Abstract
Objective: The Nipah virus poses significant health risks, particularly in regions like Kerala, India, where outbreaks have occurred. The objective of this study was to evaluate the prevalence of depression and anxiety among health care workers in a tertiary care hospital during a period of heightened concern regarding Nipah virus exposure.
Methods: A cross-sectional online survey was conducted from September 28 to November 9, 2023, involving 240 health care workers recruited through a snowball sampling method. Participants completed a self-report questionnaire that included demographic information and standardized instruments: the 9-item Patient Health Questionnaire (PHQ-9) for depression and the 7-item Generalized Anxiety Disorder scale (GAD-7) for anxiety.
Results: The study population comprised predominantly young adults aged 18–30 years (56.7%), with a majority being female (73.3%). Clinically significant depression was reported by 21.2% of participants, with varying severity levels, while 18% exhibited clinically significant anxiety. Nursing staff demonstrated a significantly higher prevalence of both depression and anxiety compared to non-nursing staff (P < .05). A significant correlation was found between PHQ-9 and GAD-7 scores (P < .001). Higher rates of depression were observed among staff exposed to the Nipah virus (P < .001) and those who had been quarantined (P < .001). Anxiety levels were notably elevated in the age 51–60 years group (P = .011).
Conclusion: The findings indicate a concerning prevalence of depression and anxiety among health care workers, particularly among nursing staff and those with exposure to the Nipah virus. These results highlight the urgent need for targeted mental health interventions and support systems within health care settings to address the psychological well being of staff during public health crises.
Prim Care Companion CNS Disord 2025;27(2):24m03818
Author affiliations are listed at the end of this article.
Nipah viral infection is a zoonotic disease caused by the Nipah virus, an RNA virus belonging to the Henipavirus genus within the Paramyxoviridae family. Fruit bats of the Pteropus genus serve as the reservoirs for this virus. Human infection can occur through direct contact with bats (as observed in India and Bangladesh) or through contact with other infected animals like pigs (as seen in Malaysia). The transmission of the infection among humans is possible, particularly through contact with the body fluids of an infected person, as evidenced in disease outbreaks in Bangladesh, West Bengal, and Kozhikode, Kerala.1,2 The incubation period of Nipah virus varies from 4 to 21 days. Studies have shown that the risk of infection was highest among spouses and principal caregivers.3,4
During September 12–15, 2023, the Ministry of Health and Family Welfare, Government of India, reported 6 laboratory-confirmed Nipah virus cases, resulting in 2 fatalities, in the Kozhikode district of Kerala. This marked the sixth Nipah virus outbreak in India since 2001 and the fourth in Kerala.5 Kerala’s initial Nipah outbreak occurred in 2018, predating the global COVID-19 pandemic. The 2018 outbreak claimed the lives of 21 of 23 infected individuals, while subsequent outbreaks in 2019 and 2021 resulted in 2 fatalities each.6 However, the state health officials responded well to the outbreaks and have been successful in managing the crisis and promptly curtailing the virus spread in the community.
Since there is no specific treatment or vaccination for Nipah virus infection, the main objectives for containing the viral spread encompass strict isolation, biorisk mitigation, and hospital infection control policies, including the mandatory use of personal protective equipment by health care workers. Effective surveillance, contact tracing, suspect isolation, and testing are also vital for disease control, but these efforts rely heavily on the dedicated labor force, primarily consisting of doctors, nurses, and other health care workers. Working in the midst of a deadly virus with a case fatality rate ranging from 40% to 75%, along with the added responsibility of effectively containing the virus, places significant psychological stress on health care workers. Numerous health care workers have been infected with the virus in past outbreaks, and tragic incidents such as the death of a nurse have significantly added to the fear of contracting the virus among health care workers.
One of the primary strategies imposed by the state for all outbreaks is the effective isolation of contacts. Indeed, studies have examined the prevalence of psychological distress among individuals subjected to isolation during past epidemics.7 It is important to note that these studies did not exclusively focus on health care workers. The abrupt and total social isolation, coupled with the fear of impending illness, undoubtedly has a profound impact on an individual’s psycho-social well-being, and this holds true for health care workers as well. One of the significant locations for disease transmission, as observed in previous outbreaks, is within hospital settings. Consequently, a majority of isolated contacts are often health care workers. It is important to attend to the psychological well-being of these individuals, since most health care workers will have to go back to the high-risk environment after the isolation period. Additionally, any psychological trauma experienced by these individuals will impact their future response to similar situations. The index patient of this outbreak arrived at the emergency department of our hospital on August 28, 2023, and was subsequently admitted to the medical intensive care unit. The patient died after 2 days, but the Nipah-positive diagnosis was only confirmed on September 14, 2023. This unexpected situation resulted in many health care workers having to go into isolation. A few days later, a nursing officer from the emergency department who came in contact with the index case was also confirmed positive. This led to a total of 114 health care workers, including 15 doctors, to undergo isolation.
This study explores the prevalence of psychological morbidity among hospital staff in our hospital who bravely confronted the epidemic. This knowledge will aid health care systems in anticipating these stressors during future incidents, enabling them to proactively address the psychological needs of health care workers in such future outbreaks.
METHODS
This study employed a cross-sectional online survey design and was conducted from September 28, 2023, to November 9, 2023, at a tertiary care hospital and research center located in Calicut, Kerala, India. Participants were recruited using a snowball sampling method. The survey was administered through an online self-report questionnaire created via Google Forms. The questionnaire link was distributed to hospital staff known to the researchers via WhatsApp and various social media platforms, with participants encouraged to share the link with other hospital colleagues.
Ethical approval for the study was granted by the hospital’s ethics committee, and participation was entirely voluntary. The questionnaire included demographic and personal information such as age, sex, years of employment, job title, marital status, and household living arrangements. Participants answered questions related to Nipah virus exposure and quarantine history. Additionally, the survey incorporated 2 standardized instruments: the 9-item Patient Health Questionnaire (PHQ-9) and the 7-item Generalized Anxiety Disorder scale (GAD-7), which assess clinically significant levels of depression and anxiety, respectively.8,9
The PHQ-9 is a widely recognized tool for screening major depressive disorder, boasting a sensitivity and specificity of 88%. It consists of 9 items rated on a 4- point scale from 0 (not at all) to 3 (every day), yielding a total score between 0 and 27. Depression severity is categorized based on the total score: mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27).
The GAD-7, used to evaluate anxiety symptoms, comprises 7 questions regarding anxiety experienced over the past 2 weeks, also utilizing a 4-point scale from 0 (not at all) to 3 (every day). The total score ranges from 0 to 21, with anxiety severity classified as mild (5–9), moderate (10–14), and severe (15–21).
Data analysis was performed using SPSS version 22.0. Descriptive statistics were calculated to determine percentages, means, and SDs. The association between sociodemographic factors and Nipah-related characteristics with psychological morbidities was evaluated using the χ2 test. An independent samples t-test was conducted to compare continuous variables.
RESULTS
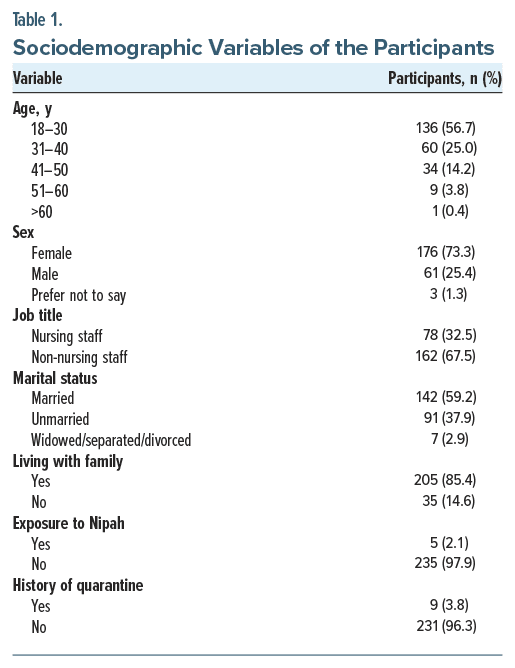
A total of 240 health care workers were involved in this study. The majority of the participants were aged 18–30 years (56.7%), followed by 31–40 years (25%), and 73.3% of the study population were female. Also, 59.2% were married, and 85.4% were living with their family during the study period. Among the respondents, 67.5% were non-nursing staff, and 32.5% were nursing staff. Only 5 participants were exposed to the Nipah virus, and 9 were quarantined. The sociodemographic variables are summarized in Table 1.
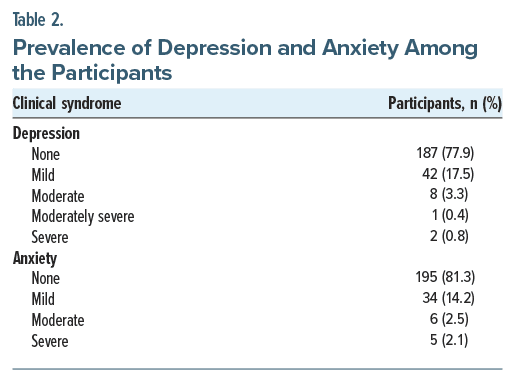
Of the participants, 53 (21.2%) reported clinically significant depression according to PHQ-9 scores: 42 (17.5%) reported mild depression, 8 (3.3%) reported moderate depression, 1 (0.4%) reported moderately severe depression, and 2 (0.8%) reported severe depression.
Additionally, 45 (18%) study participants reported clinically significant anxiety: 34 (14.2%) reported mild anxiety, 6 (2.5%) reported moderate anxiety, and 5 (2.1%) reported severe anxiety. The psychological morbidities are summarized in Table 2.
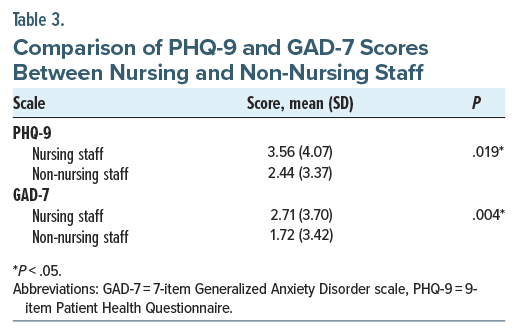
There was a significantly higher prevalence of depression and anxiety among nursing staff compared to non-nursing staff (Table 3). The mean PHQ-9 and GAD-7 scores were significantly higher among nursing staff compared with other hospital staff in 2-tailed t-tests. There was significant correlation between PHQ-9 and GAD-7 scores (P < .001).
There was significantly higher depression among Nipah-exposed hospital staff (χ2 = 49.6, df = 4, P < .001) and quarantined staff (χ2 = 30.1. df = 4, P < .001). Also, anxiety was higher among the age group 51–60 years (χ2 = 26, df = 12, P = .011).
DISCUSSION
This study was conducted to evaluate the prevalence of depression and anxiety in health care workers exposed to the Nipah virus epidemic in September 2023 at IQRAA International Hospital and Research Center. The prevalence of depression and anxiety in health care workers was 21.2% and 18%, respectively. While several studies emphasize the importance of evaluating psychological morbidities during an epidemic,10 there is limited existing literature on this topic during Nipah outbreaks in the district. This study represents the first comprehensive attempt, to our knowledge, to identify depression and anxiety among health care workers during a Nipah outbreak. A similar study conducted at the same hospital during the first wave of COVID-19, utilizing the same questionnaires (PHQ-9 and GAD-7), revealed depression in 16.4% and anxiety in 13.8% of the assessed health care workers.11 This finding suggests that psychological morbidities were more prevalent during the Nipah outbreak, despite most health care workers having recently experienced a pandemic setting, including quarantine, isolation, and personal protective equipment measures. This higher prevalence is likely attributable to the severity of Nipah infection and the high mortality rate observed in previous outbreaks.
A study12 conducted during the 2018 Nipah epidemic identified psychological morbidities among health care workers and the general public. It highlighted issues such as anxiety arising from a lack of adequate information about the disease and misinformation spread on social media.12 It is evident from studies reviewing newspapers, publications, and reports during the Nipah outbreak in Kerala that the spread of misinformation and fake news, particularly through social media, played an important role in causing panic and misunderstanding among the general population, including health care workers, during the epidemic. Such events significantly impacted the psychosocial well-being of the general population during the outbreaks.13
Although this was the sixth viral outbreak in the district and the general population and health care workers of Kozhikode were previously exposed to similar situations, the lack of clarity on the disease spread and the high mortality rates in previous outbreaks fueled anxiety and uncertainties. This is particularly true for health care workers, as there have been instances in which they have contracted the virus in previous outbreaks, including the unfortunate death of a nurse in 2018.
The findings of this study also suggest that depression and anxiety were more prevalent among nursing staff compared to other hospital staff. Nursing roles have been identified as independent risk factors for developing mental health problems in previous studies.10–12 The prominence of psychological morbidities among nursing staff was also observed in a similar study conducted during the first and second waves of the COVID-19 pandemic in the same hospital.11
There are limitations to our study that must be considered. The main limitation is that the study utilized an online survey methodology to collect data, which is known to produce selection bias. Another limitation is that the study was limited to a single tertiary care hospital.
CONCLUSION
This study revealed a high rate of clinically significant anxiety (18%) and depression (21.2%) among hospital staff. Moreover, psychological morbidities were significantly higher among nursing staff compared to other hospital staff. Adequate debriefing about the disease and the status of the epidemic should be provided at regular intervals to all health care workers exposed to the virus, especially to those who are quarantined. This measure might significantly reduce uncertainties and anxious thoughts in quarantined individuals. Additionally, efforts should be made to formulate guidelines for assessing and properly intervening to prevent and treat psychological morbidities among health care workers in future outbreaks. These guidelines should be developed either at institutional or regional levels, incorporating valuable input from psychiatrists, psychologists, social workers, and other medical professionals involved in public health. Such measures should be put in place, as Nipah outbreaks typically occur unexpectedly, and outbreaks are predicted in the future.
Article Information
Published Online: April 15, 2025. https://doi.org/10.4088/PCC.24m03818
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 22, 2024; accepted December 12, 2024.
To Cite: Mohamed F, Uvais NA, Shihabudheen P, et al. Assessing psychological morbidities in hospital staff during Nipah virus concerns: prevalence of depression and anxiety. Prim Care Companion CNS Disord 2025;27(2):24m03818.
Author Affiliations: Department of General Medicine, IQRAA International Hospital, Kozhikode, Kerala, India (Mohamed); Department of Psychiatry, IQRAA International Hospital, Kozhikode, Kerala, India (Uvais); Department of Critical Care, IQRAA International Hospital and Research Centre, Calicut, India (Shihabudheen); Department of Hospital Administration, IQRAA International Hospital and Research Centre, Calicut, Kerala, India (Nalakath).
Corresponding Author: N. A. Uvais, MBBS, DPM, Department of Psychiatry, IQRAA International Hospital, Malaparamba, Kozhikode, Kerala 673009, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Clinically significant depression was reported by 21.2% of participants, with varying severity levels, while 18% exhibited clinically significant anxiety.
- Nursing staff demonstrated a significantly higher prevalence of both depression and anxiety compared to non-nursing staff.
- Higher rates of depression were observed among staff exposed to the Nipah virus and those who had been quarantined.
References (13)

- Ang BSP, Lim TCC, Wang L. Nipah virus infection. J Clin Microbiol. 2018;56(6):e01875–e01917.
- Sahay RR, Yadav PD, Gupta N, et al. Experiential learnings from the Nipah virus outbreaks in Kerala towards containment of infectious public health emergencies in India. Epidemiol Infect. 2020;148:e90. PubMed CrossRef
- Aditi SM. Nipah virus infection: a review. Epidemiol Infect. 2019;147:e95.
- Nikolay B, Salje H, Hossain MJ, et al. Transmission of Nipah virus - 14 years of investigations in Bangladesh. N Engl J Med. 2019;380(19):1804–1814. PubMed CrossRef
- World Health Organization. Nipah virus infection - India. Disease Outbreak News [Internet]. World Health Organization; 2023. Accessed March 20, 2024. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON490.
- AlJazeera. Nipah trackers get samples from bats, trees as 800 tested in India’s Kerala [Internet]. 2023. Accessed March 20, 2024. https://www.aljazeera.com/news/2023/9/14/nipah-trackers-get-samples-from-bats-trees-as-800-tested-inindias-kerala
- Kannampulakkal SM, Sudevan SS, Tharayil HM, et al. Psychosocial effects of isolation on Nipah virus infection suspects during an outbreak. J Assoc Physicians India. 2021;69(1):41–45.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed CrossRef
- Preti E, Di Mattei V, Perego G, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):43.
- Uvais NA, Nalakath MJ. Prevalence of psychological morbidities among hospital staff during the second wave of COVID-19 in India. Prim Care Companion CNS Disord. 2023;25(5):22m03469.
- Swathy SS, Sidharthan M, Issudeen M, et al. Psychological interventions during Nipah viral outbreak in Kozhikode district, 2018. Indian J Psychol Med. 2018;40(4):387–389. PubMed CrossRef
- Lithin Z, Harikrishnan U, Jayakumar C, et al. Psychosocial perspective of Nipah virus outbreak in Kerala, India. Int J Sci Stud. 2019;6(11):159–162.
Enjoy this premium PDF as part of your membership benefits!