Abstract
Objectives: To present experiences with an alternative psychiatry clerkship curriculum during the pandemic and potential initiatives for medical education in the future.
Methods: The psychiatry clerkship curriculum at Penn State College of Medicine was revised from a block rotation to a longitudinal integrated model in 2020 in response to the COVID-19 pandemic. Educational activities were separated into indirect patient care and direct patient care experience. Outcomes were measured via end of course evaluations and compared to the data from the previous year.
Results: The percentage of students who “agreed” or “strongly agreed” with “faculty/preceptors provided effective teaching” was 96% (N = 98) compared to 97% (N = 95) in the previous year, and the percentage who “agreed/strongly agreed” with “the feedback I received from attendings/residents helped me improve my patient care skills during the rotation” was 95% (N = 97) compared to 98% (N = 95) previously. The percentage of students who “agreed/strongly agreed” with “I was able to establish a meaningful relationship with at least 1 preceptor/attending during this rotation” was 94% (N = 98) compared to 97% (N = 95) previously, and the percentage who “agreed/strongly agreed” with “I was able to play a significant role in patient care during this rotation” was 88% (N = 98) compared to 91% (N = 94) previously. Also, 90% of students (N = 98) versus 93% (N = 95) from the year prior rated the quality of their educational experience during the clerkship as “4” or “5” on a Likert scale.
Discussion: The pandemic disrupted traditional undergraduate medical education and required adaptations to the clerkship curriculum to provide meaningful learning experiences. Integration of virtual patient care and telehealth services into medical education will serve to develop well-rounded physicians prepared for the future of health care.
Prim Care Companion CNS Disord 2025;27(1):24m03809
Author affiliations are listed at the end of this article.
The outbreak of the coronavirus disease 2019 (COVID-19) pandemic dramatically hastened changes to health care systems, clinical practice, medical education, and training. Medical education, which most commonly involves both didactics and in-person patient care experience during clerkships, aims to provide learners with the skill sets required to become competent and compassionate physicians.1,2 During the COVID-19 pandemic, social distancing, infection prevention strategies, and limitations on resources, presented significant challenges in undergraduate medical education. Public and learner safety were prioritized, travel was restricted only to essential medical staff, and students were therefore removed from the traditional learning environment. Medical educators were tasked with efficiently creating and implementing remote learning experiences, as the pandemic restricted in-person clinical experiences, didactics, and conferences.1–6
At Penn State College of Medicine, the administration urgently suspended in-person clinical clerkship experiences for medical students due to the aforementioned safety concerns and to minimize risk of viral transmission. Given this limitation, the Department of Psychiatry and Behavioral Health promptly established an alternative curriculum,3 including both remote learning and an abbreviated in-person experience when learners were able to return to the clinical environment. The goal of this new alternative curriculum was to provide a meaningful educational experience, focusing on developing critical thinking skills in a safe virtual learning format, including not only didactics and case discussions but also exposure to telehealth patient services and assistance with transitioning back to the physical patient care areas. In this article, we discuss our experiences with the alternate psychiatry curriculum at our institution during the COVID-19 pandemic and potential initiatives for medical education in the future.
METHODS
In collaboration with the Office of Medical Education at Penn State College of Medicine, the psychiatry clerkship curriculum was revised from a block rotation to a longitudinal integrated model. This revision was in line with all other clerkships at our institution. Educational activities were separated into indirect patient care (IPC) or “virtual learning” and, upon return to campus, direct patient care (DPC).
The IPC activities included synchronous virtual orientation providing an overview of the revised curriculum, video case-based learning discussing assessment and management of common psychiatric presentations, and virtual team-based learning sessions covering mood, psychotic, and substance use disorders, as well as child and consultation-liaison psychiatry. Additionally, students participated in a synchronous virtual telepsychiatry simulation session with standardized patients, which allowed learners to practice psychiatric interviewing, mental status examination, assessment, and management skills. These simulations also included crisis intervention, verbal de-escalation, and review of transference-countertransference in the management of challenging presentations. Asynchronous activities were also assigned during the IPC experience, which involved virtual self-learning modules on a broader selection of mental health and addiction topics. In addition, opportunities were created for research and scholarship, with students having access to research advisors. During this phase, learners were also integrated into patient care delivery via virtual rounds and clinic-based telehealth patient visits. The IPC activities introduced students to telehealth skills and experiential learning by allowing opportunities for clinical care, while safely preparing them for return to in-person patient care.
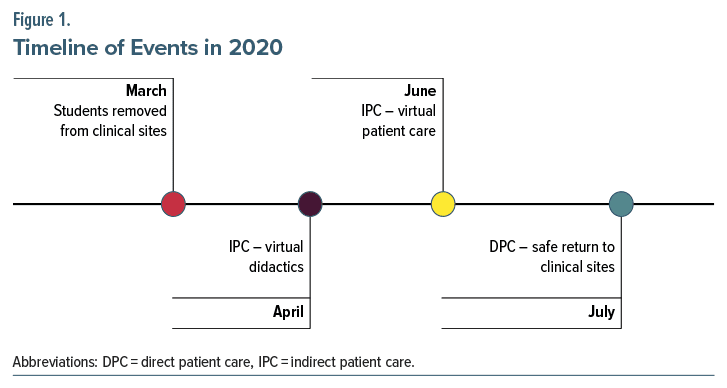
During the DPC phase, learners physically returned to patient care areas with safety guidelines in place. As capacity allowed, learners were provided adequate exposure to their areas of interest for an abbreviated in-person clinical experience. Several safety measures were in place to minimize risk of infection to patients, staff, and students. Some of these measures required learners and staff to wear masks at all times, learners to not directly provide care to patients who tested positive or were under investigation for COVID-19, and, in some clinical settings, removing learners and nonessential staff from patient care areas where patient isolation was a challenge. A timeline of events is illustrated in Figure 1.
Outcome measures were obtained via collection of data from end of course evaluations completed by learners. These surveys were provided to every student, and responses were anonymous. The evaluations served to assess the students’ perception of the quality and effectiveness of the curriculum and their satisfaction with the learning opportunities. Items evaluated were as follows: (1) faculty/preceptors provided effective teaching, (2) the feedback I received from attendings/ residents helped me improve my patient care skills during the rotation, (3) I was able to establish a meaningful relationship with at least 1 preceptor/ attending during this rotation, (4) I was able to play a significant role in patient care during this rotation, and (5) rate the quality of your educational experiences in this course/clerkship. Feedback provided by learners related to these measures was compared to data collected regarding student responses to the same questions from the prepandemic curriculum in the previous year.
RESULTS
The percentage of students who “agreed” or “strongly agreed” with “faculty/preceptors provided effective teaching” was 96% (N = 98) with the revised curriculum compared to 97% (N = 95) in the previous year. The percentage who agreed or strongly agreed with “the feedback I received from attendings/residents helped me improve my patient care skills during the rotation” was 95% (N = 97) with the revised curriculum compared to 98% (N = 95) in the previous year. The percentage of students who “agreed” or “strongly agreed” with “I was able to establish a meaningful relationship with at least 1 preceptor/attending during this rotation” was 94% (N = 98) with the revised curriculum compared to 97% (N = 95) in the previous year.
Also, 88% (N = 98) of learners “agreed” or “strongly agreed” with “I was able to play a significant role in patient care during this rotation” with the revised curriculum compared to 91% (N = 94) in the previous year. Ninety percent of students (N=98) taking the revised curriculum rated the quality of their educational experience during the clerkship as a 4 or 5 on a 5-point Likert scale, correlating to “good” or “excellent,” respectively, compared to 93% (N=95) of students providing these ratings during the previous prepandemic year.
Interestingly, more students taking the revised curriculum “strongly agreed” with item 1 (72%) compared with the previous year (60%). The percentage of students who selected “strongly agree” with item 2 was 67% with the revised curriculum (vs 59% the previous year). On item 3, 73% (vs 54% the previous year) “strongly agreed,” and on item 4, 54% (vs 46% the previous year) “strongly agreed.” On item 5, 56% of learners rated the course as “excellent” with the revised curriculum compared with 57% the previous year.
DISCUSSION
The spread of COVID-19 has dramatically impacted medical education. Social distancing prevented learners from gathering together for in-person educational activities, including didactic sessions, clinical rotations and clerkships, and cocurricular meetings. Hospital systems faced significant loss of income, leading to limitations on funding for medical education.5 However, the pandemic also provided an opportunity for medical educators to rethink traditional teaching methods and explore new and innovative ways of delivering high-quality medical education. Given limitations, rapid adaptation of existing didactic and clerkship curriculum toward virtual synchronous and asynchronous learning became imperative. To adapt to this unprecedented situation, medical educators had to redesign their curricula to meet the learning objectives and competencies required for future physicians, while ensuring the safety and well-being of students, faculty, and patients. Several strategies were implemented to deliver high-quality medical education in a virtual environment, including interactive online platforms, multimedia resources, virtual simulation, virtual rounding, and telehealth services.
Though the COVID-19 pandemic presented an unprecedented challenge in medical education, alternative curriculums, particularly those focused on telehealth and the modern delivery of medicine, can be used to provide learners necessary skills to become knowledgeable, compassionate, and adaptable physicians. These challenges emphasized the need for trainees and medical education to be flexible, responsive, and innovative in the face of uncertainty and disruption. Providing opportunities for both synchronous and asynchronous learning, including virtual didactics and DPC via telehealth services, provides students the experience necessary to become adaptable and forward-thinking clinicians. As our clinician educators, learners, and patients are now better accustomed to sharing virtual platforms for education and health care needs, we plan to utilize these resources concurrently, if necessary, in the future. We now have the framework to conduct the IPC and DPC activities simultaneously instead of in succession.
Despite the benefits associated with evolving curriculums, some difficulties with ensuring adequate learner engagement, interaction, and feedback were encountered. These challenges highlight the need for further research and innovation into medical education. Based on our experience and learner feedback, we have continued with virtual orientation and feedback sessions with students to minimize travel time and disruption in clinical learning. Additionally, we are utilizing some of these resources including virtual simulation and online learning modules for learners unable to participate during required educational sessions to supplement their learning and meet course objectives. As health care delivery evolves, virtual patient care and interdisciplinary collaboration are becoming increasingly important. In our experience, some of these virtual tools may be effectively and efficiently utilized for medical education and health care needs. As such, medical education providing experience in these areas will serve to develop adaptable and well-trained physicians, prepared for practice, in an ever-changing health care landscape during the COVID-19 pandemic and beyond.1–4
CONCLUSION
The impact of COVID-19 on medical education has been profound. Despite challenges, the revised psychiatry clerkship curriculum was well received, with the overwhelming majority of responses to the new curriculum being positive. Overall, the revised psychiatry clerkship curriculum, based on the outcome measures evaluated, was comparable to the prepandemic curriculum in terms of student feedback. By embracing the changes to the psychiatric curriculum, medical educators can equip students with the skills and knowledge they need to become knowledgeable, compassionate, and adaptable physicians.
Article Information
Published Online: February 11, 2025. https://doi.org/10.4088/PCC.24m03809
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 9, 2024; accepted October 21, 2024.
To Cite: Hameed U, Batchelder E, Hameed A. Psychiatry clerkship and the COVID-19 pandemic: lessons learned at Penn State College of Medicine. Prim Care Companion CNS Disord. 2025;27(1):24m03809.
Author Affiliations: Department of Psychiatry and Behavioral Health, Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania (all authors); Penn State College of Medicine, Hershey, Pennsylvania (all authors).
Corresponding Author: Usman Hameed, MD, Department of Psychiatry and Behavioral Health, Penn State Milton S. Hershey Medical Center, 500 University Dr, Hershey, PA 17033 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Effectiveness of virtual education and telemedicine is an area of ongoing research.
- The current and future generations of physicians are adapting to virtual learning and clinical care.
- Virtual platforms may serve as an efficient means to access high-quality educational programs as well as health care services.
References (6)

- Mian A, Khan S. Medical education during pandemics: a UK perspective. BMC Med. 2020;18(1):100. PubMed CrossRef
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. PubMed
- Batchelder E, Piper L, Sarwar S, et al. Psychiatric medical education in the age of COVID-19: the Penn state health experience. Prim Care Companion CNS Disord. 2020;22(5):20com02773. PubMed
- Ferrel MN, Ryan JJ. The impact of COVID-19 on medical education. Cureus. 2020;12(3):e7492. PubMed CrossRef
- Kaul V, Gallo de Moraes A, Khateeb D, et al. Medical education during the COVID-19 pandemic. Chest. 2021;159(5):1949–1960. PubMed
- Newman NA, Lattouf OM. Response to student contribution: methods and patient confidentiality. J Card Surg. 2020;35(9):2446.
Enjoy this premium PDF as part of your membership benefits!