Abstract
Objective: To develop an evidence and consensus-based clinical recommendation (CR) regarding primary care management of insufficient and disturbed sleep associated with concussion/mild traumatic brain injury (mTBI) in service members and veterans.
Participants: A multidisciplinary expert working group (EWG) of 23 subject matter experts was selected by the Defense Health Agency (DHA) Traumatic Brain Injury Center of Excellence (TBICoE), based on relevant expertise and experience, from candidates nominated by DHA communities of interest.
Evidence: The TBICoE core working group (CWG) conducted a literature search using PubMed and Google Scholar databases for articles relevant to sleep and mTBI from 2014 to 2018. Resulting studies were reviewed by the CWG, and questions addressing gaps in the literature were formulated.
Consensus Process: Questions addressing gaps in the literature were distributed to the EWG, and consensus was achieved over the course of 5 online meetings. Based on the available evidence and EWG consensus, TBICoE developed a draft of the clinical recommendations and submitted it to the EWG for review and feedback. Feedback was adjudicated by TBICoE, and areas of nonconsensus were addressed via email utilizing a modified Delphi method.
Conclusion: The evidence and EWG agree that addressing sleep early following mTBI is imperative to promoting recovery and preventing chronic mTBI symptoms, maladaptive sleep behaviors, and chronic sleep disorders.
Prim Care Companion CNS Disord 2024;26(5):23nr03691
Author affiliations are listed at the end of this article.
By any definition, traumatic brain injury (TBI) is a major public health concern. Each year in the United States, more than 2.5 million Americans experience a TBI, resulting in significant adverse health consequences and increased economic costs.1 Additionally, TBI has been identified as a signature injury of the armed conflicts in Iraq and Afghanistan, impacting more than 450,000 service members since 2000.2 In civilian and military samples, the majority of TBIs are classified as mild and can result in a broad range of medical and psychiatric symptoms including posttraumatic stress, depression, anxiety, posttraumatic headache, cognitive complaints, and diminished quality of life.3
Notably, insufficient and disturbed sleep are among the most common self-reported complaints following mild TBI (mTBI) and can emerge during the acute, subacute, or chronic recovery stages and can persist for years.4,5 Clinical sleep disorders such as insomnia and obstructive sleep apnea (OSA) are also common, with prevalence estimates markedly higher than in the general population.4–6 Insufficient and disturbed sleep are also highly comorbid with, and can precede, exacerbate, and prolong, many of the consequences of TBI commonly encountered in clinical practice (eg, posttraumatic stress disorder [PTSD], anxiety, depression, and cognitive complaints), likely contributing independently and synergistically to morbidity, poorer functional and social outcomes, decreased quality of life, delayed recovery from mTBI, and long-term sequelae of mTBI.7–9
Insufficient sleep and disturbed sleep are highly prevalent in service members and veterans (SMVs), with prevalence and incidence rates far exceeding those of the general population.10 Since the onset of Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF), there have been significant increases in the rates of sleep disorders, particularly OSA and insomnia.11,12 The high rate of insufficient and disturbed sleep in the military has been attributed to service-related disorders (eg, TBI and PTSD) and service requirements (eg, deployments, shift work, and high operational tempo).13–17 PTSD, which is commonly comorbid with mTBI in SMVs,18 also adversely impacts sleep and is characterized by intrusive symptoms such as nightmares and arousal as well as reactivity changes such as insomnia/difficulty sleeping.19
The potential consequences of untreated insufficient and disturbed sleep (eg, cognitive impairment, decreased performance, and increased accidents) in the high-risk military service environment (eg, operating heavy machinery and weapons) underscore the necessity of ensuring restorative sleep in this population.16,17 Insufficient and disturbed sleep often co-occurs with, and is implicated in, numerous other sequelae of TBI, representing a common treatment target.9,10 While impaired sleep can worsen outcomes, healthy sleep and targeted sleep interventions can improve poor sleep, health related quality of life, and functional outcomes following mTBI.9,10 Addressing insufficient and disturbed sleep early after mTBI is therefore imperative to promoting recovery and preventing or reducing chronic mTBI symptoms.20
Primary care managers (PCMs) are optimally positioned to address insufficient and disturbed sleep early after mTBI. The role of civilian PCMs in the care of veterans of all ages is expected to increase as the 2019 Veterans Affairs (VA) Mission Act increased the number of veterans eligible to receive care in the civilian network from 8% to 40% of the VA’s 9.5 million patients.
Evidence-based recommendations, such as the Traumatic Brain Injury Center of Excellence (TBICoE) Management of Sleep Disturbances Following Concussion/mTBI (Sleep CR), are therefore needed to help standardize care across military and civilian health care systems, as well as guide civilian PCMs who may be less familiar with caring for SMVs with mTBI and its sequelae. While these recommendations are tailored to SMVs, the clinical approaches are based on evidence from SMVs and the general population, as well as from expert consensus, and can be readily applied to the general population.
METHODS
TBICoE uses a standardized and systematic process to develop clinical recommendations (CRs). For each CR, development is led by a core working group (CWG) consisting of subject matter experts (SMEs). The CWG conducts background work including an environmental scan, literature review, identification of evidence gaps/ questions, and organization of a multidisciplinary expert working group (EWG). The EWG consists of nominees from Defense Health Agency communities of interest including the services specialty leaders and the TBI advisory committee. Nominees are then selected by the CWG using a standardized approach to ensure representation from relevant areas of expertise and diverse settings (eg, academia, clinical, research, military, and civilian). Representatives from primary care are also included to ensure that the recommendations are applicable and usable in the primary care setting. For the development of the Sleep CR, 23 SMEs representing sleep, neurology, psychiatry, and other relevant specialties were included (see Supplementary Table 1 for a complete list of EWG members and their specialties). CRs are developed based on the body of evidence in the literature and in the absence of sufficient literature, EWG consensus. Consensus within the EWG was achieved utilizing a modified Delphi method.21,22
In the current project, a search was conducted to identify literature relevant to insufficient and disturbed sleep associated with mTBI. PubMed and Google Scholar databases were searched from January 1, 2014, to November 30, 2018, using all permutations of search terms related to sleep (eg, sleep, sleep disturbance, and insomnia) and search terms related to TBI (eg, mTBI, TBI, and concussion). Two CWG members independently reviewed the resulting studies for relevancy and inclusion/exclusion criteria. Inclusion criteria included peer-reviewed articles published in English with an n > 30, assessing adults (>18 years old) diagnosed primarily (>50%) with mTBI or concussion (vs moderate, severe, or penetrating TBI). Exclusion criteria included case studies, non–peer-reviewed sources, animal models, and studies in pediatrics or in patients diagnosed primarily (>50%) with moderate, severe, or penetrating TBI.
The entire CWG reviewed the resultant, relevant studies and formulated questions addressing gaps in the literature. Questions fell into 4 main content categories including diagnosis and outcomes, interventions, management, and military-specific considerations (see Supplementary Table 2 for a list of the EWG questions).
To answer these questions, the EWG was divided and assigned to 1 of the 4 content categories based on their expertise. These 4 small EWGs met independently via webinars to review and discuss the questions. A full EWG with all the SMEs was then convened, and a sleep specialist in the EWG facilitated discussion of the individual group recommendations to establish consensus. The CWG developed a preliminary draft of the recommendations, and the EWG was asked to provide feedback. Feedback was adjudicated by the CWG, and any remaining areas of nonconsensus were addressed via email utilizing a modified Delphi method.21,22
RESULTS
The literature review yielded 66 studies that formed the evidentiary basis for the CRs. Of those 66 studies, 5 were US Preventive Services Task Force Level I, 53 were Level II, and 8 were Level III studies. Approximately one-third included SMV participants. Review of the literature and EWG consensus resulted in inclusion of CRs for conditions commonly seen in SMVs in clinical practice including excessive daytime sleepiness (EDS), insomnia disorder, OSA, circadian rhythm sleep wake disorders (CRSWDs), parasomnias, insufficient sleep syndrome (ISS), and restless leg syndrome (RLS). Findings from the literature review indicated that EDS, insomnia, OSA, parasomnias, CRSWDs, and RLS were associated with mTBI.6,23,24
Relatively less evidence was identified for the prevalence of parasomnias and RLS following mTBI. Even so, the parasomnias, confusional arousals, and sleep paralysis, as well as RLS, were included to assist PCMs with identifying these conditions and minimize unnecessary referrals to Sleep Medicine. The parasomnias, trauma-related nightmares (TRN) and trauma-associated sleep disorder (TSD), were included as they are common in SMVs with PTSD,25–28 and as discussed previously, PTSD is frequently comorbid with TBI.18 Sleepwalking was included due to safety concerns with military operational requirements. Shift work disorder (SWD) and ISS were also included despite lack of evidence following mTBI, as they are common in the military population due to operational requirements and could impede recovery after mTBI.
The following results detail the evidence-based recommendations outlined in the CR that PCMs can use to identify and manage EDS, insomnia, OSA, CRSWDs, parasomnias, ISS, and RLS in the mTBI population. The entire CR can be accessed at https://health.mil/Sleep-mTBI-CR.29
Clinical Recommendation
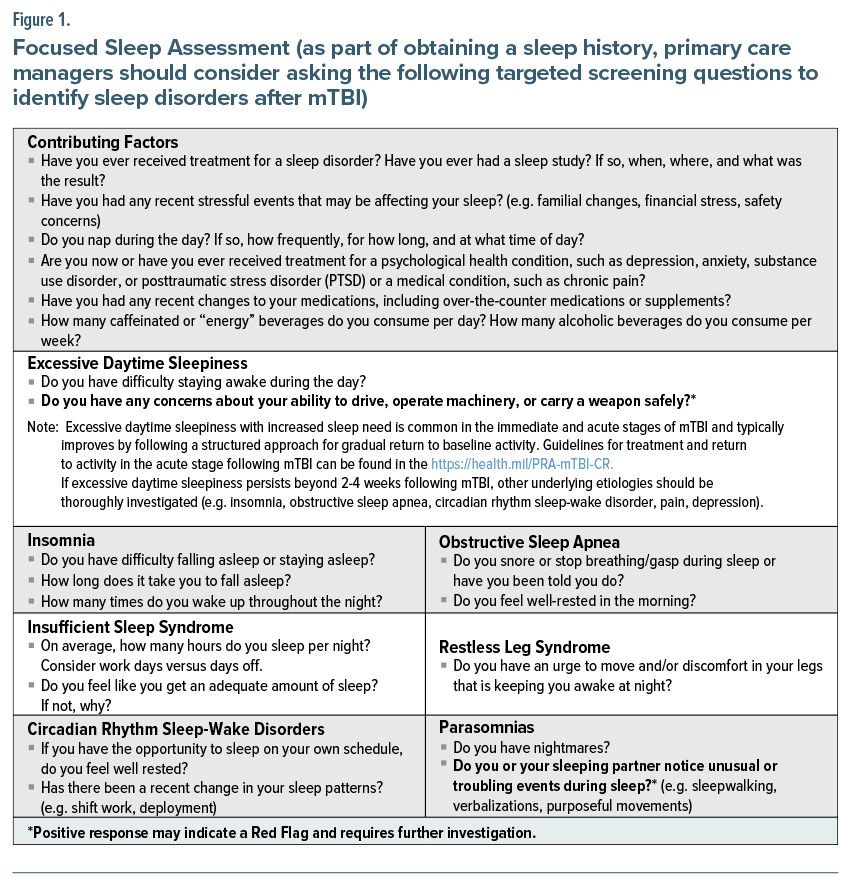
Assessment. Given the high incidence of insufficient and disturbed sleep following mTBI, the consequences of impaired sleep, and the benefits of improved sleep on a range of mTBI symptoms, all SMVs should be screened for insufficient and disturbed sleep following mTBI using questions such as “How often do you have difficulty falling or staying asleep, feel sleepy during the day, or experience unusual or troubling events during sleep (eg, purposeful movements or nightmares)?” Positive responses should prompt targeted screening questions (Figure 1), assessment of emergent symptoms and contributing factors including maladaptive sleep behaviors, comorbid medical and psychiatric conditions, and medications. Early referral to the appropriate specialty should be considered in patients with preexisting sleep or psychiatric conditions or polypharmacy (particularly multiple psychoactive medications).
EDS. EDS with increased sleep need is common in the immediate and acute phase following mTBI and typically resolves following a structured, progressive return to baseline activity: health.mil/PRA-mTBI-CR,30 including healthy sleep practices: https://health.mil/Sleep-and-TBI-FactSheet.9,31 EDS is also a diagnostic criterion for numerous other sleep disorders (eg, insomnia, OSA, CRSWDs, and ISS) and psychiatric conditions (eg, depression). These and other potentially contributory etiologies should be investigated if EDS persists following mTBI.32 If EDS raises safety concerns (eg, inability to stay awake or subjective sleepiness while driving, operating machinery, or handling weapons), immediate referral to Sleep Medicine is indicated.
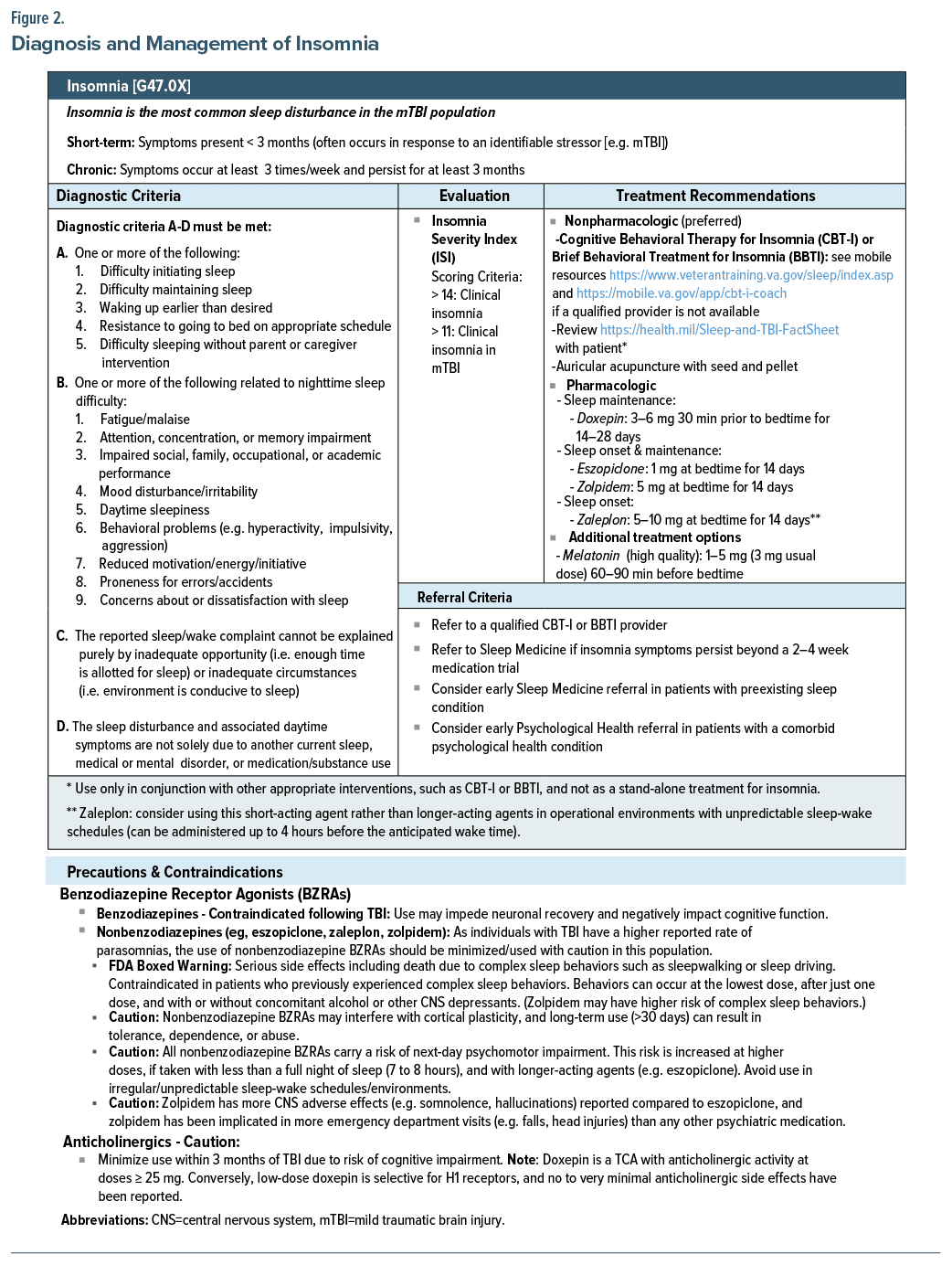
Insomnia. Insomnia, defined as difficulty initiating and/or maintaining sleep with an associated daytime consequence, is the most common sleep disorder in the mTBI population (see Figure 2).33 In service members, the prevalence is estimated to be almost 50%,13 versus 6%–10% in the civilian population.34 In addition to TBI, deployments and other medical and psychiatric conditions (eg, PTSD, depression, anxiety, and OSA) have been associated with an increased risk of insomnia.11,35
Evaluation. The most commonly used validated evaluation tool is the Insomnia Severity Index (ISI). A lower threshold for the clinical diagnosis of insomnia using the ISI is recommended in the TBI population based on a study36 assessing the psychometric properties and validity of the ISI in veterans with a history of TBI. Study results suggest that an ISI total score >11 is indicative of clinical insomnia. This lower threshold is aligned with recommendations for patients seen in clinical settings.36
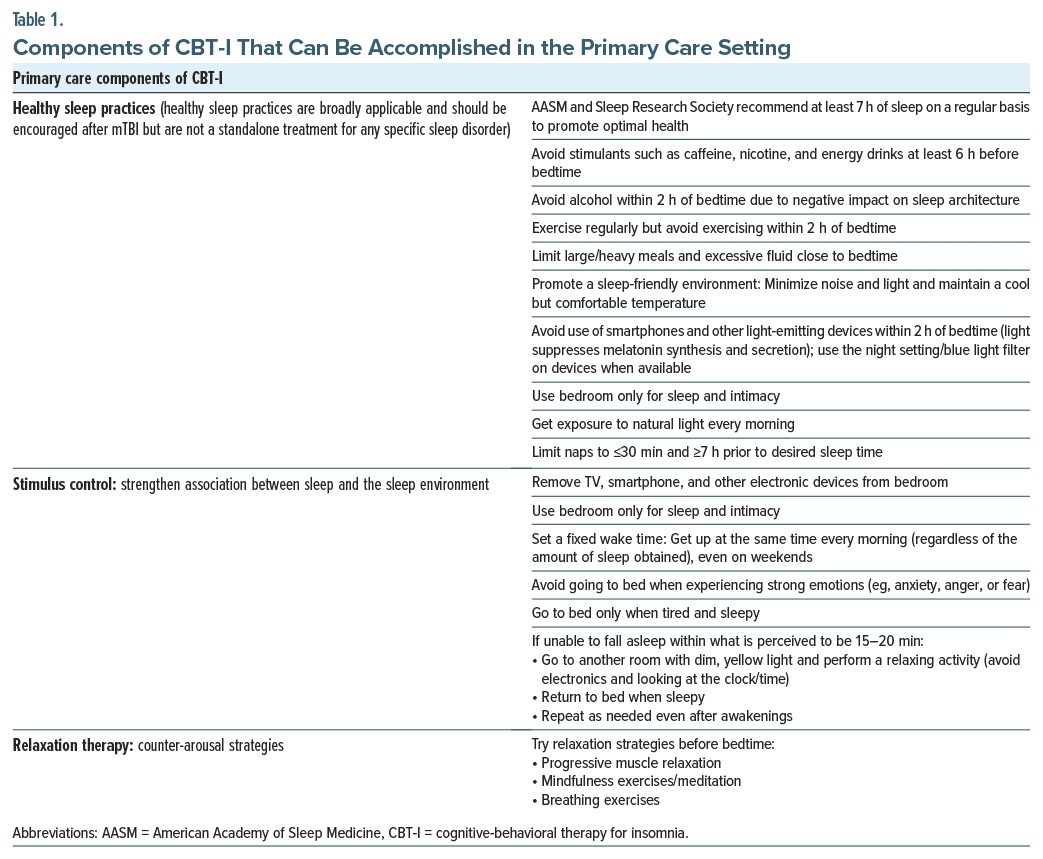
Treatment (nonpharmacologic). Cognitive-behavioral therapy for insomnia (CBT-I) is the treatment of choice for insomnia and insomnia with comorbid medical or psychiatric conditions.9,37 CBT-I is a multicomponent treatment for insomnia that targets difficulties with initiating and/or maintaining sleep through behavioral and cognitive interventions, including sleep restriction, stimulus control, relaxation therapy, cognitive restructuring, and sleep hygiene (healthy sleep practices). CBT-I has similar short-term effectiveness and better long term results compared to medications.38 Additionally, CBT-I has been shown to improve outcomes in a broad range of comorbid conditions, including TBI, PTSD, depression, chronic pain, and alcohol abuse.9,39
While referral to a CBT-I trained provider is required, PCMs can educate patients on CBT-I and initiate certain components in the primary care setting, including elements of stimulus control and relaxation therapy as well as education on healthy sleep practices (see Table 1 for primary care components of CBT-I and refer to https://health.mil/Sleep-and-TBI-FactSheet for a patient handout).31 Of note, education on healthy sleep practices should only be used in conjunction with other appropriate interventions and not as a stand-alone treatment for insomnia.40
While the VA is working to increase access, CBT-I is not yet widely available in primary and community care settings, and additional efforts are needed to increase access for SMVs not eligible for VA care.41 If CBT-I is unavailable, brief behavioral therapy for insomnia (BBT-I) can be considered as a potential alternative. BBT-I is a condensed version of CBT-I that focuses on sleep restriction and stimulus control and has demonstrated effectiveness in reducing insomnia symptoms.42 BBT-I can also be administered primarily remotely and by a range of clinicians. If in-person CBT-I or BBT-I is unavailable, mobile and online interventions may be considered (eg, CBT-i Coach, Insomnia Coach, or Path to Better Sleep).43 For more information on CBT-I and BBT-I, interested providers can refer to publicly available VA resources: https://www.healthquality.va.gov/guidelines/CD/insomnia/TreatingInsomniaProviders9212020508.pdf.44
Pharmacologic. If medications are used, they should be used short term and in conjunction with CBT-I or BBT-I, with the goal of tapering off the medication rather than maintaining long-term use.38,45,46 Before initiating a medication, the risks versus benefits must be weighed, including consideration of the impact on mTBI pathology (eg, cognitive impairment), sleep architecture, and comorbidities, as well as the impact on military operational requirements or constraints (eg, unpredictable sleep-wake schedules). Medications with central nervous system side effects should be minimized or used cautiously, particularly acutely postinjury, with a start low, titrate slow (and tapering off slow with chronic use) approach.
While evidence is limited in the mTBI population, nonbenzodiazepine, benzodiazepine receptor agonists (nonbenzodiazepine BZRAs) (eg, eszopiclone, zaleplon, and zolpidem), and the tricyclic antidepressant doxepin have demonstrated benefit in the general population and are recommended for the treatment of insomnia by the American Academy of Sleep Medicine (AASM).47 However, nonbenzodiazepine BZRAs should be used with caution due to the potential for next-day psychomotor impairment, cognitive dysfunction, and impaired cortical plasticity.48,49 Additionally, nonbenzodiazepine BZRAs carry a US Food and Drug Administration (FDA) boxed warning due to the risk of complex sleep behaviors (eg, sleepwalking). As individuals with TBI have a higher reported rate of parasomnias, nonbenzodiazepine BZRAs should be used with caution in this population. Tricyclic antidepressants (TCAs) should also be minimized within 3 months following mTBI due to anticholinergic effects and risk of cognitive impairment. Low-dose doxepin, however, is selective for H1 receptors, and minimal, if any, anticholinergic effects have been reported at doses less than 25 mg.50
Of note, the EWG encouraged caution when using medications that are not FDA approved for insomnia, including low-dose trazodone, which lacks outcomes data and can be associated with headache, somnolence, and other undesirable side effects in patients with mTBI.47
Orexin receptor antagonists (eg, suvorexant) are a relatively new class of medications that block the binding of wake-promoting neuropeptides orexin A and B to receptors OX1R and OX2R, which is thought to suppress wake drive. Orexin receptor antagonists were considered but not included in this primary care recommendation due to the desire for more evidence, concerns regarding their long half-life requiring at least 7 hours of sleep, risk of daytime somnolence, and prior authorization requirements. However, orexin receptor antagonists are a reasonable option if pharmacotherapy is indicated and the patient has failed or experienced adverse effects with nonbenzodiazepine BZRAs or low-dose doxepin. Orexin receptor antagonists or low-dose doxepin can also be considered if patients are older or have cognitive dysfunction.51
Results from limited studies in the TBI population indicate that melatonin and melatonin receptor agonists (ramelteon) may improve symptoms of insomnia and have a relatively benign side effect profile at low doses.52 The EWG recommended melatonin as an alternative treatment option for insomnia but expressed concern regarding variability in composition as melatonin is a dietary supplement not regulated by the FDA. Providers can direct patients to quality supplements verified by independent organizations such as United States Pharmacopeia or National Sanitation Foundation. Of note, the EWG also discussed ramelteon but did not include this medication in the CR based on a cost-benefit analysis. Additionally, TRICARE-eligible beneficiaries can obtain melatonin at military pharmacies, as the Department of Defense Pharmacy and Therapeutics Committee voted to add melatonin to the Military Health System Genesis over-the-counter list in order to standardize dispensing of melatonin at military treatment facilities.
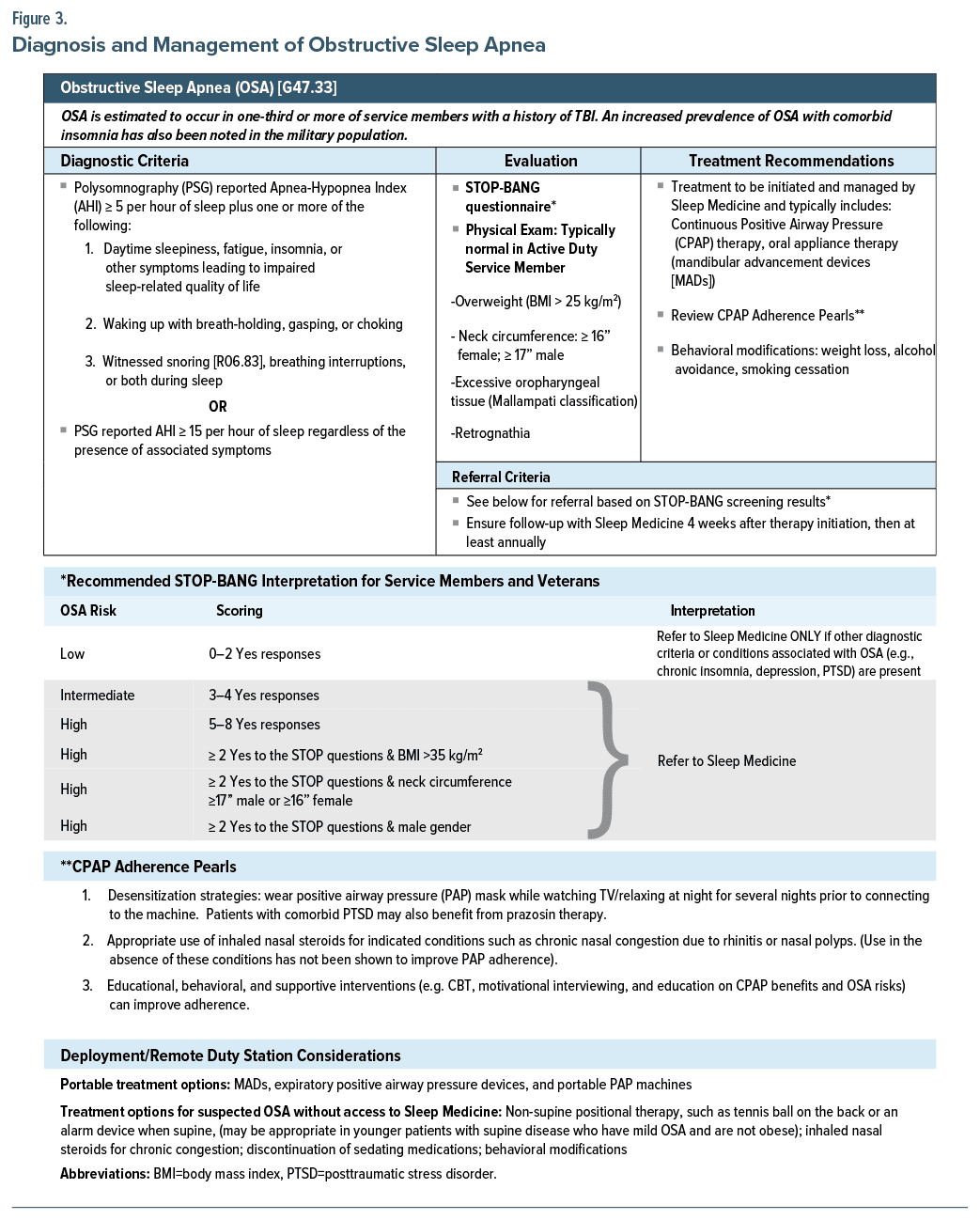
OSA. An increased prevalence of OSA (a sleep-related breathing disorder) has been noted in SMVs, despite fewer traditional risk factors such as obesity or older age.53–55 Deployment, TBI, and other medical and psychiatric conditions (eg, insomnia, PTSD, depression, and anxiety) have been associated with an increased risk of OSA.11,35,56–59
Diagnosis and evaluation. OSA risk can be stratified using the STOP-BANG questionnaire, which assesses the presence/absence of 8 risk factors including age >50 years and body mass index >35 kg/m2.60 However, SMVs with OSA may not reach the threshold of suspicion for OSA diagnosis using the STOP-BANG and often do not adhere to the traditional OSA presentation. Generally, service members and OEF/OIF/Operation New Dawn (OND) veterans are younger, are not overweight, have a normal physical examination, and report more sleepiness and score higher on the Epworth Sleepiness Scale (ESS).54,55 Additionally, the STOP-BANG has not been validated in populations with a high prevalence of OSA (eg, SMVs with a history of PTSD).
The EWG concluded that a negative screen should not negate the need for a polysomnography (PSG) in these high-risk populations and recommended lowering the threshold for suspicion of OSA and referral to Sleep Medicine in the STOP-BANG. Generally, a clinician would refer to Sleep Medicine for PSG if the STOP-BANG indicated intermediate to high risk of OSA (≥3). However, the EWG recommended that SMVs scoring low risk (≤2) also be referred to Sleep Medicine if they also displayed other diagnostic criteria (eg, daytime sleepiness) or conditions associated with OSA such as cardiovascular, cerebrovascular, or pulmonary disease, mood disorders, PTSD, cognitive dysfunction, chronic insomnia, and chronic opioid use44 (Figure 3).
Treatment. While there is a paucity of data assessing efficacy of positive airway pressure (PAP) therapy in patients with OSA and service-related disorders (eg, mTBI and PTSD), limited data do indicate that PAP therapy improves daytime sleepiness, quality of life, and nightmare frequency in SMVs with OSA and PTSD.61,62 However, the benefits of the therapy are often limited by lack of adherence.58
Anxiety, PTSD, and comorbid insomnia have all been associated with low PAP adherence.58,63,64 In PTSD patients, common symptoms such as sleep fragmentation, recurrent awakenings, insomnia, and nightmares, as well as mask discomfort and claustrophobia, have been identified as barriers to optimal PAP usage.64 Furthermore, even when PTSD patients are adherent, response to PAP therapy can be blunted compared to patients without PTSD.61
Primary care methods to increase PAP adherence include ensuring close follow-up with Sleep Medicine prior to and following PAP therapy initiation, desensitization strategies, and educational, behavioral, and supportive interventions (Figure 3).65,66 Appropriate treatment of any co-occurring, contributory conditions such as PTSD and insomnia will also help improve PAP adherence. Patients with comorbid PTSD may benefit from prazosin therapy, and patients with PTSD or sleep initiation insomnia may benefit from nonbenzodiazepine BZRAs. Additionally, awareness of alternate OSA treatment options can help PCMs educate reluctant patients. Portable PAP machines are available as well as mandibular advancement devices (MADs). In a randomized crossover trial of 35 veterans with OSA and PTSD, veterans were significantly more adherent to and preferred MAD over PAP therapy, and both therapies achieved equivalent health outcomes.67 MAD also confers the added benefit of managing bruxism, a parasomnia that can also occur after mTBI.
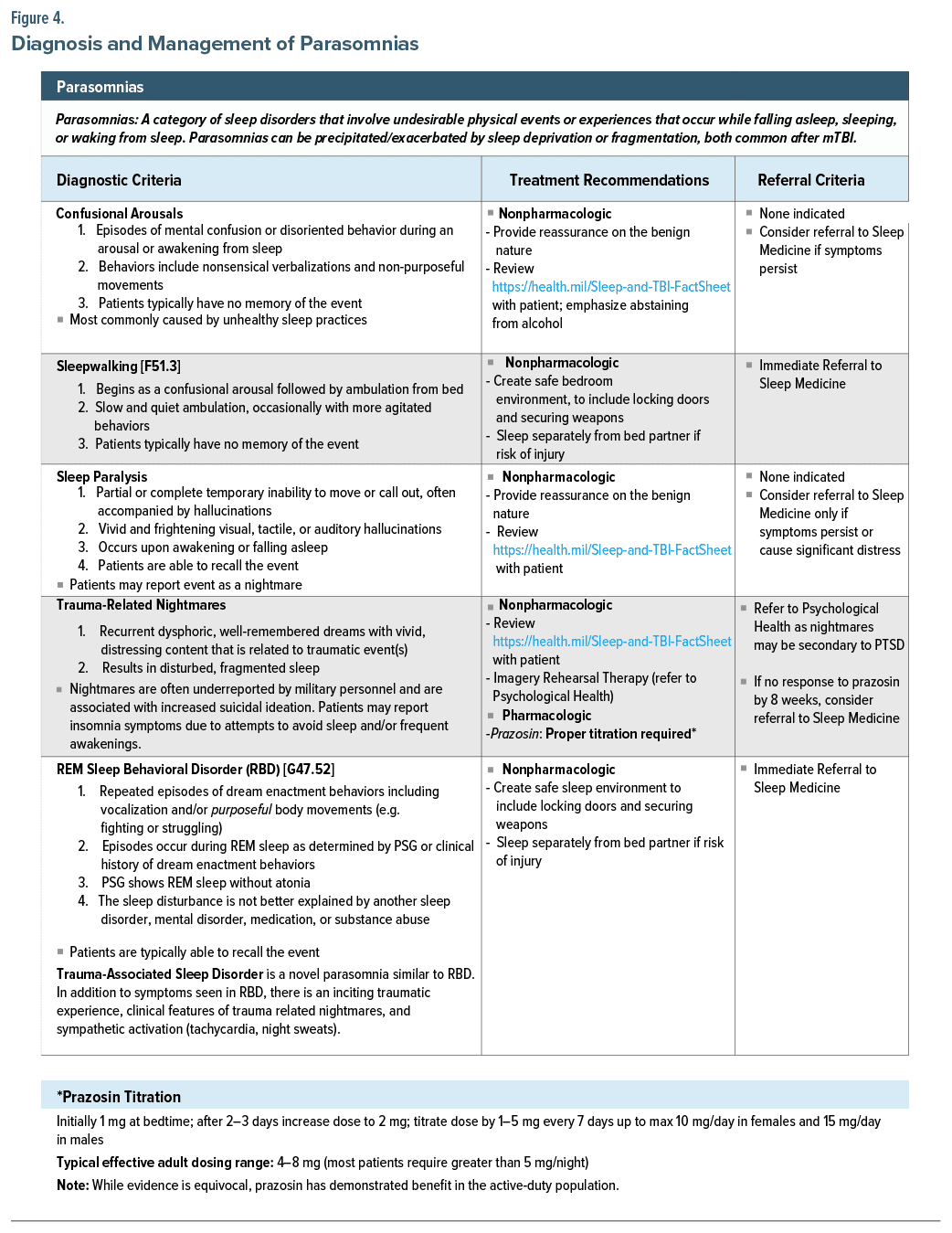
Parasomnias. Parasomnias can be precipitated/ exacerbated by sleep deprivation or fragmentation, both common after mTBI. Parasomnias are disruptive sleep disorders that involve undesirable physical events or experiences that occur while falling asleep, sleeping, or waking from sleep (eg, confusional arousals, sleep paralysis, sleepwalking, TRN, rapid eye movement [REM] sleep behavioral disorder [RBD], and TSD) (Figure 4).
Confusional arousals and sleep paralysis. Confusional arousals and sleep paralysis, while generally not associated with TBI, occur often and can be managed in the primary care setting. Confusional arousals are characterized by episodes of mental confusion or disoriented behavior (eg, nonsensical verbalizations and nonpurposeful movements) during an arousal or awakening from sleep.68 Sleep paralysis is characterized by partial or complete temporary inability to move or call out and is often accompanied by vivid and frightening visual, tactile, or auditory hallucinations that occur upon awakening or falling asleep.68 Confusional arousals and sleep paralysis are benign in nature and can generally be managed through healthy sleep practices: https://health.mil/Sleep-and-TBI-FactSheet.31
Sleepwalking. Although also not generally associated with TBI, sleepwalking warrants mentioning due to potential safety concerns, especially in the context of military operational requirements. Creation of a safe sleep environment (eg, locking doors, securing weapons, and sleeping separately if risk of injury) is indicated as well as immediate referral to Sleep Medicine for assessment and management.
TRN. TBI and PTSD commonly co-occur, especially in SMVs,18 and TRN are considered a hallmark symptom of PTSD,25,26 suggesting an increased incidence/prevalence of nightmares relative to the non-TBI population. Nightmares are often underreported by military personnel and are associated with increased suicidal ideation. Patients may report insomnia symptoms due to attempts to avoid sleep and/or frequent awakenings.69
Treatment. The EWG recommended imagery rehearsal therapy70 and prazosin for the treatment of nightmares in SMVs. Imagery rehearsal therapy is a brief cognitive behavioral intervention designed to destigmatize nightmares and rescript and rehearse repetitive disturbing dreams to reduce distress.70 While the efficacy of prazosin for nightmares has recently been questioned,71 prazosin has demonstrated benefit in SMVs.72 SMVs with higher sympathetic activation may be more likely to benefit from prazosin.71,72 Prazosin’s antiadrenergic activity blunts the persistent nocturnal elevation in noradrenergic activity implicated in TRN and the hyperarousal state of PTSD. Prazosin may have failed to demonstrate this benefit due to the lack of high sympathetic activation in the study population.71 Further supporting this theory, prazosin has been shown to be effective in TSD, a disorder also characterized by noradrenergic hyperarousal.73
Decreased efficacy of prazosin for nightmares may also occur due to untreated OSA. In patients with OSA and nightmares, PAP therapy has been associated with decreased nightmare frequency.62 As TRN are a component of PTSD, and PTSD and OSA commonly co occur in SMVs,58 screening for and treating comorbid OSA is imperative to effectively managing nightmares. Additionally, the EWG noted that antidepressants, which are commonly prescribed for PTSD and TBI patients, can precipitate/exacerbate nightmares, as well as dream enactment behaviors (DEBs), potentially counteracting the effects of prazosin.
RBD. RBD is characterized by repeated episodes of DEBs including vocalizations and/or purposeful body movements (eg, fighting or struggling) with loss of atonia during REM sleep. Studies suggest that RBD or symptoms of RBD are associated with neurodegeneration, OSA, TBI, PTSD, and antidepressant use. Untreated OSA can present with RBD-like symptoms, but these symptoms will resolve with effective treatment (eg, PAP).74
TSD. TSD is a novel parasomnia similar to RBD. In addition to the symptoms seen in RBD, TSD is characterized by an inciting traumatic experience, clinical features of TRN, and autonomic hyperarousal (eg, tachycardia and night sweats). Complicating the clinical presentation, TSD shares clinical features and is commonly comorbid with PTSD and OSA.27,28 Patients presenting with sleep complaints and a history of trauma should be screened not only for symptoms of PTSD but also for symptoms consistent with TSD. However, as with RBD, providers must remain cognizant that occult OSA increases the risk for many of these same symptoms (eg, autonomic hyperarousal and DEBs), which can benefit from effective treatment (eg, PAP).
DEBs characteristic of both RBD and TSD can pose a safety risk to the individual or their bed partner and creating a safe sleep environment (eg, locking doors, securing weapons, and sleeping separately if risk of injury) is indicated as well as immediate referral to Sleep Medicine for assessment and management.
CRSWDs. CRSWDs are characterized by a chronic misalignment between the preferred sleep-wake schedule and internal circadian clock, for example, wanting to sleep from 2300 (11 PM) until 0700 (7 AM) but only being able to sleep from 0300 (3 AM) until 1100 (11 AM). CRSWDs can be caused by extrinsic (eg, timing of light exposure) or intrinsic factors (malfunction of the circadian system, perhaps worsened by TBI). The sleep-wake pattern must be accompanied by symptoms of insomnia, EDS, or both. The specific CRSWD is further delineated depending on the CRSWD subtype.68 Two intrinsic CRSWDs that can occur in patients with TBI are delayed sleep-wake phase disorder and irregular sleep-wake rhythm disorder.24 SWD, an extrinsic CRSWD, occurs due to misalignment between the endogenous circadian rhythm and the imposed work schedule, which can be a common occurrence due to military requirements (eg, deployments and high operational tempo),16 and can impede recovery following mTBI.
In the primary care environment, CRSWDs should be assessed through clinical interview, sleep diary, and (if possible) actigraphy monitoring for 7–14 (work and free) days. Symptoms of CRSWD are often misattributed to insomnia24; however, CRSWD should be suspected if patients attain quality sleep when on their preferred sleep-wake schedule. Treatment of circadian dysregulation depends on the subtype and includes strategically timed blue light therapy and melatonin.9 Impact of light exposure, poor sleep practices, and comorbid depression should also be considered.
ISS. While evidence is lacking regarding the prevalence of ISS post-TBI, ISS is prevalent in the military population due to unique stressors (eg, high operational tempo)16 as well as in the general population. The AASM and the Sleep Research Society recommend at least 7 hours of sleep for adults on a regular basis to promote optimal health. However, more than one-third of adults in the US report less than 7 hours of sleep per 24 hours.75
ISS is characterized by EDS due to volitional curtailed sleep68 and is associated with numerous adverse effects and health outcomes (eg, cognitive impairment, reduced performance, and increased risk of accidents)16,17,75 and can impede recovery from TBI.
Symptoms associated with ISS include EDS, depression, fatigue, lethargy, cognitive difficulties, and irritability. ISS symptoms can be misattributed to insomnia; however, given the opportunity, patients with ISS will fall asleep rapidly, while patients with insomnia often report difficulty initiating or maintaining sleep. Evaluation and management of ISS consists of tracking sleep via a sleep diary for 7–14 (work and free) days, as well as implementation of healthy sleep practices (refer to https://health.mil/Sleep-and-TBI-FactSheet for a patient handout)31 and lifestyle or shift work modifications to allow for sufficient sleep time.
RLS. RLS may be increased in the TBI population.23 RLS is a clinical diagnosis characterized by an unpleasant or uncomfortable urge to move the limbs (usually the legs). Symptoms occur or worsen during periods of rest or inactivity, particularly in the evening, and are alleviated with movement.76
Nonpharmacologic treatment measures include applying warm compresses to the affected area, weighted blanket, and compression stockings at night. Pharmacologic measures include repletion of low ferritin levels (≤75 mcg/L), and γ-aminobutyric acid analogs (eg, gabapentin enacarbil). Dopaminergic agents (eg, pramipexole and ropinirole) are not recommended in the TBI population due to the potential to precipitate/ exacerbate parasomnias and behavioral disturbances such as impulse control.77
During sleep, patients with RLS may experience repetitive, highly stereotyped movements of the limbs, referred to as periodic limb movements of sleep (PLMS).76 PLMS are not specific to RLS and can occur in healthy older adults and are associated with other conditions including OSA. Patients who are unresponsive to RLS treatment, report continued functional impairment, or screen positive for OSA should be referred to Sleep Medicine. If present, treatment of comorbid OSA may decrease PLMS and RLS symptoms.78
CONCLUSION
In summary, insufficient sleep and disturbed sleep as well as clinical sleep disorders, such as insomnia and OSA, are very common and are associated with worsened outcomes following mTBI. Indeed, insufficient and disturbed sleep can precede, exacerbate, or prolong many of the most common sequelae of mTBI, including PTSD, depression, pain, and cognitive complaints. Early identification and targeted treatment for insufficient and disturbed sleep is vital for improved outcomes following mTBI. TBICoE therefore assembled a national EWG of SMEs to develop actionable recommendations for the management of insufficient and/or disturbed sleep following mTBI for non–sleep specialists seeking to deliver evidence-based, patient-centered care.
Article Information
Published Online: September 12, 2024. https://doi.org/10.4088/PCC.23nr03691
© 2024 Physicians Postgraduate Press, Inc.
Submitted: December 22, 2023; accepted May 2, 2024.
To Cite: Gold JM, Gano AL, McKinney GL, et al. Primary care management of sleep disturbances associated with concussion/mild traumatic brain injury in service members and veterans. Prim Care Companion CNS Disord. 2024;26(5):23nr03691.
Author Affiliations: Traumatic Brain Injury Center of Excellence, Silver Spring, Maryland (Gold, McKinney); Em Key Solutions, St. Petersburg, Florida (Gold); Cognosante Military & Veterans Health, Falls Church, Virginia (Gano); Sleep Disorders Center, Division of Pulmonary, Critical Care, and Sleep Medicine, and Department of Psychiatry, University of Maryland School of Medicine, Baltimore, Maryland (Wickwire).
Corresponding Author: Joanne M. Gold, PharmD, Em Key Solutions Support for TBICoE, Research Portfolio Management Division, Research & Engineering Directorate, Defense Health Agency, 3241 Regal Rd, Bethlehem, PA 18020 ([email protected]).
Relevant Financial Relationships: Dr Wickwire’s institution has received research support from the AASM Foundation, Department of Defense, Merck, NIH/NIA, ResMed, the ResMed Foundation, and the SRS Foundation; he has served as a scientific consultant to Axsome Therapeutics, DayZz, Eisai, EnsoData, Idorsia, Merck, Nox Health, Primasun, Purdue, and ResMed and is an equity shareholder in WellTap. Drs Gold, McKinney, and Gano have no relevant financial relationships or potential conflicts of interest to disclose.
Funding/Support: This material is supported by the Traumatic Brain Injury Center of Excellence (TBICoE). No outside sources of funding contributed to this project.
Role of the Sponsor: Department of Defense, Defense Health Agency, TBICoE is responsible for the development of the clinical recommendation described herein, including the collection, analysis, interpretation, and synthesis of evidence and expert opinion, as well as the preparation, review, and approval of this manuscript.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily represent the official policy or position of the Defense Health Agency, Department of Defense, or any other US Government agency. This work was prepared under Contract HT0014-22-C-0016 with DHA Contracting Office (CO-NCR) HT0014 and, therefore, is defined as US Government work under Title 17 U.S.C.§101. Per Title 17 U.S.C.§105, copyright protection is not available for any work of the US Government. For more information, please contact [email protected].
Supplementary Material: Available at Psychiatrist.com.
References (78)

- Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths–United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1–16.
- Department of Defense Numbers for Traumatic brain injury worldwide. Accessed October 16, 2023. https://health.mil/Military-Health-Topics/Centersof-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBIWorldwide-Numbers
- Centers for Disease Control and Prevention. Traumatic brain injury and concussion. Accessed October 13, 2023. https://www.cdc.gov/traumaticbraininjury/index.html
- Theadom A, Cropley M, Parmar P, et al. Sleep difficulties one year following mild traumatic brain injury in a population-based study. Sleep Med. 2015;16(8):926–932. PubMed CrossRef
- Leng Y, Byers AL, Barnes DE, et al. Traumatic brain injury and incidence risk of sleep disorders in nearly 200,000 US veterans. Neurology. 2021;96(13):e1792–e1799. PubMed CrossRef
- Mathias JL, Alvaro PK. Prevalence of sleep disturbances, disorders, and problems following traumatic brain injury: a meta-analysis. Sleep Med. 2012;13(7):898–905. PubMed CrossRef
- Kalmbach DA, Conroy DA, Falk H, et al. Poor sleep is linked to impeded recovery from traumatic brain injury. Sleep. 2016;41(10):zsy147. PubMed CrossRef
- Chan LG, Feinstein A. Persistent sleep disturbances independently predict poorer functional and social outcomes 1 year after mild traumatic brain injury. J Head Trauma Rehabil. 2015;30(6):E67–E75. PubMed CrossRef
- Wickwire EM, Schnyer DM, Germain A, et al. Sleep, sleep disorders, and circadian health following mild traumatic brain injury in adults: review and research agenda. J Neurotrauma. 2018;35(22):2615–2631. PubMed CrossRef
- McKeon AB, Stocker RPJ, Germain A. Traumatic brain injury and sleep disturbances in combat-exposed service members and veterans: where to go next? NeuroRehabilitation. 2019;45(2):163–185. PubMed CrossRef
- Caldwell JA, Knapik JJ, Shing TL, et al. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. PubMed CrossRef
- Moore BA, Tison LM, Palacios JG, et al. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. PubMed CrossRef
- Troxel WM, Shih RA, Pederson ER, et al. Sleep in the military: promoting healthy sleep among U.S. Servicemembers. Rand Health Q. 2015;5(2):19. PubMed
- Gilbert KS, Kark SM, Gehrman P, et al. Sleep disturbances, TBI and PTSD: implications for treatment and recovery. Clin Psychol Rev. 2015;40:195–212. PubMed CrossRef
- Martindale SL, Farrell-Carnahan LV, Ulmer CS, et al. Sleep quality in returning veterans: the influence of mild traumatic brain injury. Rehabil Psychol. 2017;62(4):563–570. PubMed CrossRef
- Capaldi VF, Balkin TJ, Mysliwiec V. Optimizing sleep in the military: challenges and opportunities. Chest. 2019;155(1):215–226. PubMed CrossRef
- Good CH, Brager AJ, Capaldi VF, et al. Sleep in the United States military. Neuropsychopharmacology. 2020;45(1):176–191. PubMed CrossRef
- Iljazi A, Ashina H, Al-Khazali HM, et al. Post-traumatic stress disorder after traumatic brain injury-A systematic review and meta-analysis. Neurol Sci. 2020;41(10):2737–2746. PubMed
- Stocker RPJ, Paul BTE, Mammen O, et al. Effects of blast exposure on subjective and objective sleep measures in combat veterans with and without PTSD. J Clin Sleep Med. 2016;12(1):49–56. PubMed
- Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–377. PubMed CrossRef
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–1015. PubMed
- Monguet JM, Trejo A, Martí T, et al. Health consensus: a digital adapted Delphi for healthcare. IJUDH. 2017;7(1):27–43.
- Walker JM, James NT, Campbell H, et al. Sleep assessments for a mild traumatic brain injury trial in a military population. Undersea Hyperb Med. 2016;43(5):549–566. PubMed
- Orff HJ, Ayalon L, Drummond SPA. Traumatic brain injury and sleep disturbance: a review of current research. J Head Trauma Rehabil. 2009;24(3):155–165. PubMed CrossRef
- Ross RJ, Ball WA, Sullivan KA, et al. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146(6):697–707. PubMed CrossRef
- Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24–33. PubMed CrossRef
- Mysliwiec V, O’Reilly B, Polchinski J, et al. Trauma associated sleep disorder: a proposed parasomnia encompassing disruptive nocturnal behaviors, nightmares, and REM without atonia in trauma survivors. J Clin Sleep Med. 2014;10(10):1143–1148. PubMed CrossRef
- Mysliwiec V, Brock MS, Creamer JL, et al. Trauma associated sleep disorder: a parasomnia induced by trauma. Sleep Med Rev. 2018;37:94–104. PubMed CrossRef
- Sleep Disturbances Following Concussion/mTBI Work Group. Traumatic Brain Injury Center of Excellence. DOD clinical recommendation for the management of sleep disturbances following concussion/mTBI: guidance for primary care management. 2020. https://health.mil/Sleep-mTBI-CR
- Progressive Return to Activity Work Group. Traumatic brain injury center of excellence. DOD Clinical Recommendation for the Progressive Return to Activity: Primary Care for Acute Concussion Management. 2024. http://health.mil/PRAmTBI-CR.
- Sleep Disturbances Following Concussion/mTBI Work Group. Traumatic Brain Injury Center of Excellence. Healthy Sleep Following Concussion/mTBI Patient Fact Sheet; 2022. https://health.mil/Sleep-and-TBI-FactSheet.
- Jaffee MS, Winter WC, Jones CC, et al. Sleep disturbances in athletic concussion. Brain Inj. 2015;29(2):221–227. PubMed CrossRef
- Zhou Y, Greenwald BD. Update on insomnia after mild traumatic brain injury. Brain Sci. 2018;8(12):223. PubMed
- Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin. 2013;8(3):281–297.
- Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–557. PubMed CrossRef
- Kaufmann CN, Orff HJ, Moore RC, et al. Psychometric characteristics of the Insomnia Severity Index in veterans with history of traumatic brain injury. Behav Sleep Med. 2019;17(1):12–18. PubMed
- Marshall S, Bayley M, McCullagh S, et al. Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700. PubMed CrossRef
- Mitchell MD, Gehrman P, Perlis M, et al. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract. 2012;13:40. PubMed CrossRef
- Ludwig R, Vaduvathiriyan P, Siengsukon C. Does cognitive-behavioural therapy improve sleep outcomes in individuals with traumatic brain injury: a scoping review. Brain Inj. 2020;34(12):1569–1578. PubMed CrossRef
- Chung KF, Lee CT, Yeung WF, et al. Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract. 2018;35(4):365–375. PubMed CrossRef
- Germain A, Richardson R, Stocker R, et al. Treatment for insomnia in combat exposed OEF/OIF/OND military veterans: preliminary randomized controlled trial. Behav Res Ther. 2014;61:78–88. PubMed CrossRef
- Buysse DJ, Germain A, Moul DE, et al. Efficacy of brief behavioral treatment for chronic insomnia in older adults. Arch Intern Med. 2011;171(10):887–895. PubMed CrossRef
- Zachariae R, Lyby MS, Ritterband LM, et al. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10. PubMed CrossRef
- VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea. (2019). Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea Work Group. 2019. Washington, DC: U.S. Government Printing Office.
- El-Solh AA, O’Brien N, Akinnusi M, et al. Predictors of cognitive behavioral therapy outcomes for insomnia in veterans with post-traumatic stress disorder. Sleep Breath. 2019;23(2):635–643. PubMed CrossRef
- Cheung JMY, Ji XW, Morin CM. Cognitive behavioral therapies for insomnia and hypnotic medications: considerations and controversies. Sleep Med Clin. 2019;14(2):253–265. PubMed CrossRef
- Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. PubMed CrossRef
- Stranks EK, Crowe SF. The acute cognitive effects of zopiclone, zolpidem, zaleplon, and eszopiclone: a systematic review and meta-analysis. J Clin Exp Neuropsychol. 2014;36(7):691–700. PubMed CrossRef
- Seibt J, Aton SJ, Jha SK, et al. The non-benzodiazepine hypnotic zolpidem impairs sleep-dependent cortical plasticity. Sleep. 2008;31(10):1381–1391. PubMed
- Yeung WF, Chung KF, Yung KP, et al. Doxepin for insomnia: a systematic review of randomized placebo-controlled trials. Sleep Med Rev. 2015;19:75–83. PubMed CrossRef
- Hoyer D, Allen A, Jacobson LH. Hypnotics with novel modes of action. Br J Clin Pharmacol. 2020;86(2):244–249. PubMed CrossRef
- Cassimatis M, Browne G, Orr R. The utility of melatonin for the treatment of sleep disturbance after traumatic brain injury: a scoping review. Arch Phys Med Rehabil. 2023;104(2):340–349. PubMed
- Williams SG, Collen J, Orr N, et al. Sleep disorders in combat-related PTSD. Sleep Breath. 2015;19(1):175–182. PubMed CrossRef
- Colvonen PJ, Masino T, Drummond SPA, et al. Obstructive sleep apnea and posttraumatic stress disorder among OEF/OIF/OND veterans. J Clin Sleep Med. 2015;11(5):513–518. PubMed CrossRef
- Lettieri CJ, Eliasson AH, Andrada T, et al. Obstructive sleep apnea syndrome: are we missing an at-risk population? J Clin Sleep Med. 2005;1(4):381–385. PubMed
- Haynes ZA, Stewart IJ, Poltavskiy EA, et al. Obstructive sleep apnea among survivors of combat-related traumatic injury: a retrospective cohort study. J Clin Sleep Med. 2022;18(1):171–179. PubMed
- Foster S, Brock MS, Hansen SL, et al. Sleep disorders related to deployment in active duty service members and veterans. Curr Pulmonol Rep. 2016;5(2):101–110. PubMed CrossRef
- Zhang Y, Weed JG, Ren R, et al. Prevalence of obstructive sleep apnea in patients with posttraumatic stress disorder and its impact on adherence to continuous positive airway pressure therapy: a meta-analysis. Sleep Med. 2017;36:125–132. PubMed CrossRef
- Collen J, Orr N, Lettieri CJ, et al. Sleep disturbances among soldiers with combat related traumatic brain injury. Chest. 2012;142(3):622–630. PubMed CrossRef
- Chung F, Abdullah HR, Liao P. STOP-bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149(3):631–638. PubMed CrossRef
- Lettieri CJ, Williams SG, Collen JF. OSA syndrome and posttraumatic stress disorder: clinical outcomes and impact of positive airway pressure therapy. Chest. 2016;149(2):483–490. PubMed CrossRef
- El-Solh AA, Vermont L, Homish GG, et al. The effect of continuous positive airway pressure on post-traumatic stress disorder symptoms in veterans with post traumatic stress disorder and obstructive sleep apnea: a prospective study. Sleep Med. 2017;33:145–150. PubMed CrossRef
- Budhiraja R, Kushida CA, Nichols DA, et al. Impact of randomization, clinic visits, and medical and psychiatric cormorbidities on continuous positive airway pressure adherence in obstructive sleep apnea. J Clin Sleep Med. 2016;12(3):333–341. PubMed CrossRef
- Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8(6):667–672. PubMed CrossRef
- Wickwire EM, Lettieri CJ, Cairns AA, et al. Maximizing positive airway pressure adherence in adults: a common-sense approach. Chest. 2013;144(2):680–693. PubMed CrossRef
- Askland K, Wright L, Wozniak DR, et al. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2020;4(4):CD007736. PubMed CrossRef
- El-Solh AA, Homish GG, Ditursi G, et al. A randomized crossover trial evaluating continuous positive airway pressure versus mandibular advancement device on health outcomes in veterans with posttraumatic stress disorder. J Clin Sleep Med. 2017;13(11):1327–1335. PubMed CrossRef
- American Academy of Sleep Medicine. The AASM International Classification of Sleep Disorders – Third Edition, Text Revision (ICSD-3-TR). American Academy of Sleep Medicine; 2023.
- Creamer JL, Brock MS, Matsangas P, et al. Nightmares in United States military personnel with sleep disturbances. J Clin Sleep Med. 2018;14(3):419–426. PubMed CrossRef
- Morgenthaler TI, Auerbach S, Casey KR, et al. Position paper for the treatment of nightmare disorder in adults: an American Academy of sleep medicine position paper. J Clin Sleep Med. 2018;14(6):1041–1055. PubMed CrossRef
- Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507–517. PubMed CrossRef
- Raskind MA, Millard SP, Petrie EC, et al. Higher pretreatment blood pressure is associated with greater posttraumatic stress disorder symptom reduction in soldiers treated with prazosin. Biol Psychiatry. 2016;80(10):736–742. PubMed CrossRef
- Brock MS, Powell TA, Creamer JL, et al. Trauma associated sleep disorder: clinical developments 5 years after discovery. Curr Psychiatry Rep. 2019;21(9):80. PubMed CrossRef
- Pham CK, SankariA, Slowik JM. Rapid Eye Movement Sleep Behavior Disorder. StatPearls Publishing. Accessed November 22, 2023. https://www.ncbi.nlm.nih.gov/books/NBK555928/
- Chattu VK, Sakhamuri SM, Kumar R, et al. Insufficient Sleep Syndrome: is it time to classify it as a major noncommunicable disease? Sleep Sci. 2018;11(2):56–64. PubMed CrossRef
- Allen RP, Picchietti DL, Garcia-Borreguero D, et al. Restless legs syndrome/Willis Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria—history, rationale, description, and significance. Sleep Med. 2014;15(8):860–873. PubMed CrossRef
- Garcia-Borreguero D, Silber MH, Winkelman JW, et al. Guidelines for the first-line treatment of restless legs syndrome/Willis-Ekbom disease, prevention and treatment of dopaminergic augmentation: a combined task force of the IRLSSG, EURLSSG, and the RLS-foundation. Sleep Med. 2016;21:1–11. PubMed CrossRef
- Silva C, Peralta AR, Bentes C. The urge to move and breathe - the impact of obstructive sleep apnea syndrome treatment in patients with previously diagnosed, clinically significant restless legs syndrome. Sleep Med. 2017;38:17–20. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!