Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(2):24f03873
Author affiliations are listed at the end of this article.
Have you ever wondered whether and how you should manage anxiety, agitation, and fear in your critically ill patients? Have you been unsure about how you can initiate, maintain, and discontinue analgesics and sedatives safely? Have you hoped that you could mitigate the stress that accompanies and follows an intensive care unit (ICU) stay? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, a 64-year-old woman with history of anxiety and interstitial lung disease, was admitted to the ICU after receiving a bilateral lung transplant. Immediately after surgery, she became intensely agitated, which required the use of multiple sedating agents (including dexmedetomidine, benzodiazepines [BZDs], and opiates). After 10 days on this regimen, which controlled her agitation, her sedatives were weaned over the next 2 days to facilitate a spontaneous breathing trial. Unfortunately, Ms A became increasingly agitated, hypertensive, tachycardic, and diaphoretic. Psychiatric consultation was requested to help manage her distress and hyperdynamic state.
On evaluation, Ms A was anxious and disoriented and had impaired attention and difficulty breathing. Nursing staff reported that Ms A had slept poorly and become paranoid since her sedating medications were tapered. She was diagnosed with delirium, and several recommendations were made (eg, restart dexmedetomidine to reduce anxiety/agitation and facilitate sleep, start haloperidol for agitation associated with hyperactive delirium, and begin ramelteon to optimize her sleep/wake cycle). Within several days, her agitation, anxiety, distress, and sleep were markedly improved, and 1 week later, she was transferred out of the ICU.
Two weeks later, psychiatry was reconsulted before her discharge to a rehabilitation facility. She had been having nightmares and flashbacks about her ICU stay. She was diagnosed as having an acute stress disorder and was referred for outpatient psychiatric follow-up.
WHY ARE ANALGESICS AND SEDATIVES NEEDED IN THE ICU?
Pain, fear, anxiety, sleep disturbances, and agitation are common symptoms among critically ill patients. These symptoms not only cause distress and interfere with medical care but also contribute to morbidity post discharge and therefore warrant swift and effective interventions. Opioids and sedatives are among the most common pharmacologic interventions in ICUs, as their short half-lives, flexible dosing schedules, and varied routes of administration allow for rapid dose titration and symptomatic relief. However, the use of these agents must be judicious, as opioids and sedatives carry the potential of side effects, tolerance, and contribution to delirium. The 2018 Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (ie, the PADIS guidelines) provide a road map for evidence-based, patient-centered protocols, including the ABCDEF (A-F) bundle (where “C” represents “choice of analgesia and sedation”)1 to ensure effective treatment while preventing debilitating physical, affective, behavioral, and cognitive sequelae of critical care (ie, postintensive care syndrome).2,3
HOW ARE ANALGESICS AND SEDATIVES USED IN THE ICU?
Analgesia in ICUs is primarily achieved through the use of opioids, among them natural opiates (such as morphine) and synthetic opioids (such as fentanyl and hydromorphone). Opioids bind primarily to μ-opioid receptors, although they also have some affinity for δ- and κ-opioid receptors as well.4 These receptors are distributed throughout the brain and spinal cord, and their inhibition interferes with the transmission of pain signals, thereby reducing or abolishing the perception of pain. Opioids also facilitate sedation and ventilatory synchrony through the induction of respiratory depression and cough suppression.4,5
Sedation is accomplished through the modulation of γ-aminobutyric acid (GABA) and α-adrenergic receptors. GABA is the main inhibitory neurotransmitter. GABA receptors are subdivided into GABAA and GABAB; GABAA receptors, associated with fast synaptic inhibition, are found throughout the central nervous system (but in particularly high concentrations in the limbic system) and are the major molecular targets for the action of BZDs and other GABA modulators.
Propofol is a GABAA allosteric modulator. It is a parenterally administered anesthetic that produces a rapid, but short lived, loss of consciousness. It is administered via continuous infusion to provide sedation to intubated and mechanically ventilated ICU patients.6 Midazolam, a parenterally administered BZD, similarly provides sedation when administered continuously.7 Current guidelines recommend use of non BZD sedatives over BZDs for sedation and agitation in the ICU, due to their better short- and long-term outcomes. Nevertheless, BZDs remain popular as adjunctive sedating agents.2
Dexmedetomidine, on the other hand, is a highly selective α2-adrenoreceptor agonist. Presynaptic activation of α2-adrenoreceptors inhibits the release of norepinephrine, terminating the propagation of pain signals. Postsynaptic activation inhibits sympathetic activity, decreasing blood pressure and heart rate. Combined, these effects can produce analgesia and sedation.8 Dexmedetomidine induces arousable sedation, which has been shown to mimic stage 2 non–rapid eye movement (REM) sleep with limited effect on respiratory drive; therefore, dexmedetomidine has been approved for sedation of intubated and mechanically ventilated adults, as well as for sedation of nonintubated adults.9 It has also been associated with more favorable outcomes than other sedatives (in terms of length of ICU stay, duration of mechanical ventilation, and incidence of delirium).2
The continuous infusion of opiates and sedatives is often a necessary component of care for patients who require mechanical ventilation. While the Society of Critical Care Medicine (SCCM) supports an approach that achieves adequate pain control and sedation with the exclusive use of opioids, many patients also require a GABA agonist or α-adrenergic agent to achieve treatment goals. The synergistic effects of coadministered agents allow for the use of a lower dose of each agent used.10
HOW CAN ANALGESICS AND SEDATIVES BE INITIATED, MAINTAINED, AND WITHDRAWN SAFELY IN CRITICALLY ILL INDIVIDUALS?
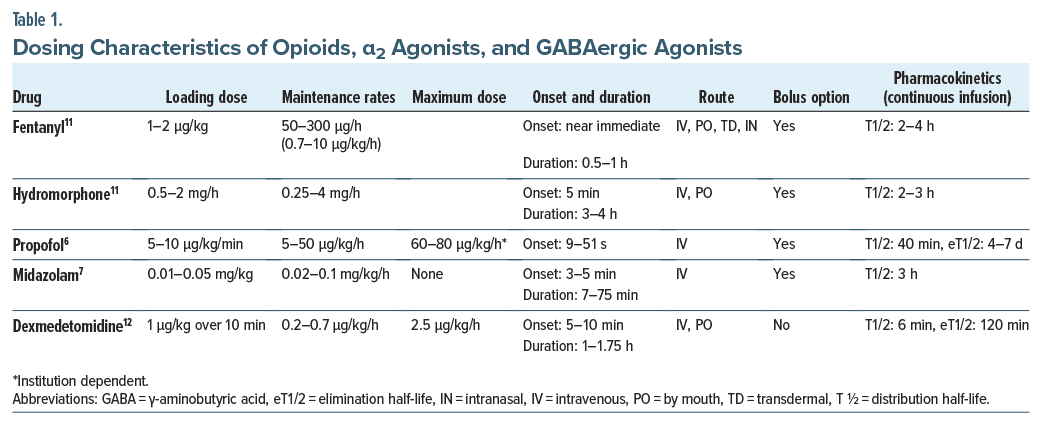
Table 1 outlines recommended induction (loading) and maintenance doses, maximum doses, expected rates of onset and duration, routes of administration, options for bolus administration, and pharmacokinetics of continuous infusion for these agents. The maintenance of these agents must include careful monitoring and correction of side effects. Doses should be adjusted to specific clinical goals, which should be re-evaluated routinely based on clinical status, and the use of the lowest effective doses should always be a priority. Although there is considerable overlap, each class of these agents has distinct side effects worth noting.
Side Effects
Even target doses of opioids may lead to oversedation, constipation, urinary retention, nausea, vomiting, pruritus, respiratory depression, hypotension, and euphoria. Prolonged use may result in opioid induced hyperalgesia.13 Propofol’s most common and problematic side effects include oversedation, respiratory depression, and hypotension. However, with the use of prolonged continuous infusions, hypertriglyceridemia, pancreatitis, and a propofol related infusion syndrome (a potentially fatal syndrome involving multiple organ dysfunction) can develop.14,15
Side effects of BZDs commonly include oversedation, respiratory depression, and hypotension.14 Several studies involving ICU patients have shown that BZDs worsen outcomes for time to light sedation, time to extubation, and length of ICU stay when compared to the use of propofol or dexmedetomidine.2 The most common side effects of dexmedetomidine are hypotension and bradycardia, while tachyphylaxis (the diminished response to successive doses) often develops to the anxiolytic and hypnotic effects of continuously administered dexmedetomidine.16 Opioids and BZDs have both been strongly implicated in the development, maintenance, and/or exacerbation of delirium.12,16
Tolerance and Withdrawal
With prolonged use, all analgesics and sedatives may result in the body’s tolerance of the agent, which manifests with the need for higher doses to maintain effective analgesia or sedation, further increasing the risk and severity of side effects,13 as well as risk for withdrawal.
Recognition of iatrogenic withdrawal from analgesics or sedatives requires vigilance and a high index of suspicion, as symptoms may often be misinterpreted as complications of the critical illness or delirium (eg, agitation), particularly due to the lack of well-validated tools for the detection or measurement of iatrogenic withdrawal in critically ill adults.17 Continuous opioid infusions longer than 3 days in duration are associated with an increased risk for iatrogenic opioid withdrawal syndrome (OWS), when opioid doses are tapered rapidly or are discontinued.18 The prevalence of iatrogenic OWS in ICUs is reported as 15%–40%; however, higher prevalence rates are observed when standardized monitoring protocols and diagnostic criteria are implemented.18,19 OWS signs and symptoms include mydriasis, piloerection, lacrimation, rhinorrhea, increased pulmonary secretions, and diarrhea. OWS signs and symptoms are more specific than withdrawal symptoms from other substances (eg, drugs that work at the alcohol, BZD, and barbiturate receptors), which lead to signs of autonomic hyperarousal (eg, tachycardia, hypertension, hyperreflexia, and agitation).
Signs of OWS typically develop within 2 days after a decrease in their dosing; however, they can arise up to 2 weeks after the opioid has been tapered or discontinued. If a patient demonstrates signs of OWS, a basal dose reduction of 10%–25% daily can be employed (in part dependent on the duration of the continuous infusion, the duration of the premorbid opioid use history, and the patient’s physiologic reaction to the taper). Cross-tapering to another opioid, especially a longer-lasting one (eg, buprenorphine and methadone) that lacks active metabolites, is a viable strategy that that may mitigate problematic side effects of opioid use.13 Other adjunctive agents (eg, α2 agonists such as dexmedetomidine and clonidine) or glutamate modulators (eg, ketamine) can help to mitigate withdrawal symptoms, although they may mask the diagnosis if they are started before OWS arises.
Manifestations of BZD withdrawal include signs and symptoms of adrenergic excess (eg, tachycardia, diaphoresis, tremor, and mydriasis), as well as nausea, vomiting, anxiety, headache, hallucinations, sensory disturbances, agitation, confusion, and seizures. Given that both BZDs and propofol are GABAergic agents, their withdrawal states have a significant overlap of signs and symptoms, though only a few case reports have detailed the manifestations and course of propofol withdrawal.20,21 Propofol is a very short-lasting medication, and it accumulates less than many BZDs following a continuous infusion; these properties increase the likelihood that a withdrawal state will develop once the infusion has been discontinued, as it leads to a more rapid dissociation from receptors and a less gradual self-taper. Unfortunately, evidence-based guidelines are lacking regarding when to be concerned about, and how to manage, propofol withdrawal. Given its nonspecific and overlapping symptoms with delirium, rebound hypertension, and tachycardia, the diagnosis can be challenging. Clinicians should consider slowing the taper should a withdrawal syndrome appear or a cross taper with lorazepam, but guidance on these strategies is limited.
If a BZD withdrawal syndrome is considered, a fixed taper of 10%–25% per day (of the total daily dose) is reasonable, analogous to the management strategy used in alcohol withdrawal. As BZDs can be deliriogenic in the critically ill, this fixed-dose strategy can help to clarify the clinical course while removing the danger associated with missing a potentially life-threatening drug withdrawal or complicating the management of other causes of delirium for which BZDs have been administered. In this setting, symptomatic management of delirium can be undertaken.22
Dexmedetomidine withdrawal syndrome presents with tachycardia, hypertension, anxiety, agitation,headache, and tremor within 24 hours of the drug’s discontinuation.23 Unfortunately, the medical literature on this syndrome remains sparse. Although there has been no standardized method of assessment, recent studies estimate that its incidence is between 30% and 64%.23,24 Several studies have shown promising results when cross-titration has been used with enteral clonidine, an α2-adrenoreceptor agonist with a longer half-life, to mitigate adverse effects from the discontinuation of dexmedetomidine.25 A prospective observational study and a retrospective analysis that investigated the mitigation of the risks of dexmedetomidine withdrawal using a rapid cross titration to clonidine while weaning from dexmedetomidine showed that aggressive clonidine dosing was well-tolerated; moreover, it allowed for a safe transition to an oral agent that could be tapered over several days, taking advantage of clonidine’s longer half life.16,26 Guanfacine, an α2-adrenoreceptor agonist with greater α2 selectivity than both clonidine and dexmedetomidine, is another option with a growing literature base. As compared to the other α2 agonists, guanfacine is less likely to result in adverse cardiovascular effects, including hypotension and bradycardia, and it can prove effective when managing α2 agonist withdrawal as well as dexmedetomidine weaning.27
Unfortunately, the SCCM guidelines for the prevention and management of pain, agitation, sedation, delirium, immobility, and sleep disruption in critically ill patients fail to offer a recommendation on the risk of, or the management of, withdrawal syndromes following administration of sedatives or analgesics.2 The diagnosis of a withdrawal syndrome can be challenging in critically ill individuals who are emerging from deeper and longer lasting sedation, while agitation and autonomic instability commonly appear in emergence delirium, unmasked pain, and each of the above-mentioned withdrawal states. Withdrawal from medications that stimulate GABAergic receptors is more worrisome due to its risk of inducing seizures and death.
Further, the pharmacokinetics of many of these medications are significantly altered by critical illness, and it is hard to predict when a patient has accumulated a drug, thus decreasing the likelihood of withdrawal, or when they have rapidly metabolized the drug, which raises the risk.28 Spontaneous awakening trials have been efficacious regarding lowering the risk of withdrawal symptoms, when used in protocolized fashion after 2 weeks of a continuous infusion.29 When protocolized daily re-titration of sedation has not been possible, or when longer duration infusions have been utilized, a more pragmatic approach should be taken to mitigate both the risk for and effect of withdrawal.
While each of these withdrawal syndromes presents challenges in terms of diagnostic clarity and management, a poly-drug withdrawal is even more complicated, and it can lead to inappropriate treatment of one syndrome with a drug from another class. When multiple medication classes with the potential for withdrawal have been used for longer periods, the use of a step-wise approach to identify and manage withdrawal syndromes can mitigate problems. This can be accomplished through multiple avenues: instituting single agent tapering and monitoring for effects, alternating the taper of drug classes every few days, and using conservative, fixed-dose, tapering schedules for at least one of the classes to isolate the possibility of withdrawal from that class.
HOW DO ANALGESICS AND SEDATIVES COMPARE IN TERMS OF THE DEVELOPMENT AND MANAGEMENT OF DELIRIUM?
The “neurotransmitter hypothesis of delirium” posits that delirium is associated with reduced availability of acetylcholine (↓Ach) and excess release of dopamine (↑DA), norepinephrine (↑NE), and/or glutamate (↑GLU) and that the cholinergic and dopaminergic systems interact with each other and influence the glutamatergic (GLU; the primary excitatory neurotransmitter) and GABA pathways.30,31
Opioids
Opioids have consistently been invoked as a primary precipitating factor in the development of delirium, in part due to their ability to increase activity of DA and GLU, while decreasing ACh activity or altering GABAergic effects.32–34 Consistent with this theory, Duprey and colleagues35 found that administering an opioid to awake patients without delirium was associated with an increased risk for delirium the next day. Moreover, each daily 10-mg IV morphine-equivalent dose was associated with a 2.4% greater risk for delirium the next day, suggesting that opioid use in ICUs increases the odds of developing delirium in a dose-dependent fashion.
Sedatives
Sedatives in ICUs have long been recognized as predisposing to delirium especially when used continuously, and they contribute to a host of other neuropsychiatric side effects (including anxiety, depression, posttraumatic stress disorder [PTSD], and cognitive impairment via disruption of physiologic sleep patterns, inhibition of central ACh, and disruption of circadian rhythm).22,30,36
Many psychotropics also compromise thalamic gating functions and lead to sensory overload and hyperarousal. Gaudreau and Gagnon37 proposed that drug-induced delirium might result from such transient thalamic dysfunction that is caused by exposure to medications that interfere with central glutamatergic, GABAergic, dopaminergic, and cholinergic pathways at critical sites of action.
The only sedative not shown to provoke delirium is dexmedetomidine.38 Maldonado and colleagues39 were among the first to report a substantial reduction in postoperative delirium among patients undergoing cardiac surgery when dexmedetomidine was administered (ie, 3%), as compared with the use of conventional GABAergic agents (ie, 50% incidence of delirium with propofol or midazolam). Since then, multiple studies have found a lower incidence of delirium when dexmedetomidine was employed as the primary sedating agent, as well as demonstrating reductions in the mean duration of mechanical ventilation and ICU length of stay when compared to conventional GABAergic based sedation.40 These results might be associated with multiple pharmacologic and physiologic effects of dexmedetomidine, including its relative lack of respiratory depression (with poor oxygenation being a known risk factor for delirium), unimpressive impact on acetylcholine (deficient in delirium), antinociceptive effects (with documented reduction in the need for opiate agents), and modulating effects of the 2 main excitatory neurotransmitter systems, the noradrenergic and glutamatergic systems.30
HOW DO ANALGESICS AND SEDATIVES TARGET AGITATION AND SLEEP?
Agitation
Agitation may be the result of neurotransmitter dysfunction in the reticular activating system (RAS) that projects to higher cortical structures.41 The primary modulators of RAS function are GLU, GABA, and ACh systems.41 Monoaminergic and orexigenic subsystems augment these pathways to fine-tune RAS circuitry.41 Fortunately, several GABAergic agents (eg, propofol and midazolam) and α2-adrenergic agents (eg, dexmedetomidine) can override these neurotransmitter systems to reduce agitation and facilitate sedation.
Sleep
Sleep abnormalities, such as prolonged sleep latency, multiple short bouts of sleep during the day and night, sleep fragmentation, decreased sleep efficiency, numerous arousals, a preponderance (increased) of stage 2 sleep (N2), decreased or absent stage 3 and 4 (N3 and 4, “deep”) sleep, increased arousals, altered circadian timing, and severely diminished or absent REM sleep, are common in the ICU.42 Unfortunately, it is extremely difficult to promote biomimetic sleep patterns (ie, the induction and maintenance of REM and non-REM stages 1–3 [N1–N3] brain states that approximate natural sleep) in the ICU through pharmacologic interventions.43
The α2 agonists modulate norepinephrine transmission to promote sleep by acting on endogenous sleep pathways, enhancing deep sleep without affecting REM sleep.44 Dexmedetomidine promotes a deeper, more physiologic, sleep pattern with a shortened N1 stage and promotion of slow wave sleep (N3). The increase in N3 sleep occurs in a dose-dependent manner, although with some compensatory decreased time spent in REM sleep.43,45 While commonly used at a continuous level, dexmedetomidine has further reduced the incidence of delirium and enhanced sleep quality if it is dosed in a “cycled” format—with higher doses used at night and lower doses during the day—to protect sleep architecture.38,46
However, GABAergic agents are notorious for their negative impact on sleep architecture. BZDs act in a dose dependent fashion to increase N2 sleep but to decrease all other stages, with potent suppression of slow wave sleep and REM.47 Similarly, propofol decreases the total amount of time spent in REM sleep, but it does not induce a biomimetic form of sleep waves. This is observed in propofol’s effects more on posterior brain regions seen in physiologic sleep and notable disrupted spindle activity, both of which are thought to be due to propofol’s indiscriminate effects on GABA receptors throughout the brain.48 Lastly, opioids have a similarly detrimental effect on sleep architecture, with a reduction in stage N3 and REM sleep.49 This is distinct from opioids’ effects on suppressing respiratory drive, as well as on increasing apneic events in those with and without sleep apnea.49
CAN ANALGESICS AND SEDATIVES MITIGATE THE TRAUMATIC EFFECTS OF BEING TREATED IN THE ICU?
Many survivors of critical illness experience trauma and stressor-related symptoms after discharge from the ICU.30 Nearly three-fourths of ICU survivors experience delusional memories about their ICU experience.38 These memories are often profoundly negative, with hallucinations, dreams, or nightmares about people (often medical staff) trying to hurt them. Those with delusional or illusory memories are apt to develop PTSD, as well as panic attacks and phobias.50 Factual (although unpleasant) memories, on the other hand, may indeed be protective against the development of trauma-related disorders.
Trauma- and stressor-related disorders, such as PTSD, have been associated with a dysfunctional fear system, which is governed by the amygdala. The amygdala detects and reflexively responds to threat through associative learning.51 Hypotheses about the development of PTSD revolve around excessive consolidation of, and failure to extinguish, fear memories.32
Given the direct involvement of N-methyl-D aspartate, GABA, and adrenergic systems in fear memory processes, as well as the hypothesized modulation of emotional memory and stress responses by opioid receptors, it is likely that all analgesics and sedatives have some effect on the fear-memory system and thereby on the traumatic effects of critical illness and an ICU stay.33,34,51
Rodent studies have demonstrated that the modulation of fear-learning occurs (through its effects on fear consolidation or retention) in association with the use of opioids, midazolam, propofol, or dexmedetomidine. However, results have varied and depended on the dose used (ie, subtherapeutic, therapeutic, or supra-therapeutic) and the timing of their administration relative to the adverse event.34 These studies suggest that unlike explicit memory, fear-memory processes occur outside of consciousness.34
The level of sedation is a risk factor for the development of PTSD, with deeper levels of sedation (eg, with coadministration of a BZD and an opioid) leading to a higher risk.52 The effect of GABA on memory consolidation is thought to be the biggest offender in ICU related PTSD. BZDs impact cortical, corticothalamic, and corticolimbic networks, with these circuits playing a key role in the regulation of fear and anxiety responses and the development of mood symptoms.36 In addition, there is a decreased density of GABA-A receptors in the hippocampus and amygdala.36,53 These circuit-related phenomena have led to studies showing a 2 to 5 times higher risk of developing PTSD in those who receive a BZD than in those who do not, with the cumulative dose and duration of BZDs in the ICU being linked with the development of PTSD.36,53 BZDs are associated with PTSD: worse overall severity, significantly increased risk of developing PTSD with use after recent trauma, worse psychotherapy outcomes, aggression, depression, and substance use.53
While GABAergic agents are often identified as one of the more influential agents on memory consolidation, there is a growing body of literature on opioid-associated amnestic syndrome, defined by acute memory loss with known hippocampal impact. Fentanyl is often implicated in these cases, which is notable given its frequent use in ICUs. On the other hand, higher doses of morphine for pain control have decreased the incidence of PTSD in at least 2 studies.43
Propofol has been repeatedly associated with an increased risk of developing PTSD symptoms in comparative but small studies.32,34 On the other hand, a recent randomized clinical trial of low-dose dexmedetomidine used intra- and postoperatively as an adjunct to typical anesthesia (propofol) showed reduced rates of PTSD when compared to a placebo group.54
HOW CAN CLINICIANS DECIDE WHICH CLASS OF AGENTS SHOULD BE USED FIRST AND WHICH SHOULD BE DISCONTINUED FIRST?
Given their detrimental effects on sleep architecture and quality, as well as neuropsychiatric side effects (including delirium, cognitive impairment, PTSD, and anxiety), GABAergic agents (eg, midazolam, propofol) should be weaned as early as possible. This should be followed by a dose reduction, if feasible, in continuous opioid administration. Complete cessation of opioids, however, may not be possible given an ongoing need for analgesia (a reminder that untreated pain on its own is a risk factor for the development of delirium).55
The last agent to be removed should be the α2 agonist (eg, dexmedetomidine) due to its ability to reduce the incidence of delirium and the need for supplemental pain medications and its lack of respiratory suppression, allowing for use without invasive respiratory support.39
The use of α2 agonists can facilitate the weaning of conventional sedative agents. More recently, researchers have demonstrated that the use of the long-acting α2 agonist guanfacine might assist with weaning patients off dexmedetomidine, when this agent has been used for extended periods. Kim and colleagues56 demonstrated that the addition of guanfacine decreased the requirement of all other CNS depressants commonly used for the management of hyperactive delirium, including opioids (a 57% reduction) and GABAergic (9% reduction) agents, which not only lowers the patient’s exposure to deliriogenic agents but also predictably limits dexmedetomidine use and reduces overall cost of care and ICU length of stay. More recently, Jiang and colleagues27 reported similar results.
When a patient is transferring out of the ICU, the ICU team should simplify the treatment regimen whenever possible, taking into consideration what the patient is likely to need on the medical or surgical floor and what may be needed even after hospital discharge (eg, to a rehabilitation facility or to home). When feasible, GABAergic agents should be tapered, rather than discontinued abruptly. During this transition, α2 agonists may mitigate anxiety, insomnia, and pain and may be continued after transfer (being mindful that dexmedetomidine is only available in ICUs and a switch to another α2 agent [eg, guanfacine, clonidine] should be considered). Interventions to manage delirium should be continued, as delirium’s etiology may remain active. Tapering such treatments will depend on the etiology of delirium and its trajectory.
WHAT OTHER STRATEGIES CAN BE USED TO REDUCE ANXIETY, PAIN, AGITATION, AND FEAR IN CRITICALLY ILL PATIENTS?
Beyond pharmacology, psychosocial factors should be addressed to help manage anxiety, pain, agitation, and fear. Critical care settings can be overstimulating and overwhelming. Moreover, obtaining adequate amounts of restful sleep can be nearly impossible in ICUs, as days are filled with medical tests, procedures, and examinations and nighttime interruptions are commonplace. Discussions about what transpired in the ICU can be valuable for patients and their family members, and correcting misconceptions often reduces distress.
The “F” in the ABCDEF bundle represents family engagement and empowerment. Family members are uniquely positioned to provide background information related to the premorbid functioning and personality of their loved one, which helps to guide the team towards communication strategies and treatment approaches to reduce stress and build rapport with the patient. Loved ones and friends are often uniquely positioned to notice subtle cognitive changes and can serve as a helpful proxy for delirium identification and symptom tracking. Extended visiting hours in the ICU has been shown to reduce the incidence of delirium, as well as mitigate anxiety symptoms and improve patient satisfaction.57
Bedside therapies, including music therapy and hypnosis, are other powerful strategies to help mitigate distress in the ICU. Music therapy has numerous studies to support its positive effects in critical care, demonstrating evidence to reduce self-reported pain and anxiety levels in patients, as well as objective measures of hyperarousal (respiratory rate and heart rate).58 Hypnosis has similarly proven effective at reducing pain.59 Patients’ abilities to self-hypnotize can also prove useful in managing the distress surrounding noninvasive ventilation and increasing feelings of safety while hospitalized.60 Intensivists, primary care physicians, and psychiatrists can expand their recommendations to include these nonpharmacologic, multimodal techniques to reduce the impact of distress and agitation, which can reduce the level of postintensive care psychopathology.
CONCLUSION
Critical care has increasingly moved towards the use of protocol-based, assessment-driven, treatment algorithms for the titration of analgesics and sedatives. The SCCM encourages the use of evidence-based stepwise approaches to titrate opiates and sedatives to mitigate pain, agitation, and confusion, while minimizing the risk of developing delirium, prolonged deep sedation, and other adverse side effects associated with the use of these agents.2 Such algorithms are characterized by several features, eg, the frequent assessment of pain, monitoring of the level of agitation and sedation, and tracking the manifestations of delirium. These factors are facilitated by the use of validated tools, by close postdose monitoring of symptoms that facilitates dose adjustments, and by continuous monitoring for adverse effects that minimizes unnecessary medication exposure.61 The use of such algorithms has reduced overuse of opiates and sedatives and decreased 30-day mortality rates, ICU and hospital length of stay, duration of mechanical ventilation, and presence of coma and delirium.61
While being critically ill can be traumatic, several aspects of an ICU stay raise one’s risk for treatment-induced traumatic experiences, including administration of BZDs and opioids, as well as frightening memories related to one’s ICU stay.36,50,62 The use of analgesics and sedatives has been associated with impaired cognition (eg, involving attention, language, orientation, psychomotor function, and verbal working/delayed episodic memory),63 sleep disturbance (in 35%–57%), and fatigue (in 10%) as well as delirium,64 all of which can exacerbate risk of trauma- and stressor-related disorders (such as PTSD). Intensivists, psychiatrists, and primary care physicians each play a critical role in the management of the sequelae of critical illness.
Article Information
Published Online: April 1, 2025. https://doi.org/10.4088/PCC.24f03873
© 2025 Physicians Postgraduate Press, Inc.
Submitted: October 14, 2024; accepted January 17, 2025.
To Cite: Gunther MG, Bieber ED, Bui M, et al. Mitigation of anxiety, agitation, and pain in critically ill patients. Prim Care Companion CNS Disord 2025;27(2):24f03873.
Author Affiliations: Department of Psychiatry and Behavioral Sciences, School of Medicine, Stanford University, Stanford, California (Gunther, Maldonado); Pritzker Department of Psychiatry and Behavioral Health, Ann & Robert H. Lurie Children’s Hospital of Chicago, Illinois (Bieber); Department of Psychiatry and Behavioral Science, Northwestern University Feinberg School of Medicine, Chicago, Illinois (Bieber); Department of Psychiatry, School of Medicine, Virginia Commonwealth University, Richmond, Virginia (Bui); Department of Psychiatry, School of Medicine, University of Texas Southwestern, Dallas, Texas (deVries); Department of Psychiatry and Behavioral Medicine, School of Medicine, Wake Forest University, Winston-Salem, North Carolina (Dragonetti); Department of Psychiatry, Weill Cornell Medicine, New York, NY (Ha); Department of Psychiatry and Neurobehavioral Sciences, School of Medicine, University of Virginia, Charlottesville, Virginia (Rosen); Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts (Stern).
Gunther, Bieber, Bui, deVries, Dragonetti, Ha, and Rosen are co-first authors; Maldonado and Stern are co-senior authors.
Corresponding Authors: Matthew G. Gunther, MD, MA, Department of Psychiatry and Behavioral Sciences, School of Medicine, Stanford University, 401 Quarry Rd, #2317, Stanford, CA 94305 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Opioids (eg, fentanyl, hydromorphone, and morphine) are used to achieve analgesia and sedation; however, these medications also induce a myriad of adverse side effects (eg, oversedation, constipation, urinary retention, nausea, vomiting, pruritus, respiratory depression, hypotension, and euphoria), and following a rapid dose decrease, they can precipitate opiate withdrawal.
- Protocol-based, assessment-driven, treatment algorithms can mitigate pain, agitation, and confusion, while minimizing the risk of developing delirium, prolonged deep sedation, and other adverse side effects associated with the use of these agents.
- One major challenge to identifying withdrawal syndromes from analgesics and sedatives in critically ill individuals relates to the extensive overlap of signs and symptoms of opiate withdrawal and the systemic effects of critical illnesses.
- If a GABAergic withdrawal syndrome is considered, a fixed taper of 10%–25% per day (of the total daily dose) is reasonable, analogous to the management strategy used in alcohol withdrawal.
- The last agent to be removed should be the α2 agonist (eg, dexmedetomidine) due to its ability to reduce the incidence of delirium and the need for supplemental pain medications and its lack of respiratory suppression, allowing for use without invasive respiratory support.
- Intensivists, primary care physicians, and psychiatrists each play a critical role in the management of the sequelae of critical illness (including posttraumatic stress disorder).
References (64)

- Marra A, Ely EW, Pandharipande PP, et al. The ABCDEF bundle in critical care. Crit Care Clin. 2017;33(2):225–243. CrossRef
- Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–e873.
- Ramnarain D, Aupers E, Den Oudsten B, et al. Post Intensive Care Syndrome (PICS): an overview of the definition, etiology, risk factors, and possible counseling and treatment strategies. Expert Rev Neurother. 2021;21(10):1159–1177. CrossRef
- Trescot AM, Datta S, Lee M, et al. Opioid pharmacology. Pain Physician. 2008;11(2 suppl):S133–S153.
- Kosten T, George T. The neurobiology of opioid dependence: implications for treatment. SPP. 2002;1(1):13–20. PubMed CrossRef
- DailyMed - DIPRIVAN- propofol injection, emulsion. 2023. Accessed October 1, 2024. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e3105799-a4b6-f3f4-e6e2-b2b29bbdb538
- DailyMed - MIDAZOLAM HYDROCHLORIDE injection, solution. 2023. Accessed October 1, 2024. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=1abda8b8-48a8-4995-af86-39220d1aa240
- Gertler R, Brown HC, Mitchell DH, et al. Dexmedetomidine: a novel sedative analgesic agent. Proc (Bayl Univ Med Cent). 2001;14(1):13–21. PubMed CrossRef
- Scott-Warren V, Sebastian J. Dexmedetomidine: its use in intensive care medicine and anaesthesia. BJA Educ. 2016;16(7):242–246. CrossRef
- Dutta A, Sethi N, Sood J, et al. The effect of dexmedetomidine on propofol requirements during anesthesia administered by bispectral index-guided closed loop anesthesia delivery system: a randomized controlled study. Anesth Analg. 2019;129(1):84–91. CrossRef
- Hughes CG, McGrane S, Pandharipande PP. Sedation in the intensive care setting. Clin Pharmacol. 2012;4:53–63. CrossRef
- DailyMed - DEXMEDETOMIDINE HYDROCHLORIDE injection, solution, concentrate DEXMEDETOMIDINE HYDROCHLORIDE IN DEXTROSE dexmedetomidine hydrochloride injection. 2021. Accessed October 1, 2024. https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=0d2710f2-ee47-4114-ab5c-8dca74cdcb8d
- Martyn JAJ, Mao J, Bittner EA. Opioid tolerance in critical illness. N Engl J Med. 2019;380(4):365–378. CrossRef
- Devabhakthuni S, Armahizer MJ, Dasta JF, et al. Analgosedation: a paradigm shift in intensive care unit sedation practice. Ann Pharmacother. 2012;46(4):530–540. PubMed CrossRef
- Singh A, Anjankar AP. Propofol-related infusion syndrome: a clinical review. Cureus. 2022;14(10):e30383.
- Terry K, Blum R, Szumita P. Evaluating the transition from dexmedetomidine to clonidine for agitation management in the intensive care unit. SAGE Open Med. 2015;3:2050312115621767. PubMed CrossRef
- Eadie R, McKenzie CA, Hadfield D, et al. Opioid, sedative, preadmission medication and iatrogenic withdrawal risk in UK adult critically ill patients: a point prevalence study. Int J Clin Pharm. 2023;45(5):1167–1175. CrossRef
- Fox MA, Carothers C, Dircksen KK, et al. Prevalence and risk factors for iatrogenic opioid withdrawal in medical critical care patients. Crit Care Explor. 2023;5(5):e0904. CrossRef
- Lamey PS, Landis DM, Nugent KM. Iatrogenic opioid withdrawal syndromes in adults in intensive care units: a narrative review. J Thorac Dis. 2022;14(6):2297–2308. CrossRef
- Imray JM, Hay A. Withdrawal syndrome after propofol. Anaesthesia. 1991;46(8):704. PubMed CrossRef
- Tobias JD. Tolerance, withdrawal, and physical dependency after long-term sedation and analgesia of children in the pediatric intensive care unit. Crit Care Med. 2000;28(6):2122–2132. PubMed CrossRef
- Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104(1):21–26. PubMed CrossRef
- Pathan S, Kaplan JB, Adamczyk K, et al. Evaluation of dexmedetomidine withdrawal in critically ill adults. J Crit Care. 2021;62:19–24. CrossRef
- Bouajram RH, Bhatt K, Croci R, et al. Incidence of dexmedetomidine withdrawal in adult critically ill patients: a pilot study. Crit Care Explor. 2019;1(8):e0035. CrossRef
- Glaess SS, Attridge RL, Christina Gutierrez G. Clonidine as a strategy for discontinuing dexmedetomidine sedation in critically ill patients: a narrative review. Am J Health Syst Pharm. 2020;77(7):515–522. PubMed CrossRef
- Gagnon DJ, Riker RR, Glisic EK, et al. Transition from dexmedetomidine to enteral clonidine for ICU sedation: an observational pilot study. Pharmacotherapy. 2015;35(3):251–259. PubMed CrossRef
- Jiang S, Hernandez M, Burke H, et al. A retrospective analysis of guanfacine for the pharmacological management of delirium. Cureus. 2023;15(1):e33393.
- Morales Castro D, Dresser L, Granton J, et al. Pharmacokinetic alterations associated with critical illness. Clin Pharmacokinet. 2023;62(2):209–220. CrossRef
- Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet. 2008;371(9607):126–134. PubMed CrossRef
- Maldonado JR. Delirium pathophysiology: an updated hypothesis of the etiology of acute brain failure. Int J Geriat Psychiatry. 2018;33(11):1428–1457. PubMed CrossRef
- Trzepacz PT. The neuropathogenesis of delirium. A need to focus our research. Psychosomatics. 1994;35(4):374–391. PubMed CrossRef
- Usuki M, Matsuoka Y, Nishi D, et al. Potential impact of propofol immediately after motor vehicle accident on later symptoms of posttraumatic stress disorder at 6-month follow up: a retrospective cohort study. Crit Care. 2012;16(5):R196. PubMed CrossRef
- Westbrook RF, Greeley JD, Nabke CP, et al. Aversive conditioning in the rat: effects of a benzodiazepine and of an opioid agonist and antagonist on conditioned hypoalgesia and fear. J Exp Psychol Anim Behav Process. 1991;17(3):219–230. PubMed CrossRef
- Vogt KM, Pryor KO. Anesthesia and the neurobiology of fear and posttraumatic stress disorder. Curr Opin Anaesthesiol. 2022;35(5):593–599. CrossRef
- Duprey MS, Dijkstra-Kersten SMA, Zaal IJ, et al. Opioid use increases the risk of delirium in critically ill adults independently of pain. Am J Respir Crit Care Med. 2021;204(5):566–572. CrossRef
- Kok L, Slooter AJ, Hillegers MH, et al. Benzodiazepine use and neuropsychiatric outcomes in the ICU: a systematic review. Crit Care Med. 2018;46(10):1673–1680. CrossRef
- Gaudreau JD, Gagnon P. Psychotogenic drugs and delirium pathogenesis: the central role of the thalamus. Med Hypotheses. 2005;64(3):471–475. PubMed CrossRef
- Lewis K, Alshamsi F, Carayannopoulos KL, et al. Dexmedetomidine vs other sedatives in critically ill mechanically ventilated adults: a systematic review and meta-analysis of randomized trials. Intensive Care Med. 2022;48(7):811–840. CrossRef
- Maldonado JR, Wysong A, Van Der Starre PJA, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3):206–217. PubMed CrossRef
- Flükiger J, Hollinger A, Speich B, et al. Dexmedetomidine in prevention and treatment of postoperative and intensive care unit delirium: a systematic review and meta-analysis. Ann Intensive Care. 2018;8(1):92.
- Kandel ER, Koester J, Mack S, et al, eds. Principles of Neural Science. Sixth edition. McGraw Hill; 2021.
- Elliott R, McKinley S, Cistulli P, et al. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. PubMed CrossRef
- Akeju O, Hobbs LE, Gao L, et al. Dexmedetomidine promotes biomimetic non rapid eye movement stage 3 sleep in humans: a pilot study. Clin Neurophysiol. 2018;129(1):69–78. PubMed CrossRef
- Nelson LE, Lu J, Guo T, et al. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology. 2003;98(2):428–436. PubMed CrossRef
- Liu H, Wei H, Qian S, et al. Effects of dexmedetomidine on postoperative sleep quality: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2023;23(1):88. CrossRef
- Hong KS, Kim NR, Song SH, et al. Cycling of dexmedetomidine may prevent delirium after liver transplantation. Transpl Proc. 2018;50(4):1080–1082. CrossRef
- Weinhouse GL, Schwab RJ. Sleep in the critically ill patient. Sleep. 2006;29(5):707–716. CrossRef
- Murphy M, Bruno MA, Riedner BA, et al. Propofol anesthesia and sleep: a high density EEG study. Sleep. 2011;34(3):283–91A. PubMed CrossRef
- Cutrufello NJ, Ianus VD, Rowley JA. Opioids and sleep. Curr Opin Pulm Med. 2020;26(6):634–641. CrossRef
- Jones C, Griffiths RD, Humphris G. Disturbed memory and amnesia related to intensive care. Memory. 2000;8(2):79–94. PubMed CrossRef
- Ressler KJ, Berretta S, Bolshakov VY, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18(5):273–288. CrossRef
- Costa JBD, Marcon SS, Macedo CRLD, et al. Sedation and memories of patients subjected to mechanical ventilation in an intensive care unit. Rev Bras Ter Intensiva. 2014;26(2):122–129. PubMed CrossRef
- Guina J, Rossetter SR, DeRHODES BJ, et al. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract. 2015;21(4):281–303.
- Yu Y, Li Y, Han D, et al. Effect of dexmedetomidine on posttraumatic stress disorder in patients undergoing emergency trauma surgery: a randomized clinical trial. JAMA Netw Open. 2023;6(6):e2318611.
- Maldonado JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin. 2017;33(3):461–519.
- Kim J, Van Zyl E, Benitez-Lopez M, et al. Use of guanfacine as an alternative to dexmedetomidine for sedation and agitation management in the intensive care unit. J Psychosomatic Res. 2020;133:110062. CrossRef
- Kleinpell R, Heyland DK, Lipman J, et al. Patient and family engagement in the ICU: report from the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2018;48:251–256. CrossRef
- Golino AJ, Leone R, Gollenberg A, et al. Impact of an active music therapy intervention on intensive care patients. Am J Crit Care. 2019;28(1):48–55. CrossRef
- van Veen S, Drenth H, Hobbelen H, et al. Non-pharmacological interventions feasible in the nursing scope of practice for pain relief in palliative care patients: a systematic review. Palliat Care Soc Pract. 2024;18:26323524231222496.
- Schmidt B, Schneider J, Deffner T, et al. Hypnotic suggestions of safety improve well-being in non-invasively ventilated patients in the intensive care unit. Intensive Care Med. 2021;47(4):485–486. CrossRef
- Skrobik Y, Ahern S, Leblanc M, et al. Protocolized intensive care unit management of analgesia, sedation, and delirium improves analgesia and subsyndromal delirium rates. Anesth Analg. 2010;111(2):451–463. PubMed CrossRef
- Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015;43(5):1121–1129. PubMed CrossRef
- Pask S, Dell’Olio M, Murtagh FEM, et al. The effects of opioids on cognition in older adults with cancer and chronic noncancer pain: a systematic review. J Pain Symptom Manage. 2020;59(4):871–893.e1.
- Dhingra L, Ahmed E, Shin J, et al. Cognitive effects and sedation. Pain Med. 2015;16(suppl 1):S37–S43. CrossRef
Enjoy this premium PDF as part of your membership benefits!