Abstract
Objective: To establish the prevalence of sleepiness in Colombian medical students and associated variables.
Methods: A cross-sectional study was conducted with the participation of university students aged ≥18 years. Students completed scales for sleepiness, insomnia, depressive symptoms, anxiety symptoms, sleep hygiene, and cognitive social capital (measured as social support) between September and November 2022. Raw and adjusted odds ratios (ORs) with 95% CIs were calculated.
Results: Three hundred nine students agreed to participate, of whom 169 (54.7%) were women. The prevalence of sleepiness was 53.1%, insomnia 41.1%, depression 61.2%, anxiety 31.1%, poor sleep hygiene 16.2%, and poor cognitive social capital 23.6%. Sleepiness was associated with the interaction of depression risk and poor cognitive social capital (OR = 4.08, 95% CI, 1.57–10.62) and insomnia risk (OR = 4.01, 95% CI, 2.34–6.89).
Conclusions: The prevalence of sleepiness is high among medical students and is associated with depression, anxiety, and insufficient social capital. Expanding knowledge about the variables related to sleepiness among university students is crucial.
Prim Care Companion CNS Disord 2025;27(1):24m03807
Author affiliations are listed at the end of this article.
According to research, sleepiness in medical students is highly prevalent, with around a third of students reporting this symptom.1,2 Jahrami et al1 reported a prevalence of sleepiness between 11% and 63%, with a pooled prevalence of 34.6%, in a meta analysis that included 2,582 medical college students. Similarly, Binjabr et al2 grouped 59,427 university students in a meta-analysis, and sleepiness prevalence ranged between 10% and 63%, with a pooled prevalence of 33.3%.
Sleepiness is frequently a leading symptom among people who meet the criteria for idiopathic hypersomnolence, narcolepsy, Kleine-Levin syndrome, and obstructive sleep apnea/hypopnea.3 Sleepiness is a secondary symptom associated with mental disorders such as anxiety disorders, depressive disorders, and primary insomnia.3–6 Similarly, people with sleep deprivation related to study, work, medical conditions, substance use, or lifestyle may report sleepiness.7–9 Sleepiness is a symptom of heterogeneous conditions or situations with multiple social health determinants among college or university students.10–12 The prevalence of sleepiness is usually significantly higher in medical students than in students taking other university courses.13
Some studies have reported that anxiety had a consistent association with sleepiness in medical students.14–18 Also, depression,14–17,19 social capital (measured as social support),20 and sleep hygiene could be related to sleepiness.21,22 However, depression and social support have been reported not to correlate with sleepiness in other studies.18,23,24 These divergent findings may be explained by the demographic and cultural heterogeneity of the participants, the instruments for measuring the variables, or the statistical analysis models.14–25
The current study examined the prevalence of sleepiness and simultaneously analyzed its association with anxiety, depression, social capital, sleep hygiene, and insomnia. These variables were adjusted for gender since previous investigations reported that sleepiness was significantly greater in women than men.13,15,26 Models were tested with all the variables significantly associated as independent factors and with the interaction between some of them. Epidemiologic studies are frequently powered primarily to assess the effect of 1 or more independent variables separately. Exploring interactions would allow for observation of the complex relationship between multiple independent variables and a dependent variable, such as sleepiness.27 No previous studies have reported the relationship between insomnia and sleepiness. The objective of the current study was to establish the prevalence of sleepiness and analyze some associated variables among medical students at a university in Santa Marta, Colombia.
METHODS
A cross-sectional study was conducted, and medical students from a Colombian public university in the Colombian Caribbean were invited to participate.
Participants and Sample Size
In Colombia, primary education lasts 5 years, and secondary education lasts 6 years. After completing these 11 years, students can study medicine. Medicine is taught in 12 semesters: the first 5 in introductory courses, 5 in clinical training, and 2 in a rotating internship. Generally, the best students enter medicine at public universities, like those who participated in this research. At this university, the medicine program has 223 credits, with a high academic load and a low rate of dropout, less than 5%.
Participation of 323 students would be adequate for an expected prevalence of sleepiness of 30%,1,2 with a confidence level of 95% and a margin of error of 5.28 This number of participants would also allow adjustment through logistic regression for up to 5 variables, approximated at a rate of 20 participants for each variable included.29 All students aged 18 years and older were invited to participate, and pregnant students were excluded.
Instruments
Students completed an online questionnaire that requested sociodemographic information such as age, sex (female or male), socioeconomic level, origin (urban or rural), and semester completed. Additionally, they completed scales to quantify cognitive social capital,30 sleep hygiene,31 insomnia,32 anxiety,33 depression,34 and sleepiness.35
Cognitive Social Capital Scale. The Cognitive Social Capital Scale (CSCS-5) explores the current perception of the relationship with neighbors. Each item presents 4 response alternatives, from completely disagree to completely agree, rated from 0 to 3. The higher the score, the greater the cognitive social capital.30 This study considers poor (between 0 and 5) and high (6 or more) capital.36 This scale has shown high internal consistency in the Colombian adult population.30 In the present study, the CSCS-5 showed high internal consistency, with a Cronbach α of 0.77.
Sleep Hygiene Index. The Sleep Hygiene Index (SHI-10) quantifies the activities of daily living that promote excellent sleep quality through 10 items that offer 5 response options rated from 0 to 4: the higher the score, the lower the sleep hygiene. The SHI-10 has presented high internal consistency among Spanish-speaking university students.31 Arbitrarily, scores were dichotomized into poor (inferior to 30) and excellent (30 or more) sleep hygiene. In the present study, the SHI-10 showed a Cronbach α of 0.72.
Athens Insomnia Scale. The Athens Insomnia Scale (AIS) includes 8 items that measure the hours and quality of sleep and associated daytime manifestations. The items offer 4 response options that are rated from zero to 3. Scores above 10 suggest insomnia with clinical significance (insomnia risk).32 The AIS presented high internal consistency in a previous Colombian study with the general population.36
Generalized Anxiety Disorder. The 7-item Generalized Anxiety Disorder scale compiles 7 items that explore anxiety symptoms during the most recent month, with 4 response options rated from zero (never) to 3 (almost every day). Scores ≥10 indicate anxiety symptoms with clinical significance (anxiety risk).33 This instrument has shown excellent internal consistency in Colombian adults.37 The internal consistency was notable in the present sample, with a Cronbach α of 0.91.
Patient Health Questionnaire-9. The 9-item Patient Health Questionnaire (PHQ-9) assesses depressive symptoms based on DSM-5 criteria. It has 9 items with 4 response options rated from zero (not at all) to 3 (almost every day). Scores greater than 9 were classified as clinically significant depressive symptoms (depression risk).34 The PHQ-9 has shown high internal consistency among Colombian medical students.38 In the current student sample, internal consistency was high, with a Cronbach α of 0.88.
Epworth Sleepiness Scale. The Epworth Sleepiness Scale (ESS) investigates how often people fall asleep in 8 different situations in daily life. The ESS offers 4 response options, scored from zero (unlikely) to 3 (highly probable). Scores above 10 indicate excessive sleepiness.35 The ESS has presented high internal consistency in Colombian patients with chronic obstructive sleep apnea.39 In this group of students, the ESS showed an internal consistency of 0.80 (Cronbach α).
Procedure
The students completed the questionnaire in a classroom on the university campus. The application was made collectively after asking and excluding minors and students who reported being pregnant. Students who agreed to participate were sent the link to the Google Form questionnaire; they were given a tablet to complete the form if they did not have a mobile phone at the time of application. The questionnaire was displayed if they responded affirmatively to the informed consent. The item-by item format was preferred because the grid format can induce more errors in the response.40 All questions were mandatory to ensure values were present. Completion of the form took around 20 minutes. The information was collected between September and November 2022.
Data Analysis
The descriptive analysis included observing frequency and percentage for categorical variables and calculating mean and SD for continuous variables.
Sleepiness was taken as the dependent variable. The bivariate analysis took sleep hygiene (categorical) as the dependent variable, demographic variables, and measurements with scales as independent variables. Cognitive social capital, sleep hygiene, insomnia, anxiety, and depression were the independent variables, and the demographic variables (age, sex, semester, origin, and income) were handled as covariates. Crude and adjusted odds ratios (ORs) and 95% CIs were calculated.
The independent variables were adjusted for each other, as individuals or in interaction with another, and for significant covariates or with probability values less than 20%.41 The Hosmer-Lemeshow test was used to determine the goodness of fit of the final model. The model with a P value more significant than .05 was accepted. Finally, the Nagelkerke R2 was calculated to determine the variance explained by the model.42 Statistical analysis was completed using IBM-SPSS statistical software.43
Ethical Statement
According to minutes 005 of the ordinary virtual session of June 9, 2022, the Institutional Ethics Committee of the university approved this project. The students signed an informed consent form, and free measurement scales were used. No clinical interventions were performed. A sleepiness prevention manual was cocreated with a group of students and distributed free of charge in the academic community.
RESULTS
Descriptive Analysis
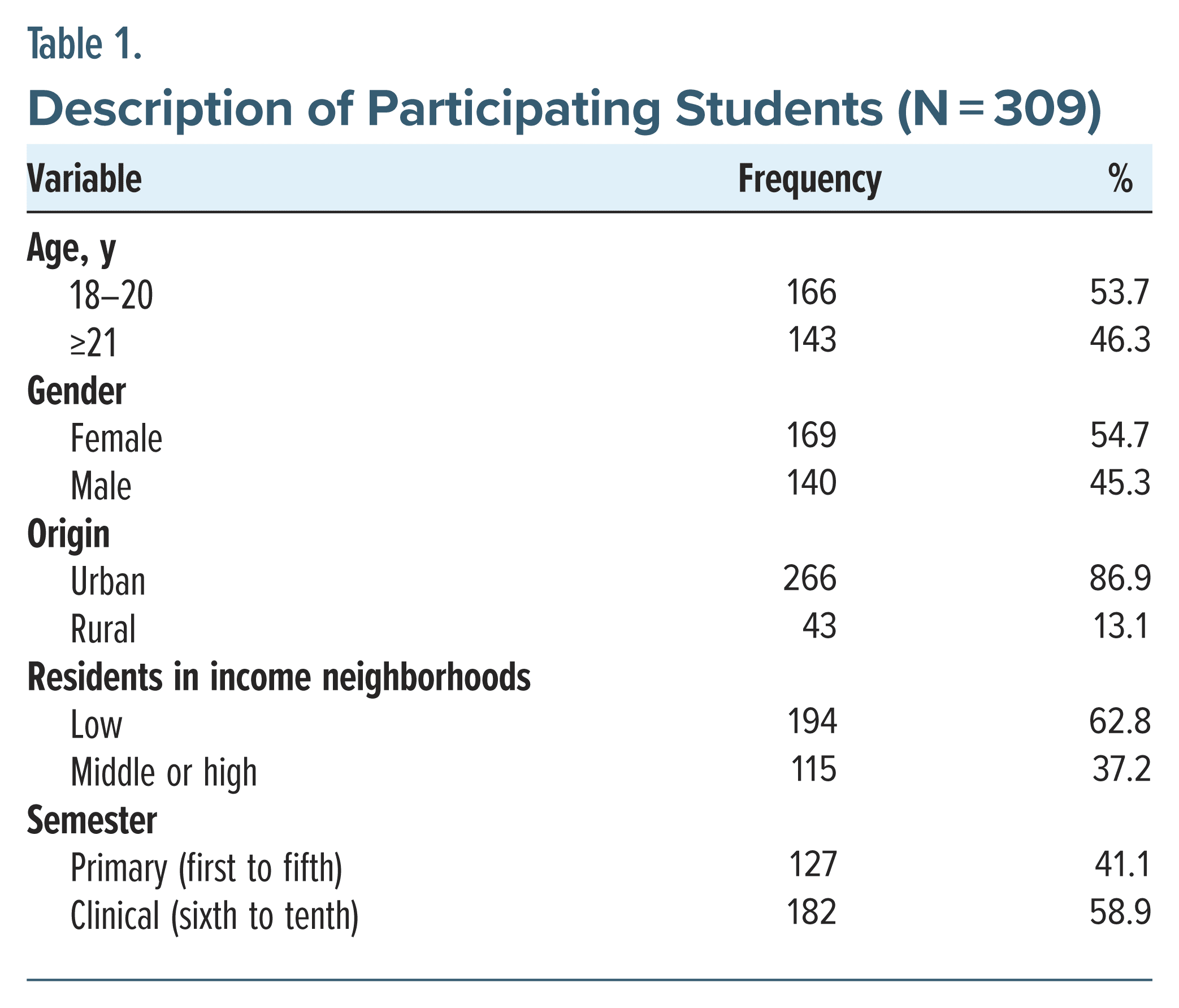
Three hundred nine students aged between 18 and 39 years participated (mean = 20.8, SD = 2.7). The most significant percentage of participants was women, between 18 and 20 years old, from urban areas, living in low-income neighborhoods, and taking a clinical semester. More dichotomized demographic variables are provided in Table 1.
Bivariate and Multivariate Analyses
For the independent variables, the frequency and percentages were 73 (23.6%) for poor cognitive social capital, 50 (16.2%) for poor sleep hygiene, 127 (41.1%) for risk of insomnia, 96 (31.1%) for risk of generalized anxiety, and 189 (61.2%) for risk of depression. Finally, 164 students (53.1%) presented excessive daytime sleepiness.
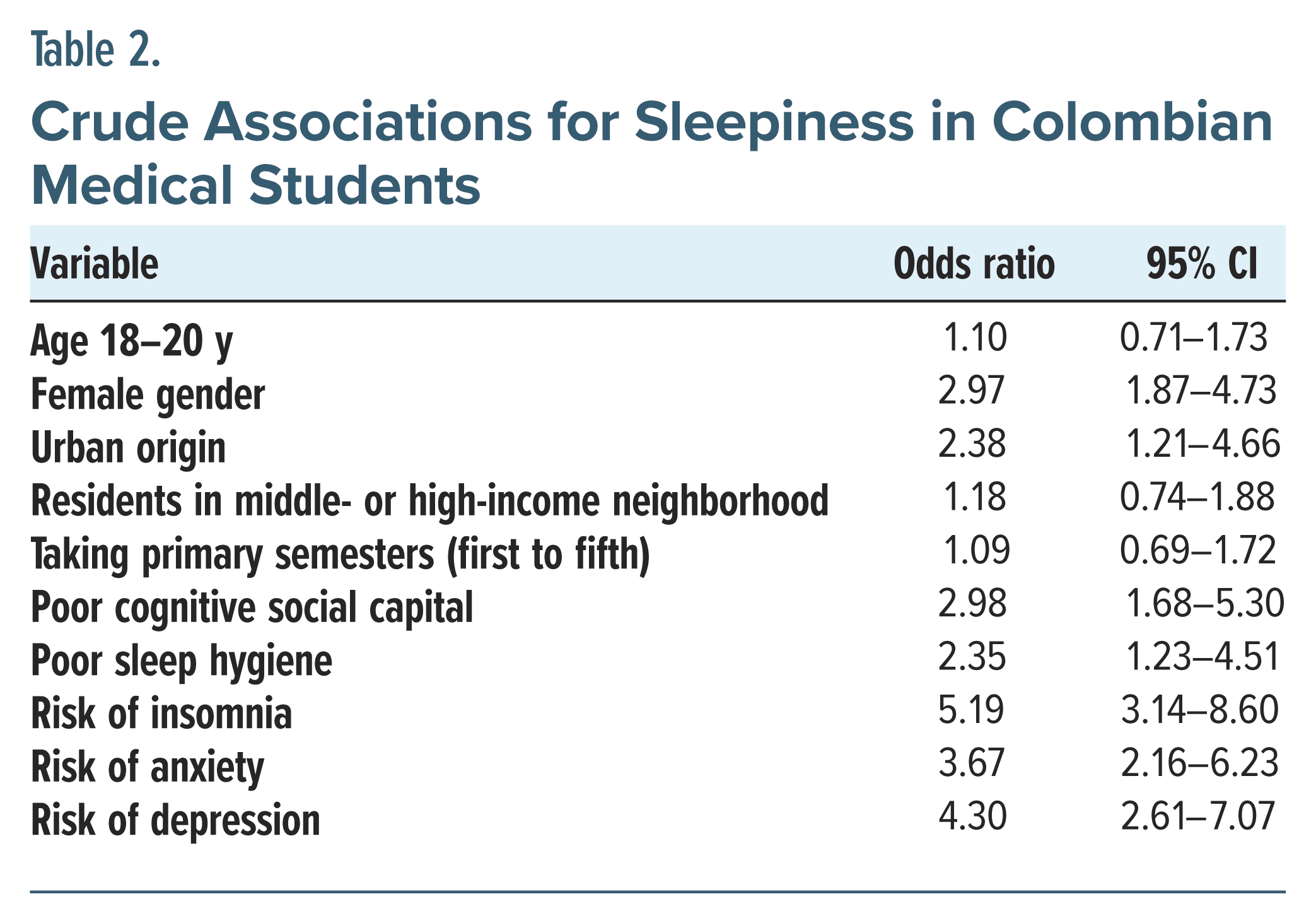
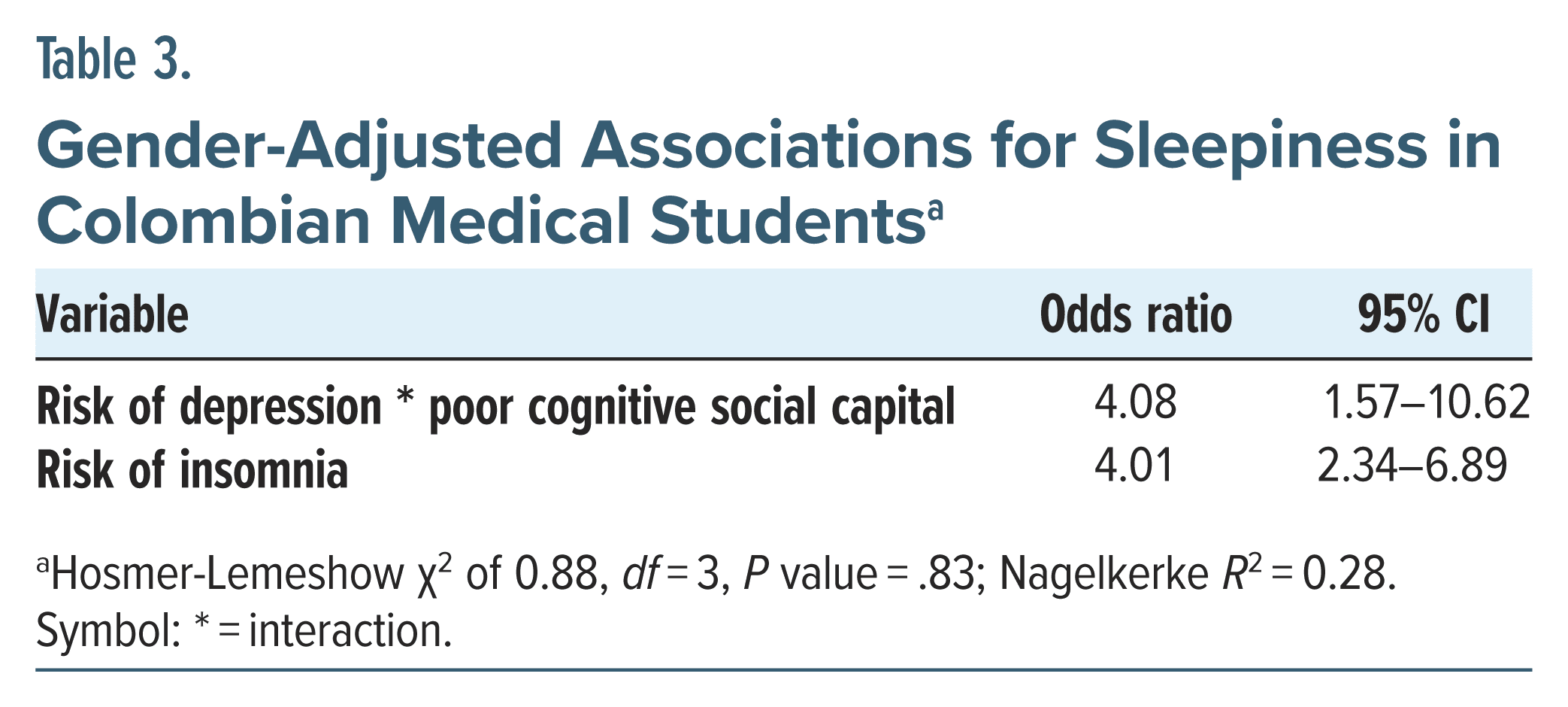
All independent variables (cognitive social capital, sleep hygiene, insomnia, anxiety, and depression) and the gender covariate showed a statistically significant crude association with sleepiness. Consequently, gender was considered for the adjustment of the independent variables. Table 2 provides the ORs and 95% CIs. Finally, the interaction between depression, cognitive social capital, and insomnia (as an independent variable) showed a statistically significant gender-adjusted relationship with sleepiness. Anxiety and sleep hygiene lost statistical significance during the adjustment process and were excluded from the final model. The final model fit adequately and explained 28% of the variance (Nagelkerke R2)—model details are provided in Table 3.
DISCUSSION
In the present study, a prevalence of sleepiness of 53.1% was observed. This finding is above the world average reported among medical colleges or universities.1,2 In a meta-analysis of 9 studies that included 2,582 participants from medical colleges, sleepiness measured with the ESS was between 11% and 63%, with a pooled prevalence of 34.6% (95% CI, 18.3–50.9).1 In another meta-analysis that reviewed 109 studies that grouped 59,427 university students, it was reported that the prevalence of sleepiness, measured with the ESS, was between 10.3% and 63.0%, with a pooled prevalence of 33.3% (95% CI, 26.5–40.9). Additionally, the authors broke down the prevalence before and during the COVID-19 pandemic and noted that the frequency of sleepiness was higher than before, 54.5% vs 28.6%.2 This variability in findings shows the variability of prevalence possibly related to the variables and social determinants associated with each sample of medical students.4–9
Depression risk, insomnia risk, and poor cognitive social capital showed a statistically significant association with sleepiness in the present sample of Colombian students; however, somnolence was independent of anxiety risk and poor sleep hygiene. Previous studies showed similar findings for depression risk14–17,19 and poor cognitive social capital.20 However, other studies reported the independence of sleepiness from depression and social support, a measurement highly correlated with social capital.18,23,24
The relationship between insomnia and sleepiness among medical students had previously been ignored. However, daytime sleepiness may be present in people with difficulty falling or staying asleep or waking up early.3,5 Researchers should prioritize considering academic overload as a predictor of excessive daytime sleepiness among university students, particularly medical students. The degree’s study plans involve a large volume of reading in the primary semesters, to which are added long hours of practice that require a reduction in the usual hours of sleep.44
The current study shows that sleepiness was independent of anxiety risk and poor sleep hygiene after controlling for the block variables. Previous studies among medical students reported a statistically significant association between anxiety and sleepiness.14–18 The instrument used to measure anxiety may explain the difference. This research is the first study to our knowledge that applied the GAD-7 to measure anxiety33; this instrument was constructed based on the American Psychiatric Association criteria for generalized anxiety disorder and, consequently, is a measure of anxiety closer to the contemporary clinical approach.3 On the other hand, some previous studies documented that poor sleep hygiene increased the risk of sleepiness in medical students.21,22 The divergence between the findings presented is frequent in epidemiologic studies, possibly explained by the characteristics, demographics, cultural differences, and other social determinants of sleep health.45
Practical Implications
It is crucial to investigate the prevalence and the situations or variables that may be related to sleepiness in medical students and students in other fields.46 It is essential to identify the cause or associated factors, given that sleepiness is a symptom common to several clinical conditions and physical and mental health situations or problems.3–9 For example, managing depressive symptoms, common in higher education students, would help reduce the frequency of sleepiness in the student population.46
It is essential that sleep hygiene is promoted throughout the academic community and that risk factors for sleepiness in university students are identified early, particularly in high-risk students such as medical students.13,46 Healthy sleep is a fundamental condition for the cognitive activities necessary for learning and the level of academic achievement expected by students, families, and academic authorities.44 University students may need more hygiene practices supporting sleep health.47 Poor sleep behaviors ultimately lead to poor sleep health, resulting in diminished quantity and quality of sleep and excessive daytime sleepiness.48 Sleep hygiene programs can be beneficial in preventing and managing this problem. Sleep hygiene programs can be implemented on college campuses to encourage regular schedules and sleep-friendly environments, daily physical activity, and eating habits by reducing stimulant substances such as caffeine. These strategies promote a repairing and sound sleep.46 All university levels can commit to this task. For example, the governing board may limit class schedules and semester academic load, and professors could be educators and guides in promoting sleep health.46,49 Moreover, university student welfare offices can promote mental health and the early identification of psychological distress, such as anxiety or depression. These actions can improve the sleep quality and general well-being of university students.46
Study Strengths and Limitations
This study had the strength of simultaneously exploring the association of sleepiness with cognitive social capital, sleep hygiene, insomnia, anxiety, and depression. Furthermore, possible interactions between these variables were tested during the analysis, given their complex relationship with sleepiness.27 However, it can be considered a limitation that there were 14 fewer participants than initially calculated and expected, and there is the possibility of type 2 error due to the wide CIs for variables such as sleep hygiene and anxiety.50 Furthermore, the measurement of variables such as perception of overload or academic performance that could be significant predictors in this population was omitted.47 Future research should consider these points and expand the sample size.45,50
CONCLUSION
Sleepiness is a common complaint and affects 1 out of 2 medical students in Santa Marta, Colombia. In this group of students, sleepiness is significantly related to depression, anxiety, and insufficient social capital. It is necessary to expand knowledge about the variables related to sleepiness among university students and take preventive measures and actions to manage cases.
Article Information
Published Online: February 18, 2025. https://doi.org/10.4088/PCC.24m03807
© 2025 Physicians Postgraduate Press, Inc.
Submitted: July 6, 2024; accepted October 3, 2024.
To Cite: Campo-Arias A, Pedrozo-Pupo JC, Caballero-Domínguez CC. Sleepiness in Colombian medical students: prevalence and associated variables. Prim Care Companion CNS Disord. 2025;27(1):24m03807.
Author Affiliations: Universidad del Magdalena, Santa Marta, Magdalena, Columbia (all authors).
Corresponding Author: Adalberto Campo-Arias, MD, MSc, Universidad del Magdalena, Calle 29H3 No. 22-01, Santa Marta 470004, Colombia ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Sleepiness affects half of Colombian medical students.
- Sleepiness is often associated with symptoms of anxiety, insomnia, and poor cognitive social capital.
- It is necessary to screen for sleepiness in medical students, establish the cause, and manage the cases.
References (50)

- Jahrami H, Alshomili H, Almannai N, et al. Predictors of excessive daytime sleepiness in medical students: a meta-regression. Clock Sleep. 2019;1(2):209–219. PubMed CrossRef
- Binjabr MA, Alalawi IS, Alzahrani RA, et al. The worldwide prevalence of sleep problems among medical students by problem, country, and COVID-19 status: a systematic review, meta-analysis, and meta-regression of 109 studies involving 59427 participants. Curr Sleep Med Rep. 2023;9(3):161–219.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision. American Psychiatric Association; 2022.
- Simon EK, Berki ZH, Gettys GC, et al. Sleep problems and disorders in patients with anxiety disorders. Psychiatr Ann. 2016;46(7):396–400.
- Hein M, Lanquart JP, Loas G, et al. Prevalence and risk factors of excessive daytime sleepiness in insomnia sufferers: a study with 1311 individuals. J Psychosom Res. 2017;103(1):63–69. PubMed CrossRef
- Hein M, Lanquart JP, Loas G, et al. Prevalence and risk factors of excessive daytime sleepiness in major depression: a study with 703 individuals referred for polysomnography. J Affect Disord. 2019;243:23–32. PubMed CrossRef
- Leibowitz SM, Lopes MC, Andersen ML, et al. Sleep deprivation and sleepiness caused by sleep loss. Sleep Med Clin. 2007;1(1):31–45.
- Singh R, Sharma R, Suri JC, et al. Is daytime napping a healthy habit in adolescents? Indian J Sleep Med. 2009;4(4):136–142.
- Singh R, Sharma R, Suri JC, et al. Effect of early school timings on mood and performance of students. Indian J Sleep Med. 2010;5(3):88–94.
- Kelly RJ, Bagley EJ, Gordon JD. Sleep and internalizing symptoms in emerging adulthood: the role of ethnicity and subjective social status. Emerg Adulthood. 2018;6(5):299–311.
- Becerra MB, Bol BS, Granados R, et al. Sleepless in school: the role of social determinants of sleep health among college students. J Am Coll Health. 2020;68(2):185–191. PubMed CrossRef
- Lin CY, Imani V, Griffiths MD, et al. Temporal associations between morningness/ eveningness, problematic social media use, psychological distress and daytime sleepiness: mediated roles of sleep quality and insomnia among young adults. J Sleep Res. 2021;30(1):e13076. PubMed
- Dutra da Silva RC, Garcez A, Pattussi MP, et al. Prevalence and factors associated with excessive and severe daytime sleepiness among healthcare university students in the Brazilian Midwest. J Sleep Res. 2022;31(3):e13524.
- Mume CO, Olawale KO, Osundina AF. Excessive daytime sleepiness, nocturnal sleep duration and psychopathology among Nigerian university students. South Afr J Psychiatry. 2011;17(4):108–111.
- Concepcion T, Barbosa C, Vélez JC, et al. Daytime sleepiness, poor sleep quality, eveningness chronotype, and common mental disorders among Chilean college students. J Am Coll Health. 2014;62(7):441–448. PubMed CrossRef
- Shen Y, Meng F, Tan SN, et al. Excessive daytime sleepiness in medical students of Hunan province: prevalence, correlates, and its relationship with suicidal behaviors. J Affect Disord. 2019;255:90–95. PubMed CrossRef
- Barbosa-Medeiros MR, Lopes Mendes Figueiredo JF, de Oliveira Melo L, et al. Factors associated with daytime sleepiness in medical students. Rev Pesq Cuid Fundam. 2021;13(1):774–779.
- Mohamad Sobri WBW, Naing NN, Wan-Arfah N, et al. Prevalence and factors associated with excessive daytime sleepiness among Malaysian medical students. Electron J Gen Med. 2024;21(2):em571.
- Dagnew B, Andualem Z, Dagne H. Excessive daytime sleepiness and its predictors among medical and health science students of University of Gondar, Northwest Ethiopia: institution-based cross-sectional study. Health Qual Life Outcome. 2020;18(1):299. PubMed CrossRef
- Chen S, Li H, Wen D. Social support and daytime sleepiness among Chinese medical students: mediating roles of loneliness and problematic smartphone use. Psychol Res Behav Manag. 2023;16(2023):4083–4093.
- Escobar-Córdoba F, Benavides-Gélvez R, Montenegro-Duarte G, et al. [Excessive daytime drowsiness in ninth-semester medical students attending the Universidad Nacional de Colombia]. Rev Fac Med. 2011;59(3):191–200.
- Niño García JA, Barragán Vergel MF, Ortiz Labrador JA, et al. [Factors associated with excessive daytime sleepiness in medical students of a higher education institution of Bucaramanga]. Rev Colomb Psiquiatr. 2019;48(4):222–231.
- Robbins R, Jean-Louis G, Gallagher RA, et al. Examining social capital in relation to sleep duration, insomnia, and daytime sleepiness. Sleep Med. 2019;60:165–172. PubMed CrossRef
- Garbuio ALP, Carvalhal TAO, Tomcix MFR, et al. Sleep quality, latency, and sleepiness are positively correlated with depression symptoms of Brazilians facing the pandemic-associated stressors of COVID-19. Medicine. 2022;101(33):e28185.
- Kintschev MR, Shimada SS, Silva MOD, et al. Chronotype change in university students in the health area with excessive daytime sleepiness. Rev Bras Educ Med. 2021;45:e031.
- Monsalve K, García SP, Chávez FD, et al. [Prevalence of insomnia and sleepiness in medical students belonging to an educational institution of Medellin (Colombia), 2013]. Arch Med. 2014;14(1):92–102.
- VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Method. 2014;3(1):33–72.
- Lakens D. Sample size justification. Collabra. 2022;8:33267.
- Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. John Wiley & Sons; 2013.
- Campo-Arias A, Caballero-Domínguez CC, Pedrozo-Pupo JC. Internal consistency and dimensionality assessment of the Cognitive Social Capital Scale among Colombian adults. Med Clin Soc. 2024;8(1):75–83.
- Prados G, Chouchou F, Carrión-Pantoja S, et al. Psychometric properties of the Spanish version of the Sleep Hygiene Index. Res Nurs Health. 2021;44(2):393–402.
- Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555–560. PubMed CrossRef
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. PubMed CrossRef
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. PubMed CrossRef
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. PubMed CrossRef
- Caballero-Domínguez CC, De Luque-Salcedo JG, Campo-Arias A. Social capital and psychological distress during Colombian coronavirus disease lockdown. J Community Psychol. 2021;49(2):691–702.
- Monterrosa-Blanco A, Cassiani-Miranda CA, Scoppetta O, et al. Generalized anxiety disorder scale (GAD-7) has adequate psychometric properties in Colombian general practitioners during COVID-19 pandemic. Gen Hosp Psychiatry. 2021;70:147–148.
- Cassiani-Miranda CA, Vargas-Hernández MC, Pérez-Anibal E, et al. [Reliability and dimensionality of PHQ-9 in screening symptoms of depression among health science students in Cartagena, 2014]. Biomedica. 2017;37(0):112–120. PubMed CrossRef
- Pedrozo-Pupo JC, Córdoba AP, Campo-Arias A. [Factor structure and internal consistency of the Epworth Sleepiness Scale]. Rev Fac Med. 2020;68(2):183–187.
- Revilla M, Toninelli D, Ochoa C. An experiment comparing grids and item-by-item formats in web surveys completed through PCs and smartphones. Telemat Inf. 2017;34(1):30–42.
- Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–349. PubMed CrossRef
- Nagelkerke NJ. A note on a general definition of the coefficient of determination. Biometrika. 1991;78(3):691–692.
- IBM Corp. IBM SPSS Statistics for Windows, Version 24.0. IBM Corp; 2016.
- Carrión-Pantoja S, Prados G, Chouchou F, et al. Insomnia symptoms, sleep hygiene, mental health, and academic performance in Spanish university students: a cross-sectional study. J Clin Med. 1989;2022(7);11.
- Ahrens W, Pigeot I. Handbook of Epidemiology. Springer; 2007.
- McNeil MP, Davidson ES. Sleep college and university campuses. In: Vaughn JA, Viera AV, eds. Principles and Practice of College Health. Springer;2021:233–245.
- Begum M, Chandana Puchakayala DS. Study to determine prevalence of poor sleep quality and its correlation with sleep hygiene practices among medical students. Asian J Med Sci. 2022;13(9):151.
- Carrillo-Mora P, Fonseca-Vázquez DM, Magaña-Vázquez K, et al. Poor sleep quality in medical students is related to sleep habits and emotional symptoms: a pilot study conducted in México. Sleep Vigil. 2021;5:99–102.
- Hughes AJ, Gunn H, Siengsukon C, et al. Eliminating sleep health disparities and achieving health equity: seven areas for action in the behavioral sleep medicine community. Behav Sleep Med. 2023;21(5):633–645.
- Bolarinwa OA. Sample size estimation for health and social science researchers: the principles and considerations for different study designs. Niger Postgrad Med J. 2020;27(2):67–75. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!