Substance abuse during peripartum is rising in the United States. In 2019, 7% of US women used prescription opioids during pregnancy, with 20% misusing the drugs.1 Approximately 8.3% of pregnant women used illicit substances, and 8.4% used tobacco products in 2020.2 From 2017 to 2020, drug overdose deaths in the United States among pregnant and postpartum females increased by 81%.3
Most recent prevalence estimates of substance use disorders (SUDs) during pregnancy and postpartum come from surveys relying on participant self-reporting, which suffer from recall bias and rarely distinguish between substance use and SUD. There is a shortage of studies that assess the current prevalence of SUDs in pregnant and postpartum women utilizing medical records, which are considered more reliable than self-reported information. This study aims to calculate the prevalence of SUD diagnosis among visits of pregnant and postpartum females in 2020 using inpatient and emergency department (ED) data from the National Hospital Care Survey (NHCS).
Methods
Data Source. The NHCS 2020 was utilized, which captures information from nonfederal, noninstitutional hospital–based inpatient and ED data using administrative and electronic health records.4 We used the public version of the dataset, which contains 5% of the total sample. The NHCS is categorized as a public health surveillance endeavor, and it has received approval from the National Center for Health Statistics Ethics Review Board.
Study Population. Pregnant and postpartum female visits were identified with the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes related to pregnancy, childbirth, and the puerperium (see Supplementary Material). SUDs were identified using ICD-10-CM codes within the F10–F19 range, corresponding to mental and behavioral disorders because of psychoactive substance use (see Supplementary Material).
Prevalence Calculation. The NHCS data include base weights and replicate weights to ensure the data accurately reflect the national population. RStudio (version 2024.04.2+764) was used for analysis. A survey design object was created using the “svrepdesign” function from the R survey package, addressing the NHCS’s complex design and enabling precise variance estimation (see Supplementary Material for Rcodes used for analysis). Weighted prevalence estimates and 95% CIs for each SUD were calculated using the “svymean” function utilizing replicate weight. The analysis focused on calculating the weighted prevalence of SUDs in pregnant and postpartum females.
Results
The sample of pregnant and postpartum females included 14,764 discharges in inpatient settings and 10,500 visits to EDs, which after application of weight were 3,884,390 and 3,344,087 in inpatient and ED settings, respectively.
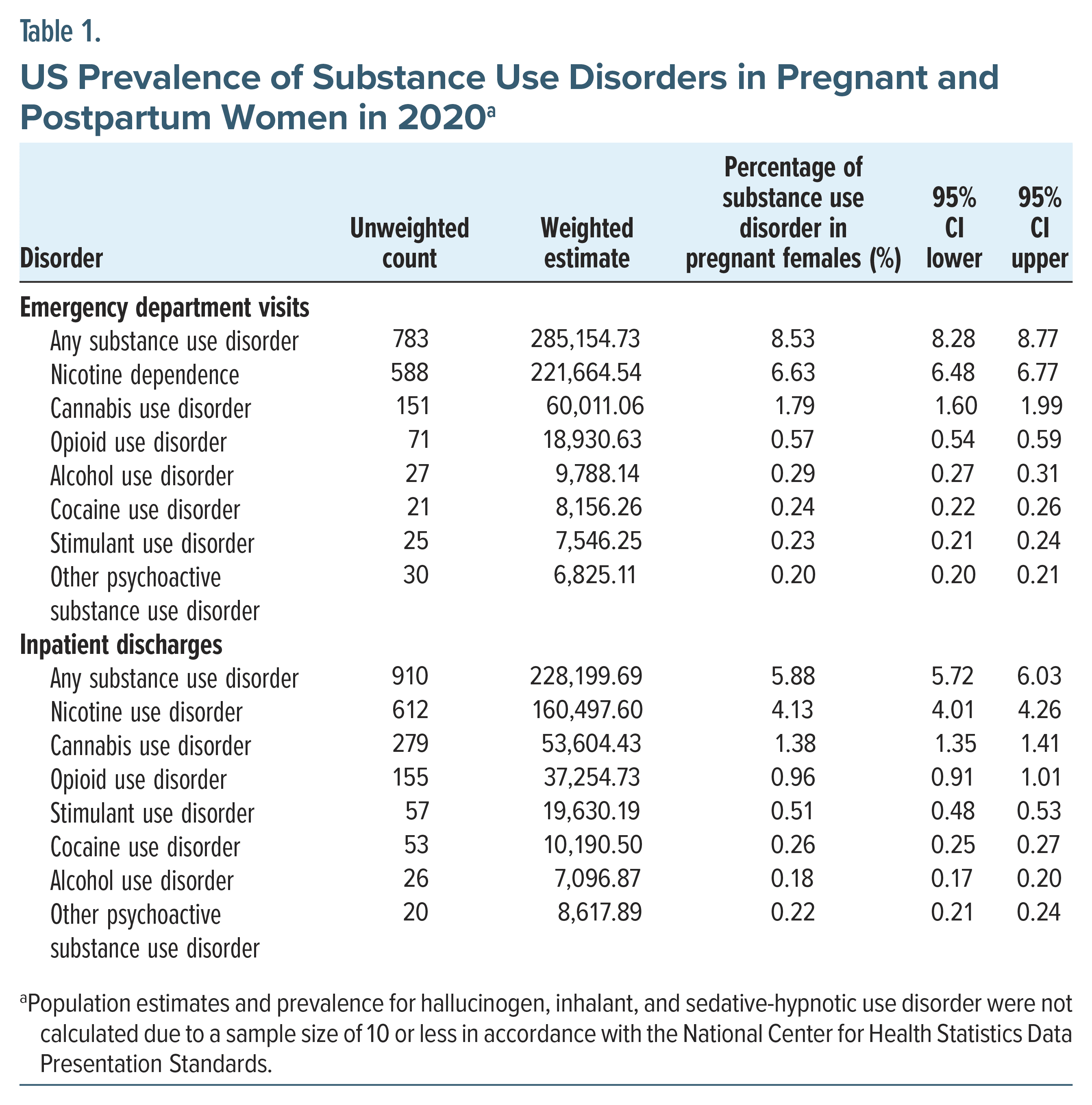
SUD diagnoses were notably more prevalent in the ED setting, with an overall prevalence of 8.53%. Nicotine dependence was found to be the most prevalent disorder among pregnant and postpartum female visits, affecting 6.63% of cases. This was followed by cannabis use disorder at 1.79% and opioid use disorder at 0.57% (Table 1).
In the inpatient setting, the overall prevalence of any SUD was slightly lower at 5.88% discharges. Here, nicotine dependence was also the most common, with a prevalence of 4.13%, followed by cannabis use disorder at 1.38% and opioid use disorder at 0.96% (Table 1).
Discussion
SUDs during pregnancy and the postpartum period are associated with many adverse outcomes for both mother and child.5 We analyzed the 2020 NHCS dataset to determine the prevalence of SUD diagnosis among pregnant and postpartum female visits.
Nicotine dependence diagnosis was present in 6.63% of visits in the ED and 4.13% in inpatient settings. A recent survey found that 12.1% of women reported smoking before pregnancy, and 5.4% reported smoking during pregnancy, aligning closely with our estimates.6 These findings underscore the critical issue of nicotine dependence among those who continue to smoke during pregnancy, highlighting the necessity for active screening and targeted interventions. The higher prevalence of cannabis use disorder may be attributed to its increasing legalization across the United States.7
Opioid use disorder diagnosis, though less common than nicotine and cannabis use disorders, had a prevalence of 0.57% in the ED and 0.96% in inpatient visits. The study also found that overall SUD prevalence was higher in the ED (8.53%) compared to inpatient settings (5.88%).
Several factors may contribute to the underrepresentation of opioid use disorder and alcohol use disorder in this study compared to previous research. First, this study relied on administrative and medical record data. Often, when the primary reason for a hospital visit does not involve substance use, patients may not report their SUDs due to fear of stigma, leading to potential underreporting. Moreover, nicotine use disorder paralleled the self-reported rates of nicotine use, suggesting that different substances may carry different levels of stigma. Patients might be reluctant to disclose the use of certain substances in emergency and inpatient settings if the visit’s primary reason is not substance related, due to concerns over the involvement of child protective services.
Another reason for the less reported prevalence of visits with alcohol use disorder and opioid use disorder compared to other studies may be related to the nature of the dataset, which records visits rather than patients. Pregnant and postpartum females with SUDs often have more frequent contact with health care services. If a patient has previously experienced stigma at a health care facility due to their SUD and fears the involvement of child protective services, they may choose to present at a different facility and not disclose their substance use.
This underreporting highlights the need for health care providers to create a nonjudgmental environment that encourages honesty about substance use, which is crucial for delivering appropriate care and intervention. Future studies could benefit from qualitative research that explores the reasons behind underreporting and the role of stigma in health care settings for pregnant and postpartum women with SUDs.
This study’s strength lies in its use of a nationally representative dataset, providing generalizable findings. However, the cross-sectional design limits the ability to track changes. Relying on medical records can produce biased results when the reason for the encounter is not substance use. The dataset’s unit is encounters, not patients, meaning some patients may be represented more than once if they were readmitted. Future research should focus on longitudinal studies to better understand SUD trends and their impact on maternal and child health.
Article Information
Published Online: March 6, 2025. https://doi.org/10.4088/PCC.24br03838
© 2025 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2025;27(2):24br03838
Submitted: August 24, 2024; accepted October 25, 2024.
To Cite: Rizvi A, Yadav G, Shayeb M, et al. Prevalence of substance use disorders among pregnant and postpartum women in the United States: a cross-sectional analysis of the National Hospital Care Survey 2020. Prim Care Companion CNS Disord 2025;27(2):24br03838
Author Affiliations: William R. Sharpe Jr. Psychiatric Hospital, West Virginia University, Weston, West Virginia (Rizvi); Department of Psychiatry, Texas Tech University, Permian Basin, Texas (Yadav, Shayeb, Jain).
Corresponding Author: Abid Rizvi, MD, 936 Sharpe Hospital Rd, Weston, West Virginia 26452 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Additional Information: The original dataset for the National Hospital Care Survey 2020 is available from the National Center for Health Statistics and can be assessed at https://www.cdc.gov/nchs/nhcs/data/index.html#cdc_data_description_data_systems-datasets.
Supplementary Material: Available at Psychiatrist.com.
References (7)

- Harter K. Opioid use disorder in pregnancy. Ment Health Clin. 2019;9(6):359–372.
- Wendell AD. Overview and epidemiology of substance abuse in pregnancy. Clin Obstet Gynecol. 2013;56(1):91–96.
- Stewart A, Ko J, Salvesen von Essen B, et al. Association of mental health conditions, recent stressful life events, and adverse childhood experiences with postpartum substance use - seven States, 2019-2020. MMWR Morb Mortal Wkly Rep. 2023;72(16):416–420.
- National Center for Health Statistics. National Hospital Care Survey. US Department of Health and Human Services, CDC; 2020. Accessed August 10, 2024. https://www.cdc.gov/nchs/nhcs/data/index.html#cdc_data_description_data_systems-datasets
- Giuliani E, Townsel CD, Jiang L, et al. Emergency department utilization for substance use disorder during pregnancy and postpartum in the United States (2006-2016). Womens Health Issues. 2022;32(6):586–594.
- Kipling L, Bombard J, Wang X, et al. Cigarette smoking among pregnant women during the perinatal period: prevalence and health care provider inquiries - pregnancy risk assessment monitoring system, United States, 2021. MMWR Morb Mortal Wkly Rep. 2024;73(17):393–398.
- Thompson R, DeJong K, Lo J. Marijuana use in pregnancy: a review. Obstet Gynecol Surv. 2019;74(7):415–428.
Enjoy this premium PDF as part of your membership benefits!