, et al. Long-term efficacy and safety of zolpidem extended-release 12.5 mg, administered 3 to 7 nights per week for 24 weeks, in patients with chronic primary insomnia: a 6-month, randomized, double-blind, placebo-controlled, parallel-group, multicenter study. Sleep. 2008;31(1):79–90. CrossRef
- Liu L, Jia L, Jian P, et al. The effects of benzodiazepine use and abuse on cognition in the elders: a systematic review and meta-analysis of comparative studies. Front Psychiatry. 2020;11:00755.
- He Q, Chen X, Wu T, et al. Risk of dementia in long-term benzodiazepine users: evidence from a meta-analysis of observational studies. J Clin Neurol. 2019;15(1):9–19. PubMed CrossRef
- Kolla BP, Lovely JK, Mansukhani MP, et al. Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1–6. PubMed CrossRef
- Young JS, Bourgeois JA, Hilty DM, et al. Sleep in hospitalized medical patients, part 2: behavioral and pharmacological management of sleep disturbances. J Hosp Med. 2009;4(1):50–59. PubMed CrossRef
- Kanji S, Mera A, Hutton B, et al. Pharmacological interventions to improve sleep in hospitalised adults: a systematic review. BMJ Open. 2016;6(7):e012108. CrossRef
- Buysse DJ. Insomnia. JAMA. 2013;309(7):706–716. PubMed
- Spadoni G, Bedini A, Lucarini S, et al. Pharmacokinetic and pharmacodynamic evaluation of ramelteon: an insomnia therapy. Expert Opin Drug Metab Toxicol. 2015;11(7):1145–1156. PubMed CrossRef
- Khaing K, Nair BR. Melatonin for delirium prevention in hospitalized patients: a systematic review and meta-analysis. J Psychiatr Res. 2021;133:181–190. CrossRef
- Chen S, Shi L, Liang F, et al. Exogenous melatonin for delirium prevention: a meta-analysis of randomized controlled trials. Mol Neurobiol. 2016;53(6):4046–4053. PubMed CrossRef
- Wibrow B, Martinez FE, Myers E, et al. Prophylactic melatonin for delirium in intensive care (Pro-MEDIC): a randomized controlled trial. Intensive Care Med. 2022;48(4):414–425. PubMed CrossRef
- Kato K, Hirai K, Nishiyama K, et al. Neurochemical properties of ramelteon (TAK 375), a selective MT1/MT2 receptor agonist. Neuropharmacology. 2005;48(2):301–310. PubMed CrossRef
- Janto K, Prichard JR, Pusalavidyasagar S. An update on dual orexin receptor antagonists and their potential role in insomnia therapeutics. J Clin Sleep Med. 2018;14(8):1399–1408. PubMed CrossRef
- Cheng JY, Filippov G, Moline M, et al. Respiratory safety of lemborexant in healthy adult and elderly subjects with mild obstructive sleep apnea: a randomized, double-blind, placebo-controlled, crossover study. J Sleep Res. 2020;29(4):e13021. PubMed CrossRef
- Fietze I, Bassetti CLA, Mayleben DW, et al. Efficacy and safety of daridorexant in older and younger adults with insomnia disorder: a secondary analysis of a randomised placebo-controlled trial. Drugs Aging. 2022;39(10):795–810. PubMed CrossRef
- Kishi T, Nishida M, Koebis M, et al. Evidence-based insomnia treatment strategy using novel orexin antagonists: a review. Neuropsychopharmacol Rep. 2021;41(4):450–458. PubMed CrossRef
- Xu S, Cui Y, Shen J, et al. Suvorexant for the prevention of delirium: a meta analysis. Med (Baltimore). 2020;99(30):e21043. PubMed CrossRef
- Krystal AD, Lankford A, Durrence HH, et al. Efficacy and safety of doxepin 3 and 6 mg in a 35-day sleep laboratory trial in adults with chronic primary insomnia. Sleep. 2011;34(10):1433–1442. PubMed
- Krystal AD, Durrence HH, Scharf M, et al. Efficacy and safety of doxepin 1 mg and 3 mg in a 12-week sleep laboratory and outpatient trial of elderly subjects with chronic primary insomnia. Sleep. 2010;33(11):1553–1561. CrossRef
- Gerretsen P, Pollock BG. Drugs with anticholinergic properties: a current perspective on use and safety. Expert Opin Drug Saf. 2011;10(5):751–765. PubMed CrossRef
- Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306(12):1359–1369. PubMed CrossRef
- Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294(15):1934–1943. PubMed CrossRef
- Watt JA, Gomes T, Bronskill SE, et al. Comparative risk of harm associated with trazodone or atypical antipsychotic use in older adults with dementia: a retrospective cohort study. CMAJ. 2018;190(47):E1376–E1383. CrossRef
- Herzig SJ, Rothberg MB, Moss CR, et al. Risk of in-hospital falls among medications commonly used for insomnia in hospitalized patients. Sleep. 2021;44(9):zsab064. PubMed CrossRef
- Krystal AD. Treatment of insomnia. In: Schatzberg AF, Nemeroff CB, eds. The American Psychiatric Association Publishing Textbook of Psychopharmacology DSM. 5th ed. American Psychiatric Association Publishing; 2017:1349–1376.
- Stahl SM. Stahl’s Essential Psychopharmacology: Prescriber’s Guide. 7th ed. Cambridge University Press; 2020.
- Gillis CM, Poyant JO, Degrado JR, et al. Inpatient pharmacological sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652–657. PubMed CrossRef
- Bell CM, Fischer HD, Gill SS, et al. Initiation of benzodiazepines in the elderly after hospitalization. J Gen Int Med. 2007;22(7):1024–1029. PubMed CrossRef
- Edinoff AN, Nix CA, Hollier J, et al. Benzodiazepines: uses, dangers, and clinical considerations. Neurol Int. 2021;13(4):594–607. PubMed CrossRef
- Passarella S, Duong MT. Diagnosis and treatment of insomnia. Am J Health Syst Pharm. 2008;65(10):927–934. CrossRef
- Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin. 2008;24(3):493–515, vi. CrossRef
Enjoy this premium PDF as part of your membership benefits!