Abstract
Objective: Geriatric depression is a common and disabling mental health condition that often goes undetected, possibly due to complaints that are less typical and more somatic in nature. Irritability is neither a formal criterion for depression in adults nor a component of routine screening instruments; however, it is commonly expressed by older adults. The objective of this study was to establish the frequency of irritability in adults aged 60 and older and determine its utility in detecting geriatric depression.
Methods: Retrospective data were derived from a chart review of 2,300 individuals referred to our clinic from January 2015 to February 2023. Depression was established using the Beck Depression Inventory-II (BDI-II). Irritability was determined using a screening instrument containing 2 items assessing subjective experience of irritability and observations of irritability by others.
Results: Of 1,317 study participants meeting inclusion criteria, 514 (40%) responded positive for irritability. This group had significantly higher BDI-II scores compared to individuals denying irritability (P< .001). Using the recommended cut point for the BDI-II in primary care settings, participants meeting criteria for depression (n = 488, 37%) reported significantly greater levels of irritability than those without depression (P < .001).
Conclusions: In our sample, irritability was associated with higher levels of depression. In addition to employing traditional screening instruments for depression, practitioners working with a geriatric population should inquire as to the presence of irritability, either subjectively experienced or observed by others. Irritability appears to be a useful marker to facilitate detection and subsequent treatment of geriatric depression.
Prim Care Companion CNS Disord 2025;27(1):24m03808
Author affiliations are listed at the end of this article.
Geriatric depression is a common psychiatric condition that represents a significant source of disability and a major risk factor for increased mortality and morbidity in older adults.1–3 While prevalence rates of geriatric depression vary across clinical and community settings, there is overall concern that these rates will continue to rise, given projections that the number of Americans aged 65 years and older is expected to nearly double from 58 million in 2018 to 95 million by 2060, and the portion in the total population will increase from 17% to 23%.4,5 Given this anticipated demographic trajectory, as well as the availability of effective pharmacologic and psychosocial treatments, accurate detection of depression in older individuals is critical. However, geriatric depression is often overlooked, with as many as 50% of cases going undiagnosed.2 Late-life depression may be more difficult to detect, particularly in primary care settings, where data suggest that many older adults receive their mental health treatment at higher rates compared to younger adults.6 A significant percentage of older adults have clinically significant depressive symptoms that do not meet standard criteria for major depressive disorder,7 with symptomatic presentations that may be less typical, subsyndromal in nature, or possibly dominated by somatic complaints.8,9 Given these elements, there is a general consensus that systematic screening for depression in older adults is warranted, particularly in primary care settings.
The Patient Health Questionnaire-9 (PHQ-9) depression module10 is a 9-item self-administered instrument designed to detect the presence and severity of a major depressive episode as characterized in the DSM.11 The PHQ-212 was subsequently developed and consists of the first 2 items of the PHQ-9 (diminished interest or pleasure in activity and feelings of sadness, depression, hopelessness, or feeling down), which represent the diagnostic criteria for major depressive disorder in the DSM. Both instruments have been proven effective in detecting depression, either alone or in combination. Moreover, the PHQ-2 was found to be a valid screening tool for major depressive disorder in older individuals aged ≥65 years, although the recommendation was made that it should be followed by broader diagnostic questioning.13 Based on our observations, we believe that a critical component of this more comprehensive follow-up should be to assess for the presence of irritability.
Irritability is a common behavioral symptom that can be associated with various medical, psychiatric, and substance-related conditions. It has long been recognized as a symptom of major depression and was listed as an integral symptom in DSM editions prior to 1987, when the current diagnostic criteria were introduced. While the DSM-5 allows irritability to satisfy the depressed mood criteria in children and adolescents, irritability (described in the DSM-5 as persistent anger, an exaggerated sense of frustration over minor matters, and a tendency to respond to events with angry outbursts or by blaming others) is currently designated as an associated feature of major depressive disorder in adults. This is despite the fact that several cross-sectional studies have demonstrated relatively high prevalence rates of irritability during major depressive episodes. Benazzi and Akiskal14 used a structured interview to assess 254 individuals meeting criteria for unipolar major depression and found irritability to be present in 37.4% of their sample. Perlis and colleagues15 assessed the first 1,456 outpatients with nonpsychotic major depressive disorder entering the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study and found that 582 (40%) reported irritability more than half the time in the week prior to assessment. A follow-up study of the final 2,307 participants who eventually enrolled in STAR*D indicated that 1,067 (46%) had experienced irritability at least half the time in the preceding week.16 Fava and colleagues17 reviewed data from the National Comorbidity Survey Replication (N = 9,282 respondents) and found that after excluding individuals meeting criteria for bipolar spectrum disorders, irritability during depressive episodes was reported by roughly half of respondents with lifetime major depressive disorder. Longitudinal studies also support the association between irritability and depression. Judd and colleagues18 reviewed longitudinal data from 536 participants with major depressive disorder who had enrolled in the National Institute of Mental Health Collaborative Depression Study and who were systematically followed up for a mean of 16 years (and up to 30 years in some cases). They found that 292 participants (54.5%) demonstrated overt irritability at study intake and that irritability across the follow-up periods was associated with greater psychosocial impairment and reduced life satisfaction.
Irritability in the setting of geriatric depression seems to be less characterized. Data from the studies previously cited consist of samples with a mean age of early 40s.14,15,18 Given the projected expansion of the 65-and older age group over the next several decades, it is reasonable to expect a commensurate increase in the prevalence of geriatric depression. Our concern remains the underdetection of depression within this population as a whole, but also specifically with those manifesting irritability since this symptom is not captured by either the PHQ-9 or PHQ-2. The objective of the current study was to establish the frequency of irritability, either subjectively experienced or overtly manifested and detected by others, in a sample of geriatric individuals and determine its clinical relevance in the detection of depression.
METHODS
Study Population
Retrospective data were derived from a chart review of 2,300 individuals who were consecutively referred by primary care physicians to our specialty neuroscience clinic in South Florida for cognitive and behavioral assessment from January 2015 to February 2023. Inclusion criteria for this study were aged ≥60 years, completion of all investigational scales, and a Mini Mental State Examination19 score >27 (to minimize confounding effects of behavioral change associated with cognitive decline). This resulted in a total sample size of 1,317 individuals for our analyses.
Measurements
Primary study measures consisted of the Beck Depression Inventory-II (BDI-II)20 and the South Florida Cognitive Screener (SFCS).21 The BDI-II is a widely used 21-item self-report inventory measuring the severity of depression symptoms across various age groups, including geriatric individuals.22 When used in primary care and other nonpsychiatric medical settings, a BDI-II cut point of 13 has been recommended to detect the presence of clinically significant depression.23 The SFCS is an 8-item self-report screening instrument developed to capture the most common cognitive, functional, and behavioral complaints that may represent early signs of cognitive decline. Two of the items query for the presence of irritability: an irritability self-report (ISR) item assessing whether the individual directly experiences irritability (“Are you more irritable than usual?”) and an irritability observed-by-other report (IOR) item in which irritability has been commented upon by a collateral individual (“Has a friend or family member told you that you are more irritable?”). In addition to conducting direct comparisons between positive vs negative endorsement on the ISR and IOR items, individuals were also assigned to groups according to their pattern of responding on these 2 items as follows: (1) no irritability (NI), in which irritability was denied on both items; (2) ISR+IOR, in which both items were positively endorsed; (3) ISR/IOR, in which either item was positively endorsed; (4) +ISR−IOR, in which ISR was endorsed but IOR was denied; and (5) +IOR−ISR, in which IOR was positively endorsed but ISR was denied.
Statistical Analyses
Descriptive statistics were calculated for the whole sample and each of the 5 groups. Means and SDs were calculated for MMSE and BDI-II scores. An initial comparison was conducted with 2 independent samples t-tests to compare the means of the BDI-II for positive response on the self-report item (+ISR) vs negative response on this item (−ISR), as well as for positive response on the observed-by-other item (+IOR) vs denying this item (−IOR). Independent sample t-tests were also performed to compare means on the BDI-II between the NI group and each of the other 5 groups. Finally, χ2 comparisons were made on the basis of self-report (+ISR vs −ISR) in individuals with BDI-II scores >13. A difference with a P value ≤.05 was considered statistically significant. SPSS Statistic Software version 28.0 for Mac was used for all statistical analysis.
RESULTS
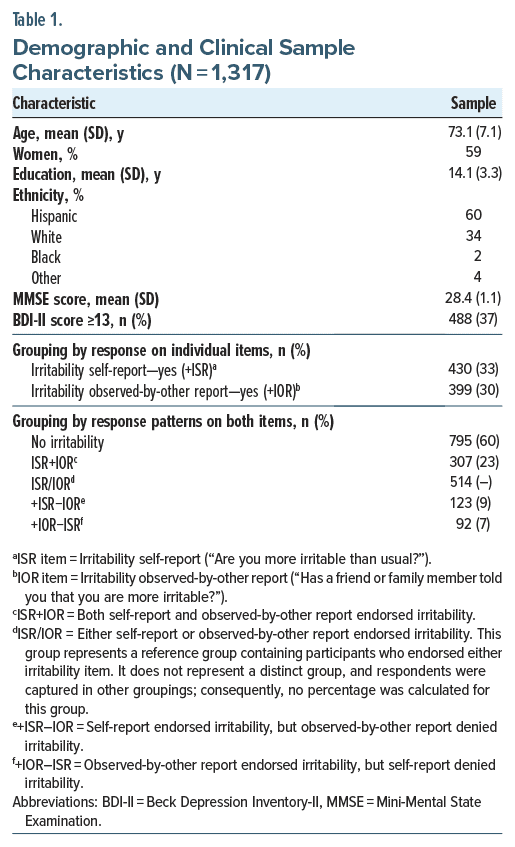
In total, 1,317 individuals met the inclusionary criteria for our analyses. Table 1 summarizes demographic and clinical information for the whole sample, as well as composition of groups defined by pattern of responding on ISR and IOR, singularly and in combination. Mean age for all groups was equivalent with similar sex and ethnic distributions. MMSE scores were nearly identical across the 5 groups.
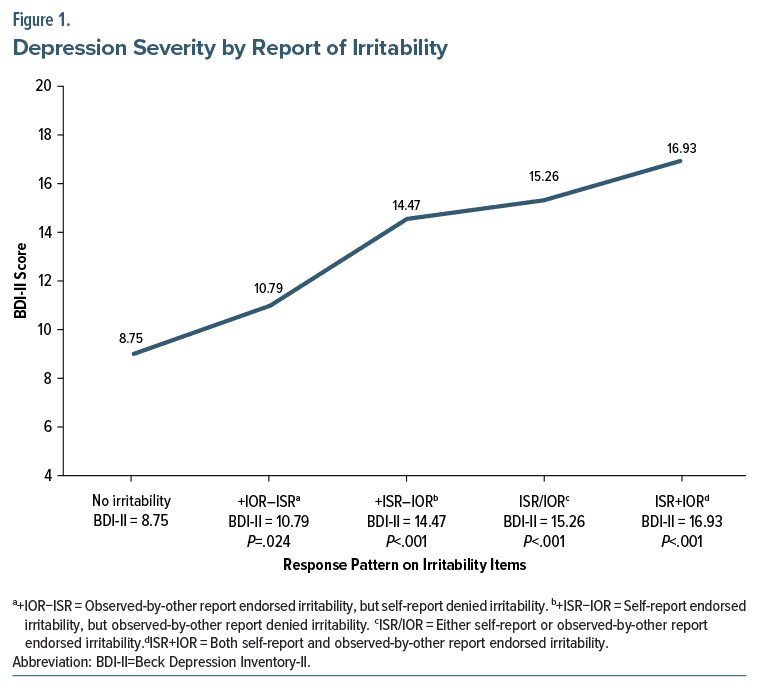
Comparing BDI-II scores for individuals with +ISR (n=430, mean=16.14, SD=9.38) vs those with –ISR (n=887, mean=8.94, SD=7.59) indicated significantly higher BDI scores (at the P<.001 level) for the +ISR group. A similar difference was obtained comparing the BDI-II scores of the +IOR group (n=399, mean=15.38, SD=9.76) vs the –IOR group (n=918, mean=9.51, SD=7.83), also at the P<.001 level. All t-test comparisons between the NI group and each of the 4 groups endorsing some combination of positive irritability yielded significant differences in BDI-II scores (Figure 1). Finally, for individuals scoring above the recommended cut point of 13 (n=488), a significantly higher rate of irritability was noted on ISR compared to those scoring below 13 (+ISR of 53.9% vs +ISR of 20.2%; P<.001).
DISCUSSION
The objective of this study was to determine the utility of irritability in detecting depression in geriatric individuals. Our concern regarding geriatric depression is based on the expected rise in its prevalence, its adverse impact on morbidity and mortality, and observations that it frequently goes undetected and untreated. We chose to focus on irritability because—despite recognition that it is a common element in depression that is more frequently reported in depressed vs nondepressed individuals17—it is not assessed by either the PHQ-9 or PHQ-2. Given observations that geriatric depression may present differently in primary care settings, with symptoms that are less typical and more somatic in nature,8,9 our concern has been that not assessing for irritability within this population may allow individuals screened with the PHQ to go undetected. Moreover, even when depression is detected, irritability as a component of the depressive episode has been associated with higher levels of anxiety, greater life dissatisfaction, increased morbidity/mortality (particularly cardiovascular disease), and elevated risk for suicide.3,7,15,16,18 Consequently, assessing for irritability may not only increase detection of geriatric depression but also facilitate identification of a subgroup of depressed individuals that may require more aggressive treatment and closer monitoring.
Our study is limited by a single-site design, which impacts generalizability of our findings. We encourage investigators at other sites working with geriatric individuals to systematically assess for the presence of irritability and depression to obtain data that would allow for comparison with other demographic samples.
This is the first study, to the best of our knowledge, to empirically characterize the relationship between irritability and geriatric depression. In our sample of individuals aged ≥60 years, irritability proved to be effective in distinguishing depressed from nondepressed individuals. We assessed for irritability not only by having individuals report on their own subjective experience of being irritable but also by asking whether others around them had commented on the presence of irritability. Even for individuals who denied experiencing irritability but acknowledged that others had observed their irritability, there was a significantly greater difference in level of depression (P<.05) compared to those who were denying any manifestation of irritability. In our sample, 54% of individuals who met criteria for depression on the BDI-II reported irritability (vs 20% who fell below the BDI-II depressive cut score, a significant difference at the P <.001 level). This association between irritability and depression is similar, if not slightly greater, than what has been noted in other cross-sectional studies with younger depressed individuals.14–17 Our data did not allow us to determine the percentage of depressed individuals demonstrating irritability who would nonetheless have been detected by routine screening with the PHQ-9; in light of our findings, we feel that this is an issue warranting additional investigation.
Irritability appears to be a useful marker to facilitate identification of geriatric depression, hopefully leading to its subsequent treatment. We believe our findings support the recommendation that practitioners working with older adults should move beyond routine screening instruments for depression and actively inquire as to the presence of irritability, either subjectively experienced by the individual or observed and commented upon by others, to increase detection rates of geriatric depression and develop appropriate therapeutic interventions.
Article Information
Published Online: January 30, 2025. https://doi.org/10.4088/PCC.24m03808
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 8, 2024; accepted October 1, 2024.
To Cite: Rivas-Vazquez RA, Diaz SG, Rodriguez C, et al. Importance of screening for irritability when assessing for geriatric depression. Prim Care Companion CNS Disord. 2025;27(1):24m03808.
Author Affiliations: First Choice Neurology, Miami, Florida (R.A. Rivas-Vazquez, Diaz, Rodriguez, E.V. Rivas-Vazquez); Division of Neuropsychology, Cognitive Neuroscience and Division of Epilepsy, Miller School of Medicine, University of Miami, Miami, Florida (Rey).
Corresponding Author: Rafael A. Rivas-Vazquez, PsyD, First Choice Neurology, 8940 N Kendall Dr #802e, Miami, FL 33176 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Although relatively common and associated with increased morbidity and mortality, geriatric depression oftentimes goes undetected and untreated.
- Irritability is frequently encountered in the geriatric population but is not assessed by routine depression screening instruments (possibly because irritability is not included as a diagnostic symptom in the current classification system).
- Detection and subsequent treatment of geriatric depression would be greatly enhanced if practitioners were to query for the presence of irritability.
References (23)

- Obuobi-Donkor G, Nkire N, Agyapong VIO. Prevalence of major depressive disorder and correlates of thoughts of death, suicidal behaviour, and death by suicide in the geriatric population—a general review of literature. Behavioral Sci. 2021;11(11):142. PubMed CrossRef
- Zenebe Y, Akele B, W/Selassie M, Necho M. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann Gen Psychiatry. 2021;20(1):55. CrossRef
- Gundersen E, Bensadon B. Geriatric depression. Prim Care. 2023;50(1):143–58. CrossRef
- 4. Population projections data. U.S. Census Bureau website. Accessed June 4, 2024. https://www.census.gov
- Fact sheet: Aging in the United States. Population Reference Bureau. Accessed June 4, 2024. https://www.prb.org/resources/fact-sheet-aging-in-the-united-states/
- Kessler RC, Birnbaum H, Bromet E, et al. Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R). Psychol Med. 2010;40(2):225–237. PubMed CrossRef
- Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):249–265. CrossRef
- Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s - delirium, dementia, and depression. Curr Psychiatry Rep. 2013;15(6):365. PubMed CrossRef
- Gallo JJ, Rabins PV. Depression without sadness: alternative presentations of depression in late life. Am Fam Physician. 1999;60(3):820–826. PubMed
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2022.
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. PubMed CrossRef
- Li C, Friedman B, Conwell Y, et al. Validity of the Patient Health Questionnaire 2 (PHQ-2) in identifying major depression in older people. J Am Geriatr Soc. 2007;55(4):596–602. PubMed CrossRef
- Benazzi F, Akiskal H. Irritable-hostile depression: further validation as a bipolar depressive mixed state. J Affect Disord. 2005;84(2–3):197–207. PubMed CrossRef
- Perlis RH, Fraguas R, Fava M, et al. Prevalence and clinical correlates of irritability in major depressive disorder: a preliminary report from the Sequenced Treatment Alternatives to Relieve Depression study. J Clin Psychiatry. 2005;66(2):159–274. PubMed
- Perlis RH, Fava M, Trivedi MH, et al. Irritability is associated with anxiety and greater severity, but not bipolar spectrum features, in major depressive disorder. Acta Psychiatr Scand. 2009;119(4):282–289. CrossRef
- Fava M, Hwang I, Rush AJ, et al. The importance of irritability as a symptom of major depressive disorder: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):856–867. PubMed CrossRef
- Judd LL, Schettler PJ, Coryell W, et al. Overt irritability/anger in unipolar major depressive episodes: past and current characteristics and implications for long term course. JAMA Psychiatry. 2013;70(11):1171–1180. PubMed CrossRef
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198.
- Beck AT, Steer RA, Brown G. Beck Depression Inventory–II (BDI-II) [Database Record]. APA PsycTests; 1996. https://doi.org/10.1037/t00742-000
- Rivas-Vazquez RA, Rey G, Quintana A, et al. Brief cognitive screener detects early signs of cognitive decline in Anglo and Hispanic patients. Prim Care Companion CNS Disord. 2023;25(6):23br03591. PubMed CrossRef
- Steer RA, Rissmiller DJ, Beck AT. Use of the Beck Depression Inventory II with depressed geriatric inpatients. Behav Res Ther. 2000;38(3):311–318. PubMed CrossRef
- von Glischinski M, von Brachel R, Hirschfeld G. How depressed is “depressed”? A systematic review and diagnostic meta-analysis of optimal cut points for the Beck Depression Inventory revised (BDI-II). Qual Life Res. 2019;28(5):1111–1118. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!