Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2024;26(4):23f03670
Author affiliations are listed at the end of this article.
Have you often wondered how the neuropsychiatric sequelae of traumatic brain injuries (TBIs) can be managed? Have you been skeptical about the benefits of pharmacologic interventions to mitigate impaired attention, concentration, fatigue, aggression, irritability, pain, seizures, and disturbed sleep? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, a 35-year-old woman, sustained a mild TBI (mTBI) in a motor vehicle collision. She complained of neck pain, but no other injuries were apparent when she arrivmbining bupropion with other medications ted at the local emergency department (ED).
On initial evaluation, Ms A had a Glasgow Coma Scale1 score of 14, and she had posttraumatic amnesia (PTA) that lasted for approximately 8 hours. A computed tomography scan of her head and an x-ray of her cervical spine were unremarkable. Ms A was discharged from the ED with a prescription for ibuprofen for her headache and cyclobenzaprine for her neck pain. She was advised to follow up with her primary care provider (PCP).
Ms A stayed at home for 3 days after her ED discharge and then returned to work and to her PhD studies. When Ms A saw her PCP 3 weeks later, she reported severe headaches with photophobia, dizziness, poor sleep, irritability, and difficulty concentrating. In addition, she was having angry outbursts directed toward her husband and 3 children. Although she was taking acetaminophen “around the clock” to relieve the headache, she was not taking other medications. Prior to her TBI, she rarely drank alcohol and did not use tobacco.
According to her spouse, Ms A could expect to receive familial support from her parents and siblings. There was no family history of neurological or psychiatric conditions.
On examination, Ms A’s physical examination was significant for mild muscle tenderness with palpation of the muscles of the neck, with no loss of range of motion. She had no focal neurological deficits. Although Ms A had been diagnosed with an mTBI, her PCP was concerned about her multiple complaints and the severity of her symptoms.
DISCUSSION
Common behavioral and cognitive concerns following TBIs include physical injuries, behavioral problems (eg, aggression and irritability), psychiatric conditions (eg, posttraumatic stress disorder [PTSD], major depressive disorder [MDD]), and cognitive problems (eg, with impairments in memory, attention, and executive function), which can persist and be problematic. While most patients with mTBI fully recover, a minority report continued psychiatric and neurological complaints. The persistence of postconcussive symptoms including headaches, nausea, fatigue, irritability, and cognitive complaints greater than 90 days is nonspecific and may not be directly attributable to the concussion or may be associated with co-occurring or preexisting conditions such as depression, PTSD, insomnia, alcohol or substance use disorders, or pain. Fortunately, several medications can improve attention, concentration, cognition, fatigue, and wakefulness.
PRIMARY CARE TOOLKIT
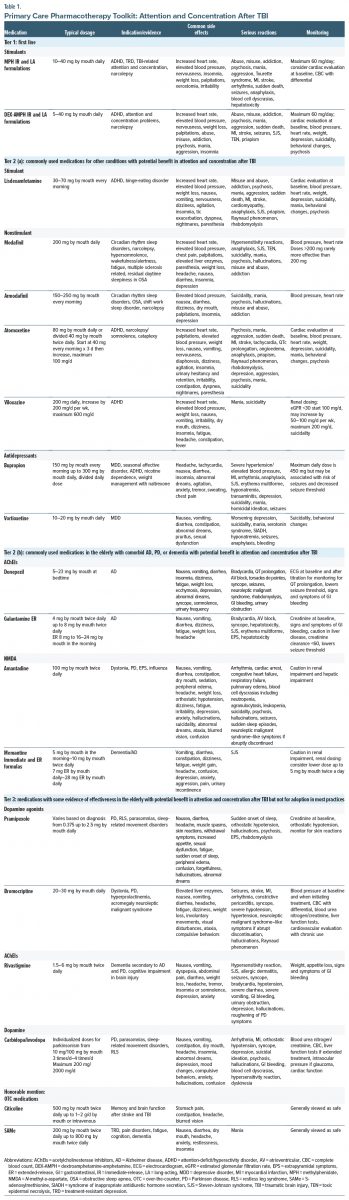
Unfortunately, there are no US Food and Drug Administration (FDA)–approved medications for impaired attention and concentration in patients with a TBI. In the following sections, we will review the non–FDA-approved medications that have evidence for, and that have been trialed in, post-TBI impairments in attention and concentration and categorize them into tiers based on the available evidence for their efficacy (Figure 1, Figure 2, and Table 1); details of their dosing, side effects, and relative contraindications are provided. Tier 1 includes the first-line medications for the treatment of impaired attention and concentration (methylphenidate [MPH] and dextroamphetamine-amphetamine [DEX-AMPH]), Tier 2 (a) lists medications that are commonly used for other conditions but that might enhance attention and concentration following a TBI, and Tier 2 (b) includes medications used in elderly individuals with comorbid Alzheimer disease (AD), Parkinson disease (PD), or dementia that might improve attention and concentration after a TBI. Tier 3 also includes medications that have some evidence in the elderly but that have not been adopted for use in most practices. Honorable mention agents include over-the-counter (OTC) medications (citicoline and S-adenosylmethionine [SAMe]), having some evidence for enhancing attention and concentration post-TBI.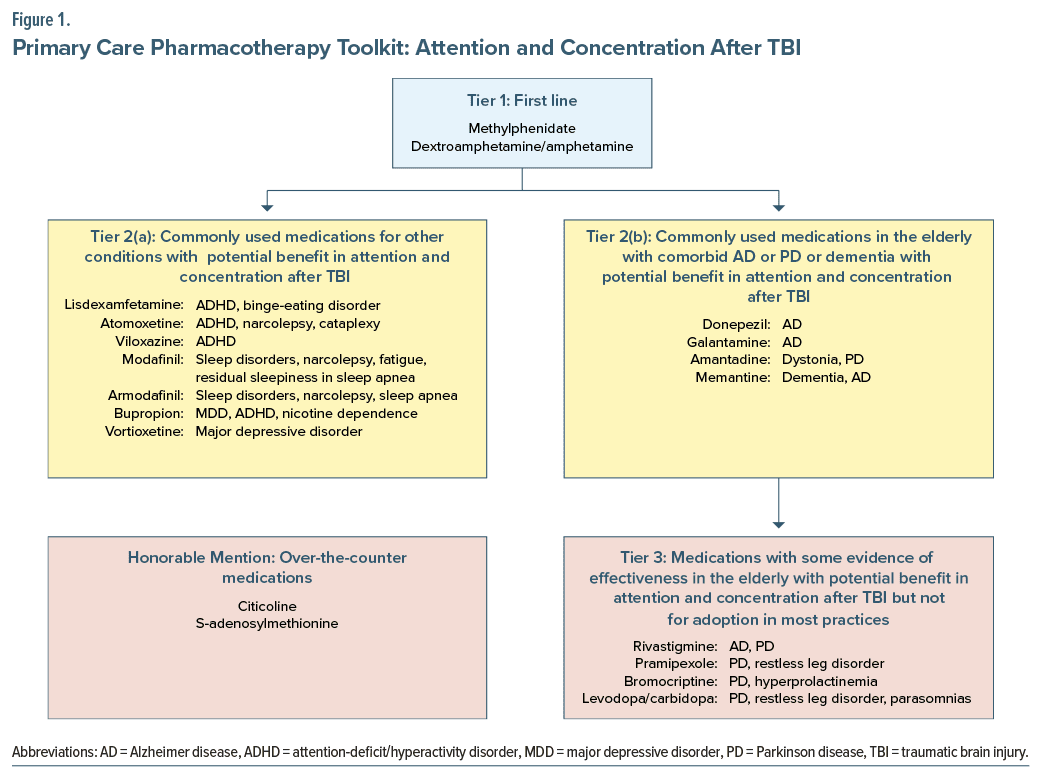
TIER 1 MEDICATIONS: FIRST LINE
Stimulants: Norepinephrine-Dopamine Reuptake Inhibitors
MPH. MPH is a dopamine and norepinephrine reuptake inhibitor with stimulant effects. It is FDA approved for the treatment of attention-deficit/hyperactivity disorder (ADHD), but it can also mitigate manifestations of treatment-resistant depression (TRD), narcolepsy, and TBI-related impairments in attention and concentration ability. MPH is available in both immediate-release (IR) and long-acting (LA) formulations; its usual dose is 10–40 mg daily, which can be divided into twice-daily (morning and early afternoon) dosing based on the half life of its formulations. Although the maximum daily dose is 60 mg/day, doses above 40 mg may produce more side effects without providing a significant improvement in cognition.
The beneficial effects of MPH on cognition occur through its inhibition of extracellular dopamine reuptake by the dopamine transporter in the caudate, putamen, nucleus accumbens, and prefrontal cortex.2 Although MPH also inhibits the reuptake of norepinephrine, the literature supports the notion that the primary mechanism of clinical improvement of cognition is through its modulation of dopamine levels.2 MPH appears to stimulate the cerebral cortex and subcortical structures.3,4 It is metabolized by the liver by carboxylesterase to an inactive metabolite.4 In studies of patients with moderate-to-severe TBI, MPH has improved attention and cognitive processing speed.4 Use of MPH in conjunction with cognitive therapies (eg, speech and language therapy, physical therapy, and occupational therapy) can facilitate recovery.2 Moreover, MPH and placebo have similar safety profiles, and MPH can effectively improve mental fatigue and cognition in patients with TBI.3 A systematic review by Maksimowski and Tampi4 examined the efficacy of stimulants (eg, DEX, MPH, and modafinil) regarding depression and reaction time in individuals post-TBI; most studies found that their beneficial effects began within minutes to hours of administering the first dose of a stimulant. Overall, MPH was well tolerated and had minimal side effects compared with placebo. A review showed that MPH improved attention, fatigue, and depression.5 In addition, a Cochrane review of pharmacotherapy for chronic cognitive impairment post-TBI found that MPH was associated with reduced combativeness and led to improved psychosocial outcomes (with a moderate-to-large effect size).6
Factors to consider before prescribing a stimulant include a history of hypertension, cigarette smoking, obesity, and other cardiac risk factors, as well as a family history of myocardial infarction (MI) in men aged <45 years or women aged <55 years. Medications that increase norepinephrine levels (eg, the serotonin-norepinephrine reuptake inhibitor [SNRI] venlafaxine, which may elevate blood pressure) should be coprescribed with caution. Coadministration with bupropion, a dopamine norepinephrine reuptake inhibitor, is relatively contraindicated for the same reason. In addition, since there is some evidence that stimulants (eg, MPH, DEX AMPH, and bupropion) may lower the seizure threshold, their coprescription in those post-TBI or with a history of seizure should be approached with caution. Caution is also advised when other medications that can lower the seizure threshold (such as tramadol) are used. When prescribing MPH, clinicians should also remember that urine toxicology testing will be negative for amphetamines. Monitoring during the use of stimulants should involve a baseline cardiac assessment, as well as a complete blood count (CBC) with a differential, given the potential cardiac risks and blood cell dyscrasias associated with these medications.
DEX-AMPH. DEX-AMPH is an FDA-approved agent for the treatment of ADHD and narcolepsy; however, it has limited evidence to support its use in enhancing impaired attention and concentration post-TBI. It is available in IR and LA formulations. The maximum dose is 60 mg/day; however, like MPH, doses >40 mg may produce more side effects without improving cognition. DEX promotes the release of dopamine and norepinephrine from storage vesicles in presynaptic neuron terminals and blocks the reuptake of dopamine and norepinephrine from the synaptic cleft.4 Urine toxicology in those taking DEX will be positive for amphetamines. Monitoring of DEX-AMPH is like that for MPH: a cardiac evaluation is appropriate at baseline, as well as a CBC with a differential. Ongoing assessment of vital signs is needed when coadministering other medications that increase norepinephrine, such as venlafaxine and bupropion. Since DEX-AMPH may decrease the seizure threshold, prescription of this medication in patients post-TBI or a history of seizure should be done with caution. Doses >40 mg are prone to elevation of blood pressure and heart rate, without bolstering clinical efficacy.
TIER 2 (A): COMMONLY USED MEDICATIONS FOR OTHER CONDITIONS WITH POTENTIAL BENEFIT IN ATTENTION AND CONCENTRATION AFTER TBI
Lisdexamfetamine
Lisdexamfetamine is a prodrug that is hydrolyzed from the parent compound to lysine and d-amphetamine.7 It is an FDA-approved stimulant for the treatment of ADHD and binge-eating disorder. In a small, randomized, double-blind placebo-controlled crossover trial assessing the effectiveness of lisdexamfetamine for attentional deficits associated with moderate-to-severe TBI, improvements in measures of sustained attention, working memory, and executive functioning were identified8; overall, the medication was well tolerated.
Nonamphetamine Stimulants
Atomoxetine. Atomoxetine, an FDA-approved SNRI for the treatment of ADHD, has preclinical evidence of potential benefit for attention in rodent models of hypoxic anoxic brain injury; however, clinical trials have not shown significant improvement in attention post-TBI.9,10 Moreover, a double-blind randomized controlled trial (RCT) that investigated atomoxetine (40 mg twice daily versus placebo) on several scales of attention10 revealed that it was well tolerated but did not meaningfully improve scores on measures of attention. Given the lack of evidence for improving attention after TBI, other stimulant medications should be trialed before using atomoxetine unless there is concern for substance misuse or abuse.
Viloxazine. Like atomoxetine, viloxazine is an FDA approved SNRI for the treatment of ADHD. Like atomoxetine, it has a lower potential for misuse and abuse than stimulant medications; however, there is no literature to support its use following TBI.
Modafinil/armodafinil. Modafinil and its R-enantiomer armodafinil are nonamphetamine stimulants. Each has slightly different pharmacokinetics; armodafinil maintains a higher plasma concentration 6–14 hours after administration than an equivalent dose of modafinil.11 Armodafinil’s duration of promoting wakefulness in healthy adults is longer than that of modafinil.11 Modafinil and armodafinil are FDA approved for use in narcolepsy and shift-work sleep disorder and have been noted to improve wakefulness/alertness and multiple sclerosis–related fatigue, as well as residual daytime sleepiness in obstructive sleep apnea. While the exact mechanism of action (MOA) of modafinil and armodafinil is unknown, there appears to be agreement that they differ from classical psychostimulants.12 A review of modafinil for improvement of patient outcomes following TBI investigated the research of the MOA of modafinil and found that modafinil does not involve catecholamine (eg, dopamine and norepinephrine) release or reuptake and that it appears to decrease γ-aminobutyric acid (GABA) and increase serotonin and glutamine levels in preclinical models.11 However, researchers found that modafinil can indirectly affect extracellular levels of serotonin, glutamine, histamine, orexin, and GABA.12
Antidepressants
Bupropion. Bupropion has a structure that is like amphetamine stimulants, with a phenylethylamine-based skeleton. Its MOA is related to it being a nonselective inhibitor of the dopamine and norepinephrine transporters and an antagonist at nicotinic acetylcholine receptors. Doses above 300 mg may increase the risk of seizures. In patients post-TBI, past seizures may pose a significant contraindication to a bupropion trial, given the risk of inducing a seizure. Combining bupropion with other medications that lower the seizure threshold, such as tramadol in combination with an SSRI, may further increase the risk of seizures. A Cochrane review of the use of bupropion for ADHD in adults found low quality evidence for bupropion decreasing the severity of ADHD symptoms.13 Although there may be some theoretical benefit to using bupropion in individuals post-TBI given its possible benefit in adults with ADHD, there has been no mention of its impact on attention or concentration ability.14 Given its lack of evidence in TBI, its side effect profile, and the risk for a decrease in the seizure threshold, the risks of its use may outweigh its theoretical benefits. However, the misuse and abuse potential of bupropion is lower than that of the classical stimulants detailed previously, while other factors (eg, weight loss, comorbid nicotine use disorders, a lack of prior seizures, or mTBI) may be reasons to consider bupropion with caution and at doses ≤300 mg total/day.
Vortioxetine. Vortioxetine, an FDA-approved agent for the treatment of MDD, exhibits a unique MOA that includes increases in serotonergic, noradrenergic, dopaminergic, cholinergic, histaminergic, and glutamatergic neurotransmission.15 Vortioxetine inhibits serotonin reuptake, antagonizes 5-hydroxytryptamine 3 receptors, and facilitates serotonin 5-hydroxytryptamine 1A receptors. In addition, there is preclinical and clinical evidence for vortioxetine in cognitive function in individuals with mild cognitive impairment.16,17 There is also preclinical evidence that vortioxetine might mitigate neuronal damage in rats exposed to focal cerebral ischemia reperfusion.18 A case report of vortioxetine on depression secondary to hypoxic brain injury with residual cognitive deficits revealed a marked improvement in mood, motivation, and engagement; however, there was no change in cognitive deficits after 3 months of treatment.19 There have been no studies that have evaluated vortioxetine in individuals with TBI. Given the relative tolerability of vortioxetine, in patients with TBI, depression after TBI, and cognitive dysfunction, a trial of vortioxetine may be reasonable in those with comorbid MDD.
TIER 2 (B): COMMONLY USED MEDICATIONS IN THE ELDERLY WITH COMORBID AD, PD, OR DEMENTIA WITH POTENTIAL BENEFIT IN ATTENTION AND CONCENTRATION AFTER TBI
Acetylcholinesterase Inhibitors
Acetylcholinesterase inhibitors (AChEIs) are frequently prescribed for the treatment of dementia due to AD. Use of these medications leads to improvement in cholinergic deficiency in the cortex and basal forebrain, which may lead to improvement in some aspects of cognition.12
Donepezil. Donepezil is the most prescribed AChEI that is FDA approved for the treatment of dementia associated with AD. The typical dose is 5–10 mg daily. There is some evidence showing that donepezil improves cognitive function and communication in patients after strokes as well as TBI.12 In a small, randomized trial, donepezil showed some benefit in improving short-term memory and sustained attention in individuals after moderate-to-severe TBI.12 Additionally, the beneficial effects of donepezil persisted up to 14 weeks after treatment was discontinued. Two additional trials demonstrated that donepezil may improve communication and cognition recovery after stroke.12 Donepezil may lower the seizure threshold, so the drug should be prescribed with caution when other medications that lower the seizure threshold (such as bupropion or stimulants) are used.
Galantamine. Galantamine is a reversible AChEI that is FDA approved for the treatment of mild-to-moderate dementia associated with AD. A recent review of AChEIs to enhance recovery from TBI found one study on galantamine.20 It was not found to be effective in improving behavioral or cognitive function. Overall, Florentino and associates20 found that the literature on the use of AChEIs (including donepezil, rivastigmine, and galantamine) for the treatment of cognitive impairments in individuals within 90 days after TBI suggested a potential benefit; however, the literature was limited by small sample sizes and concern for methodological quality.
N-methyl-D-aspartate receptor antagonists. The N-methyl-D-aspartate (NMDA) receptor is the main receptor of glutamate, which is the primary excitatory neurotransmitter in the brain. NMDA receptor antagonists include amantadine and memantine, as well as dextromethorphan, dextrorphan, ketamine, and magnesium.21 Dextromethorphan is used in combination with quinidine for the treatment of pathological laughter and crying associated with TBI. It has also been used in combination with bupropion for rapid treatment of MDD. Ketamine has evidence in subanesthetic doses for TRD, suicidality, PTSD, and pain disorders. Magnesium has evidence in headache prevention, muscle relaxation, and constipation. Amantadine and memantine bind within the channel of the NMDA receptor complex at the phencyclidine (PCP) binding site.21
Amantadine. Amantadine was initially used for the prophylaxis and treatment of influenza A and was later found to be beneficial in the treatment of PD due to its dopaminergic properties.21 Amantadine is used for dystonia, PD, extrapyramidal symptoms, and influenza. Amantadine’s MOA includes both presynaptic and postsynaptic effects. Amantadine facilitates presynaptic dopamine release from neurons and delays its reuptake, leading to an increase in dopamine concentration in the synaptic cleft.21 It is also thought to have NMDA antagonist activity, which may be neuroprotective.21 Studies of amantadine in TBI suggest a potential benefit for attention and cognitive functioning. Improvements noted with amantadine may include decreased fatigue, distractibility, increased arousal level, attention and concentration, sequencing skills, and processing time.21 In addition, amantadine was found to have marked benefits in global outcome.6 A review found that amantadine was the pharmacologic agent with the most support for improvement in cognitive impairment after TBI.12
Memantine. Memantine is an NMDA receptor antagonist that is typically dosed much lower than amantadine, given its higher affinity for the binding site. Memantine is FDA approved for the treatment of dementia associated with AD. There is more research on memantine in slowing cognitive decline or improving cognition compared to amantadine.21 However, there is limited evidence with respect to the use of memantine following TBI.
There is both preclinical and clinical evidence of the potential benefit of amantadine and memantine in patients after TBI and stroke. Both are commonly used off-label in patients post-TBI in the acute rehabilitation setting.21 A review examined the potential benefit of these medications on neuroplasticity, functional recovery, fatigue, behavior, agitation, cognition, and other symptoms.21 Most of the research has been limited to small trials with a concern for bias. Although most of the studies have been positive, their effect sizes were small.21
TIER 3: MEDICATIONS WITH SOME EVIDENCE OF EFFECTIVENESS IN THE ELDERLY WITH POTENTIAL BENEFIT IN ATTENTION AND CONCENTRATION AFTER TBI BUT NOT FOR ADOPTION IN MOST PRACTICES
Acetylcholinesterase Inhibitors
Rivastigmine. Rivastigmine is an AChEI that is FDA approved for dementia secondary to AD and PD, and it has limited evidence for use in cognitive impairmen t in brain injury. A Cochrane review revealed rivastigmine was better than placebo on one primary measure of a single cognitive outcome in a secondary analysis in participants with more severe memory impairment.6 In a review, Kakehi and Thompkins12 reported that rivastigmine did not show improvement in attention or memory over placebo in those with TBI. They theorized that rivastigmine may benefit patients with TBI and more severe memory impairment.
Dopamine Agonists
Ropinirole and pramipexole. Ropinirole and pramipexole are nonergot direct dopamine agonists that are highly selective for dopamine receptors.22 Ropinirole has high affinity for D2 receptors, whereas pramipexole has a 7- fold higher affinity for D3 receptors.22 However, there is no literature to support the use of ropinirole in TBI. Pramipexole is FDA approved for the treatment of PD and moderate-to-severe primary restless leg syndrome (RLS). It is used off-label for sleep-related eating disorder and rapid eye movement sleep behavior disorders. Additionally, there is some evidence to support the use of pramipexole in patients with TRD in unipolar and bipolar depression.23 Pramipexole is thought to reduce anhedonia and amotivation that are thought to be impacted by the dopamine system.23 D3 receptors are found in high concentrations in mesolimbic areas implicated in mental processes related to emotion and mood.24 Although the effective dosage and titration of pramipexole in TRD augmentation have not been clearly defined, an overall response rate of 62.5% and remission of 48.1% with pramipexole augmentation have been noted.24 A systematic review of pramipexole in TRD revealed a mean maximum pramipexole dose between 0.69 and 2.18 mg/day.24 There is preclinical evidence that pramipexole may protect against TBI-induced blood brain barrier dysfunction as well as inhibit neuronal cell death.25,26 Additional preclinical studies of pramipexole in rats with global ischemia-reperfusion injuries demonstrated improved neurological function; it was thought to produce neuroprotective effects on neurons in the hippocampus.27 However, there have been no preclinical or clinical studies on the use of pramipexole in attention and concentration after TBI. Given the lack of significant evidence, it is unclear if pramipexole and ropinirole are useful in patients after TBI, except in the setting of potential sleep-related movement disorders, such as RLS or TRD.
Bromocriptine. Bromocriptine is a selective D2 agonist that stimulates dopamine receptors; it is FDA approved for the treatment of PD and acromegaly and has been shown to inhibit the secretion of prolactin. It has been used to treat dystonia and as an adjunct for glycemic control in type 2 diabetes mellitus, as well as in neuroleptic malignant syndrome. Given its role as a dopamine agonist, bromocriptine may enhance working memory.12 A retrospective review of 5 patients treated with bromocriptine after TBI showed improvement from a vegetative state to a minimally conscious state.12 Over 12 months of treatment, the patients improved steadily. A subsequent double-blind placebo-controlled crossover trial of 12 patients with moderate-to-severe TBI and attention deficits treated with bromocriptine found no effect on attention.12 Another prospective cohort study of 36 patients with TBI and a minimally conscious state showed an improvement in arousal, aphasia, and cognitive function.12 However, a review of the literature did not support the routine use of bromocriptine after TBI.12
Dopamine
Levodopa/carbidopa. Levodopa is a presynaptic dopamine precursor that is decarboxylated to dopamine.20 It is usually given with carbidopa, a peripherally acting decarboxylase inhibitor.20 Levodopa is FDA approved for the treatment of PD. Additionally, there is evidence for use in parasomnias and sleep-related movement disorders such as RLS. There are preclinical studies evaluating the potential benefit of levodopa in animal models of learning and memory in ischemia reperfusion.28,29 However, significant evidence to support the use of levodopa/carbidopa for patients with TBI is lacking.
HONORABLE MENTION: OTC MEDICATIONS
Citicoline
Citicoline is the generic name for cytidine 5’- diphosphocholine (CDP-choline). Citicoline has evidence for potential benefit in memory and brain function after stroke and TBI. It is an OTC supplement that is generally viewed as safe. Limitations may be that OTC medications are unregulated, and the product may vary widely in price and quality. Citicoline is a precursor involved in the pathway of choline metabolism of cerebral phospholipids (including phosphatidylcholine and acetylcholine) that has preclinical and clinical evidence of potential benefit in TBI.30 Citicoline has improved brain energy metabolism and modulated the levels of acetylcholine, dopamine, and norepinephrine.30 Citicoline treatment in patients with moderate-to-severe TBI has accelerated cerebral edema reabsorption and recovery, resulting in shorter hospital length of stay with a higher independence rate in treated patients.30 Citicoline has been shown to be safe, and it may be beneficial in the management of acute stroke (whether ischemic or hemorrhagic) and cognitive disorders associated with TBI.30
SAMe
SAMe is synthesized from the metabolic reaction that combines adenosine triphosphate and methionine.31 SAMe acts as a methyl donor in over 100 reactions that regulate metabolic pathways (including methylation of phospholipids, amino acids, and the neurotransmitters dopamine, serotonin, and norepinephrine).31 The dosage prescribed has varied for different indications and in different studies, so that determining the appropriate dose is difficult. The typical dose used in TRD is 400 mg by mouth twice daily up to 800 mg by mouth twice daily, while treatment of pain has used 3- times-daily dosing at various doses. A recent review by Schieffler and Matta31 postulated that the involvement of SAMe in these monoamine pathways may be key to their potential improvement in both mood and cognition in TBI. Numerous case reports, preclinical and clinical trials, and systematic reviews have highlighted the potential benefit of SAMe in the treatment of depression, TRD, pain, fatigue, attention, and cognition.31 Individuals with TBI treated with SAMe showed a statistically significant reduction in clinical scores compared to those treated with placebo.31 Given SAMe’s role in cognition and memory, there is a potential that SAMe may improve cognitive complaints in individuals after TBI.31
WHICH MEDICATIONS CAN REDUCE IMPULSIVITY, AGGRESSION, AND AGITATION AFTER TBI?
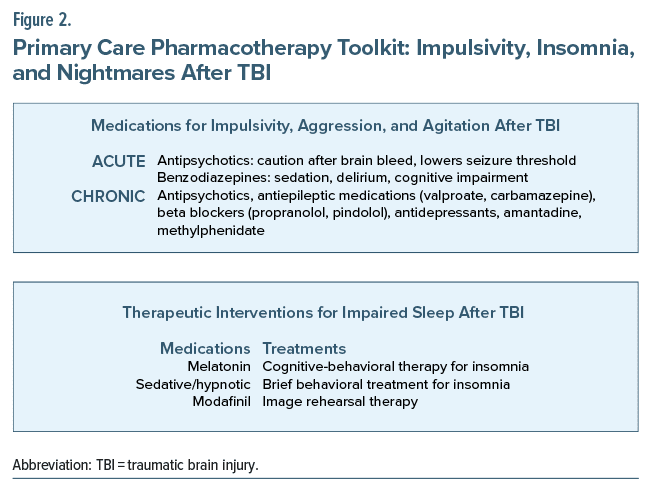
Several neuropsychiatric manifestations (eg, irritability, agitation, and aggression) can be seen in the immediate aftermath of a TBI as well as months later (Figure 2). Shortly after sustaining a head injury, patients are typically treated in hospital settings. During that phase, aggression is often treated with the short term use of antipsychotics and benzodiazepines. Although antipsychotics can reduce agitation and aggression, they can increase the duration of PTA.32 Benzodiazepines, such as lorazepam, can also be administered acutely, but cautious prescribing is appropriate, as they can be associated with undue sedation and impaired cognition.
Months and years after the injury, patients may develop a “short fuse” and become easily agitated, verbally aggressive, threatening, or violent. The pharmacotherapy of impulsivity, agitation, and aggression in the post–acute stage often includes antipsychotics,32–34 antiepileptic drugs (such as valproate and carbamazepine),32–36 lithium,33 buspirone,33 antidepressants,33 beta-blockers33,34 (such as propranolol or pindolol), amantadine,37 and MPH.32–34 In a meta-analysis of pharmacotherapies used for cognitive and behavioral impairment, MPH was associated with reductions in anger and aggression and enhanced psychosocial function, whereas amantadine improved aberrant behavioral symptoms.38
THERAPEUTIC INTERVENTIONS FOR IMPAIRED SLEEP AFTER TBI
Problems with sleeping are common following a TBI. Roughly half of patients who have sustained a TBI develop some sleep disturbance, and nearly half (46%) are diagnosed with a sleep disorder, of which one-fourth have sleep apnea (compared to 2% in the general population), and nearly half (11%–49%) have hypersomnia.39 As assessed by polysomnography or actigraphy, patients post-TBI demonstrated less efficient sleep and total sleep time and more time awake after sleep onset, as compared with non-TBI controls.40 Sleep problems following a TBI are often treated with melatonin. Two small RCTs reported improved subjective sleep quality,41 daytime alertness,42 and executive functioning43 in association with melatonin administration. A double-blind, randomized, placebo controlled crossover trial studying 33 outpatients who had sustained a TBI (ranging from mild to severe) with self-reported sleep disturbance found that compared to placebo, prolonged-release melatonin (2 mg) was associated with improved sleep quality (P ≤ .0001), but it had no effect on sleep-onset latency (P = .23).41 Additionally, melatonin was associated with improved sleep efficiency as well as decreased anxiety and fatigue (P ≤ .05 for both). However, melatonin had no significant effect on daytime sleepiness (Epworth Sleepiness Scale, P = .15). A systematic review and meta analysis of the effect of melatonin on sleep problems following TBI found that it significantly improved behavioral outcomes without causing serious adverse events.44,45
A bevy of sedative-hypnotics have been used by clinicians to treat post-TBI insomnia. However, the data from controlled studies are sparse. Therefore, clinicians should “start low and go slow” and carefully weigh the sleep benefits of the medication with the potential for cognitive impairment. Modafinil, studied for EDS following TBI, has been associated with improvement in EDS and the ability to remain awake, but without improvement in posttraumatic fatigue.46,47
WHAT NONPHARMACOLOGIC STRATEGIES CAN IMPROVE IMPAIRED ATTENTION, BEHAVIORS, COGNITION, AND SLEEP?
The Cognitive Task Force of the American College of Rehabilitation Medicine48 reviewed 112 studies of cognitive rehabilitation interventions and conducted a follow-up review several years later49 and concluded that cognitive rehabilitation in those post–acute TBI48,49 was of greater benefit than conventional rehabilitation and that it was the best treatment for people with neurocognitive impairment and functional limitations. The Task Force also found substantial evidence for social communication deficits after TBI,48,49 attention training (graded exercises to stimulate attention),48,49 and metacognitive strategies (eg, feedback, self-monitoring, self-regulation, and strategy use) to promote generalization of real-world tasks and to reduce functional disability.48,49
When an adapted 8-session cognitive-behavioral therapy (CBT) protocol was used in 24 outpatients following a TBI, investigators found improvements in sleep quality (Pittsburgh Sleep Quality Index [PSQI]), daytime fatigue (Brief Fatigue Inventory), and depression.50 Gains were maintained for 2 months after therapy cessation.50 A systematic review of the literature on CBT and sleep disturbances analyzed 12 trials that involved 476 patients following a TBI and found significant improvements in self-reported sleep quality after CBT (PSQI, P < .001; ISI, P = .028).51
CBT for insomnia (CBTi) (a form of CBT that targets sleep-incompatible thoughts, beliefs, and behaviors over 6–8 weeks of treatment)52 includes stimulus control (eg, limiting the bed for sleeping and intimate relations, waking up at the same time every day, leaving the bedroom, and going to a dark room until they are sleepy); sleep restriction (eg, avoiding napping during the day and having a fixed wake-up time); sleep hygiene (eg, avoiding stressful situations before going to bed, not eating or smoking at least 3 hours before going to bed, not using alcoholic beverages and caffeine 4–6 hours before going to bed, and avoiding bright lights, TV, and electronic devices before going to bed); using progressive muscle relaxation (eg, contracting different muscle groups and then relaxing them, one by one, all over the body for 1–2 seconds repeatedly during the day); visualizing peaceful scenes or oneself breathing quietly, falling asleep, and having a good night’s sleep; and cognitive therapy (eg, changing negative thoughts about sleep to more realistic ones, avoiding blaming negative events on poor sleep, establishing real expectations related to insomnia and the need for sleep). Two meta-analyses of computerized CBTi in those without PTSD showed mild to-moderate improvements in insomnia severity, sleep duration, and sleep efficiency. Despite improved sleep quality, nearly 50% continued to experience residual insomnia.52
Other promising behavior therapies for insomnia in PTSD52 include web-based individual or group therapy, telehealth, or mobile applications. Abbreviated treatments that emphasize behavioral components of CBTi (ie, stimulus control and sleep restriction) rather than the cognitive restructuring of dysfunctional beliefs about sleep have been developed. Brief behavioral treatment for insomnia has been shown to be efficacious in military and civilian cohorts, showing clinically significant improvements in insomnia compared with use of educational brochures that promote sleep hygiene.
In patients with comorbid PTSD and TBI, nightmares occur in about 70%.52 Unfortunately, nightmares have been implicated in suicide, particularly in US service members who have returned from combat zones. Cross sectional research has suggested that the number of nightmares experienced may predict repeat suicide attempts better than the length of time over which nightmares occurred. The effect of nightmares on suicide has been independent of several confounders (eg, age, sex, and presence of anxiety and depressive symptoms). For those with PTSD-related nightmares, image rehearsal therapy (IRT)52 has been used. It has several components: closing the eyes and picturing the nightmare, developing a new preferred dream to have instead of the nightmare, altering the plot of the old dream or creating a new dream that contains an acceptable storyline, including each sensory modality while rehearsing the dream, and rehearsing the dream for 15–20 minutes each night. The Standards of Practice Committee of the American Academy of Sleep Medicine gave a level A rating to IRT for nightmare disorder in patients with PTSD. A meta-analysis found that IRT improves sleep, reduces nightmare frequency and intensity, and improves sleep quality. Treatment effects of IRT were sustained for 6–12 months.52
Insomnia and nightmares often co-occur; therefore, IRT and CBTi can be used in tandem.52 Thus, IRT and CBTi are associated with greater improvement in sleep quality than with IRT alone. However, inclusion of CBTi did not show incremental benefits for nightmares or PTSD symptoms after a single therapy with IRT. The long-term efficacy of combined IRT and CBTi remains unstudied and unknown. In addition, combining a targeted sleep intervention, such as IRT or CBTi, with trauma-focused CBT can be problematic. Thus, an intense prolonged exposure protocol may hinder adherence to other behavioral interventions. Also, PTSD therapy may alleviate insomnia and nightmares without the need for additional interventions. One possible approach is to weigh the relative contribution of sleep disturbances and PTSD symptoms and add IRT only when residual insomnia and nightmares persist after CBT for PTSD.52
WHAT HAPPENED TO MS A?
Ms A was in a great deal of distress because of her physical symptoms and not feeling “like herself”; although she had many work, school, and family demands, she agreed to treatment for her mTBI. She was using acetaminophen around the clock for her headache; it was ineffective and placed her at risk for rebound headache. Headache and poor sleep were her primary concerns, so her PCP started her on a low dose of propranolol. This medication was chosen to avoid use of sedating medications and because Ms A and her spouse reported irritability. She was also started on melatonin to address her insomnia.
The PCP provided information to Ms A and her spouse; he let her know that while complete rest was not recommended, she should titrate her activity level (both physical and mental) to her symptoms. The PCP provided documentation for Ms A so that she could have accommodations at work and school, along with a referral to physical therapy to help increase her activity and address her dizziness.
Ms A was seen by a physical therapist, who did not perform a Buffalo Concussion Treadmill test at the initial visit, since Ms A had been started on propranolol; however, physical therapy treated both her cervicalgia and her benign paroxysmal vertigo by means of vestibular rehabilitation and canalith repositioning. At her next visit, Ms A reported that her sleep, headache, dizziness, and mood had improved, as well as less irritability. Ms A stated that she was still having some neck discomfort, although it had improved with the physical therapy, so she was referred for acupuncture (for neck pain and insomnia).
Approximately 2 weeks later, her dizziness had resolved, and her headaches had improved significantly (down to 1–3 days per week from 7 days per week), but she reported that while her memory seemed to have improved somewhat, her concentration was still extremely poor and noticeable even on nights where she was able to get at least 5–6 hours of sleep. Her PCP added MPH in the hope that it would improve her concentration.
At subsequent visits, Ms A reported that her concentration had significantly improved with the medication, but she requested discontinuation of propranolol, as she was gradually increasing her activity level and was now impeded by the administration of a beta-blocker. Her PCP weaned her off propranolol, and at follow-up, she reported only mild headaches, and she was no longer irritable.
Within a year, Ms A asked to be taken off MPH, as her concentration had improved significantly, and she preferred to be off controlled substances. Ms A still had occasional headaches, but these were no more than she had experienced before her TBI, and she was treated with OTC pain relievers. As a result, Ms A was satisfied that she had fully recovered from her TBI, and she was fully functional at work, home, and school.
CONCLUSION
Cognitive complaints, including difficulties with attention, concentration, and memory, are common in patients after TBI. Many medications including stimulants and those detailed above have been studied in the treatment of cognition after TBI. When deciding which medications to prescribe, it is important to review the evidence, potential risks, benefits, and adverse effects, as well as the specific underlying comorbid illnesses (eg, TBI in a patient with PD after a fall). The medication studied most often and with data that supports its use in cognitive impairment after TBI is amantadine. Other medications that have shown benefits with more limited evidence include MPH and modafinil. Given the potential decrease in seizure threshold, many medications that have shown benefit in attention and concentration should be used with caution and may be relatively contraindicated in patients with a history of a seizure disorder or a seizure after TBI. All stimulants and even nonstimulant medications, such as bupropion, can have adverse reactions (such as MI, cerebrovascular accidents, or sudden death), so a detailed cardiac history and family cardiac history should be performed, and individual risk factors should be assessed in each patient (including smoking history, weight, and other risk factors for MI). Additionally, some medications may cause depression, suicidality, mania, or psychosis and be misused or abused and lead to dependence. For medications that can lead to mania, an evaluation for underlying bipolar diathesis should be performed.
Article Information
Published Online: July 16, 2024. https://doi.org/10.4088/PCC.23f03670
© 2024 Physicians Postgraduate Press, Inc.
Submitted: November 3, 2023; accepted March 6, 2024.
To Cite: Matta SE, LaCroix C, Tanev K, et al. Pharmacologic management of the sequelae of traumatic brain injuries. Prim Care Companion CNS Disord. 2024;26(4):23f03670.
Author Affiliations: Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts (Matta, Tanev, Stern); Harvard Medical School, Boston, Massachusetts (Matta, Tanev, Stern); Department of Psychiatry, Department of Physical Medicine and Rehabilitation, Uniform Services University of the Health Sciences, Bethesda, Maryland (LaCroix).
Corresponding Author: Theodore A. Stern, MD, Harvard Medical School, Massachusetts General Hospital, 55 Fruit St, WRN 606, Boston, MA 02114 ([email protected]).
Drs Matta, LaCroix, and Tanev are co-first authors. Dr Stern is the senior author.
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Cognitive complaints including difficulties with attention, concentration, and memory are common in patients after traumatic brain injury (TBI).
- Many medications, including stimulants, nonamphetamine stimulants, antidepressants, dopamine agonists, acetylcholinesterase inhibitors, N-methyl-D-aspartate antagonists, and dopaminergic precursors, have been studied in the treatment of cognition after TBI.
- In addition to the use of pharmacologic agents, cognitive rehabilitation, and cognitive-behavioral therapy for insomnia can help mitigate disrupted sleep and insomnia associated with posttraumatic stress disorder and TBI.
- Medical monitoring for pharmacologic agents should assess blood pressure, heart rate, weight, rhabdomyolysis, myocardial infarction, anxiety, agitation, behavioral changes, depression, suicidal ideation, mania, and psychosis.
References (52)

- Teasdale G, Jennet B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. PubMed CrossRef
- Levin H, Troyanskaya M, Petrie J, et al. Methylphenidate treatment of cognitive dysfunction in adults after mild to moderate traumatic brain injury: rationale, efficacy, and neural mechanisms. Front Neurol. 2019;10:925. PubMed
- Zhang WT, Wang YF. Efficacy of methylphenidate for the treatment of mental sequelae after traumatic brain injury. Medicine (Baltimore). 2017;96(25):e6960. PubMed CrossRef
- Maksimowski MB, Tampi RR. Efficacy of stimulants for psychiatric symptoms in individuals with traumatic brain injury. Ann Clin Psychiatry. 2016;28(3):156–166. PubMed
- Iaccarino MA, Philpotts LL, Zafonte R, et al. Stimulant use in the management of mild traumatic brain injury: a qualitative literature review. J Atten Disord. 2020;24(2):309–317. PubMed CrossRef
- Dougall D, Poole N, Agrawal N. Pharmacotherapy for chronic cognitive impairment in traumatic brain injury. Cochrane Database Syst Rev. 2015;2015:CD009221. PubMed CrossRef
- Goodman DW. Lisdexamfetamine dimesylate (vyvanse), a prodrug stimulant for attention-deficit/hyperactivity disorder. P T. 2010;35(5):273–276, 282–287. PubMed
- Tramontana MG, Cowan RL, Zald D, et al. Traumatic brain injury-related attention deficits: treatment outcomes with lisdexamfetamine dimesylate (Vyvanse). Brain Inj. 2014;28(11):1461–1472. PubMed CrossRef
- Ripley DL, Morey CE, Gerber D, et al. Atomoxetine for attention deficits following traumatic brain injury: results from a randomized controlled trial. Brain Inj. 2014;28(12):1514–1522. PubMed CrossRef
- Toshimitsu M, Kamei Y, Ichinose M, et al. Atomoxetine, a selective norepinephrine reuptake inhibitor, improves short-term histological outcomes after hypoxic-ischemic brain injury in the neonatal male rat. Int J Dev Neurosci. 2018;70:34–45. PubMed CrossRef
- Borghol A, Aucoin M, Onor I, et al. Modafinil for the improvement of patient outcomes following traumatic brain injury. Innov Clin Neurosci. 2018;15(3–4):17–23.
- Kakehi S, Tompkins DM. A review of pharmacologic neurostimulant use during rehabilitation and recovery after brain injury. Ann Pharmacother. 2021;55(10):1254–1266. PubMed CrossRef
- Verbeeck W, Bekkering GE, Van den Noortgate W, et al. Bupropion for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2017;10(10):CD009504. PubMed CrossRef
- Teng CJ, Bhalerao S, Lee Z, et al. The use of bupropion in the treatment of restlessness after a traumatic brain injury. Brain Inj. 2001;15(5):463–467. PubMed CrossRef
- Sanchez C, Asin KE, Artigas F. Vortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical data. Pharmacol Ther. 2015;145:43–57. PubMed CrossRef
- Frampton JE. Vortioxetine: a review in cognitive dysfunction in depression. Drugs. 2016;76(17):1675–1682. PubMed CrossRef
- Bishop MM, Fixen DR, Linnebur SA, et al. Cognitive effects of vortioxetine in older adults: a systematic review. Ther Adv Psychopharmacol. 2021;11:20451253211026796. PubMed CrossRef
- Emam AM, Saad MA, Ahmed NA, et al. Vortioxetine mitigates neuronal damage by restricting PERK/eIF2α/ATF4/CHOP signaling pathway in rats subjected to focal cerebral ischemia-reperfusion. Life Sci. 2021;283:119865. PubMed CrossRef
- Ahsan SM, Ahsan SD, Khalid O, et al. Usefulness of vortioxetine noted in depression secondary to hypoxic brain injury and residual cognitive deficits. Ther Adv Psychopharmacol. 2020;10:2045125320943399. PubMed CrossRef
- Florentino SA, Bawany MH, Ma HM. Acetylcholinesterase inhibitors to enhance recovery from traumatic brain injury: a comprehensive review and case series. Brain Inj. 2022;36(4):441–454. PubMed CrossRef
- Ma HM, Zafonte RD. Amantadine and memantine: a comprehensive review for acquired brain injury. Brain Inj. 2020;34(3):299–315. PubMed CrossRef
- Zafonte RD, Lexell J, Cullen N. Possible applications for dopaminergic agents following traumatic brain injury: part 2. J Head Trauma Rehabil. 2001;16(1):112–116. PubMed CrossRef
- Fawcett J, Rush AJ, Vukelich J, et al. Clinical experience with high-dosage pramipexole in patients with treatment-resistant depressive episodes in unipolar and bipolar depression. Am J Psychiatry. 2016;173(2):107–111. PubMed
- Tundo A, Betro S, de Filippis R, et al. Pramipexole augmentation for treatment resistant unipolar and bipolar depression in the real world: a systematic review and meta-analysis. Life (Basel). 2023;13(4):1043. PubMed
- Huang J, Lan H, Xie C, et al. Pramipexole protects against traumatic brain injury induced blood-brain barrier (BBB) dysfunction. Neurotox Res. 2022;40(4):1020–1028. PubMed CrossRef
- Liu C, Sun X, Cai Y, et al. Pramipexole alleviates traumatic brain injury in rats through inhibiting necroptosis. Neurosci Lett. 2022;791:136911. PubMed CrossRef
- Kang X, Liu L, Wang W, et al. Effects of different doses of dopamine receptor agonist pramipexole on neurobehaviors and changes of mitochondrial membrane potentials in rats with global cerebral ischemia-reperfusion injury. J Stroke Cerebrovasc Dis. 2023;32(7):107142. PubMed CrossRef
- Wang W, Liu L, Jiang P, et al. Levodopa improves learning and memory ability on global cerebral ischemia-reperfusion injured rats in the Morris water maze test. Neurosci Lett. 2017;636:233–240. PubMed CrossRef
- de Oliveira PA, Ben J, Matheus FC, et al. Moderate traumatic brain injury increases the vulnerability to neurotoxicity induced by systemic administration of 6-hydroxydopamine in mice. Brain Res. 2017;1663:78–86. PubMed CrossRef
- Secades JJ. Role of citicoline in the management of traumatic brain injury. Pharmaceuticals (Basel). 2021;14(5):410. PubMed CrossRef
- Schieffler DA, Matta SE. Evidence to support the use of S-adenosylmethionine for treatment of post-concussive sequelae in the military. Mil Med. 2022;187(9–10):e1182–e1192. PubMed CrossRef
- Williamson D, Frenette AJ, Burry LD, et al. Pharmacological interventions for agitated behaviours in patients with traumatic brain injury: a systematic review. BMJ Open. 2019;9(7):e029604. PubMed CrossRef
- Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury–a state-of-the-art review. J Rehabil Res Dev. 2009;46(6):851–879. PubMed CrossRef
- Hicks AJ, Clay FJ, Hopwood M, et al. The efficacy and harms of pharmacological interventions for aggression after traumatic brain injury-systematic review. Front Neurol. 2019;10:1169. PubMed CrossRef
- Chatham-Showalter PE. Carbamazepine for combativeness in acute traumatic brain injury. J Neuropsychiatry Clin Neurosci. 1996 Winter;8(1):96–99. PubMed CrossRef
- Plantier D, Luauté J, SOFMER group. Drugs for behavior disorders after traumatic brain injury: systematic review and expert consensus leading to French recommendations for good practice. Ann Phys Rehabil Med. 2016;59(1):42–57. PubMed CrossRef
- Hammond FM, Bickett AK, Norton JH, et al. Effectiveness of amantadine hydrochloride in the reduction of chronic traumatic brain injury irritability and aggression. J Head Trauma Rehabil. 2014;29(5):391–399. PubMed CrossRef
- Wheaton P, Mathias JL, Vink R. Impact of pharmacological treatments on cognitive and behavioral outcome in the post-acute stages of adult traumatic brain injury: a meta-analysis. J Clin Psychopharmacol. 2011;31(6):745–757. PubMed CrossRef
- Castriotta RJ, Murthy JN. Sleep disorders in patients with traumatic brain injury: a review. CNS Drugs. 2011;25(3):175–185. PubMed CrossRef
- Grima N, Ponsford J, Rajaratnam SM, et al. Sleep disturbances in traumatic brain injury: a meta-analysis. J Clin Sleep Med. 2016;12(3):419–428. PubMed CrossRef
- Grima NA, Rajaratnam SMW, Mansfield D, et al. Efficacy of melatonin for sleep disturbance following traumatic brain injury: a randomised controlled trial. BMC Med. 2018;16(1):8. PubMed CrossRef
- Kemp S, Biswas R, Neumann V, et al. The value of melatonin for sleep disorders occurring post-head injury: a pilot RCT. Brain Inj. 2004;18(9):911–919. PubMed CrossRef
- Lequerica A, Jasey N, Portelli Tremont JN, et al. Pilot study on the effect of ramelteon on sleep disturbance after traumatic brain injury: preliminary evidence from a clinical trial. Arch Phys Med Rehabil. 2015;96(10):1802–1809. PubMed CrossRef
- Barlow KM, Esser MJ, Veidt M, et al. Melatonin as a treatment after traumatic brain injury: a systematic review and meta-analysis of the pre-clinical and clinical literature. J Neurotrauma. 2019;36(4):523–537. PubMed
- Cassimatis M, Browne G, Orr R. The utility of melatonin for the treatment of sleep disturbance after traumatic brain injury: a scoping review. Arch Phys Med Rehabil. 2023;104(2):340–349. PubMed
- Kaiser PR, Valko PO, Werth E, et al. Modafinil ameliorates excessive daytime sleepiness after traumatic brain injury. Neurology. 2010;75(20):1780–1785. PubMed CrossRef
- Jha A, Weintraub A, Allshouse A, et al. A randomized trial of modafinil for the treatment of fatigue and excessive daytime sleepiness in individuals with chronic traumatic brain injury. J Head Trauma Rehabil. 2008;23(1):52–63. PubMed CrossRef
- Cicerone KD, Langenbahn DM, Braden C, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;92(4):519–530. PubMed CrossRef
- Cicerone KD, Goldin Y, Ganci K, et al. Evidence-based cognitive rehabilitation: systematic review of the literature from 2009 through 2014. Arch Phys Med Rehabil. 2019;100(8):1515–1533. PubMed CrossRef
- Nguyen S, McKay A, Wong D, et al. Cognitive behavior therapy to treat sleep disturbance and fatigue after traumatic brain injury: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2017;98(8):1508–1517.e2. PubMed CrossRef
- Li X, Feng Y, Xia J, et al. Effects of cognitive behavioral therapy on pain and sleep in adults with traumatic brain injury: a systematic review and meta-analysis. Neural Plast. 2021;2021:6552246. PubMed CrossRef
- El-Solh AA. Management of nightmares in patients with posttraumatic stress disorder: current perspectives. Nat Sci Sleep. 2018;10:409–420. PubMed CrossRef
This PDF is free for all visitors!