Virus-borne infections play a significant role in neuropsychiatric manifestations, with delirium being a systemic infection’s most common secondary complication.1 HIV, herpes simplex virus, varicella-zoster virus, influenza A and other influenza viruses, and hepatitis C virus are viruses that result in infections associated with depression and anxiety. HIV infection may also result in psychosis and mania.2 Respiratory viruses have been associated with psychosis since the 1918 influenza (Spanish flu) pandemic.3 In 1919, Menninger published a case series of 100 patients with neuropsychiatric sequelae associated with influenza infection, including 23 patients with “other psychosis.”3,4
About one-third of the patients with SARS-CoV-2 develop neuropsychiatric symptoms, such as anxiety, depression, psychosis, brain fog, and suicidal behavior.5 Recently, several cases have reported new-onset psychotic symptoms in individuals following an infection with SARS-CoV-2.5,6 The possible etiologic factors are viral exposure, treatment modality (possibly steroids), and psychosocial stress.7,8 From studying recently published case reports,9–11 the psychotic symptoms develop approximately 2 weeks after the remission of fever and flu-like and upper respiratory symptoms. However, these symptoms can develop within the week of the onset of upper respiratory symptoms.4
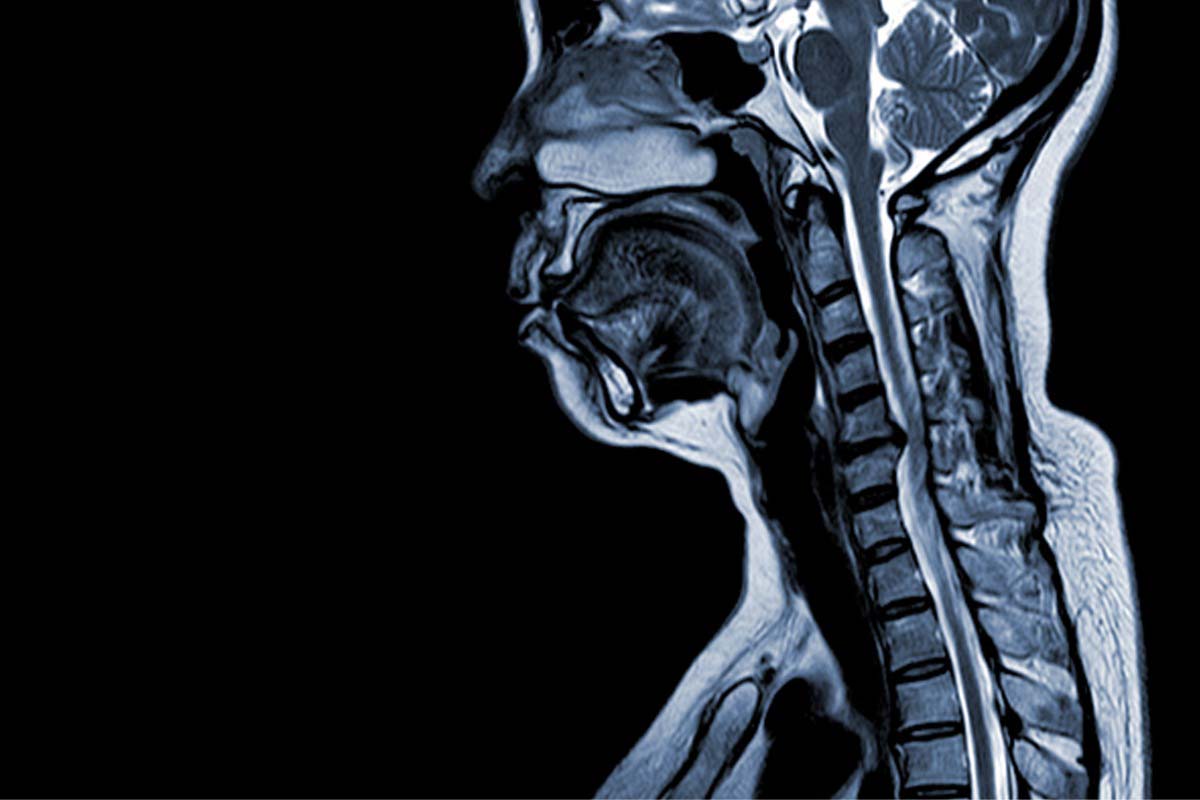
Besides the respiratory system, SARS-CoV-2 targets the central nervous system (CNS), which can lead to cerebrovascular diseases, encephalopathy, and encephalitis.12 Acute psychosis is a rare CNS condition possibly triggered by the inflammatory response to a SARS-CoV-2 infection.7,9 Direct viral infiltration in the CNS triggers the neuroinflammatory reaction, and the microglial-induced demyelinating process causes encephalopathy. Peripheral hypercytokinemia triggers a noninflammatory response, disrupting the blood-brain barrier. The transmigration of the peripheral immune cell into the CNS causes an imbalance in neurotransmitters, which may be responsible for neuropsychiatric manifestations.13 Although it is commonly thought that psychosis related to COVID-19 is due to inflammation, sometimes the inflammatory markers are normal.14
To better understand the neuropsychiatric symptoms and their management following a COVID-19 infection, we reviewed some case reports in the pediatric and adult population. One report15 was of a 15-year-old girl with no known psychiatric history who presented with visual and tactile hallucinations, delusions, and paranoia 2.5 weeks after being infected with COVID-19. She was treated with dexamethasone 4 mg for 5 days for COVID-19, with all her laboratory results being within normal limits except for a positive SARS-CoV-2 serology. Her psychosis was treated with olanzapine 5 mg, which was increased to 7.5 mg, to which she responded. Her symptoms improved, and she was discharged within 5 days.15 In March 2021, a 69-year-old woman presented with symptoms of catatonia, bizarre behavior, visual hallucinations, and paranoid delusions following a resolved COVID-19 infection.16 Her catatonia responded to a trial of therapeutic lorazepam. Other case reports4,9–11 reveal persecutory delusions, auditory and visual hallucinations, disorganized behavior, and agitation as some of the most commonly presenting symptoms. COVID-19–related psychosis tends to respond well to antipsychotics, mood stabilizers, and benzodiazepines. The widely used antipsychotics are haloperidol, risperidone, aripiprazole, and olanzapine.4,9–11
A study from China17 demonstrated the relationship between psychosis-like experiences (PLEs) and COVID-19–related psychological symptoms, including depression, anxiety, neurasthenia, fear, obsession-compulsion, and hypochondriasis. The study17 suggested the predictive value of PLEs for measuring the psychological impact of a public health emergency. The PLEs are associated with many psychosocial factors, such as ethnic minority, urbanization, perceived stress, and childhood trauma.17 In addition, there is evidence of coronavirus-associated psychosis through neuroinflammation, with linked factors including stress, isolation, and uncertainty, further showing how pandemics can increase the risk of psychosis.18
As neuropsychiatric complications can develop within weeks of a COVID-19 infection, health care providers should consider COVID-19 a causative agent of sudden and new-onset psychotic disorders. We propose well-designed and large-scale research studies to explore the pathophysiology behind SARS-CoV-2 and other coronaviruses altering neuronal activity and neurotransmission.
Article Information
Published Online: July 13, 2023. https://doi.org/10.4088/PCC.22br03436
© 2023 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord. 2023;25(4):22br03436
Submitted: October 22, 2022; accepted January 13, 2023.
To Cite: Sultana T, Kamil SH, Billoo F, et al. New-onset psychosis secondary to COVID-19 infection. Prim Care Companion CNS Disord. 2023;25(4):22br03436.
Author Affiliations: Department of Psychopharmacology Research, Manhattan Psychiatric Center, New York, New York (Sultana); Department of Psychiatry, Austin Family Psychiatry, Austin, Texas (Kamil); Department of Family Medicine, Family Medicine Associates, Northridge, California (Billoo); Department of Radiology, Mayo Clinic, Rochester, Minnesota (Lahori); Department of Psychiatry, Griffin Memorial Hospital, Norman, Oklahoma (Shah); Department of Psychiatry, The University of Texas Rio Grande Valley, Harlingen (Vadukapuram); Department of Psychiatry, Boston Children’s Hospital/Harvard Medical School, Boston, Massachusetts (Mansuri); Department of Psychiatry, Texas Tech University Health Sciences Center at Permian Basin, Midland (Jain).
Corresponding Author: Saher Hoda Kamil, MBBS, Department of Psychiatry, Austin Family Psychiatry, 4407 Bee Cave Road, Austin, TX 78746 ([email protected]).
Author Contributions: Drs Sultana and Kimil share equal credits for first authorship. Drs Jain and Mansuri share equal credits for senior authorship.
Relevant Financial Relationships: None.
Funding/Support: None.
References (18)

- Munjal S, Ferrando SJ, Freyberg Z. Neuropsychiatric aspects of infectious diseases: an update. Crit Care Clin. 2017;33(3):681–712. PubMed CrossRef
- Coughlin SS. Anxiety and depression: linkages with viral diseases. Public Health Rev. 2012;34(2):7. PubMed CrossRef
- Menninger KA. Psychoses associated with influenza, I: general data: statistical analysis. J Am Med Assoc. 1919;72(4):235–241.
- Smith CM, Komisar JR, Mourad A, et al. COVID-19-associated brief psychotic disorder. BMJ Case Rep. 2020;13(8):e236940. PubMed CrossRef
- Boldrini M, Canoll PD, Klein RS. How COVID-19 affects the brain. JAMA Psychiatry. 2021;78(6):682–683. PubMed CrossRef
- Smith CM, Gilbert EB, Riordan PA, et al. COVID-19–associated psychosis: a systematic review of case reports. Gen Hosp Psychiatry. 2021;73:84–100. PubMed CrossRef
- Parra A, Juanes A, Losada CP, et al. Psychotic symptoms in COVID-19 patients: a retrospective descriptive study. Psychiatry Res. 2020;291:113254. PubMed CrossRef
- Brown E, Gray R, Lo Monaco S, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79–87. PubMed CrossRef
- Alba L, Coll C, Sáez S, et al. New-onset psychosis: a case report of brief psychosis related to COVID-19 infection. Psychiatry Res. 2021;301:113975. PubMed CrossRef
- Al-Busaidi S, Al Huseini S, Al-Shehhi R, et al. COVID-19 induced new-onset psychosis: a case report from Oman. Oman Med J. 2021;36(5):e303. PubMed CrossRef
- Desai S, Sheikh B, Belzie L. New-onset psychosis following COVID-19 infection. Cureus. 2021;13(9):e17904. PubMed CrossRef
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. PubMed CrossRef
- Dantzer R. Neuroimmune interactions: from the brain to the immune system and vice versa. Physiol Rev. 2018;98(1):477–504. PubMed CrossRef
- Hébert J, Gros P, Lapointe S, et al. Searching for autoimmune encephalitis: beware of normal CSF. J Neuroimmunol. 2020;345:577285. PubMed CrossRef
- Thomas R, Hernandez MJ, Thomas R. Psychosis after infection with SARS-CoV-2 in an adolescent: a case report. J Am Acad Child Adolesc Psychiatry. 2022;61(7):844–847. PubMed CrossRef
- Zain SM, Muthukanagaraj P, Rahman N. Excited catatonia - a delayed neuropsychiatric complication of COVID-19 infection. Cureus. 2021;13(3):e13891. PubMed CrossRef
- Sun M, Wang D, Jing L, et al. Changes in psychotic-like experiences and related influential factors in technical secondary school and college students during COVID-19. Schizophr Res. 2021;231:3–9. PubMed CrossRef
- Mechanisms of new-onset psychosis during the COVID-19 pandemic: What ignited the fire? AACP website. Accessed September 18, 2022. https://www.aacp.com/article/buy_now/?id=752
Enjoy this premium PDF as part of your membership benefits!