Abstract
Objective: To examine the prevalence and key correlates of psychological resilience in Ukrainian mental health workers (MHWs), using a novel discrepancy-based psychiatric resilience (DBPR) analytic approach.
Methods: A total of 178 Ukrainian MHWs, recruited via convenience sampling from July to August 2023, completed a survey assessing their war-related exposures, occupational stress, and mental health symptoms and sociodemographic and psychosocial characteristics. DBPR scores were computed by regressing composite distress scores onto measures of war- and work-related stressors. Psychological resilience was defined as lower actual, relative to predicted, composite distress scores. Multivariable and relative importance analyses were conducted to identify and quantify factors associated with greater resilience.
Results: A total of 55.6% of MHWs were classified as resilient. Greater levels of close social relationships, presence of meaning in life, and optimism were independently associated with greater resilience.
Conclusion: A slight majority of Ukrainian MHWs exhibit psychological resilience in the face of ongoing conflict and occupational stressors. Clinical interventions to bolster social connectedness, meaning in life, and optimism may help promote resilience in this population.
Prim Care Companion CNS Disord 2024;26(5):24m03761
Author affiliations are listed at the end of this article.
Mental health workers (MHWs) are vulnerable to psychological difficulties during humanitarian crises due to stressors associated with conflict, as well as the burden of their work.1 Given the demands of their work in aiding individuals affected by crises, having the capacity to adapt to stressful experiences is essential not only for their own mental well-being but also for fulfilling their professional responsibilities.2 While increasing research has examined mental health outcomes among MHWs during the Russia-Ukraine War,3–5 no known studies have investigated psychological resilience or its associated characteristics in this population. Such information is critical to informing prevention and treatment efforts to help maintain the mental health of these workers and the individuals they serve.
A growing body of research has demonstrated the utility of a discrepancy-based psychiatric resilience (DBPR) analytic approach to operationalizing psychological resilience.6–10 This approach involves regressing a measure of psychological distress onto measures of trauma and stressor exposure, with lower actual relative to predicted distress indicative of greater resilience.9 This novel analytic approach has been employed to examine resilience in various trauma exposed populations such as military veterans.6–8 In the present study, we utilized a DBPR approach to examine the prevalence and sociodemographic and psychosocial factors (eg, social support) associated with resilience in Ukrainian MHWs amid the ongoing Russia-Ukraine War.
METHODS
In this cross-sectional study, a convenience sample of MHWs was contacted and recruited by the local nongovernmental organization (NGO) and university. A DBPR analytic approach was employed to assess psychological resilience. Further details are illustrated below.
Participants
Participants were 178 MHWs across different regions of Ukraine, recruited via convenience sampling from July to August 2023. They were invited to participate in this study by local partners of the Ukrainian NGO International Platform on Mental Health and by the local university. They completed an online survey assessing their mental health symptoms and war-related exposures, as well as sociodemographic and psychosocial characteristics, during the Russia-Ukraine War. Participation was voluntary, and participants provided electronic informed consent prior to completing the survey.
Assessments
War-related exposure variables include distress from displacement, witnessing destruction, witnessing death, and uncertainty. Ratings ranged from 0 (no impact) to 10 (a significant impact). Additionally, given the association between work-related stressors and burnout,11 we assessed burnout symptoms as a proxy of work related stressor exposure during the war. Burnout was assessed using a single-item measure from the Maslach Burnout Inventory12: “Since the most recent Russian invasion, I have felt burnt out (eg, emotionally exhausted) from my work,” rated on a scale of 0 (never) to 5 (every day).
Posttraumatic stress disorder (PTSD) symptoms were assessed using the 4-item PTSD Checklist for DSM-5,13 which indexed symptoms related to the ongoing war. Sample items include “Repeated, disturbing, and unwanted memories of the invasion/war” and “Avoiding external reminders of the invasion/war,” rated on a scale of 0 (not at all) to 4 (extremely).
Major depressive disorder (MDD) symptoms were assessed using the 2-item Patient Health Questionnaire.14 Items included “Little interest or pleasure in doing things” and “Feeling down, depressed or hopeless,” rated from 0 (not at all) to 3 (nearly every day).
Generalized anxiety disorder (GAD) symptoms were assessed using the 2-item Generalized Anxiety Disorder (GAD-2).15 Items included “Feeling nervous, anxious, or on edge” and “Not being able to stop or control worrying,” rated from 0 (not at all) to 3 (nearly every day).
With regard to sociodemographic characteristics, participants reported their age, sex, work experience, and occupation. To classify occupational roles, we referred to the Inter-Agency Standing Committee guidelines on mental health and psychosocial support in emergency settings16 and categorized participants as either health professionals (ie, those who provided professional mental health services) or volunteer workers (ie, those who provided basic services and security, community and family support, and focused, nonspecialized mental health support).
Psychosocial characteristics assessed included optimism, gratitude, presence of and search for meaning in life, and presence of close social relationships. Optimism was assessed using a single item from the Life Orientation Test-Revised17 (“In certain times, I usually expect the best,” rated from 1=strongly disagree to 6=strongly agree). Gratitude was assessed using a single item from the Gratitude Questionnaire18 (“I have so much in life to be thankful for,” rated from 1=strongly disagree to 6=strongly agree). Presence of and search for meaning in life were assessed using the Meaning in Life Questionnaire19 (“I understand my life’s meaning,” “I am searching for meaning in life,” rated from 1=absolutely untrue to 6=absolutely true). Presence of close social relationships was assessed using the 2-item measure from domain 5 of the Flourishing Measure20 (“I am content with my friendships and relationships,” “My relationships are as satisfying as I would want them to be,” which are rated from 0=strongly disagree to 10=strongly agree).
Statistical Analysis
Data analyses proceeded in 7 steps. First, scores on measures of PTSD, MDD, and GAD symptoms were entered into a principal component analysis to generate a single composite distress score. Second, to compute a composite score for war-related exposure variables, we entered 4 war-related exposure variables into a principal component analysis and reduced them to a single factor score. Third, to compute DBPR scores, we regressed composite distress scores onto 2 trauma exposure variables—war-related exposure (ie, composite scores) and work-related stressor exposure (ie, burnout). Standardized residual scores were then inverted (ie, multiplied by −1) so that higher scores were indicative of greater psychological resilience. Fourth, we conducted χ2 analyses to compare sociodemographic and occupational characteristics by DBPR score–based classification of resilience (ie, standardized DBPR score>0 [greater resilience] vs≤0 [lower resilience]). Fifth, we conducted bivariate correlations between DBPR scores and sociodemographic and psychosocial variables. Sixth, we conducted a multivariable linear regression to examine independent correlates of DBPR scores; variables that were significantly correlated with DBPR scores at a P <.05 level in the bivariate correlations were included in this model. Seventh, we conducted a relative importance analysis to quantify the relative variance in DBPR scores explained by each correlate. This analysis partitions the explained variance in a dependent variable (ie, DBPR scores) while accounting for intercorrelations of independent variables.21
RESULTS
Computation of DBPR Scores
A principal component analysis of scores on measures of PTSD, MDD, and GAD symptoms revealed that scores loaded onto a single factor (eigenvalue = 2.30, 76.6% variance explained), with factor loadings ranging from 0.80 to 0.93. A separate principal component analysis of war-related exposure variables revealed that all 4 variables loaded onto a single factor (eigenvalue = 2.47, 61.7% variance explained), with factor loadings ranging from 0.53 to 0.91.
A linear regression analysis of trauma exposure factors (war-related exposure and work-related stressor exposure) entered as independent variables and composite distress scores as a dependent variable revealed a significant association (F = 55.72, P < .001) that collectively explained 38.9% of the variance in distress scores.
Prevalence of Psychological Resilience
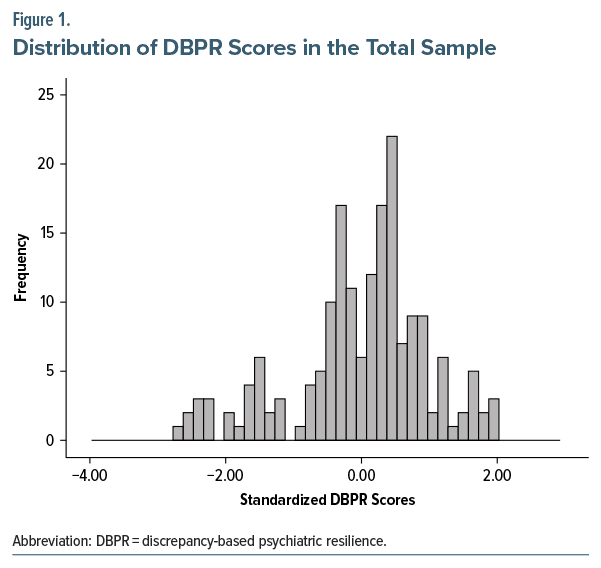
A total of 99 MHWs (55.6%) were classified as psychologically resilient (ie, standardized DBPR score > 0). These workers had a mean DBPR score of 0.68 (SD = 0.50), which was 0.68 SDs greater than the mean DBPR score in the full sample. Figure 1 shows the distribution of DBPR scores in the full sample.
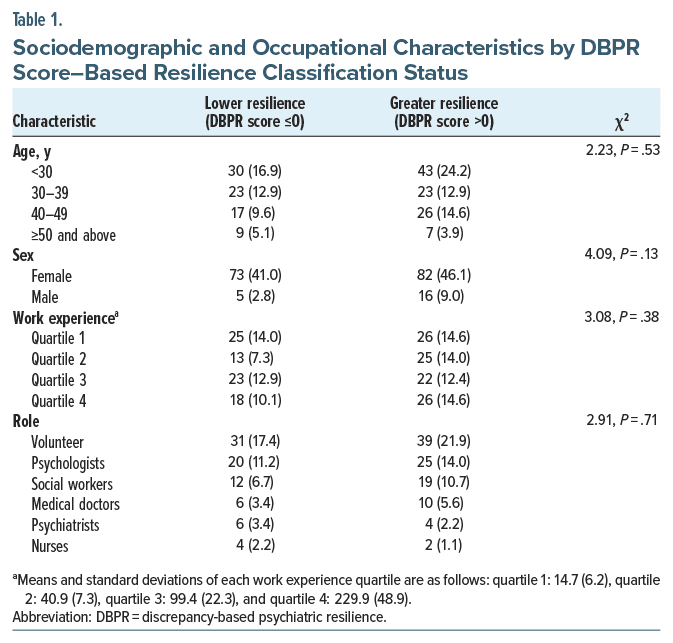
Table 1 shows sample characteristics by DBPR score–based classification of resilience (ie, standardized DBPR score > 0 [greater resilience] vs ≤ 0 [lower resilience]). None of the assessed characteristics differed between groups.
Descriptive Statistics and Results of Primary Analyses
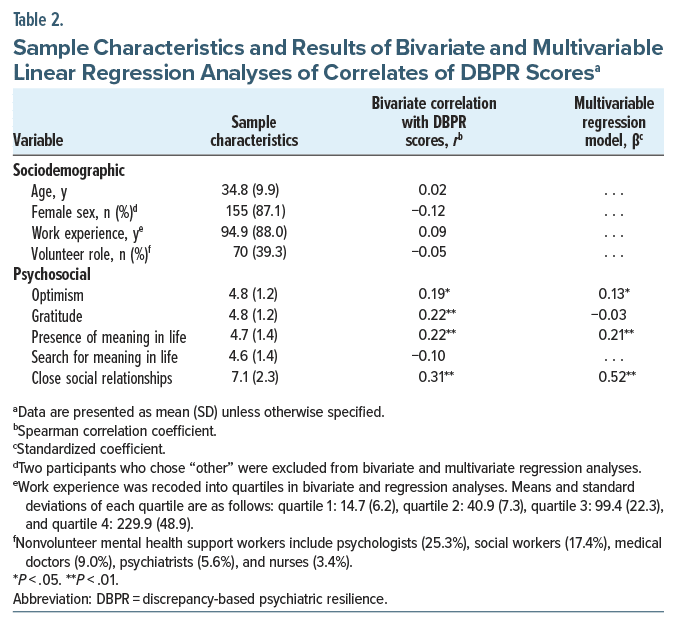
As summarized in Table 2, the majority of participants were female and volunteer MHWs. The sample had a mean age of 34.8 years and an average of 94.9 months of work experience.
Bivariate analyses revealed that higher DBPR scores, indicative of greater psychological resilience, were significantly associated with higher scores on measures of levels of close social relationships (r = 0.31, P < .001), presence of meaning in life (r = 0.22, P = .003), gratitude (r = 0.22, P = .003), and optimism (r = 0.19, P = .014).
Results of multivariable regression analysis revealed that higher levels of close social relationships (β = 0.52, P < .001), presence of meaning in life (β = 0.21, P = .003), and optimism (β = 0.13, P = .044) were independently associated with greater DBPR scores, collectively explaining 39.8% of the variance in this outcome. A relative importance analysis revealed that higher levels of close social relationships (69.4% relative variance explained [RVE]), presence of meaning in life (19.2% RVE), and optimism (11.4% RVE) explained the variance in DBPR scores.
DISCUSSION
Using a novel, DBPR analytic approach,9 results of the present study revealed that slightly more than half of the Ukrainian MHWs exhibited psychological resilience in response to war-related and occupational stressors. This study extends prior work on Ukrainian mental health and psychosocial support workers, which has primarily focused on negative mental health effects of the war. For example, a recent study3 showed that approximately half of psychosocial support workers reported poor mental health, and in another study4 of 25 Ukrainian helpline staff members, 68% screened positive for burnout, 44% for anxiety, and 40% for depression. In contrast to these previous findings, our study highlights the psychological resilience of the majority of Ukrainian MHWs (ie, the capacity to “bounce back”) in the face of war-related and occupational stressors, which is not only helpful for maintaining the mental health of these workers but also the populations that they serve. Given the high toll of providing mental health services during wartime coupled with the lack of MHWs in Ukraine due to displacement and injuries,22,23 identifying factors linked to greater resilience is crucial to preserving the mental health of this diminished workforce.
We identified 3 modifiable psychosocial factors associated with greater resilience to conflict- and work related stressors in Ukrainian MHWs. Higher levels of close social relationships were most strongly associated with greater resilience. Support from close social relationships and the broader community may help buffer MHWs from developing burnout and significant symptoms of distress (eg, anxiety) in stressful situations.2 One potential psychobiological mechanism is that greater social support may dampen hypothalamic pituitary-adrenal axis activity, leading to better stress regulation and resilience to stress.24 Further, consistent with prior work,6,7,25 greater presence of meaning in life and optimism were also independently associated with greater resilience. These factors may help promote resilience during challenging times by lowering reactivity to distress and reducing repetitive negative thoughts.26–28 They may also help promote psychological and behavioral flexibility (eg, goal reengagement and physical exercise), which can help individuals better manage and cope with stressors.27,29–31 Taken together, these results suggest that interventions that target these modifiable psychosocial factors32–34 may help promote psychological resilience in MHWs exposed to ongoing war-related and work-related stressors. Additional research is needed to evaluate this possibility.
This study has several limitations. First, participants were recruited via convenience sampling, which may limit generalizability to other MHWs or trauma-exposed populations. Second, the use of cross-sectional data negates causal interpretation between resilience and its correlates. Third, while there are other factors (eg, adaptive coping techniques and institutional support)2 associated with resilience, such variables were not assessed in this study. Fourth, while resilience is a dynamic process rather than a static outcome,35 our study is limited to providing a cross sectional “snapshot” of this phenomenon.
Notwithstanding these limitations, to our knowledge, this study is the first to examine the prevalence and correlates of psychological resilience in the Ukrainian MHWs who provide services amid the ongoing war. Key findings suggest that a slight majority of Ukrainian MHWs exhibit resilience to conflict and occupational stressors. They further indicate that 3 modifiable psychosocial factors—close social relationships, presence of meaning in life, and optimism—can be targeted as part of clinical and public health interventions to help promote resilience in this population amid the ongoing humanitarian crisis.
Further research is needed to follow up MHWs to examine temporal relationships of the variables assessed, identify biopsychosocial mechanisms underlying the association between psychosocial factors and psychological resilience, and evaluate the efficacy of interventions to promote these psychosocial factors and foster resilience to ongoing wartime and occupational stressors in this population.
Article Information
Published Online: October 22, 2024. https://doi.org/10.4088/PCC.24m03761
© 2024 Physicians Postgraduate Press, Inc.
Submitted: April 24, 2024; accepted July 12, 2024.
To Cite: Kang H, Fischer IC, Vus V, et al. Psychological resilience of mental health workers during the Russia-Ukraine War: implications for clinical interventions.
Prim Care Companion CNS Disord. 2024;26(5):24m03761.
Author Affiliations: Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, Connecticut (Kang, Pietrzak), US Department of Veterans Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, West Haven, Connecticut (Fischer, Esterlis, Pietrzak), Department of Psychiatry, Yale School of Medicine, New Haven, Connecticut (Fischer, Esterlis, Pietrzak), Laboratory of Small Group Psychology, Institute of Social and Political Psychology, Kyiv, Ukraine (Vus), International Platform on Mental Health, Kyiv, Ukraine (Vus), Sumy State Pedagogical University named after A.S. Makarenko, Sumy, Ukraine (Kolyshkina, Ponomarenko, Chobanian), Department of Psychology, Yale University, New Haven, Connecticut (Esterlis).
Corresponding Author: Robert H. Pietrzak, PhD, US Department of Veterans Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, 950 Campbell Ave 151E, West Haven, CT 06516 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Acknowledgements: The authors thank the mental health support workers who participated in this study.
Clinical Points
- Amid humanitarian crises, having the capacity to adapt to stressful experiences is essential to maintaining the psychological health of mental health workers (MHWs) and the individuals they serve.
- Interventions that bolster social connectedness, meaning in life, and optimism may help promote psychological resilience among MHWs exposed to ongoing war-related and work-related stressors.
References (35)

- Bjerneld M, Lindmark G, Diskett P, et al. Perceptions of work in humanitarian assistance: interviews with returning Swedish health professionals. Disaster Manag Response. 2004;2(4):101–108. PubMed CrossRef
- Ghodsi H, Sohrabizadeh S, Khani Jazani R, et al. Factors affecting resiliency among volunteers in disasters: a systematic literature review. Disaster Med Public Health Prep. 2022;16(1):398–404. PubMed CrossRef
- Kang H, Esterlis I, Chobanian AV, et al. Perceived mental health of psychosocial support professionals in Ukraine. Psychiatry Res. 2023;326:115320. PubMed CrossRef
- Pinchuk I, Goto R, Pimenova N, et al. Mental health of helpline staff in Ukraine during the 2022 Russian invasion. Eur Psychiatry. 2022;65(1):e45. PubMed CrossRef
- Kang H, Fischer IC, Vus V, et al. Well-being of mental health workers during the Russian-Ukrainian War. Ment Health Glob Challenges J. 2024;7(1):41–49.
- Georgescu MF, Fischer IC, Lowe S, et al. Psychological resilience in U.S. military veterans: results from the 2019–2020 national health and resilience in veterans study. Psychiatr Q. 2023;94(3):449–466. PubMed CrossRef
- Overstreet C, DeViva JC, Amstadter A, et al. Resilience to traumatic stress in U.S. military veterans: application of a novel classification approach in a nationally representative sample. J Psychiatr Res. 2021;140:301–307. PubMed CrossRef
- Thomas MM, Pietrzak RH, Nguyen DR, et al. Psychological resilience in west point graduates: results from a nationally representative study. Chronic Stress (Thousand Oaks). 2021;5:24705470211053850. PubMed CrossRef
- Amstadter AB, Myers JM, Kendler KS. Psychiatric resilience: longitudinal twin study. Br J Psychiatry. 2014;205(4):275–280. PubMed CrossRef
- Sheerin CM, Bustamante D, Bountress KE, et al. Psychiatric resilience and alcohol resistance: a twin study of genetic correlation and sex differences. Behav Genet. 2021;51(6):619–630. PubMed CrossRef
- Foo CYS, Tay AK, Yang Y, et al. Psychosocial model of burnout among humanitarian aid workers in Bangladesh: role of workplace stressors and emotion coping. Confl Health. 2023;17(1):17. PubMed
- West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445–1452. PubMed CrossRef
- Geier TJ, Hunt JC, Hanson JL, et al. Validation of abbreviated four- and eight-item versions of the PTSD checklist for DSM-5 in a traumatically injured sample. J Trauma Stress. 2020;33(3):218–226. PubMed CrossRef
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. PubMed CrossRef
- Sapra A, Bhandari P, Sharma S, et al. Using Generalized Anxiety Disorder-2 (GAD 2) and GAD-7 in a primary care setting. Cureus. 2020;12(5):e8224. PubMed CrossRef
- Inter-Agency Standing Committee. IASC Guidelines on Mental Health and Psychosocial Support in Emergency Settings. 2007.
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. PubMed CrossRef
- McCullough ME, Emmons RA, Tsang JA. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol. 2002;82(1):112–127. PubMed CrossRef
- Steger MF, Frazier P, Oishi S, et al. The Meaning in Life Questionnaire: assessing the presence of and search for meaning in life. J Couns Psychol. 2006;53(1):80–93.
- VanderWeele TJ. On the promotion of human flourishing. Proc Natl Acad Sci U S A. 2017;114(31):8148–8156. PubMed CrossRef
- Tonidandel S, LeBreton JM. Relative importance analysis: a useful supplement to regression analysis. J Bus Psychol. 2011;26(1):1–9.
- Seleznova V, Pinchuk I, Feldman I, et al. The battle for mental well-being in Ukraine: mental health crisis and economic aspects of mental health services in wartime. Int J Ment Health Syst. 2023;17(1):28. PubMed
- Goniewicz K, Burkle FM, Dzhus M, et al. Ukraine’s healthcare crisis: sustainable strategies for navigating conflict and rebuilding for a resilient future. Sustainability. 2023;15(15):11602.
- Ozbay F, Johnson DC, Dimoulas E, et al. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. 2007;4(5):35–40. PubMed
- Riolli L, Savicki V, Cepani A. Resilience in the face of catastrophe: optimism, personality, and coping in the Kosovo crisis. J Appl Soc Psychol. 2002;32(8):1604–1627.
- Ostafin BD, Proulx T. Meaning in life and resilience to stressors. Anxiety Stress Coping. 2020;33(6):603–622. PubMed CrossRef
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30(7):879–889. PubMed CrossRef
- Ishida R, Okada M. Effects of a firm purpose in life on anxiety and sympathetic nervous activity caused by emotional stress: assessment by psycho-physiological method. Stress Health. 2006;22(4):275–281.
- McKnight PE, Kashdan TB. Purpose in life as a system that creates and sustains health and well-being: an integrative, testable theory. Rev Gen Psychol. 2009;13(3):242–251.
- Haase CM, Singer T, Silbereisen RK, et al. Well-being as a resource for goal reengagement: evidence from two longitudinal studies. Motiv Sci. 2021;7(1):21.
- Hooker SA, Masters KS. Purpose in life is associated with physical activity measured by accelerometer. J Health Psychol. 2016;21(6):962–971. PubMed CrossRef
- Malouff JM, Schutte NS. Can psychological interventions increase optimism? A meta-analysis. J Posit Psychol. 2017;12(6):594–604.
- Manco N, Hamby S. A meta-analytic review of interventions that promote meaning in life. Am J Health Promot. 2021;35(6):866–873. PubMed CrossRef
- Sippel LM, Pietrzak RH, Charney DS, et al. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. 2015;20(4):10.
- Rutter M. Implications of resilience concepts for scientific understanding. Ann N Y Acad Sci. 2006;1094:1–12. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!